Abstract
Objective:
To examine the relationship of recalled adverse childhood experiences (ACEs) with migraine and episodic tension-type headache (ETTH).
Methods:
We conducted a cross-sectional analysis of ACEs among 2007 American Migraine Prevalence and Prevention Study survey respondents with ETTH and migraine. We modeled headache type using logistic regression adjusting for sociodemographic variables (age, race, sex, income), depression, and anxiety, and headache day frequency using ordinal logistic regression with a proportional odds model.
Results:
Participants had migraine (n = 8,305) or ETTH (n = 1,429). Rates of ACEs were significantly higher among respondents with migraine than ETTH for emotional neglect (24.5% vs 21.5%), emotional abuse (22.5% vs 16.7%), and sexual abuse (17.7% vs 13.3%). Odds of migraine vs ETTH were significantly higher for those reporting emotional neglect (odds ratio [OR] = 1.23, 95% confidence interval [CI] 1.07–1.42), emotional abuse (OR = 1.46, 95% CI 1.25–1.71), or sexual abuse (OR = 1.35, 95% CI 1.11–1.62) when adjusted for sociodemographics. Results remained significant only for emotional abuse when adjusting for depression and anxiety (OR = 1.33, 95% CI 1.13–1.57). Odds of migraine were higher with 2 (OR 1.52, 95% CI 1.25–1.86) vs 1 (OR 1.17, 95% CI 1.00–1.36) ACE, which held after adjusting for depression and anxiety. All forms of maltreatment were associated with higher headache day frequency category in migraine but results lost significance after adjusting for depression and anxiety.
Conclusions:
ACEs are associated with a higher risk of migraine vs ETTH. Attenuation of the influence of ACEs by depression and anxiety suggests confounding or mediation, although results for emotional abuse were generally maintained.
Childhood maltreatment is a worldwide problem linked to a broad range of medical and psychiatric comorbidities in adulthood, including neurologic and pain disorders.1–8 Estimates of the prevalence of childhood maltreatment based on self-report in adulthood range from 8% to nearly 40%.9–11 Frequent headache was associated with emotional, sexual, and physical abuse in the landmark Adverse Childhood Experiences (ACEs) Study but headache types were not differentiated.12 Other pioneering studies support the association but are limited by the nature of their samples (e.g., subspecialty headache centers), incomplete characterization of headache subtypes, or limited assessment of ACEs.6–8,13–17
Our objective was to test the hypothesis that ACEs are more strongly associated with migraine than episodic tension-type headache (ETTH). We evaluated rates of childhood emotional maltreatment (abuse and neglect) and sexual abuse in a large, US population–based sample of persons with migraine and tension-type headache using a case-control design. We also sought to determine whether ACEs were associated with headache frequency and whether the number of types of ACEs had an influence. Finally, we examined the effect of anxiety and depression on the associations among ACEs, headache subtype, and frequency.
METHODS
The American Migraine Prevalence and Prevention (AMPP) Study is a longitudinal, population-based, 2-phase study.18 In phase 1, a self-administered screening questionnaire was mailed to a stratified sample of 120,000 households encompassing 257,339 household members, selected to be representative of the US population and drawn from a panel maintained by National Family Opinion, Inc. Surveys were returned by 77,879 households (64.9%), yielding data for 162,756 household members aged 12 years and older. A total of 30,721 respondents reported experiencing “severe headache.” Usable data were obtained from 30,291 respondents, of whom 28,261 reported a headache in the preceding year. A random sample of 24,000 adults (aged 18 years and older) from those who reported experiencing at least one headache in the preceding year were selected to participate in phase 2, a longitudinal study with annual follow-up (2005–2009). Respondents are asked to complete a self-administered questionnaire assessing headache frequency, severity, symptomology, and other information necessary to assign a diagnosis based on International Classification of Headache Disorders, second edition (ICHD-2) criteria.19 Additional data collected in 2007 included sociodemographic variables, depression and anxiety measures, and selected subscales from the Childhood Trauma Questionnaire (CTQ).20 Reasons for nonparticipation were not assessed during the screening phase or at annual follow-up.
Study design.
We conducted a cross-sectional analysis of respondents to the 2007 AMPP Study survey who met ICHD-2 criteria for migraine or ETTH and completed CTQ items. Using a nested case-control study design, we sampled the outcome (headache) and used a validated questionnaire to have adult participants recall adverse experiences they had in childhood and adolescence. The migraine group included all frequencies of headache (i.e., episodic migraine [EM] and chronic migraine). Because there was not a headache-free control group available, we used the cohort with the least intense and frequent headaches, ETTH, as a comparison group.
Standard protocol approvals, registrations, and patient consents.
This study was approved by the Albert Einstein College of Medicine institutional review board.
Data collection: Variables and instruments.
Sociodemographic data.
Sociodemographic data, including age, sex, weight, and height, were obtained via self-report. Other data, including race, ethnicity, geographic region, and annual household income, were obtained from National Family Opinion, Inc. Data collected by the US Census Bureau were accessed to demonstrate that $30,000 is the upper bound for the lower third of annual household incomes.21
Headache information and diagnoses.
Information about headache frequency, severity, and associated symptoms was collected via respondent self-report. ICHD-2 criteria for primary headache were applied to responses to identify headache subtypes using the American Migraine Study/AMPP diagnostic module, which has a sensitivity of 100% and specificity of 82% for the diagnosis of migraine,22 and sensitivity of 91% and specificity of 80% for the diagnosis of chronic migraine.23
History of childhood maltreatment.
