Abstract
Objectives:
To examine the relationship between plasma lipid measurements and incident ischemic vascular events (ischemic stroke [IS], and as a positive control, myocardial infarction [MI]) in a community cohort.
Methods:
In 6,276 stroke-free Framingham participants (aged 64 ± 10 years, 56% female), we related plasma lipid levels (total cholesterol [TC], high-density lipoprotein cholesterol [HDL-C], and TC/HDL-C ratio) measured at the original cohort 15th (1977–1979) and 20th examination cycles (1986–1990) and (TC, HDL-C, TC/HDL-C ratio, triglycerides [TG], and low-density lipoprotein cholesterol [LDL-C]) measured at the offspring fourth examination (1995–1998), to 10-year risk of incident IS and MI. Utilizing genome-wide genotyping in the same subjects, we used mendelian randomization methods to assess whether observed associations were incidental or causal.
Results:
During a mean follow-up of 9 years, 301 participants experienced incident IS. In multivariable-adjusted analyses, HDL-C ≤40 mg/dL and TC/HDL ratio ≥5 were associated with increased risk of IS (hazard ratio [95% confidence interval]: 1.59 [1.23–2.05], p < 0.001 and 1.47 [1.15–1.87], p < 0.001), but not TC or LDL-C. In adjusted analysis, a strong association between TG and IS was diminished. In the MI-free sample (n = 5,875, aged 64 ± 10 years, 58% female; 403 MI events), all lipid markers were associated with MI risk. A genetic risk score comprising 47 known determinants of circulating HDL-C was not associated with IS.
Conclusions:
In a middle-aged to elderly community sample, we observed that low HDL-C and high TC/HDL-C ratio, but not LDL-C or TG were associated with risk of incident IS. We observed the usual associations between lipids and risk of MI. Our findings suggest an important, but less likely causal, role of HDL-C over other lipid biomarkers for optimal stroke risk stratification.
The role of lipid and lipoprotein biomarkers, such as of total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and triglycerides (TG), in risk prediction of ischemic heart disease is well established,1–3 but their value as independent predictors for ischemic stroke (IS) is less certain.
Given the methodologic and/or population differences, studies evaluating the relationship between lipids and the risk of stroke show variable results.4–14 Ascertainment of vascular events varies among studies; few have utilized the clinical records and objective clinical evidence at the time of the event as has the Framingham Heart Study (FHS). Furthermore, while the majority of studies used a combined endpoint of all strokes (ischemic and hemorrhagic) and rarely discriminated among stroke subtypes,4,5,8,15,16 only a few studies examined the value of a wide range of lipid biomarkers in risk prediction of IS.4,7,8,15,16 Therefore, some studies found increased risk of stroke with higher TC and/or lower HDL-C,4–8 while others did not. Little attention has been given to the TC/HDL-C ratio.7,8 Recent studies found an inverse association between nonfasting TG and risk of IS.14,15 An association between risk of stroke and LDL-C remains even less consistent.7,10,11 Large clinical trials have shown that statins, which among other things lower LDL-C levels, reduced the risk of IS in patients with prior stroke/TIA or in high-risk populations.17 Thus, the underlying mechanism of these associations in primary and secondary stroke prevention remains a subject of great interest.
We therefore related a variety of plasma lipid measurements (TC, HDL-C, TC/HDL-C ratio, TG, and LDL-C levels) to incident IS and for comparison, myocardial infarction (MI), in our middle-aged and elderly community cohorts.
METHODS
Study sample.
The design and selection criteria for FHS have been published for this community-based prospective study under way since 1948, an original cohort of 5,209 men and women.18 The offspring cohort of 5,124 participants was added in 1971.19 Both cohorts have been under ongoing surveillance and periodic in-person evaluations for cardiovascular disease (CVD) events (stroke and MI). Ten-year follow-up periods from baseline original cohort examination cycles 15 (1977–1979) and 20 (1986–1990) and offspring cohort examination cycle 4 (1995–1998) were pooled. Stroke-free attendees aged 45 to 84 years with available lipid measures and stroke follow-up were included in our sample as follows: original cohort examination 15 (n = 2,373, aged 69 ± 7 years, 59% female), original cohort examination 20 (n = 1,073, aged 75 ± 4 years, 61% female), and offspring examination 4 (n = 2,830, aged 57 ± 7 years, 51% female). Our primary analyses, examining associations between lipid measures and stroke incidence, were performed in the pooled sample of 6,276 individuals (aged 64 ± 10 years, 56% female); for analyses of incident MI, participants with prevalent MI at baseline were excluded, yielding a sample of 5,879 (aged 64 ± 10 years, 58% female).
