Abstract
Objectives:
In the current study, we aim to assess potential neurologist-related barriers to epilepsy surgery among Canadian neurologists.
Methods:
A 29-item, pilot-tested questionnaire was mailed to all neurologists registered to practice in Canada. Survey items included the following: (1) type of medical practice, (2) perceptions of surgical risks and benefits, (3) knowledge of existing practice guidelines, and (4) barriers to surgery for patients with epilepsy. Neurologists who did not complete the questionnaire after the initial mailing were contacted a second time by e-mail, fax, or telephone. After this reminder, the survey was mailed a second time to any remaining nonresponders.
Results:
In total, 425 of 796 neurologists returned the questionnaire (response rate 53.5%). Respondents included 327 neurologists who followed patients with epilepsy in their practice. More than half (56.6%) of neurologists required patients to be drug-resistant and to have at least one seizure per year before considering surgery, and nearly half (48.6%) failed to correctly define drug-resistant epilepsy. More than 75% of neurologists identified inadequate health care resources as the greatest barrier to surgery for patients with epilepsy.
Conclusions:
A substantial proportion of Canadian neurologists are unaware of recommended standards of practice for epilepsy surgery. Access also appears to be a significant barrier to epilepsy surgery and surgical evaluation. As a result, we are concerned that patients with epilepsy are receiving inadequate care. A greater emphasis must be placed on knowledge dissemination and ensuring that the infrastructure and personnel are in place to allow patients to have timely access to this evidence-based treatment.
At least one-third of people with epilepsy are drug-resistant after 2 adequate trials of antiseizure medications.1 Drug-resistant epilepsy accounts for 75% of the cost of epilepsy2 and is associated with an increased risk of mortality,3 cognitive decline,4 and reduced quality of life.5
Two randomized controlled trials6,7 and numerous observational studies8 have demonstrated that epilepsy surgery is superior to medical management in temporal lobe epilepsy, and that early surgery is highly successful. Epilepsy surgery is cost-effective9 and associated with improved social outcomes such as employment.10 Even complex patients deemed ineligible for focal resection often receive significant benefit from palliative surgical procedures such as vagus nerve stimulation, corpus callosotomy, or deep brain stimulation.11
Epilepsy surgery remains underutilized,12 and patients average nearly 20 years before being referred for a surgical evaluation.13 Neurologists are often reluctant to consider epilepsy surgery in the early stages of disease,14 have difficulties defining drug-resistant epilepsy,14 may not be informed about the risks and benefits of epilepsy surgery, and may be poorly equipped to identify patients who are potential surgical candidates.15
To date, no studies have been published examining the knowledge and perceptions of epilepsy surgery in Canadian neurologists, and studies conducted in Europe and the United States have either not been comprehensive or had low response rates.14,16,17 In the current study, we aimed to assess potential neurologist-related barriers to epilepsy surgery among Canadian neurologists nationwide.
METHODS
Questionnaire development.
A literature review was conducted before designing the questionnaire. Important questions and topics from the literature were either modified or directly included as items in our questionnaire (appendix e-1 on the Neurology® Web site at Neurology.org). The 29-item questionnaire was developed by a team composed of epileptologists, an epilepsy fellow, and research assistants. Survey items included the following: (1) medical practice characteristics, (2) perceptions of surgical risks and benefits, (3) knowledge of existing practice guidelines, and (4) barriers to epilepsy surgery. The initial questionnaire was piloted in a sample of 10 neurologists across the country to assess face validity and clarity. The time needed to complete the questionnaire was recorded and all pilot study participants provided written feedback. The 5-minute questionnaire was modified based on the pilot study results. A screening question at the beginning of the questionnaire ensured that only physicians currently treating patients with epilepsy completed the survey.
Standard protocol approvals, registrations, and patient consents.
The study was approved by the Conjoint Health Research Ethics Board at the University of Calgary.
Initial mailing.
Contact information for the 852 neurologists registered to practice in Canada was obtained from the Canadian Medical Directory. Neurologists were excluded from the study if correct contact information could not be obtained, they participated in the pilot study or were investigators in the study, were retired from medical practice, were currently practicing outside of Canada or on sabbatical/maternity leave, or were deceased. Neurologists were first contacted by mail and given 3 weeks to return the questionnaire in a prestamped envelope. No incentives were offered in return for completion of the questionnaire.
First and second reminder.
Neurologists who did not complete the questionnaire after the initial mailing were contacted a second time by e-mail, fax, or telephone. Neurologists who had not completed the questionnaire after the first 2 contacts were sent a second and final copy of the questionnaire by mail along with a prestamped envelope.
Data analysis.
Descriptive statistics were used to characterize the study participants. Differences between responders and nonresponders were assessed using χ2 and t tests. Province of practice was not examined because of small sample sizes for some provinces.