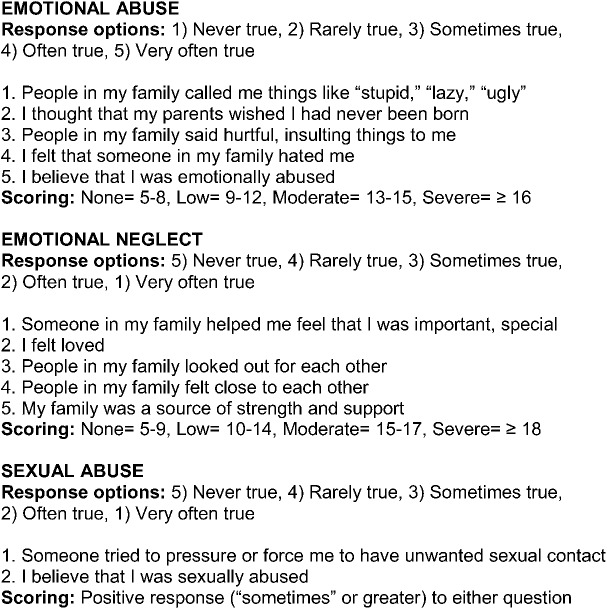
History of childhood maltreatment (younger than 18 years) was assessed using portions of the CTQ, a retrospective, self-report measure of ACEs.20 This questionnaire has shown measurement invariance across 4 samples diverse in age, geography, and health status, as well as good criterion-related validity in a sample of adolescents with corroborative data available from therapists with access to families, referring physicians, child welfare agencies, and court records.20 Our survey included subscales for emotional abuse and emotional neglect and 2 sexual abuse items. The emotional abuse and neglect subscales have 5 response options ranging from never true to very often true. Summed subscale scores range from 5 (no history of abuse or neglect) to 25 (very extreme history of abuse and neglect). The survey included 2 sexual abuse items, one taken directly from the CTQ. Cut scores were ≥13 for emotional abuse (moderate to severe), ≥15 for emotional neglect (moderate to severe), and an answer of sometimes/often/very often true to either sexual abuse question (see the figure).
Figure. Childhood Trauma Questionnaire subscales and items included in 2007 American Migraine Prevalence and Prevention Study survey.
Depression and anxiety.
Depression was assessed using the Patient Health Questionnaire–depression module (PHQ-9),24 a validated measure of major depressive disorder based on DSM-IV criteria.25 The PHQ-9 assesses depressive symptomology over the preceding 2 weeks. Sum scores range from 0 to 27. We used the validated dichotomous cut score of ≥10 indicating moderate or more severe depression in our analyses.
Anxiety was assessed using the anxiety module of the Patient Health Questionnaire,24 a validated instrument based on DSM-IV criteria,25 with questions about 7 symptoms of anxiety over the preceding 4 weeks with 3 response options: not at all, several days, and more than half the days. Anxiety was coded as a dichotomous variable according to the DSM-IV and PHQ clinical algorithms. A respondent who endorsed the first item, “feeling nervous, anxious, on edge, or worrying about a lot of different things,” and at least 3 additional symptoms with “more than half the days” was assigned a diagnosis of anxiety.
Analyses.