Lipid/lipoprotein measurements.
Plasma concentrations of lipid biomarkers were measured on previously stored and frozen blood samples. TC and HDL-C were measured at each of the 3 examinations; in addition, TG and LDL-C were measured at offspring examination cycle 4. All measurements were performed using previously reported methods specific for each lipid/lipoprotein biomarker.20–22 Given that TC/HDL-C ratio predicts coronary heart disease risk regardless of the absolute LDL-C and HDL-C,23 we also calculated the TC/HDL-C ratio using available TC and HDL-C values.
Outcomes and covariates.
Criteria for cardiovascular events have been described previously.24 Medical records obtained for all hospitalizations and physician visits related to MI or stroke during follow-up were reviewed by a committee of 2 or 3 investigators; all events were adjudicated following written guidelines. Our protocol for determining the diagnosis and stroke type has been previously published.25 Stroke was defined as an acute-onset focal neurologic deficit of presumed or definite vascular etiology persisting for ≥24 hours. When available, we utilized the data on clinical features, imaging studies, noninvasive vascular studies, and cardiac evaluations and information from autopsy studies. Stroke was classified as (1) ischemic stroke (defined as all IS including embolic strokes), and (2) atherothrombotic brain infarcts (ABIs; defined as all IS excluding embolic strokes).
Previously described and validated components of the Framingham Stroke Risk Profile (FSRP) (age, sex, hypertension, diabetes, smoking status, previous CVD, and atrial fibrillation) were used as baseline covariates.25 Given the established evidence that high TG and low HDL-C are associated with obesity and metabolic syndrome,26 we also included body mass index as a baseline covariate.
Single nucleotide polymorphisms and genotyping.
Genome-wide genotyping was available for all participants with good quality DNA. Methods for genotyping are provided in appendix e-1 on the Neurology® Web site at Neurology.org.27 Of 6,276 participants available for the analysis of plasma HDL-C levels and IS, 3,840 also had adequate genotypic data after quality control and there were 102 cases of incident IS in this subsample. Recent genome-wide association studies have identified common DNA sequence variants that contribute to blood HDL levels.28
Statistical analysis.
Lipid measurements with skewed distributions were log-transformed. Plasma concentrations of each lipid/lipoprotein value were analyzed both as continuous (TC per 10 units and lipid value per 1 SD for others) and using standardized cutpoints to create dichotomized indicator variables. Cutoffs for each lipid measurement were adopted from the National Cholesterol Education Program Adult Treatment Panel III29: high TC = ≥240 mg/dL; low HDL-C = ≤40 mg/dL; high LDL-C = ≥160 mg/dL; high TG = ≥200 mg/dL; and high TC/HDL-C ratio = ≥5. We used Cox proportional hazards techniques to relate each lipid/lipoprotein measurement to 10-year risk of incident IS, ABI, and MI. Primary analysis was done using 2 multivariable models: model 1 (adjusted for age and sex) and model 2 (adjusted for age, sex, hypertension, smoking, prevalent CVD, atrial fibrillation, diabetes mellitus, and body mass index). We investigated interactions with sex and age (<65 vs ≥65 years) and performed sex- and age-stratified analyses. In a secondary analysis, for stroke outcomes only, we adjusted for interim MI.
To examine the incremental utility of lipid/lipoprotein biomarker to age, sex, and components of the FSRP in predicting 10-year risk of IS, we calculated net reclassification improvement for markers found to have a significant effect on risk of IS in model 2.30 All analyses were performed using Statistical Analysis System (SAS Institute Inc., Cary, NC).