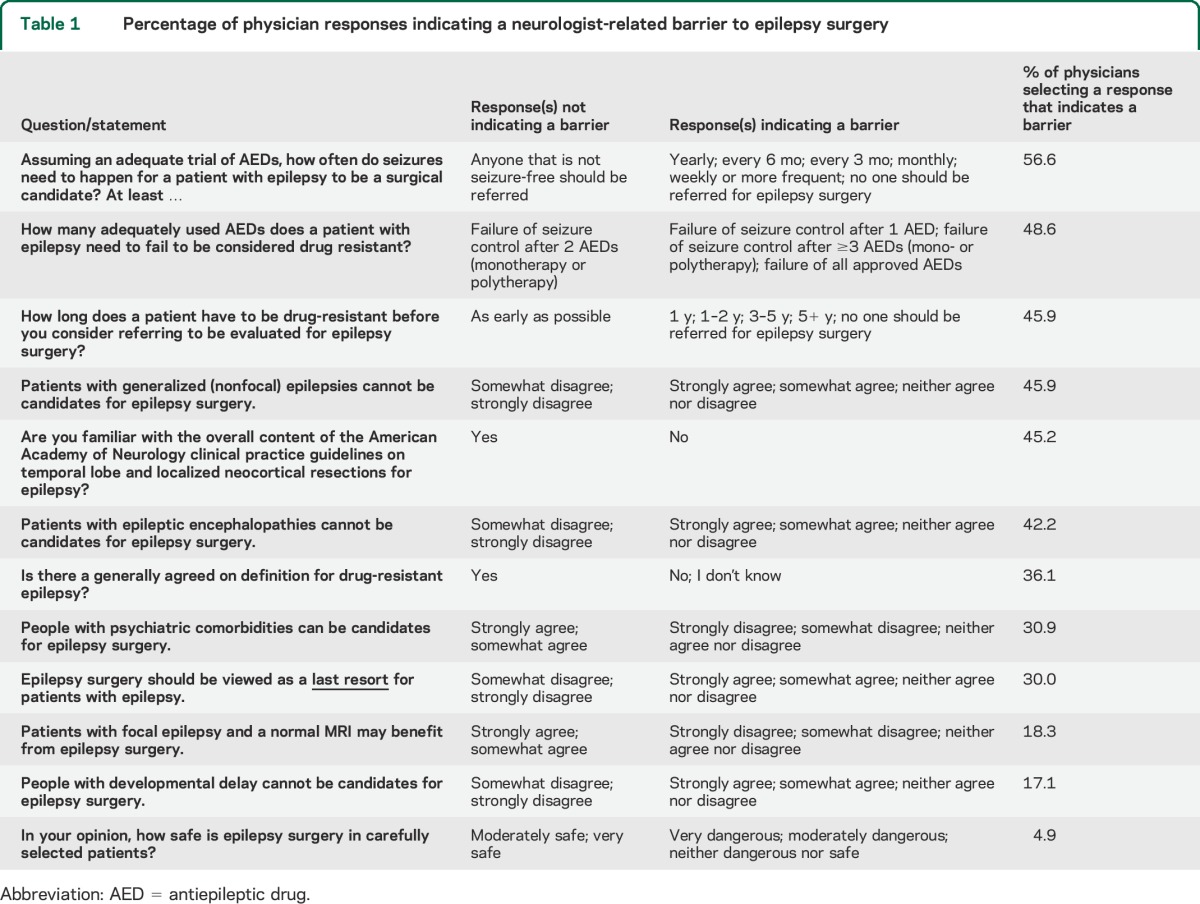
To assess how neurologists' characteristics were associated with knowledge and attitudes toward epilepsy surgery, a composite measure was generated. The purpose of this measure was to incorporate all variables that evaluated knowledge of and attitudes toward epilepsy surgery into a single variable in order to facilitate the analysis. Responses to each of 12 questions representing “neurologist-related barriers to epilepsy surgery” (see table 1) were linearly transformed. Scores for each question were added to create a composite score ranging from 0 to 100, where a neurologist who did not demonstrate a barrier for any of the items would receive a score of 100, and a neurologist who demonstrated barriers on all items would receive a score of zero.
Table 1.
Percentage of physician responses indicating a neurologist-related barrier to epilepsy surgery
To examine the relationship of time in practice to neurologist-related barriers, the date of graduation from medical school was dichotomized into “graduated in 2000 or later” and “graduated before 2000.” The year 2000 was selected based on the median year of graduation of the participants and to reflect that neurologists graduating in 2000 or later would have had access to the first epilepsy surgery randomized clinical trial7 and related clinical practice guidelines18 during their residency training. To examine how neurologist referral patterns relate to barriers, responses to the question, “How many patients have you referred for epilepsy surgery in the last year?” were dichotomized into “0–2 patients” and “3 or more patients.” These cutpoints were determined based on the median number of referrals in the survey. The relationship between the proportion of patients referred for surgical evaluation and neurologist-related barriers could not be examined because variables required to calculate the proportion were categorical. Instead, the association between the number of patients with epilepsy seen and the number of patients referred for an epilepsy surgical evaluation within the past year was examined using a χ2 test.
