Abstract
The aim of this study was to determine the association between more advanced stages of temporomandibular joint (TMJ) intra-articular disorders (“TMJ intra-articular status”), representing a transition from normal joint structure to TMJ disc displacement with and without reduction (DDwR and DDwoR) to degenerative joint disease (DJD), and patient-reported outcomes of jaw pain, function, and disability (“TMD impact”). This cross-sectional study included 614 cases from the RDC/TMD Validation Project with at least one temporomandibular disorder (TMD) diagnosis. TMJ intra-articular status was determined by 3 blinded, calibrated radiologists using magnetic resonance imaging and computed tomography as one of normal joint structure, DDwR, DDwoR, or DJD, representing the subject’s most advanced TMJ diagnosis. TMD impact was conceptualized as a latent variable consisting of 1) pain intensity (Characteristic Pain Index from the Graded Chronic Pain Scale [GCPS]), 2) jaw function (Jaw Functional Limitation Scale), and 3) disability (Disability Points from GCPS). A structural equation model estimated the association of TMJ intra-articular status with the latent measure TMD impact as a correlation coefficient in all TMD cases (n = 614) and in cases with a TMD pain diagnosis (n = 500). The correlations between TMJ intra-articular status and TMD impact were 0.05 (95% confidence interval [CI], −0.04 to 0.13) for all TMD cases and 0.07 (95% CI, −0.04 to 0.17) for cases with a pain diagnosis, which are neither statistically significant nor clinically relevant. Conceptualizing worsening of TMJ intra-articular disorders as 4 stages and characterizing impact from TMD as a composite of jaw pain, function, and disability, this cross-sectional study found no clinically significant association. Models of TMJ intra-articular status other than ours (normal structure → DDwR → DDwoR → DJD) should be explored.
Keywords: temporomandibular joint dysfunction syndrome, musculoskeletal system, craniomandibular disorders, myofascial pain syndromes, pain perception, osteoarthritis
Introduction
Temporomandibular disorders (TMDs) are a heterogeneous group of disorders affecting the masticatory system with pain as the dominating characteristic. Temporomandibular joint (TMJ) intra-articular disorders (IDs) are also prevalent, notably TMJ disc displacements (DDs) and degenerative joint disease (DJD). The impact of these IDs on patients is of interest because interventions to treat structural TMD disorders, such as TMJ surgery, differ from interventions targeting pain-related TMD. Hence, clinical decision making could be influenced if IDs are related to jaw pain, function, and disability, but this clinical impact is not well understood.
Many people view IDs as a group of disorders that starts as DD with reduction (DDwR), develops to DD without reduction (DDwoR), and then to DJD (Rasmussen 1981; Wilkes 1989; de Leeuw et al. 1995a). Conversely, others have suggested that most individuals with DDwR never develop DDwoR or DJD (Westesson and Lundh 1989; de Leeuw et al. 1995b; Salé Bryndahl and Isberg 2013), and if they do, it has little impact on jaw pain, function, or disability. Thus, it is not clear how TMJ structural status affects patients.
Previous investigations assessing this research question suffered from lack of a comprehensive set of reliable, valid patient-reported outcomes (PROs) characterizing TMD’s multidimensional impact, limited sample size, selected study populations, or lack of imaging techniques for validly diagnosing DD and DJD (Boering 1966; Rasmussen 1981; Laskin 1994; Kurita et al. 2006). The Validation Project provides data that overcome these methodologic problems: Using a large number and the full spectrum of TMD cases, TMJ intra-articular status was assessed by magnetic resonance imaging (MRI) and computed tomography (CT), and the impact of TMJ disorders was assessed by a comprehensive set of PROs, consisting of jaw pain intensity, jaw function, and pain-related disability.
The present study’s aim was to investigate in TMD cases whether more advanced stages of structural TMJ intra-articular status were related to jaw pain, jaw function, and disability.