In our genetic analyses, we used single nucleotide polymorphisms (SNPs) previously associated with HDL levels (n = 47) to construct a genetic score that is a sum of number of copies of minor alleles at each SNP weighted by the effect size per copy of the minor allele on HDL levels in our study sample. Then we tested whether this genetic score was associated with risk of IS.
Cox proportional hazards models (with generalized estimating equations to adjust for familial relationships) were used in relating the genetic score to incident IS adjusting for age, sex, and cohort (original or offspring) status. All genetic analyses were performed using R survival package.
Standard protocol approvals, registrations, and patient consents.
The institutional review board at Boston University approved this study and all participants provided written consent.
RESULTS
The baseline characteristics and lipid/lipoprotein levels are provided in table 1. The mean follow-up period for stroke (IS and ABI) and MI was 9 years (0–10).
Table 1.
Baseline characteristics

TC, HDL, and TC/HDL ratio and ischemic events.
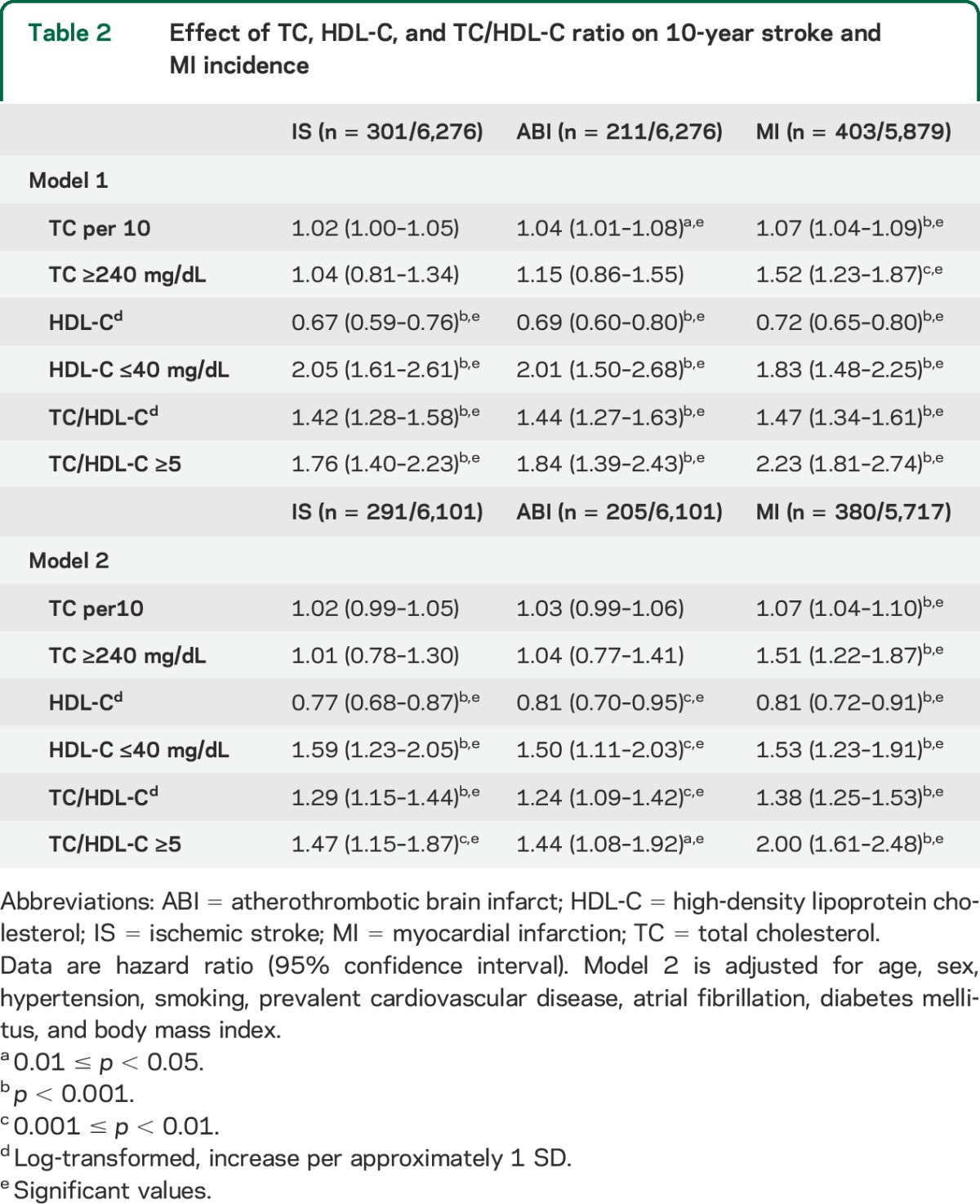
In the pooled sample, we observed 301 incident IS, 211 ABI, and 403 MI events. In age- and sex-adjusted analysis, we observed statistically significant associations between both low HDL-C and high TC/HDL-C ratio (using continuous and categorical measures) and increased risk of incident ischemic stroke (IS and ABI) and MI events (table 2). These associations remained statistically significant for all ischemic events in model 2 (for IS: hazard ratio [HR] per SD increase in HDL-C: 0.77, 95% confidence interval [CI] 0.68–0.87, p < 0.001; and for HDL-C ≤40 mg/dL: 1.59 [1.23–2.05], p < 0.001; for ABI: HR/SD HDL-C: 0.81 [0.70–0.95], p < 0.001; and for HDL-C ≤40 mg/dL: 1.50 [1.11–2.03], p < 0.001; and for MI: HR/SD HDL-C: 0.81 [0.72–0.91], p < 0.001; and for HDL-C ≤40 mg/dL: 1.53 [1.23–1.91], p < 0.001, respectively) and after adjustment for interim MI (table e-1). In table e-2, we present results based on IS subtypes: (1) ABI including large artery atherosclerosis, lacunar infarcts or small artery occlusion, and infarcts of unknown origin (cryptogenic); and (2) cardioembolic; in addition, we show that our results were similar for lacunar and nonlacunar ABIs.