Analyses were performed using IBM SPSS Statistics version 20.0.0 (IBM, Armonk, NY). A p value of ≤0.05 was used to identify statistically significant effects. Descriptive statistics were generated for all dependent variables by migraine and ETTH. We modeled dichotomous outcomes of migraine vs ETTH using binary logistic regression with CTQ subscales as predictors adjusting for sociodemographic variables. In subsequent models, we adjusted for depression and anxiety. The relationship of headache day frequency and ACEs was examined using an ordinal logistic regression proportionate odds model assuming that the odds ratios (ORs) for abuse are uniform moving across headache frequency strata from ≤4 to 5–9 to 10–14 to ≥15 days per month. The proportional odds assumption for headache frequency categories was tested on a 25% random subsample of our total population with a parallel lines test. The test results were nonsignificant and null hypothesis was retained, thus showing support for the proportionality assumption.
RESULTS
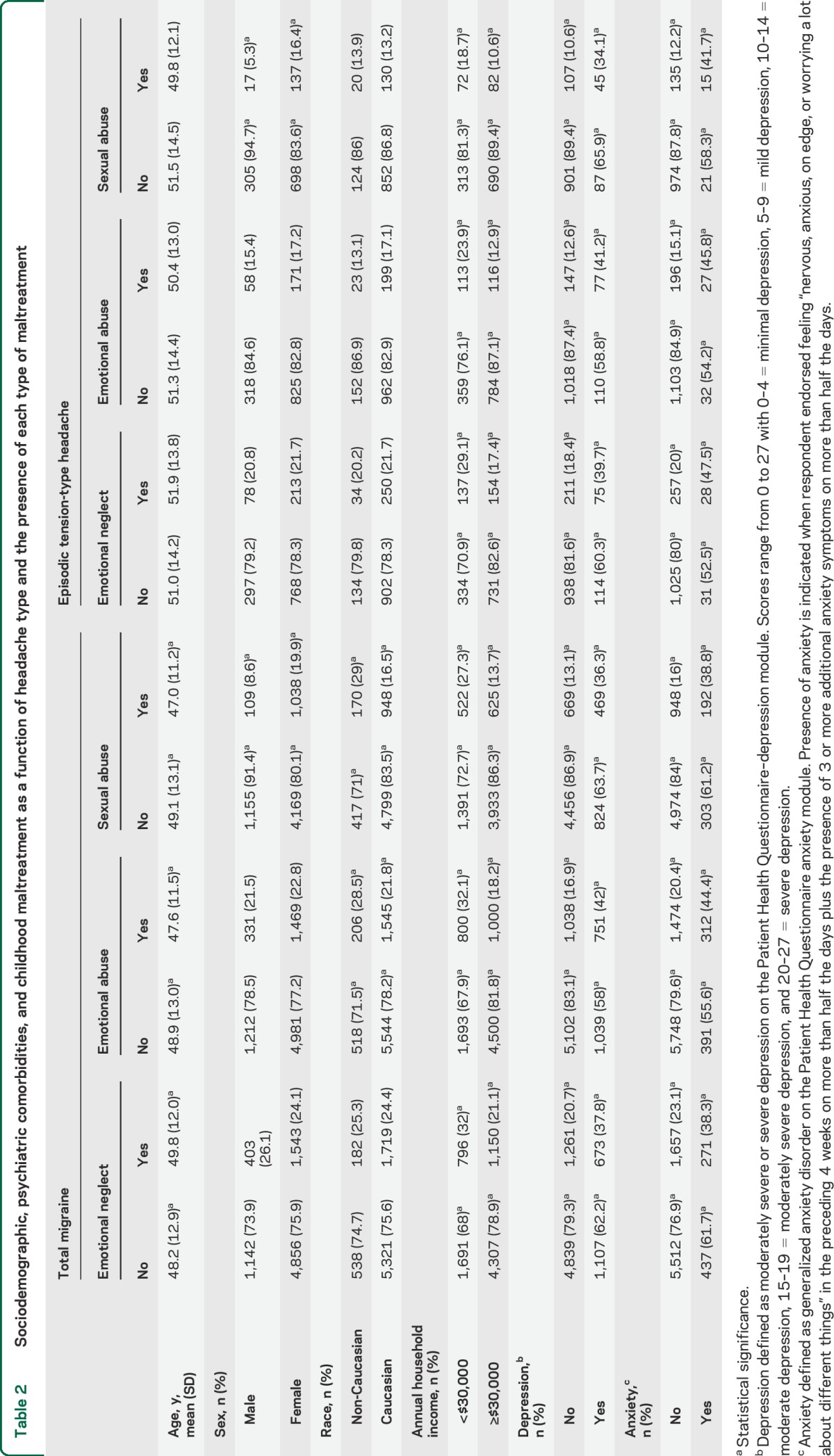
In 2007, the AMPP Study survey was sent to 20,489 and returned by 14,069 respondents (68.7%). Eligible respondents provided the necessary data for analysis and had either ICHD-2–defined migraine (n = 8,305, of whom 557 [6.8%] had chronic migraine) or ETTH (n = 1,429). Compared with the ETTH group, those with migraine were more likely to be younger, female, and have an annual household income of >$30,000 per year, and were more likely to have depression and anxiety (table 1). Overall mean scores for participants with migraine were significantly higher for the CTQ subscales of emotional abuse (migraine 10.08 [SD 5.53] vs ETTH 9.85 [SD 5.20], mean difference −0.82, p < 0.001). Means for emotional abuse were not significantly different across headache groups (migraine 9.03 [SD 5.52] vs ETTH 8.21 [SD 4.25], mean difference −0.23, p = 0.147). Rates based on cutpoints were significantly higher in the migraine group than in the tension headache group for emotional neglect (24.5% vs 21.5%), emotional abuse (22.5% vs 16.7%), and sexual abuse (17.7% vs 13.3%) (table 1). Overall, 34.2% of the ETTH group and 40.2% of the migraine group reported at least 1 of these 3 forms of maltreatment. Rates did not differ substantially by age, but rates of sexual abuse were higher in women (table 2).
Table 1.
Description of study sample from AMPP Study 2007: Sociodemographic, psychiatric comorbidities, and childhood maltreatment as a function of headache type (unadjusted)
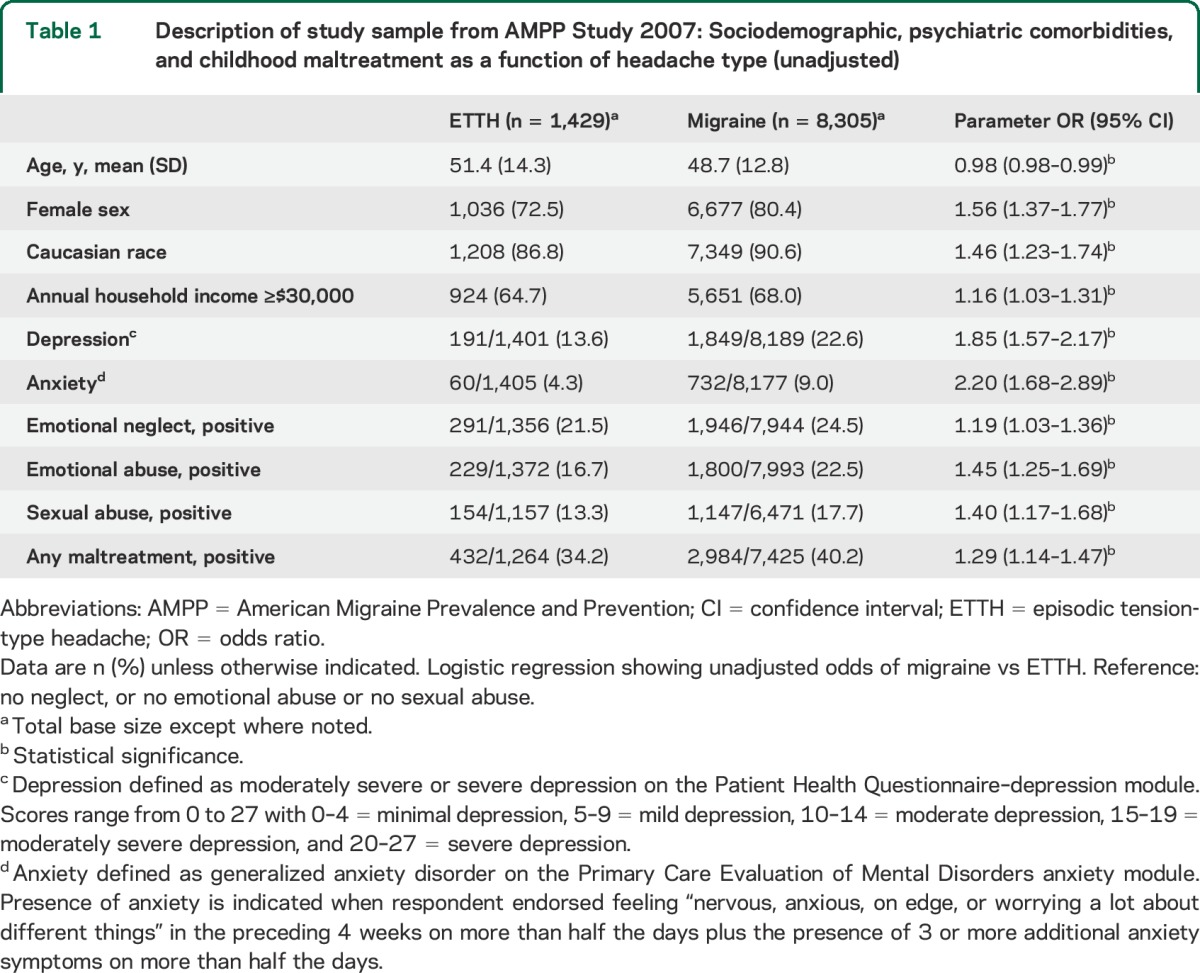
Table 2.