The relationship of each variable to the composite score was first explored through individual t tests, and then all variables found to be statistically significant at an α level of 0.05 were included in a linear regression model with the composite score as an outcome measure.
For the open-ended question asking physicians to identify the “one biggest barrier your epilepsy patients face in accessing epilepsy surgery,” traditional qualitative analysis was utilized. Responses were read to identify themes and categories, and related themes were then grouped together as branches under a larger unifying theme.
RESULTS
Physician participation.
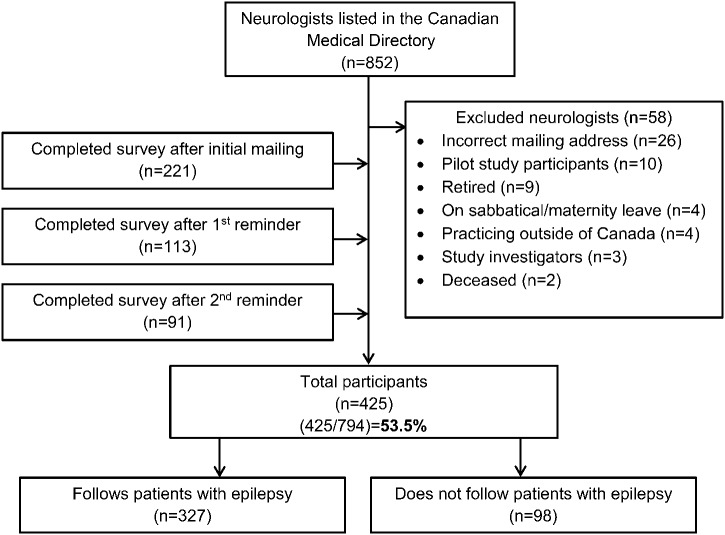
In total, 425 of 796 eligible neurologists (53.5%) returned the questionnaire (figure). Responders differed significantly from nonresponders on several characteristics. Nonresponders were more likely to practice in the provinces of Saskatchewan or Quebec (p < 0.001), to prefer communicating in French (p < 0.001), and to have graduated from medical school before 1985 (p < 0.05).
Figure. Study flow diagram.
Characteristics of participating physicians.
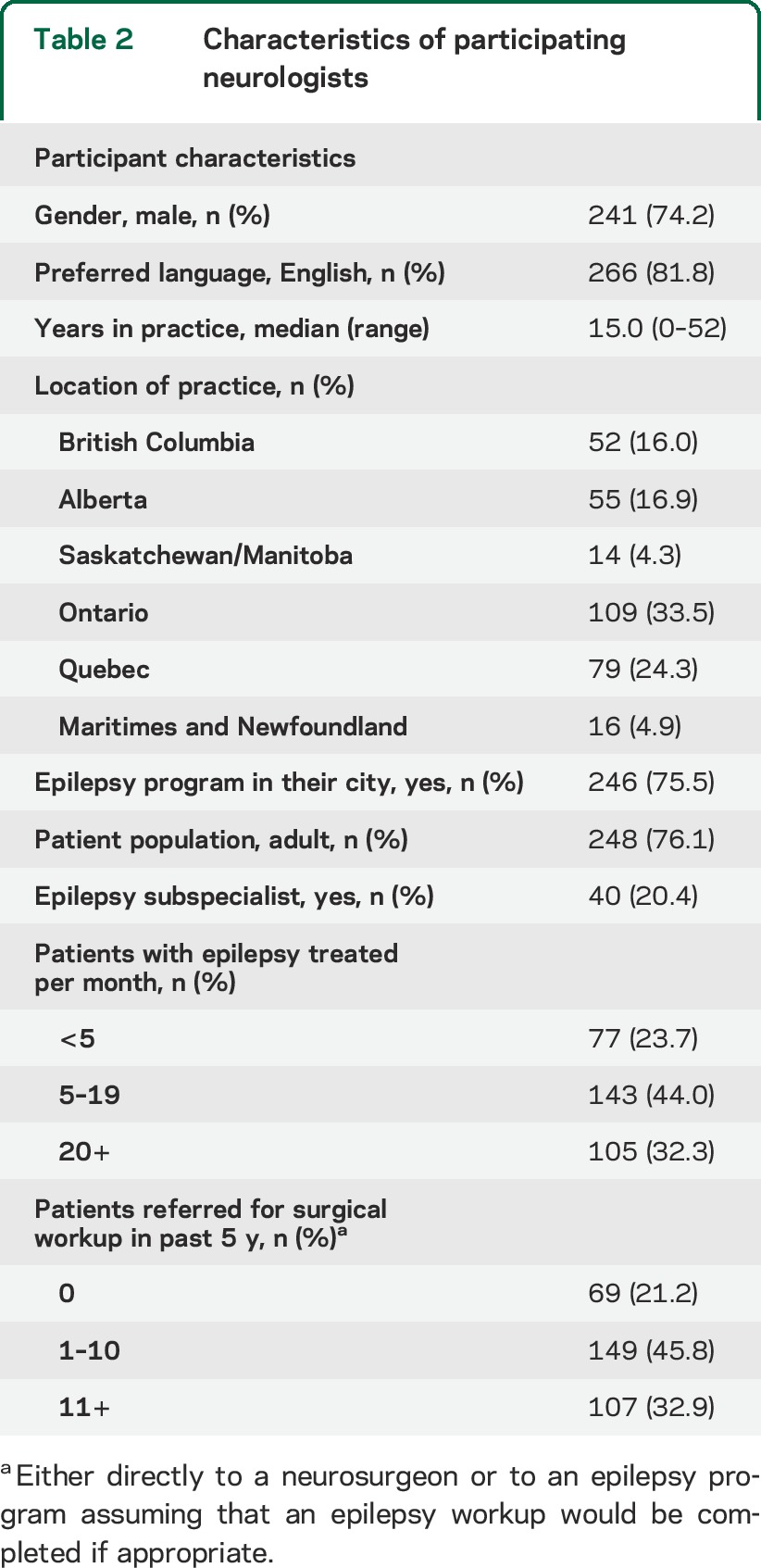
Of all participating neurologists, 327 (76.9%) followed patients with epilepsy in their practice and were asked to complete the questionnaire in full. Characteristics of participating neurologists are reported in table 2. There was a significant association between the number of patients with epilepsy seen in a neurologist's practice and the number of patients they referred for a surgical evaluation; 67.6% of neurologists who saw more than 20 patients with epilepsy per year reported referring 3 or more patients for a surgical evaluation within the past year, in comparison to 23.2% of neurologists who saw fewer than 20 patients with epilepsy per year.
Table 2.
Characteristics of participating neurologists
Neurologist-related barriers to epilepsy surgery.
Almost 90% of neurologists reported that they were quite knowledgeable about the indications for epilepsy surgery. Table 1 lists the questions that were included in the derivation of a composite score to assess neurologist-related barriers to epilepsy surgery. The question that was least indicative of a neurologist-related barrier was “In your opinion, how safe is epilepsy surgery in carefully selected patients?”