Table 2.
Effect of TC, HDL-C, and TC/HDL-C ratio on 10-year stroke and MI incidence
The association between HDL-C and ischemic events was similar in men and women (table 3). However, there was a significant interaction between age and HDL-C such that low HDL-C on risk of IS and ABI was stronger in participants younger than 65 years. There was also an interaction between sex and TC. In women only, higher TC increased risk of ABI events. There were no significant interactions with TC/HDL.
Table 3.
Effect of TC, HDL-C, and TC/HDL-C ratio on 10-year stroke and MI incidence stratified by sex and age

In reclassification analyses (table e-3), HDL-C ≤40 mg/dL when added to a risk assessment model based on stroke risk factors alone (as identified by the FSRP) resulted in significant improvement of risk prediction (net reclassification improvement for HDL-C = 0.307, 95% CI 0.185–0.417).
The associations between all lipid/lipoprotein biomarkers and incident MI were, as expected, consistent in all presented analyses.
HDL genetic score and risk of IS.
The composite genetic risk score consisting of the 47 SNPs associated with HDL-C explained 6% of the HDL-C levels in our sample (p < 0.0001). This genetic score, however, was not associated with IS (HR/SD HDL-C −0.04, 95% CI −0.67 to 0.59, p = 0.92). Given our sample size, the magnitude of the genetic score effect size on IS has to be 1.05 or larger to be detected with power >80% (details of power calculation are presented in appendix e-2.). The expected genetic score effect on IS −0.402 given HDL is causal, i.e., the effect size of genetic score on HDL-C multiply the per-SD effect of HDL-C on IS, and is much smaller than the required (1.0) for adequate power. Therefore, we cannot rule out the possibility of lack of power as a reason for the negative mendelian randomization findings for HDL-C.
TG and LDL-C and ischemic events.