Sociodemographic, psychiatric comorbidities, and childhood maltreatment as a function of headache type and the presence of each type of maltreatment
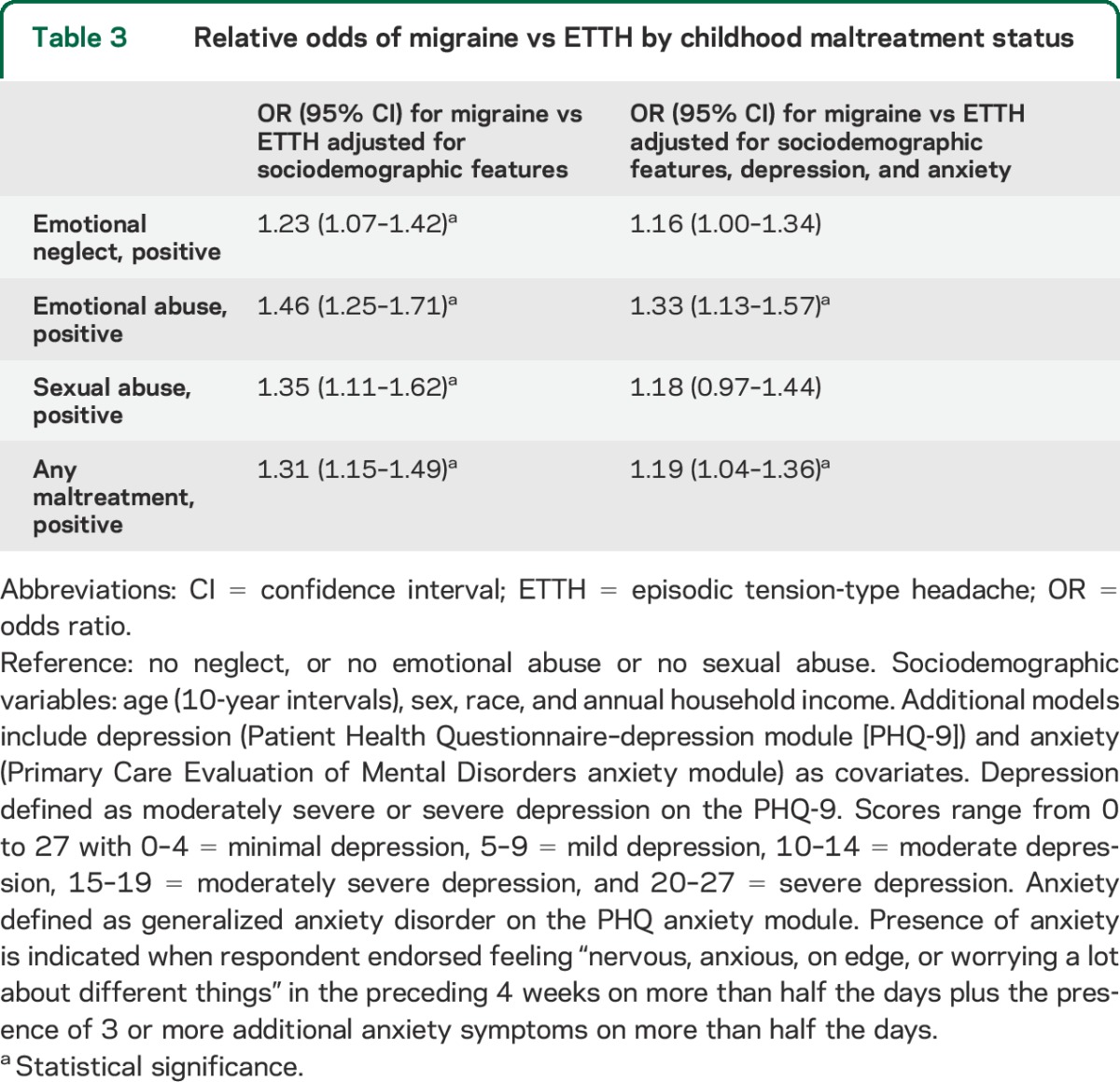
We examined the influence of each type of maltreatment on the relative odds of migraine vs ETTH (table 3). In models adjusted for sociodemographic variables, each type of maltreatment independently predicted higher relative odds of migraine. Further adjustments for depression and anxiety slightly attenuated the ORs in all models; in these fully adjusted models, emotional abuse and the composite variable, any maltreatment, remained statistically significant.
Table 3.