Methods
Setting and Subjects
This cross-sectional study included subjects of the RDC/TMD Validation Project, a multicenter project of the University of Minnesota, the University of Washington, and the University at Buffalo. From those 705 subjects, we included 614 TMD cases with at least one consensus-based TMD physical diagnosis rendered by 2 TMD experts at each site (Schiffman et al. 2010), representing a convenience sample of clinic and community TMD cases (85% female; mean ± standard deviation age, 37.1 ± 13.1 years). Subjects were included in the present study based on presence of any TMD diagnosis regardless of whether they were clinical or community cases or what symptoms they reported. For more details regarding study subjects and setting, see Ahmad et al. (2009), Schiffman et al. (2010), and Anderson et al. (2011). The present report follows the STROBE statement for cross-sectional studies.
TMJ Intra-articular Status: Soft and Hard Tissue Structural Stages of the TMJ
Three blinded, calibrated radiologists interpreted bilateral TMJ CT and MRI and rendered one of these diagnoses: normal joint structure (“normal”), DDwR, DDwoR, or DJD (Ahmad et al. 2009). For each subject, the most advanced diagnosis of the 2 TMJs was determined, resulting in 81 cases with normal joints (all had painful TMD), 217 cases with DDwR (n = 154 with a painful TMD), 75 cases with DDwoR (n = 63 with a painful TMD), and 241 cases with DJD (n = 202 with a painful TMD). Among cases with DDwR and DDwoR, 145 (69%) and 21 (28%), respectively, were found to have bilateral displacement. For cases with DJD, bilateral involvement was found for 102 (42%).
For the analyses presented here, TMJ intra-articular status was treated as a stepwise variable advancing from normal structure to DJD with DDwR and DDwoR as intermediate stages. The interrater reliability of the 3 radiologists for determining stages of TMJ intra-articular status was good to excellent (κDDwR = 0.78 [95% confidence interval (CI), 0.68 to 0.86]; κDDwoR = 0.94 [95% CI, 0.89 to 98]; κDJD = 0.71 [95% CI, 0.63 to 0.79]) (Ahmad et al. 2009).
TMD Impact: A Latent Variable Combining Jaw Pain, Function, and Disability
TMD impact was conceptualized as a latent variable, a construct characterizing how TMD affects patients. It consisted of 3 PROs:
Pain intensity, measured by Characteristic Pain Intensity (CPI) from the Graded Chronic Pain Scale (GCPS) (VonKorff et al. 1992): score range, 1 to 100 points (higher scores indicate greater pain).
Jaw function, measured by the Jaw Functional Limitation Scale 20 (JFLS-20) global scale (Ohrbach et al. 2008): score range, 1 to 200 points (higher scores indicate worse jaw function). The JFLS has 3 subscales: Mastication, Vertical Jaw Mobility, and Emotional and Verbal Expression.
Jaw disability, measured by Disability Points (DP) from the GCPS (VonKorff et al. 1992): score range, 0 to 100 points (higher scores indicate worse disability).
TMD impact was the dependent variable in the structural equation model (SEM) analyses; the 3 PROs represented the SEM measurement model.
Data Analysis
TMJ intra-articular status was treated as a measure taking values 1, 2, 3, and 4 for normal, DDwR, DDwoR, and DJD, respectively. We chose this simple model, with an equal distance of severity between stages, in the absence of evidence for more complicated models describing how the stages differ in terms of severity. This conceptualization of TMJ intra-articular status allowed us to investigate whether overall worsening of TMJ structures had a patient-perceived impact.
We first estimated simultaneously, using multivariate multiple regression, the association between TMJ intra-articular status and each PRO. This analysis investigated whether jaw pain, function, and disability increased with more advanced stages of TMJ disorders, taking into account the correlations among the PROs and adjusting for possible confounding effects from age (entered linearly) and sex. We also restricted analyses to TMD cases with DDwR, DDwoR, and DJD (3-level TMJ intra-articular status) to investigate whether results would be similar in a more homogeneous sample of TMD cases with intra-articular diagnoses. In addition to these tests of a specific formulation of TMJ intra-articular status, in secondary analyses, we performed a test using unordered TMJ intra-articular status categories. Here, DDwR, DDwoR, and DJD were each tested in the multivariate regression model against the normal (base) category, assessing whether any TMJ intra-articular status level is associated with each PRO. Finally, in exploratory analyses, we used the 3 JFLS subscales individually as outcome variables in linear regression analyses.