In a subset of 2,829 participants with TG and LDL-C measurements available, we observed 69 IS and 54 ABI events (and 103 MI events in the MI sample of 2,695). The previously observed association between low HDL-C and high TC/HDL ratio and risk of IS, ABI, and MI events was unchanged (not shown). In model 1, we also observed that high TG levels (continuous and categorical) were associated with incident IS, ABI, and MI, while high LDL-C (categorical) was associated with increased risk of MI (not shown). However, in model 2 (table 4), the association with incident IS and ABI was diminished, while high logTG and LDL-C levels of ≥160 mg/dL were still associated with increased risk of MI (p < 0.001 and p < 0.05, respectively).
Table 4.
Effect of TG and LDL-C on 10-year stroke and MI incidence

We observed significant interaction between sex and LDL-C. In women only (table e-3a), high LDL-C was associated with increased risk of IS and ABI (for IS: HR/SD increase in LDL-C: 1.44 [1.03–2.01], p < 0.05; for LDL-C ≥160 mg/dL: 2.48 [1.09–5.67], p < 0.05). There were no significant interactions with TG.
In age-specific analysis using model 2, no association with incident IS or ABI was found. There were no participants on statins at baseline in any of the 3 examinations (15, 20, and 4), but there was interim use of statin in the examination 20 and examination 4 follow-up periods. Excluding participants on statins (n = 272) did not affect our results (not shown).
DISCUSSION
In the FHS, we related lipid/lipoprotein biomarkers to risk of ischemic vascular events (IS, ABI, and MI). In pooled analysis adjusted for stroke risk factors, using continuous and/or categorical measures of lipid/lipoprotein markers, low HDL-C and high TC/HDL-C ratio were associated with increased risk of ischemic stroke (IS, ABI, and cardioembolic); all lipids/lipoproteins assessed were associated with risk of MI. An inverse association between HDL-C and risk of IS was evident for both women and men, across both age groups; the effect was significantly stronger in participants younger than 65 years. High TC increased risk of IS in women. More important, HDL-C ≤40 mg/dL as a marker of stroke risk was shown to improve the risk stratification model beyond existing risk factors within FSRP. Higher LDL-C levels increased risk of IS and ABI in women. The association between lipids/lipoproteins and risk of MI in women and men in all age groups was consistent with previously published data.1–3
This report not only confirms previous findings, but also extends these findings to all age categories and both sex groups, while presenting results for both continuous and categorical lipid measures, and for IS and MI within the same population.
The association between various lipids/lipoproteins and IS has been examined in several prospective studies that varied in sample size, study design, methods, endpoint measures, lipid levels, and/or cutoff values. Overall, it has become increasingly clear that lipid biomarkers are related to IS.4–14
Our findings that low HDL-C levels are associated with higher risk of IS for women and men across all age groups concur with recent reports. A large prospective study from Finland observed such an association in women,8 and the Cardiovascular Health Study found a similar association in men.12 An earlier report based on FHS data with fewer stroke events noted a weak association between HDL-C and stroke.9
While the mechanisms by which HDL-C is protective against IS are complex, HDL-C is a strong antiatherogenic lipid molecule with potent anti-inflammatory properties more protective for atherosclerotic stroke subtypes.6 The few studies differentiating between IS subtypes also observed similar relationships.4,5,15,16 Our findings confirm that HDL-C is a significant biological risk factor for IS among middle-aged and elderly persons. After adjusting for conventional risk factors, however, this association remained statistically significant only for men, although the strength of the association appeared similar in men and women. It is worth noting that in our study, only 18% of women and close to 50% of men had HDL-C levels of <40 mg/dL, while the median HDL-C levels were higher in women than in men (54 vs 43 mg/dL, respectively), which is consistent with prior findings that, compared with men, HDL-C levels are higher in women before menopause.31 Thus, we suspect that the smaller sample size of women with low HDL-C and the small numbers of events in women reduced our power to detect effects in women. The stronger association of low HDL with IS risk in persons younger than 65 years compared with those 65 years and older is consistent with the general observation that multiple risk factors act together to determine risk in older persons, hence the impact of any one individual risk or protective factor is attenuated.