—less than 5% of neurologists indicated that they believed epilepsy surgery was dangerous or neither dangerous nor safe. The questions that were most indicative of neurologist-related barriers included the following: requiring a minimum seizure frequency (i.e., experiencing a seizure at least yearly) for a patient to be a surgical candidate (56.6%); lack of recognition that a patient who fails 2 drugs is considered drug-resistant (48.6%); failure to identify that drug-resistant patients should be considered for a surgical evaluation regardless of epilepsy duration (45.9%); and stating that patients with generalized epilepsies cannot be candidates for epilepsy surgery (45.9%). The resulting median composite score was 66.7, indicating that 8 of 12 questions were answered appropriately (e.g., in a way that did not indicate a neurologist-related barrier).
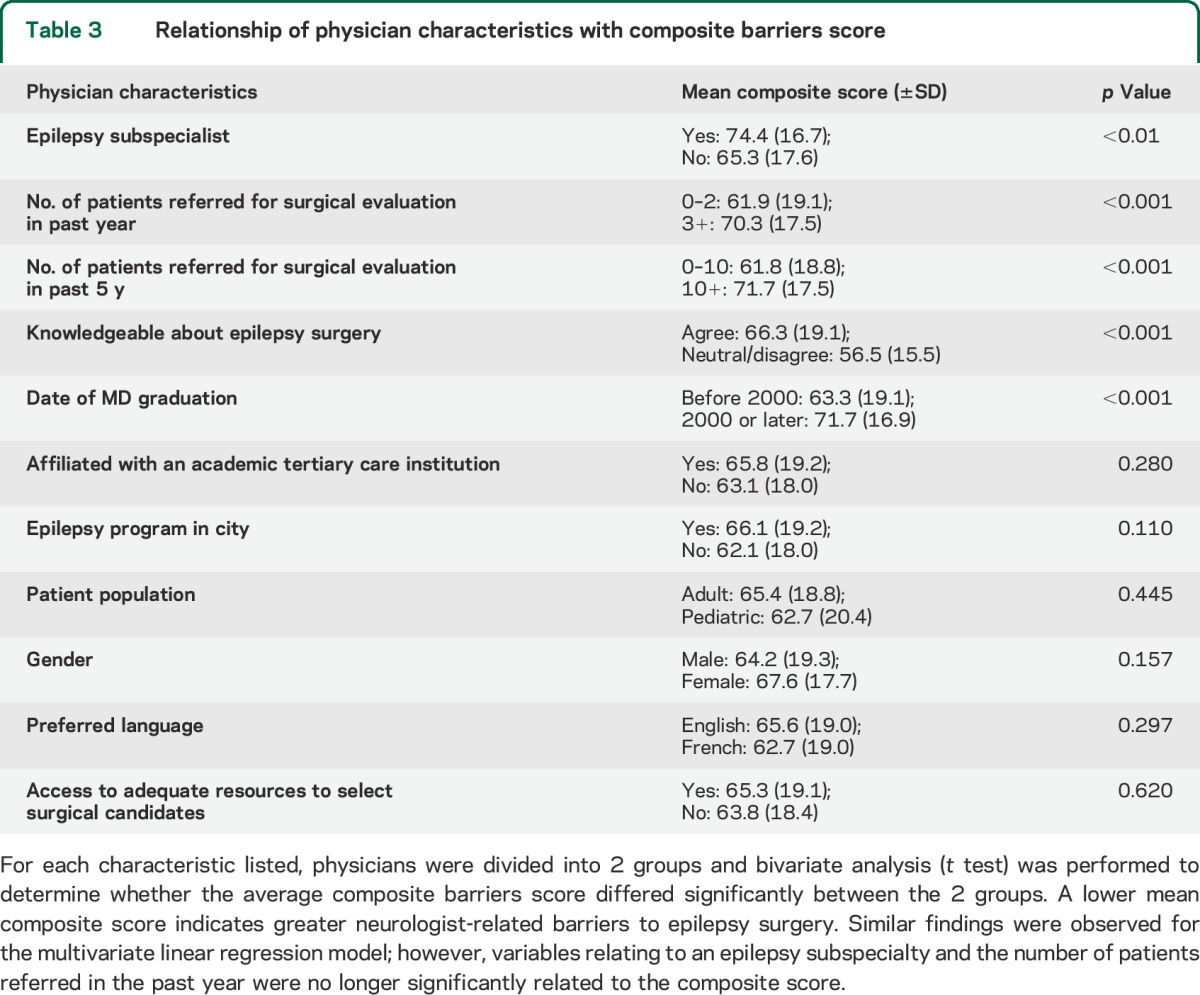
Relationship between neurologist characteristics and composite barriers score.
Bivariate analyses of differences in the composite barriers scores revealed significant differences by neurologists' characteristics (table 3). Neurologists who believed that they were knowledgeable about epilepsy surgery, were epilepsy subspecialists, had referred a greater number of patients for epilepsy surgery or a surgical evaluation in the past year or past 5 years, and those who had graduated from medical school after the year 2000 all had significantly lower neurologist-related barriers to epilepsy surgery (table 3). Similar findings were observed for the multivariate linear regression model; however, variables relating to an epilepsy subspecialty and the number of patients referred in the past year were no longer significantly related to the composite score.
Table 3.
Relationship of physician characteristics with composite barriers score
Resource barriers to epilepsy surgery.
Although 86.5% of those surveyed reported they had access to adequate expertise, technology, and resources to allow for appropriate selection of epilepsy surgical candidates, the majority reported concerns about temporal and physical barriers to access; 36.5% of neurologists estimated the waitlists for surgical evaluation at their site to be 1 year or longer, with the average wait time for an epilepsy surgical evaluation of 8.6 months. The longest waiting times were reported by neurologists from the provinces of Saskatchewan (14.2 months) and British Columbia (10.2 months), whereas neurologists from Quebec and Alberta had the shortest estimated wait times (5.9 and 7.9 months, respectively). There was a nonsignificant trend among neurologists who referred fewer patients for surgical evaluation to estimate longer waiting times. More than 40% (41.2%) of neurologists who had referred 2 or fewer patients for a surgical referral within the past year estimated the wait time for a surgical evaluation to exceed 1 year, in comparison to 29.8% of neurologists who had referred 3 or more patients within the past year (p = 0.06).