Second, we used SEM to estimate the effect of TMJ intra-articular status on TMD impact, which summarizes the 3 PROs in a latent variable. The SEM provides a more interpretable effect measure, a correlation coefficient, for the association between TMJ intra-articular status and TMD impact. The magnitude of this coefficient, and therefore the clinical relevance of the TMJ intra-articular status–TMD impact association, can be judged by comparing it with guidelines for effect sizes (Cohen 1988). In the first step, we fitted a measurement model relating the CPI, JFLS, and disability scores to the latent variable TMD impact. Fit statistics for this model could not be calculated because the model is just identified. According to recommendations for assessing goodness of fit for such a model (Brown 2012), we assessed the magnitude of the loadings, their standard errors, and their statistical significance. In a second step, we added the exposure variable as the structural part of the SEM analysis.
We performed all analyses in 2 sets of TMD cases, those with and without a painful diagnosis, representing populations to which we want to generalize our results. For details about the hypotheses investigated and the targeted populations, see the Appendix.
Results
Descriptions of Jaw Pain, Function, and Disability
Cases with Any TMD Diagnosis
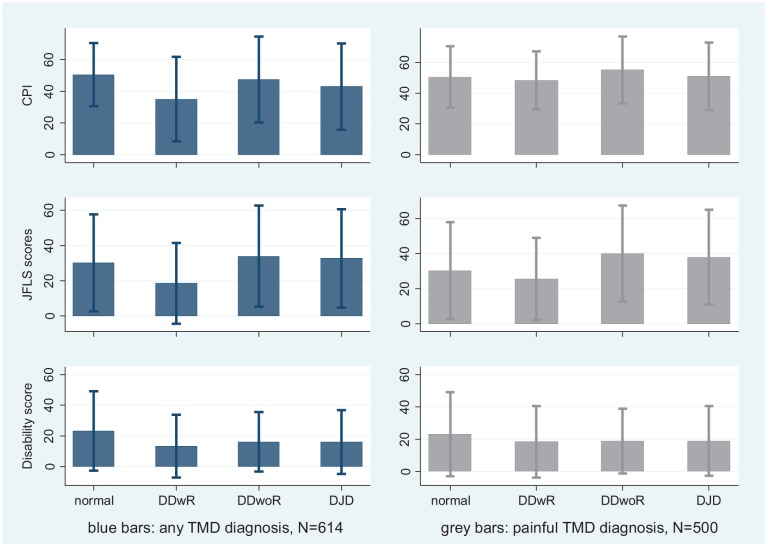
TMD cases with or without a pain diagnosis presented with substantial jaw pain, limitations in jaw functioning, and disability (Fig. 1). Average CPI for cases with structurally normal joints—all of whom had a pain diagnosis—was a moderate 51 on a 0 to 100 scale. Cases with DDwoR or DJD—some of whom did not have a pain diagnosis—had slightly lower average pain intensity. Cases with DDwR had the lowest average CPI, 31. Patterns of scores for jaw function limitation and for disability were similar to jaw pain. Overall, PRO scores were not higher for theoretically more advanced stages of TMJ intra-articular status.
Figure 1.
Means ± standard deviations for Characteristic Pain Intensity (CPI; 0 to 100), Jaw Functional Limitation Scale (JFLS; 0 to 200), and jaw disability scores (0 to 100) for all temporomandibular disorder (TMD) cases (blue bars) and for TMD cases with a pain diagnosis only (gray bars). DJD, degenerative joint disease; DDwR, disc displacement with reduction; DDwoR, disc displacement without reduction.
Cases with TMD Pain Diagnosis
TMD cases with a pain diagnosis presented slightly higher average pain, functional limitation, and disability than did cases with any diagnosis, because all these cases had at least one TMD pain diagnosis (Fig. 1); however, the changes from excluding those without pain diagnoses were small. As with all TMD cases, PRO scores were not higher for theoretically more advanced stages of TMJ intra-articular status. The largest observed difference between diagnoses was for jaw disability, comparing normal and DDwR versus DDwoR and DJD, but even this difference was only a couple points.
Correlation among Jaw Pain, Function, and Disability
Cases with Any TMD Diagnosis
The 3 PROs—jaw pain, jaw function limitation, and disability—had pairwise correlations between 0.52 and 0.62.