Nevertheless, given the relatively consistent inverse association between HDL-C and IS, the potential utility of raising HDL-C in reducing stroke risk has been suggested in recent literature. However, more clinical data are needed to support modification of primary stroke prevention gudielines.15
The absence of a significant association between the genetic HDL score and risk of IS, although possibly attributable to lack of power, is consistent with recent studies evaluating the causal relevance of HDL-C concentrations for risk of ischemic CVD.32
TC/HDL-C ratio has been shown to be a more potent predictor of CVD incidence than TC, LDL-C, or HDL-C alone.23,33 While some studies support an association between high TC and IS,5,7,8 and others do not,11,34 only a few studies examined the effect of TC/HDL-C ratio on risk of IS.8 We found a positive association between high TC/HDL-C ratio and IS while further extending these findings to specifically atherothrombotic stroke subtypes.
TC/HDL-C, a ratio between atherogenic and antiatherogenic lipid molecules, is a well-established representation of their joint contribution to CVD risk stratification.23,33 Therefore, its further role in risk stratification of IS risk could be of particular importance.
An overall association between TC and IS was not significant. There was a positive trend also seen in prior studies. Of note, in sex-specific and in fully adjusted analyses, high TC was weakly predictive of IS in women. In the Women's Health Study (WHS), which included 27,937 US women aged 45 years or older, higher TC was associated with increased risk of IS.7 However, the Atherosclerosis Risk in Communities Study11 and the EUROSTROKE Project34 did not find an association between TC levels and IS in either women or men.
Relating fasting TG levels to IS incidence, including in our prior reports, did not show consistent results.9,11 However, more recent findings from the Copenhagen City Heart Study14 and the WHS31 showed that nonfasting, elevated TG levels are related to IS.
LDL-C, which is highly correlated with TC concentration, is strongly and positively associated with coronary heart disease risk,3,9 but less consistently with IS.7,10 We observed no significant association between LDL-C and IS after adjusting for conventional risk factors, similar to our results with TC levels. There was, however, an overall trend between elevated LDL-C and ischemic stroke (IS and ABI) in women as shown in prior reports from the WHS.7
Our study has several important strengths. The sample comprises prospectively followed community-based cohorts of middle-aged and elderly persons, free of stroke at baseline, with minimal loss to follow-up. Analyses were adjusted for putative risk factors and for interim MI events. Ascertainment of vascular events was rigorous with minimal ascertainment bias. Because the majority of FHS participants are white, the generalizability to other racial groups is limited. We have fasting TG levels, whereas contemporary literature is focused on nonfasting TG levels.
We demonstrated the expected association in this dataset of various lipid subfractions with incident MI, thus confirming that the observed associations (or lack of association) of lipid measures with stroke are unlikely to be attributable to any biases in sample selection.
We examined the associations between a wide range of plasma lipid/lipoprotein biomarkers and incident CVD events (IS and MI). Contrary to other reports relating various lipid fractions to incident stroke, in this prospective study spanning the adult age span and including more than 300 systematically adjudicated stroke events, we found only lower HDL-C levels and higher TC/HDL-C ratio to be related in a strong, consistent, and statistically significant relationship to IS in men and women. These relationships persisted after adjustment for pertinent risk factors, suggesting an independent contribution to IS risk. In addition, HDL-C ≤40 mg/dL improved the risk stratification model with a powerful and independent effect. The lack of a consistent association between other lipids/lipoproteins and ischemic stroke (specifically ABI) suggests that not all lipid measures may be of equal clinical importance in stroke risk prediction and primary prevention, although LDL-C and TC levels remain relevant to the risk of MI and death.
Further studies should confirm whether raising HDL-C levels or changing TC/HDL-C ratio by lifestyle modification or pharmacologic therapies may influence the risk of IS. However, in clinical practice aimed at IS prevention, we should recognize that HDL-C may be the optimal marker to improve risk stratification.