When neurologists were asked open-endedly to identify the single largest barrier to epilepsy surgery, more than 75% of identified barriers were related to inadequate health care resources, including the following: long wait times (34.4%), limited resources (13.7%), access (11.3%), distance (7.0%), availability (6.3%), and delays (3.5%). Other themes that were not related to access included the following: apprehension of surgery by patient or guardian (10.5%), delayed referral (9.0%), lack of knowledge about epilepsy surgery by physician or patient (2.3%), and poor candidacy for epilepsy surgery (2.0%). A full breakdown of neurologist responses is available in appendix e-2.
DISCUSSION
This study represents a nationwide exploration of neurologists' knowledge of and attitudes toward epilepsy surgery. Our response rate of more than 50% is very good in terms of the usual response rates achieved in physician surveys, particularly among specialists.19 Among recent studies surveying neurologists' knowledge and perceptions about epilepsy care or epilepsy surgery, the response rates ranged between 14% and 20% with mailed surveys.14,17
Overall, this study demonstrates that neurologists have substantial knowledge gaps regarding indications for epilepsy surgery. Only 43.4% of neurologists appropriately answered that anyone with ongoing seizures should be referred, and only 51.4% correctly identified that a patient only needs to fail 2 drugs to be considered drug-resistant. In addition, only 54.1% recognized the need to refer a patient as soon as they meet the definition of drug-resistant epilepsy. Although this is of grave concern, these findings are greatly improved in comparison to a recent survey of neurologists practicing in Michigan where only 3% of neurologists would refer a patient with yearly seizures.14 In a separate study of Swedish neurologists, 68.1% of physicians responded that a high seizure frequency (>1/month) was “very important” in regard to eligibility for an epilepsy surgery assessment.20 Recently, only 18% of Swedish20 and 14% of Michigan (United States)14 neurologists correctly identified that epilepsy surgery should be considered once 2 drugs have failed.21 Despite the fact that our estimates are somewhat more promising than previous studies, it is clear that a substantial proportion of neurologists are not aware of recommended standards of practice for epilepsy surgery and drug-resistant epilepsy. As a result, we are concerned that epilepsy patients are not receiving adequate care.