Relative odds of migraine vs ETTH by childhood maltreatment status
We examined the relationship between the number of types of maltreatment and the relative odds of migraine vs ETTH. In models adjusted for sociodemographic factors, compared to the group with no maltreatment, a single type of maltreatment is associated with a marginally significant increase in the odds of migraine (OR 1.17, 95% confidence interval [CI] 1.00–1.36). The association with migraine increased for those with 2 (OR 1.52, 95% CI 1.25–1.86) or 3 types of ACEs (OR 1.44, 95% CI 1.09–1.93). With further adjustments for depression and anxiety, the relative odds of migraine vs ETTH as a function of the number of maltreatment forms decline but remain statistically significant for those with 2 (OR 1.37, 95% CI 1.12–1.68) but not 3 types of ACEs.
Using an ordinal logistic regression proportional odds model, we tested the association of childhood maltreatment and headache frequency defined with the following categories: low-frequency EM (0–4 days per month), moderate-frequency EM (5–9 days per month), high-frequency EM (10–14 days per month), and chronic migraine (≥15 days per month). When adjusted only for sociodemographic variables, there were statistically significant increases in the relative odds of being in a higher frequency headache category as a function of emotional neglect (OR 1.18, 95% CI 1.05–1.32), emotional abuse (OR 1.27, 95% CI 1.12–1.43), sexual abuse (OR 1.25, 95% CI 1.08–1.45), and the any maltreatment composite variable (OR 1.24, 95% CI 1.11–1.38). After adjustment for depression and anxiety, all of these models lost statistical significance (table 4). Interpretation of these results is offered in the discussion.
Table 4.
Relative odds of increasing headache frequency among persons with migraine as a function of maltreatment adjusting for sociodemographic variables status
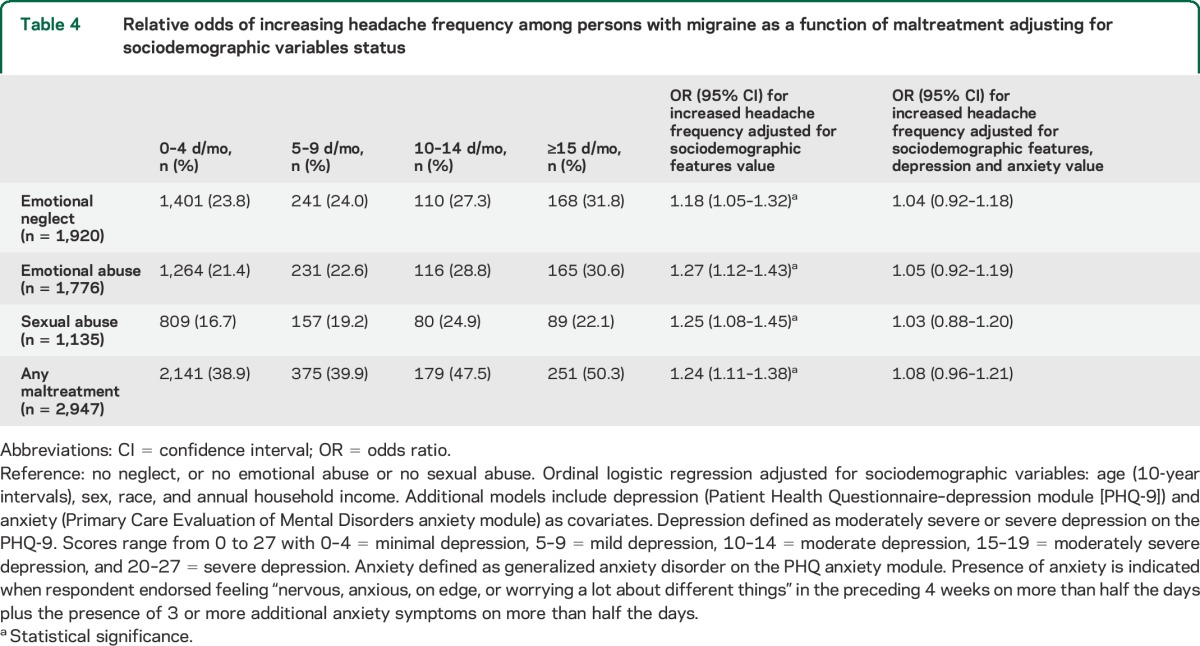
We examined the effect of number of maltreatment types on increased headache day categories and found a dose effect after adjusting for sociodemographics with the relative odds 1.18 (95% CI 1.03–1.34) for 1 ACE, 1.23 (95% CI 1.05–1.43) for 2 ACEs, and 1.40 (95% CI 1.13–1.73) for 3 ACEs, suggesting a trend. However, after adjusting for depression and anxiety, the results lost statistical significance.
DISCUSSION
We examined a population sample of persons with migraine or ETTH for 3 types of ACEs—emotional neglect, emotional abuse, and sexual abuse—in this nested case-control study. Each type of ACE was associated with an increased risk of migraine vs ETTH in analyses adjusted for sociodemographic variables. The association with migraine was stronger for emotional abuse than for sexual abuse. For emotional abuse, results remained significant after adjusting for depression and anxiety, but this was not the case for emotional neglect and sexual abuse. Replacing the binary PHQ-9 score with the continuous PHQ-9 as a covariate in logistic models testing the association of abuse and headache type did not materially alter the results. All 3 forms of maltreatment were also associated with headache day frequency category in the migraine group, but results lost significance after adjusting for depression and anxiety.