Supplementary Material
GLOSSARY
- ABI
atherothrombotic brain infarct
- CI
confidence interval
- CVD
cardiovascular disease
- FHS
Framingham Heart Study
- FSRP
Framingham Stroke Risk Profile
- HDL-C
high-density lipoprotein cholesterol
- HR
hazard ratio
- IS
ischemic stroke
- LDL-C
low-density lipoprotein cholesterol
- MI
myocardial infarction
- SNP
single nucleotide polymorphism
- TC
total cholesterol
- TG
triglycerides
- WHS
Women's Health Study
Footnotes
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
Drs. Beiser, Seshadri, and Wolf had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Pikula, Beiser, Yang, Seshadri, Wolf. Acquisition of data: Pikula, Beiser, Seshadri, Wolf. Analysis and interpretation of data: Pikula, Beiser, Wang, Yang, Seshadri, Wolf. Drafting of the manuscript: Pikula, Beiser, Seshadri, Wolf. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: Beiser, Himali, Wang, Yang. Obtained funding: Wolf, Seshadri. Study supervision: Beiser, Seshadri, Wolf.
STUDY FUNDING
This work was supported by the NIH/National Heart, Lung, and Blood Institute (NHLBI) contract N01-HC-25195 and the National Institute of Neurological Disorders and Stroke (NINDS) (R01 NS17950). The content is solely the responsibility of the authors and does not necessarily represent the official views of NHLBI or NIH/NINDS.
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Stampfer MJ, Sacks FM, Salvini S, Willett WC, Hennekens CH. A prospective study of cholesterol, apolipoproteins, and the risk of myocardial infarction. N Engl J Med 1991;325:373–381. [DOI] [PubMed] [Google Scholar]
- 2.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation 1998;97:1837–1847. [DOI] [PubMed] [Google Scholar]
- 3.Sharrett AR, Ballantyne CM, Coady SA, et al. Coronary heart disease prediction from lipoprotein cholesterol levels, triglycerides, lipoprotein(a), apolipoproteins A-I and B, and HDL density subfractions: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation 2001;104:1108–1113. [DOI] [PubMed] [Google Scholar]
- 4.Sacco RL, Benson RT, Kargman DE, et al. High-density lipoprotein cholesterol and ischemic stroke in the elderly: the Northern Manhattan Stroke Study. JAMA 2001;285:2729–2735. [DOI] [PubMed] [Google Scholar]
- 5.Tirschwell DL, Smith NL, Heckbert SR, Lemaitre RN, Longstreth WT, Jr, Psaty BM. Association of cholesterol with stroke risk varies in stroke subtypes and patient subgroups. Neurology 2004;63:1868–1875. [DOI] [PubMed] [Google Scholar]
- 6.Amarenco P, Labreuche J, Touboul PJ. High-density lipoprotein-cholesterol and risk of stroke and carotid atherosclerosis: a systematic review. Atherosclerosis 2008;196:489–496. [DOI] [PubMed] [Google Scholar]
- 7.Kurth T, Everett BM, Buring JE, Kase CS, Ridker PM, Gaziano JM. Lipid levels and the risk of ischemic stroke in women. Neurology 2007;68:556–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang Y, Tuomilehto J, Jousilahti P, Wang Y, Antikainen R, Hu G. Total and high-density lipoprotein cholesterol and stroke risk. Stroke 2012;43:1768–1774. [DOI] [PubMed] [Google Scholar]
- 9.Gordon T, Kannel WB, Castelli WP, Dawber TR. Lipoproteins, cardiovascular disease, and death: the Framingham Study. Arch Intern Med 1981;141:1128–1131. [PubMed] [Google Scholar]
- 10.Willey JZ, Xu Q, Boden-Albala B, et al. Lipid profile components and risk of ischemic stroke: the Northern Manhattan Study (NOMAS). Arch Neurol 2009;66:1400–1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shahar E, Chambless LE, Rosamond WD, et al. Plasma lipid profile and incident ischemic stroke: the Atherosclerosis Risk in Communities (ARIC) Study. Stroke 2003;34:623–631. [DOI] [PubMed] [Google Scholar]
- 12.Psaty BM, Anderson M, Kronmal RA, et al. The association between lipid levels and the risks of incident myocardial infarction, stroke, and total mortality: the Cardiovascular Health Study. J Am Geriatr Soc 2004;52:1639–1647. [DOI] [PubMed] [Google Scholar]