More than 75% of neurologists in this study consider inadequate health care resources to be the single greatest barrier to epilepsy surgery. There were substantial regional differences in approximate wait times for surgical evaluation, which may in part be explained by the fact that the management of health care in Canada is under provincial jurisdiction. Although barriers stemming from resource limitations may be unique to Canada and other publicly funded health care systems, it is probable that access to specialist epilepsy care is a substantial barrier for people with epilepsy in all health care systems. Even in mostly privatized systems such as the United States, only 52.8% of US adults with active epilepsy report seeing a neurologist within the past year,22 with an even lower proportion (27%) reported for California.23 Furthermore, uninsured individuals with epilepsy living in the United States have fewer outpatient visits and visits with neurologists,24 and more than one-third of individuals with active epilepsy living in South Carolina report not being able to see a doctor because of cost.25 Considerable disparities in epilepsy medical and surgical care have been reported in both privately and government-funded health care systems,26 with individuals living in rural locations having a significantly elevated risk of untreated epilepsy.27 Although wait times for epilepsy surgery are rarely reported in the literature, one study in publicly funded Central and East European countries found that only 7 of 10 countries had epilepsy surgery centers and the wait time for epilepsy surgery ranged from 2 weeks to 3 years.28 While the initial costs of presurgical evaluation and surgery are significant, studies have demonstrated that epilepsy surgery is a cost-effective procedure.29–31
We found that being an epilepsy specialist, having referred more patients for a surgical evaluation, having better self-reported knowledge, and graduating from medical school more recently were significantly associated with reduced neurologist-related barriers to epilepsy surgery. While a previous study of neurologist-related barriers to epilepsy surgery did not report an association between attitudes toward epilepsy surgery and years in practice,16 it is possible that recent graduates are more familiar with the literature whereas neurologists who have been in practice longer are less likely to keep up with the latest evidence, particularly if epilepsy is not their main specialty.
Some limitations in our study must be acknowledged. Despite obtaining a strong response rate, it is possible that nonresponse may have introduced selection bias into our study. It may be the case that differences between responders and nonresponders are indicative of barriers to surgical implementation. We found that nonresponders were more likely to prefer communicating in French, and unfortunately, we did not offer the survey in French despite Canada being a bilingual country. Because we did not find language preference to be related to neurologist-related barriers to epilepsy surgery, our results are unlikely to have been affected by this factor. Nonetheless, it may be worthwhile to consider language of the neurologist as a possible barrier to guideline uptake, particularly because the existing guidelines are only available in English. There was a lower response rate among neurologists who graduated from medical school before 2000. This is concerning because earlier date of graduation was found to be significantly related to neurologist-related barriers to epilepsy surgery. In contrast, there was a lower response rate in physicians who graduated from medical school before 2000, which is concerning because this variable was found to be significantly related to neurologist-related to epilepsy surgery. It is therefore possible that neurologist-related barriers to epilepsy surgery in Canada may be underestimated. The association between the province of practice and barriers to epilepsy surgery was not examined because of small sample sizes for some provinces. Future studies are warranted to explore whether the low response in certain regions could be a reflection of needed infrastructure support in these areas vs poor guideline implementation. Furthermore, we determined which epilepsy surgery topics have the largest knowledge gaps by calculating the percentage of neurologists who answered the question in a way that would indicate a barrier to quality epilepsy care (table 1). Because questions had response options ranging from 2 to 7, it is possible that items with more response options were biased toward physicians selecting a barrier answer. As 2 questions with the highest number of response options are in the top 3 items showing large neurologist-derived barriers, this appears to be a plausible concern. It should also be emphasized that the waiting times reported here are rough approximations that have not been validated. It is probable that many neurologists may not have accurate information of the time delay to receive a surgical workup.
Although our survey has not been formally validated, it was developed by a team of epilepsy surgery and survey development experts, and then pilot tested in epilepsy specialists scattered across Canada. It thus seems reasonable to assume that these results are generalizable to Canadian neurologists as a whole. Whether these results are generalizable to other developed countries is uncertain. Although previous studies in Europe20 and the United States14 reported greater knowledge deficits and reservations toward epilepsy surgery, it is difficult to know how study design and response rates affected the findings.