Previous retrospective reports have shown that childhood maltreatment is associated with headache,6–8,12 specifically migraine,15–17 but have not contrasted the association in the 2 most common forms of primary headache, migraine and tension-type headache. In the AMPP Study, we do not have data from a headache-free group. The ACE Study, using a questionnaire derived from the CTQ, provides a large survey estimating rates of abuse and neglect in a health plan–based sample.26 In the present report, rates of emotional abuse were highest for migraine (22.5%) and intermediate for ETTH (16.7%); in the ACE Study, reported rates of emotional abuse were lower for the subgroup without frequent headache (9.2%).12 Similarly, rates of emotional neglect were highest in the migraine group (24.5%) and intermediate for ETTH (21.5). In the ACE Study, rates of emotional neglect were lower (14.8%), but data for the subgroup without frequent headache are not available.12
A multicentered headache subspecialty center study used the CTQ to determine rates of emotional abuse and neglect for adult patients with migraine.27 Rates for emotional abuse (22.5% vs 20%) and emotional neglect (24.5% vs 19.0%) were higher in the AMPP Study than in the clinic-based sample, perhaps because social desirability bias leads to underreporting on questionnaires answered in the clinic.28 The elevated prevalence of recalled emotional abuse and neglect in both a population-based and a clinic-based study supports our hypothesis that ACEs are more common in persons with migraine.
Depression and anxiety, 2 disorders purported to amplify sensitivity to pain, are each associated with both migraine and abuse.29–31 Adjusting for depression and anxiety lessened the association of ACEs and migraine. However, the influence of emotional maltreatment and any maltreatment remained statistically significant after adjustment. Within general populations, a study of migraine and 3 studies of pain noted the independent influence of childhood maltreatment, although there was some evidence for depression-related mediation as well.17,29–31 Within headache clinic samples, one study found that the relationship of chronic migraine and abuse was dependent on depression,13 whereas in a second larger study, it was not.14
The attenuation of the influence of maltreatment on migraine by depression and anxiety could be attributed to mediation, confounding, or to a common brain substrate. Under the hypothesis of mediation, ACEs may contribute to the development of depression and anxiety, which in turn contribute to the development of migraine. Under the hypothesis of confounding, depression and anxiety are associated with both the exposure (ACEs) and the outcome (migraine) while not part of the causal pathway linking them. Alternatively, ACEs may give rise to a brain substrate that predisposes to depression, anxiety, and migraine, a hypothesis partially supported by evidence that ACEs are associated with enduring brain changes.32 Under the hypotheses of mediation or shared brain substrate, adjusting for depression and anxiety is overadjusting because they are in the causal pathway.
In addition to migraine and tension-type headache, a number of other pain conditions including fibromyalgia, irritable bowel syndrome, interstitial cystitis, and temporomandibular joint disorder have also been associated with recalled ACEs in retrospective studies.33 These conditions are referred to as complex persistent pain conditions.34 The term central sensitization syndromes is also applied,35 implying a potential shared pathogenesis. Studies showing that ACEs are linked to biomarkers of inflammation in adulthood suggest a possible mechanistic pathway.36 Abuse-induced stress during childhood, a time of heightened CNS plasticity, has also been hypothesized to have a role in the development of chronic pain disorders via production of psychobiological changes that enhance pain sensitivity.37
Our results suggest a dose-response effect in the relationship between number of ACEs and headache subtype. The relative odds of migraine vs ETTH were higher in those with 2 or 3 forms of ACEs in contrast to those with a single form. Results were not statistically significant for those with 3 forms of adverse experience, perhaps because of the smaller sample size. The ACE Study12 found that the prevalence and odds of developing frequent headache increased with number of ACEs experienced in childhood. The headache clinic study found within the migraine population a direct positive correlation between the number of maltreatment types and pain conditions.33 These dose-response relationships suggest the possibility of a causal relationship between abuse and pain, including migraine. Within the AMPP Study migraine group, each and any type of maltreatment was associated with the higher likelihood of increased headache frequency. Furthermore, the relative odds of increased frequency are a function of the number of maltreatment types. The attenuation of the association of ACEs with headache frequency by anxiety and depression may be attributable to confounding, mediation, or a shared brain substrate. This is at odds with headache clinic study findings that the association of emotional abuse and neglect with chronic (as opposed to episodic) migraine was independent of, although influenced by, depression and anxiety.14 A better understanding of abuse-related changes in brain structure and regulation of the endocrine, autonomic, and immune systems may help explain these discrepant findings.
Strengths of our study include a large and population-based sample. We used validated instruments such as the American Migraine Study/AMPP diagnostic module, the CTQ emotional abuse and neglect modules, and the PHQ/Primary Care Evaluation of Mental Disorders measures of depression and anxiety.
Limitations include the collection of self-reported data for a number of variables and the lack of a nonheadache control group. Most likely, the use of a tension-type headache control group, with self-described “severe” headaches, reduced our estimates of the association between migraine and ACEs. Recall bias is a limitation of case-control studies. The passage of time, coupled with the traumatic nature of ACEs may interfere with accurate recall, perhaps leading to underreporting. However, depressed mood may lead to recasting of past experiences in a negative light, raising the specter of overreporting. Two studies ascertained childhood abuse both through court documents and self-report. Abuse based on court records failed to demonstrate an association with pain in adulthood and documented maltreatment, whereas the association was demonstrated using self-reports.31,38 Analysis of one of the studies suggested that the review of court records may have missed cases of abuse.38 This could falsely attenuate the association of childhood abuse and adult pain. A third prospective study in children and adolescents found that those who were sexually abused were more likely than a matched control group to experience somatic difficulties, including pain.39
Finally, we were not able to collect the entire CTQ because of space limitations in the AMPP Study survey. Therefore, we did not have data on physical abuse and neglect, all of the sexual abuse items, or other adverse experiences of childhood.
Given the high rates of ACEs and the association with migraine, particularly in depressed persons, health care professionals should be attuned to the issues of ACEs, including development of posttraumatic stress disorder, nonsuicidal self-injurious behaviors, and revictimization. Health care professionals may consider incorporating a validated questionnaire into their clinical assessment and should have information and referral options readily available. For additional information, see the American Academy of Neurology program Recognizing Abuse in Your Neurology Patients, available at http://tools.aan.com/education/webcme/index.cfm?event=program:info&program_id=5. For patient information, see http://www.achenet.org/resources/abuse_maltreatment_and_ptsd_and_their_relationship_to_headache_and_migraine/.