- 13.Brewer HB., Jr Increasing HDL cholesterol levels. N Engl J Med 2004;350:1491–1494. [DOI] [PubMed] [Google Scholar]
- 14.Freiberg JJ, Tybjaerg-Hansen A, Jensen JS, Nordestgaard BG. Nonfasting triglycerides and risk of ischemic stroke in the general population. JAMA 2008;300:2142–2152. [DOI] [PubMed] [Google Scholar]
- 15.Kim SJ, Park YG, Kim JH, Han YK, Cho HK, Bang OY. Plasma fasting and nonfasting triglycerides and high-density lipoprotein cholesterol in atherosclerotic stroke: different profiles according to low-density lipoprotein cholesterol. Atherosclerosis 2012;223:463–467. [DOI] [PubMed] [Google Scholar]
- 16.Laloux P, Galanti L, Jamart J. Lipids in ischemic stroke subtypes. Acta Neurol Belg 2004;104:13–19. [PubMed] [Google Scholar]
- 17.Amarenco P, Goldstein LB, Szarek M, et al. Effects of intense low-density lipoprotein cholesterol reduction in patients with stroke or transient ischemic attack: the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial. Stroke 2007;38:3198–3204. [DOI] [PubMed] [Google Scholar]
- 18.Dawber TR, Meadors GF, Moore FE., Jr Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health Nations Health 1951;41:279–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families: the Framingham Offspring Study. Am J Epidemiol 1979;110:281–290. [DOI] [PubMed] [Google Scholar]
- 20.McNamara JR, Schaefer EJ. Automated enzymatic standardized lipid analyses for plasma and lipoprotein fractions. Clin Chim Acta 1987;166:1–8. [DOI] [PubMed] [Google Scholar]
- 21.Warnick GR, Benderson J, Albers JJ. Dextran sulfate-Mg2+ precipitation procedure for quantitation of high-density-lipoprotein cholesterol. Clin Chem 1982;28:1379–1388. [PubMed] [Google Scholar]
- 22.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972;18:499–502. [PubMed] [Google Scholar]
- 23.Castelli WP, Anderson K, Wilson PW, Levy D. Lipids and risk of coronary heart disease: the Framingham Study. Ann Epidemiol 1992;2:23–28. [DOI] [PubMed] [Google Scholar]
- 24.Wang TJ, Gona P, Larson MG, et al. Multiple biomarkers for the prediction of first major cardiovascular events and death. N Engl J Med 2006;355:2631–2639. [DOI] [PubMed] [Google Scholar]
- 25.Wolf PA, D'Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke 1991;22:312–318. [DOI] [PubMed] [Google Scholar]
- 26.Grundy SM. Obesity, metabolic syndrome, and cardiovascular disease. J Clin Endocrinol Metab 2004;89:2595–2600. [DOI] [PubMed] [Google Scholar]
- 27.Seshadri S, Fitzpatrick AL, Ikram MA, et al. Genome-wide analysis of genetic loci associated with Alzheimer disease. JAMA 2010;303:1832–1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kathiresan S, Willer CJ, Peloso GM, et al. Common variants at 30 loci contribute to polygenic dyslipidemia. Nat Genet 2009;41:56–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143–3421. [PubMed] [Google Scholar]
- 30.Pencina MJ, D'Agostino RB, Sr, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med 2011;30:11–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berger JS, McGinn AP, Howard BV, et al. Lipid and lipoprotein biomarkers and the risk of ischemic stroke in postmenopausal women. Stroke 2012;43:958–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kathiresan S, Melander O, Anevski D, et al. Polymorphisms associated with cholesterol and risk of cardiovascular events. N Engl J Med 2008;358:1240–1249. [DOI] [PubMed] [Google Scholar]
- 33.da Luz PL, Cesena FH, Favarato D, Cerqueira ES. Comparison of serum lipid values in patients with coronary artery disease at <50, 50 to 59, 60 to 69, and >70 years of age. Am J Cardiol 2005;96:1640–1643. [DOI] [PubMed] [Google Scholar]
- 34.Cholesterol, diastolic blood pressure, and stroke: 13,000 strokes in 450,000 people in 45 prospective cohorts. Prospective Studies Collaboration. Lancet 1995;346:1647–1653. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