Cases with TMD Pain Diagnosis
Pairwise correlations were slightly lower in this group, between 0.44 and 0.52. Confidence intervals (95%) around these coefficients were tight (±0.05 to 0.07). These substantial correlations suggested that these outcomes could be combined into a composite, latent outcome of TMD impact.
Association between TMJ Intra-articular Status and TMD Impact
Cases with Any TMD Diagnosis
In the unadjusted multivariate regression, TMJ intra-articular status was significantly associated with JFLS but not with CPI or disability (Table 1). The combined association of TMJ intra-articular status with all 3 PROs (JFLS, CPI, and disability scores) was statistically significant (P < 0.001). A one-step increase in TMJ intra-articular status was associated with a 4-point increase in JFLS (0 to 200 range). The standardized effect size for a difference between the extreme groups (normal [level 1] minus DJD [level 4]) was only −0.09 (95% CI, −0.34 to 0.16), indicating that JFLS scores worsened only slightly with TMJ intra-articular status. According to guidelines (Cohen 1988), this is smaller than a “small” effect, so despite the statistically significant association between TMJ intra-articular status and JFLS score, the relationship has no clinical relevance. Adjusting these analyses for age and sex had a negligible effect (Table 1).
Table 1.
Association between Ordered Levels of TMJ Intra-articular Status (Normal → DDwR → DDwoR → DJD) and Jaw Pain (CPI), Function (JFLS), and Disability, Analyzed Using Unadjusted and Adjusted Multivariate Multiple Regression, in TMD Cases with Any TMD Diagnosis or Cases with Only a Painful TMD Diagnosis.
| Analysis | Dependent Variable | Independent Variable | Any TMD Diagnosisa |
Painful TMD Diagnosisa |
||
|---|---|---|---|---|---|---|
| Intercept | Coefficient (95% CI) | Intercept | Coefficient (95% CI) | |||
| Unadjusted | CPI (0 to 100) | Normal → DDwR → DDwoR → DJD | 41 | 0 (–1 to 2) | 50 | 1 (–1 to 2) |
| JFLS (0 to 200) | Normal → DDwR → DDwoR → DJD | 21 | 4 (2 to 6) | 26 | 4 (2 to 6) | |
| Disability (0 to 100) | Normal → DDwR → DDwoR → DJD | 17 | −1 (−2 to 1) | 21 | −1 (−3 to 1) | |
| Adjusted (multiple regression) | CPI | Normal → DDwR → DDwoR → DJD | 40 | 0 (−2 to 2) | 48 | 1 (−1 to 2) |
| Age | −0.1 (−0.3 to 0.1) | 0.0 (−0.1 to 0.2) | ||||
| Sex | 6 (0 to 12) | 1 (−4 to 7) | ||||
| JFLS | Normal → DDwR → DDwoR → DJD | 17 | 3 (1 to 5) | 22 | 4 (2 to 6) | |
| Age | 0.0 (−0.2 to 0.2) | 0.1 (−0.1 to 0.3) | ||||
| Sex | 4 (−2 to 10) | 1 (−6 to 8) | ||||
| Disability | Normal → DDwR → DDwoR → DJD | 11 | −1 (−3 to 0) | 13 | −1 (−3 to 0) | |
| Age | 0.1 (0.0 to 0.3) | 0.2 (0.1 to 0.4) | ||||
| Sex | 3 (−2 to 8) | 1 (−5 to 7) | ||||
CI, confidence interval; CPI, Characteristic Pain Intensity; DJD, degenerative joint disease; DDwR, disc displacement with reduction; DDwoR, disc displacement without reduction; JFLS, Jaw Functional Limitation Scale; TMD, temporomandibular disorder; TMJ, temporomandibular joint.
Two subjects were excluded from analyses because of missing JFLS data.
In unadjusted analyses restricted to TMD cases with intra-articular diagnoses, the combined association of TMJ intra-articular status with all 3 PROs (JFLS, CPI, and disability scores) was also statistically significant (P < 0.001). A one-step increase of TMJ intra-articular status was associated with a 4-point increase in CPI (95% CI, 1 to 6 points), a 7-point increase in JFLS (95% CI, 5 to 9 points), and a 1-point increase in disability scores (95% CI, −1 to 3 points). Again, adjusting these analyses for age and sex had negligible effect.