ACKNOWLEDGMENT
The authors thank C. Mark Sollars, MS, for editorial assistance.
GLOSSARY
- ACE
adverse childhood experience
- AMPP
American Migraine Prevalence and Prevention
- CI
confidence interval
- CTQ
Childhood Trauma Questionnaire
- DSM-IV
Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition)
- EM
episodic migraine
- ETTH
episodic tension-type headache
- ICHD-2
International Classification of Headache Disorders, second edition
- OR
odds ratio
- PHQ
Patient Health Questionnaire
- PHQ-9
Patient Health Questionnaire–depression module
AUTHOR CONTRIBUTIONS
Dr. Tietjen contributed to study concept or design, analysis or interpretation of data, and drafting/revising the manuscript for content. Dr. Buse contributed to study concept or design, analysis or interpretation of data, and drafting/revising the manuscript for content. Dr. Fanning contributed to study concept or design, analysis or interpretation of data, statistical analysis, and drafting/revising the manuscript for content. Dr. Serrano contributed to study concept or design, analysis or interpretation of data, statistical analysis, and drafting/revising the manuscript for content. Dr. Reed contributed to study concept or design, analysis or interpretation of data, obtaining funding, and drafting/revising the manuscript for content. Dr. Lipton contributed to study concept or design, analysis or interpretation of data, obtaining funding, and drafting/revising the manuscript for content.
STUDY FUNDING
The American Migraine Prevalence and Prevention Study was funded through a research grant to the National Headache Foundation (NHF) from McNeil-Janssen Scientific Affairs, LLC (MJSA), Raritan, NJ. The AMPP Study database was donated by MJSA to the NHF for use in various projects. Analysis for this report was supported by a grant from NHF.
DISCLOSURE
G. Tietjen has received funding for research from GlaxoSmithKline. She serves on the editorial board of Headache, has reviewed for the National Institute of Neurological Disorders and Stroke (NINDS) and the Migraine Research Foundation, owns common stock in Johnson & Johnson and Stryker, served as an advisory board member, and received honoraria from MAP Pharmaceuticals and the American Headache Society. D. Buse has received funding for research and honoraria from Allergan Pharmaceuticals/MAP Pharmaceuticals, Novartis, Zogenix/Teva, the American Headache Society, and the National Headache Foundation. K. Fanning has received research support from Allergan Inc., CoLucid, Endo Pharmaceuticals, GlaxoSmithKline, MAP Pharmaceuticals, Merck & Co., Inc., NuPathe, Novartis, Ortho-McNeil, and the National Headache Foundation. D. Serrano has received research support from Allergan Inc., CoLucid, Endo Pharmaceuticals, GlaxoSmithKline, MAP Pharmaceuticals, Merck & Co., Inc., NuPathe, Novartis, Ortho-McNeil, and the National Headache Foundation. M. Reed has received funding for research and data analysis from Allergan Inc., CoLucid, Endo Pharmaceuticals, GlaxoSmithKline, MAP Pharmaceuticals, Merck, Novartis, NuPathe, Ortho-McNeil, and the National Headache Foundation. R. Lipton has received research support from the NIH (PO1 AG03949 [program director, project and core leader], RO1AG025119 [investigator], RO1AG022374-06A2 [investigator], RO1AG034119 [investigator], RO1AG12101 [investigator], K23AG030857 [mentor]), the National Headache Foundation, and the Migraine Research Fund. He serves on the editorial board of Neurology®, has reviewed for the NIA and NINDS, holds stock options in eNeura Therapeutics; serves as a consultant, advisory board member, or has received honoraria from Allergan, the American Headache Society, Autonomic Technologies, Boehringer-Ingelheim Pharmaceuticals, Boston Scientific, Bristol-Myers Squibb, CogniMed, CoLucid, Eli Lilly, ENDO, eNeura Therapeutics, GlaxoSmithKline, Merck, Novartis, NuPathe, Pfizer, and Vedanta Research. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet 2009;373:68–81. [DOI] [PubMed] [Google Scholar]
- 2.US Department of Health & Human Services. Childhood maltreatment 2011. Available at: http://www.acf.hhs.gov/programs/cb/resource/child-maltreatment-2011. Accessed December 12, 2012.