Serious knowledge gaps about epilepsy surgery among neurologists were identified in this study. There is a need for ongoing physician education regarding the early diagnosis of drug resistance when patients fail 2 antiepileptic drugs, the dire consequences of continued uncontrolled seizures, and the proven efficacy, safety, and indications for epilepsy surgery, with an emphasis on determining which patients are drug-resistant. Even patients with only a single seizure per year can still be significantly affected, because they can be restricted from driving, have decreased quality of life, and may be unable to obtain gainful employment.32 Inadequate health care resources and access-related issues appear to be important barriers to timely access to epilepsy surgery. If future improvements in physician knowledge translate into an increasing number of patients referred for surgical evaluation and/or epilepsy surgery, it is crucial that the infrastructure and personnel are in place to allow patients to have timely access to this evidence-based treatment.
Supplementary Material
ACKNOWLEDGMENT
The authors thank all of the physicians who participated in the study. J.I. Roberts holds an Alberta Innovates Health Solutions (AIHS) Graduate Studentship. N. Jetté is the holder of an AIHS Population Investigator Award and a Canada Research Chair in Neurological Health Services Research. S. Wiebe holds the Hopewell Professorship of Clinical Neurological Research from the University of Calgary. K. Sauro holds an AIHS Graduate Studentship and a WRTC Graduate Scholarship.
Footnotes
Editorial, page 112
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
Jodie I. Roberts: design/conceptualization of the study, analysis and interpretation of the data, drafting and revising the manuscript for intellectual content. Chantelle Hrazdil: design/conceptualization of the study, interpretation of the data, revising the manuscript for intellectual content. Samuel Wiebe: design/conceptualization of the study, interpretation of the data, revising the manuscript for intellectual content. Khara Sauro: analysis and interpretation of the data, revising the manuscript for intellectual content. Michelle Vautour: design/conceptualization of the study, revising the manuscript for intellectual content. Natalie Wiebe: drafting and revising the manuscript for intellectual content. Nathalie Jetté: design/conceptualization of the study, interpretation of the data, revising the manuscript for intellectual content.
STUDY FUNDING
This study was funded in part by an Alberta Innovates Health Solutions research prize to Dr. Nathalie Jetté.
DISCLOSURE
J. Roberts has a graduate studentship from Alberta Innovates Health Solutions (AIHS). C. Hrazdil reports no disclosures. S. Wiebe serves on the editorial boards of Epileptic Disorders, Epilepsy & Behavior, and Canadian Journal of Neurological Sciences and receives research support from AIHS, Canadian Institutes of Health Research (CIHR), and University of Calgary (Hopewell Professorship of Clinical Neurosciences Research). K. Sauro has a graduate studentship from AIHS and a graduate studentship from a Western Regional Training Centre Graduate Scholarship. M. Vautour and N. Wiebe report no disclosures. N. Jetté is an associate editor of Epilepsia and is the recipient of an AIHS Population Health Investigator Award and a Canada Research Chair Tier 2 in Neurological Health Services Research. She has operating funds from CIHR, Alberta Health Services, and the University of Calgary Hotchkiss Brain Institute and Faculty of Medicine. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med 2000;342:314–319. [DOI] [PubMed] [Google Scholar]
- 2.Begley CE, Annegers JF, Lairson DR, Reynolds TF, Hauser WA. Cost of epilepsy in the United States: a model based on incidence and prognosis. Epilepsia 1994;35:1230–1243. [DOI] [PubMed] [Google Scholar]
- 3.Sillanpaa M, Jalava M, Kaleva O, Shinnar S. Long-term prognosis of seizures with onset in childhood. N Engl J Med 1998;338:1715–1722. [DOI] [PubMed] [Google Scholar]
- 4.Thompson PJ, Duncan JS. Cognitive decline in severe intractable epilepsy. Epilepsia 2005;46:1780–1787. [DOI] [PubMed] [Google Scholar]
- 5.Harden CL, Maroof DA, Nikolov B, et al. The effect of seizure severity on quality of life in epilepsy. Epilepsy Behav 2007;11:208–211. [DOI] [PubMed] [Google Scholar]
- 6.Engel J, Jr, McDermott MP, Wiebe S, et al. Early surgical therapy for drug-resistant temporal lobe epilepsy: a randomized trial. JAMA 2012;307:922–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wiebe S, Blume WT, Girvin JP, Eliasziw M. A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med 2001;345:311–318. [DOI] [PubMed] [Google Scholar]
- 8.Tellez-Zenteno JF, Dhar R, Wiebe S. Long-term seizure outcomes following epilepsy surgery: a systematic review and meta-analysis. Brain 2005;128:1188–1198. [DOI] [PubMed] [Google Scholar]
- 9.King JT, Jr, Sperling MR, Justice AC, O'Connor MJ. A cost-effectiveness analysis of anterior temporal lobectomy for intractable temporal lobe epilepsy. J Neurosurg 1997;87:20–28. [DOI] [PubMed] [Google Scholar]