In our secondary analyses, testing unordered levels of TMJ intra-articular status (in contrast to the ordered TMJ intra-articular status above) while adjusting for age and sex, a mixed picture appeared (Table 2). Compared with normal, DDwR had less pain, less functional impairment, and less disability. Also compared with normal, both DDwR and DJD had less pain and less disability but more functional impairment. While the effect of DDwR was statistically significant for pain, functional impairment, and disability, the effect of DJD was significant only for pain and disability, and the effect for DDwoR was significant only for disability. In exploratory analyses using JFLS subscales as outcome variables, TMJ intra-articular status was statistically significantly associated with the Mastication and the Vertical Jaw Mobility scale but not with the Emotional and Verbal Expression scale.
Table 2.
Association between Unordered Levels TMJ Intra-articular Status (DDwR, DDwoR, or DJD vs. Base Category Normal) and Jaw Pain (CPI), Function (JFLS), and Disability, Analyzed Using Adjusted Multivariate Multiple Regression, in TMD Cases with Any TMD Diagnosis or Cases with Only a Painful TMD Diagnosis.
| Analysis | Dependent Variable | Independent Variable | Any TMD Diagnosisa |
Painful TMD Diagnosisa |
||
|---|---|---|---|---|---|---|
| Intercept | Coefficient (95% CI) | Intercept | Coefficient (95% CI) | |||
| Adjusted (multiple regression) | CPI | DDwRb | 52 | −17 (−24 to −10) | 48 | −2 (−8 to 3) |
| DDwoRb | −5 (−13 to 4) | 5 (−2 to 12) | ||||
| DJDb | −8 (−15 to −2) | 0 (–5 to 6) | ||||
| Age | −0.2 (−0.3 to 0.0) | 0.0 (−0.1 to 0.2) | ||||
| Sex | 7 (1 to 13) | 2 (−4 to 8) | ||||
| JFLS | DDwRb | 28 | −12 (−19 to −6) | 26 | −5 (−12 to 3) | |
| DDwoRb | 3 (−5 to 11) | 10 (1 to 19) | ||||
| DJDb | 2 (−5 to 9) | 7 (0 to 14) | ||||
| Age | 0.0 (−0.2 to 0.1) | 0.1 (−0.1 to 0.3) | ||||
| Sex | 5 (−1 to 11) | 3 (−4 to 9) | ||||
| Disability | DDwRb | 17 | −10 (−15 to −4) | 15 | −4 (−10 to 3) | |
| DDwoRb | −7 (−14 to 0) | −3 (−11 to 4) | ||||
| DJDb | −8 (−14 to −3) | −5 (−11 to 1) | ||||
| Age | 0.1 (0.0 to 0.2) | 0.2 (0.0 to 0.4) | ||||
| Sex | 3 (−2 to 8) | 1 (−5 to 7) | ||||
CI, confidence interval; CPI, Characteristic Pain Intensity; DJD, degenerative joint disease; DDwR, disc displacement with reduction; DDwoR, disc displacement without reduction; JFLS, Jaw Functional Limitation Scale; TMD, temporomandibular disorder; TMJ, temporomandibular joint.
Two subjects were excluded from analyses because of missing JFLS data.
Compared with normal (joints).
In the SEM, combining the JFLS, CPI, and disability scores into a latent TMD impact variable, the correlation between TMJ intra-articular status and TMD impact was 0.05 (95% CI, −0.04 to 0.13; Fig. 2). In the latent variable’s measurement model, all loadings were very high, precise (i.e., had narrow confidence intervals), and statistically significant, supporting the fit of the model. This minimal correlation of 0.05 was neither clinically relevant nor statistically significant, and the upper limit of its confidence interval excluded moderate and large associations. Again, age and sex adjustment changed results negligibly. As expected, in the SEM analyses, jaw pain, jaw function limitation, and disability had strong (0.86, 0.73, and 0.71 respectively) and precise (all 95% CI: ±0.05) loadings on the latent TMD impact measure.
Figure 2.