- 3.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prev Med 1998;14:245–258. [DOI] [PubMed] [Google Scholar]
- 4.Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Prev Med 2003;37:268–277. [DOI] [PubMed] [Google Scholar]
- 5.Sachs-Ericsson N, Blazer D, Plant EA, Arnow B. Childhood sexual and physical abuse and the 1-year prevalence of medical problems in the national comorbidity survey. Health Psychol 2005;24:32–40. [DOI] [PubMed] [Google Scholar]
- 6.McCauley J, Kern DE, Kolodner K, et al. Clinical characteristics of women with a history of childhood abuse: unhealed wounds. JAMA 1997;277:1362–1368. [PubMed] [Google Scholar]
- 7.Golding JM. Sexual assault history and headache: five general population studies. J Nerv Ment Dis 1999;187:624–629. [DOI] [PubMed] [Google Scholar]
- 8.Walker EA, Gelfand A, Katon WJ, et al. Adult health status of women with histories of childhood abuse and neglect. Am J Med 1999;107:332–339. [DOI] [PubMed] [Google Scholar]
- 9.Gorey KM, Leslie DR. The prevalence of child sexual abuse: integrative review adjustment for potential response and measurement biases. Child Abuse Negl 1997;21:391–398. [DOI] [PubMed] [Google Scholar]
- 10.Dong M, Anda RF, Dube SR, Giles WH, Felitti VJ. The relationship of exposure to childhood sexual abuse to other forms of abuse, neglect, and household dysfunction during childhood. Child Abuse Negl 2003;27:625–639. [DOI] [PubMed] [Google Scholar]
- 11.Walker EA, Torkelson N, Katon WJ, Koss MP. The prevalence rate of sexual trauma in a primary care clinic. J Am Board Fam Pract 1993;6:465–471. [PubMed] [Google Scholar]
- 12.Anda R, Tietjen G, Schulman E, Felitti V, Croft J. Adverse childhood experiences and frequent headaches in adults. Headache 2010;50:1473–1481. [DOI] [PubMed] [Google Scholar]
- 13.Tietjen GE, Brandes JL, Digre KB, et al. History of childhood maltreatment is associated with comorbid depression in women with migraine. Neurology 2007;69:959–968. [DOI] [PubMed] [Google Scholar]
- 14.Tietjen GE, Brandes JL, Peterlin BL, et al. Childhood maltreatment and migraine (part II): emotional abuse as a risk factor for headache chronification. Headache 2010;50:32–41. [DOI] [PubMed] [Google Scholar]
- 15.Tietjen GE, Khubchandani J, Herial NA, Shah K. Adverse childhood experiences are associated with migraine and vascular biomarkers. Headache 2012;52:920–929. [DOI] [PubMed] [Google Scholar]
- 16.Goodwin RD, Hoven CW, Murison R, Hotopf M. Association between childhood physical abuse and gastrointestinal disorders and migraine in adulthood. Am J Public Health 2003;93:1065–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fuller-Thomson E, Baker TM, Brennenstuhl S. Investigating the association between childhood physical abuse and migraine. Headache 2010;50:749–760. [DOI] [PubMed] [Google Scholar]
- 18.Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 2007;68:343–349. [DOI] [PubMed] [Google Scholar]
- 19.Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia 2004;24(suppl 1):9–160. [DOI] [PubMed] [Google Scholar]
- 20.Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl 2003;27:169–190. [DOI] [PubMed] [Google Scholar]
- 21.United States Census Bureau. 2005 current population survey annual social and economic supplements. Available at: http://www.census.gov/cps/. Accessed June 15, 2014.
- 22.Lipton RB, Diamond S, Reed M, Diamond ML, Stewart WF. Migraine diagnosis and treatment: results from the American Migraine Study II. Headache 2001;41:638–645. [DOI] [PubMed] [Google Scholar]
- 23.Liebenstein M, Bigal M, Sheftell F, Tepper S, Rapoport A, Lipton R. Validation of the Chronic Daily Headache Questionnaire (CDH-Q). Headache 2007;47:760–761. [Google Scholar]
- 24.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999;282:1737–1744. [DOI] [PubMed] [Google Scholar]
- 25.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 26.Centers for Disease Control and Prevention. Adverse Childhood Experiences (ACE) Study. Available at: http://www.cdc.gov/ace/index.htm. Accessed January 18, 2013.
- 27.Tietjen GE, Brandes JL, Peterlin BL, et al. Childhood maltreatment and migraine (part I): prevalence and adult revictimization: a multicenter headache clinic survey. Headache 2010;50:20–31. [DOI] [PubMed] [Google Scholar]
- 28.Tourangeau R, Yan T. Sensitive questions in surveys. Psychol Bull 2007;133:859–883. [DOI] [PubMed] [Google Scholar]
- 29.Sachs-Ericsson N, Kendall-Tackett K, Hernandez A. Childhood abuse, chronic pain, and depression in the National Comorbidity Survey. Child Abuse Negl 2007;31:531–547. [DOI] [PubMed] [Google Scholar]
- 30.Walsh CA, Jamieson E, Macmillan H, Boyle M. Child abuse and chronic pain in a community survey of women. J Interpers Violence 2007;22:1536–1554. [DOI] [PubMed] [Google Scholar]
- 31.Brown J, Berenson K, Cohen P. Documented and self-reported child abuse and adult pain in a community sample. Clin J Pain 2005;21:374–377. [DOI] [PubMed] [Google Scholar]
- 32.Teicher MH, Andersen SL, Polcari A, Anderson CM, Navalta CP, Kim DM. The neurobiological consequences of early stress and childhood maltreatment. Neurosci Biobehav Rev 2003;27:33–44. [DOI] [PubMed] [Google Scholar]
- 33.Tietjen GE, Brandes JL, Peterlin BL, et al. Childhood maltreatment and migraine (part III): association with comorbid pain conditions. Headache 2010;50:42–51. [DOI] [PubMed] [Google Scholar]
- 34.Diatchenko L, Nackley AG, Slade GD, Fillingim RB, Maixner W. Idiopathic pain disorders: pathways of vulnerability. Pain 2006;123:226–230. [DOI] [PubMed] [Google Scholar]
- 35.Yunus MB. Fibromyalgia and overlapping disorders: the unifying concept of central sensitivity syndromes. Semin Arthritis Rheum 2007;36:339–356. [DOI] [PubMed] [Google Scholar]
- 36.Danese A, Caspi A, Williams B, et al. Biological embedding of stress through inflammation processes in childhood. Mol Psychiatry 2011;16:244–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meagher M. Links between traumatic family violence and chronic pain: biopsychosocial pathways and treatment implications. In: Kendall-Tackett KA, editor. Health Consequences of Abuse in the Family: A Clinical Guide for Evidence-Based Practice. Washington, DC: American Psychological Association; 2004:155–177. [Google Scholar]
- 38.Raphael KG, Widom CS, Lange G. Childhood victimization and pain in adulthood: a prospective investigation. Pain 2001;92:283–293. [DOI] [PubMed] [Google Scholar]
- 39.Rimsza ME, Berg RA, Locke C. Sexual abuse: somatic and emotional reactions. Child Abuse Negl 1998;12:201–208. [DOI] [PubMed] [Google Scholar]