- 10.Hamiwka L, Macrodimitris S, Tellez-Zenteno JF, et al. Social outcomes after temporal or extratemporal epilepsy surgery: a systematic review. Epilepsia 2011;52:870–879. [DOI] [PubMed] [Google Scholar]
- 11.Guerrini R, Scerrati M, Rubboli G, et al. Overview of presurgical assessment and surgical treatment of epilepsy from the Italian League Against Epilepsy. Epilepsia 2013;54(suppl 7):35–48. [DOI] [PubMed] [Google Scholar]
- 12.de Flon P, Kumlien E, Reuterwall C, Mattsson P. Empirical evidence of underutilization of referrals for epilepsy surgery evaluation. Eur J Neurol 2010;17:619–625. [DOI] [PubMed] [Google Scholar]
- 13.Haneef Z, Stern J, Dewar S, Engel J., Jr Referral pattern for epilepsy surgery after evidence-based recommendations: a retrospective study. Neurology 2010;75:699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hakimi AS, Spanaki MV, Schuh LA, Smith BJ, Schultz L. A survey of neurologists' views on epilepsy surgery and medically refractory epilepsy. Epilepsy Behav 2008;13:96–101. [DOI] [PubMed] [Google Scholar]
- 15.Benbadis SR, Heriaud L, Tatum WO, Vale FL. Epilepsy surgery, delays and referral patterns: are all your epilepsy patients controlled? Seizure 2003;12:167–170. [DOI] [PubMed] [Google Scholar]
- 16.Erba G, Moja L, Beghi E, Messina P, Pupillo E. Barriers toward epilepsy surgery: a survey among practicing neurologists. Epilepsia 2012;53:35–43. [DOI] [PubMed] [Google Scholar]
- 17.Wasade VS, Spanaki M, Iyengar R, Barkley GL, Schultz L. AAN epilepsy quality measures in clinical practice: a survey of neurologists. Epilepsy Behav 2012;24:468–473. [DOI] [PubMed] [Google Scholar]
- 18.Engel J, Jr, Wiebe S, French J, et al. Practice parameter: temporal lobe and localized neocortical resections for epilepsy: report of the Quality Standards Subcommittee of the American Academy of Neurology, in association with the American Epilepsy Society and the American Association of Neurological Surgeons. Neurology 2003;60:538–547. [DOI] [PubMed] [Google Scholar]
- 19.Maheux B, Legault C, Lambert J. Increasing response rates in physicians' mail surveys: an experimental study. Am J Public Health 1989;79:638–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kumlien E, Mattsson P. Attitudes towards epilepsy surgery: a nationwide survey among Swedish neurologists. Seizure 2010;19:253–255. [DOI] [PubMed] [Google Scholar]
- 21.Kwan P, Arzimanoglou A, Berg AT, et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc task force of the ILAE Commission on Therapeutic Strategies. Epilepsia 2010;51:1069–1077. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Epilepsy in adults and access to care—United States, 2010. MMWR Morb Mortal Wkly Rep 2012;61:909–913. [PubMed] [Google Scholar]
- 23.Thompson AW, Kobau R, Park R, Grant D. Epilepsy care and mental health care for people with epilepsy: California Health Interview Survey, 2005. Prev Chronic Dis 2012;9:E60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Halpern MT, Renaud JM, Vickrey BG. Impact of insurance status on access to care and out-of-pocket costs for U.S. individuals with epilepsy. Epilepsy Behav 2011;22:483–489. [DOI] [PubMed] [Google Scholar]
- 25.Ferguson PL, Chiprich J, Smith G, et al. Prevalence of self-reported epilepsy, health care access, and health behaviors among adults in South Carolina. Epilepsy Behav 2008;13:529–534. [DOI] [PubMed] [Google Scholar]
- 26.Burneo JG, Jette N, Theodore W, et al. Disparities in epilepsy: report of a systematic review by the North American Commission of the International League Against Epilepsy. Epilepsia 2009;50:2285–2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meyer AC, Dua T, Boscardin WJ, Escarce JJ, Saxena S, Birbeck GL. Critical determinants of the epilepsy treatment gap: a cross-national analysis in resource-limited settings. Epilepsia 2012;53:2178–2185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jedrzejczak J, Marusic P, Haldre S, et al. Current status of epilepsy health care for adult patients from central and eastern European Union countries: a survey of members of the Central Europe Epilepsy Experts Working Group. Seizure 2013;22:452–456. [DOI] [PubMed] [Google Scholar]
- 29.Wiebe S, Gafni A, Blume WT, Girvin JP. An economic evaluation of surgery for temporal lobe epilepsy. J Epilepsy 1995;8:227–235. [Google Scholar]
- 30.Bowen JM, Snead OC, Chandra K, Blackhouse G, Goeree R. Epilepsy care in Ontario: an economic analysis of increasing access to epilepsy surgery. Ont Health Technol Assess Ser 2012;12:1–41. [PMC free article] [PubMed] [Google Scholar]
- 31.Langfitt JT, Holloway RG, McDermott MP, et al. Health care costs decline after successful epilepsy surgery. Neurology 2007;68:1290–1298. [DOI] [PubMed] [Google Scholar]
- 32.Chung K, Liu Y, Ivey SL, et al. Quality of life in epilepsy (QOLIE): insights about epilepsy and support groups from people with epilepsy (San Francisco Bay Area, USA). Epilepsy Behav 2012;24:256–263. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.