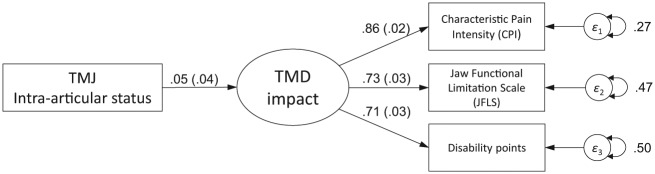
Structural equation model for the association between temporomandibular joint (TMJ) intra-articular status and temporomandibular disorder (TMD) impact. The oval represents the latent factor TMD impact; the rectangles represent measured indicators for the latent factor with their error variances (circles) or the measured exposure variable TMJ intra-articular status. The lines connecting the latent factor to indicators are factor loadings, and the line connecting the exposure variable TMJ intra-articular status to the latent outcome TMD impact is the correlation between exposure and the latent factor. Numbers provided are standardized values. Analyses were performed with Stata 12 (StataCorp LP, College Station, TX, USA) and used a maximum likelihood estimation, assuming jaw pain, function, and disability items were continuous.
Cases with TMD Pain Diagnosis
Results in this subset of cases were similar to results for cases with any TMD diagnosis, regardless of whether analyses were performed for ordered (Table 1) or unordered (Table 2) levels of TMJ intra-articular status or whether analyses were restricted to TMD cases with intra-articular diagnoses. Results of the multivariate regressions were almost identical without and with age/sex adjustment, with TMJ intra-articular status having a statistically significant but clinically trivial association with JFLS (Mastication and Vertical Jaw Mobility subscales in particular) but no association with CPI or disability (Table 1). Again, an overall association with all 3 variables was also present.
In the SEM, the correlation between TMJ intra-articular status and TMD impact was 0.07 (95% CI, −0.04 to 0.17), neither clinically relevant nor statistically significant, with the upper limit of the confidence interval excluding moderate and large associations and negligible effect of age and sex adjustment.
Discussion
The results of this cross-sectional study suggest that what is currently understood as a change of TMJ structure from normal joint structures to DD to DJD may not be perceived by patients as relevant in terms of jaw pain, function, and disability.
It is challenging to compare our findings with the literature because the association between structural TMJ intra-articular status (stages of ID) and PROs has not been studied using the latent variable “TMD impact.” In addition, the literature presents only fragmented evidence. Some studies assessed only disc position and other studies focused on osseous changes, while our study assessed both and integrates them in one model. While we characterized TMD impact as a latent composite of jaw pain, jaw function, and disability, the impact of TMD can be conceptualized and, consequently, measured differently. However, some studies have reported the association of ID stages to pain and, to a lesser degree, to jaw function and disability.
Intra-articular Disorders and Pain
Several authors (Westesson and Lundh 1989; Bertram et al. 2001; Emshoff et al. 2001; Campos et al. 2008) have reported significant associations between ID stages and jaw pain, but only one (Emshoff et al. 2003) reported the magnitude of this association. Using MRI in subjects with and without TMJ pain, the study found that TMJ pain occurred significantly more often in patients with DDwoR with DJD (OR [odds ratio], 11.7; 95% CI, 0.96 to 42.7) and DDwoR without DJD (OR, 10.2; 95% CI, 1.91 to 54.1). Conversely, other studies (Ohlmann et al. 2006; Palconet et al. 2012) did not find an association between ID stages and TMJ pain or reported a small correlation between maximum condylar change on cone-beam computed tomography (CBCT) and pain ratings (Palconet et al. 2012). Longitudinal studies provided evidence that outcomes for patients with different ID stages differed little at follow-up and were good in general. For example, in 40 patients with DDwoR for a period of 2.5 years without treatment, 75% of the cases had decreased pain (60% became asymptomatic) while only 25% showed no improvement or required treatment (Kurita et al. 1998).
Intra-articular Disorders and Function
We found no studies of the association of JFLS with TMJ intra-articular status. However, using the Jaw Disability Scale from the Research Diagnostic Criteria for TMD, which includes some items consistent with the JFLS, Karacayli et al. (2011) found that chronic TMD pain patients with MRI-depicted DDwR, compared with healthy controls, had more difficulty with jaw function, including talking, smiling, and cleaning their teeth or face. In their classic articles, Rasmussen and Wilkes reported that jaw pain and function were related to stages of ID (Rasmussen 1981; Wilkes 1989); however, jaw function was mainly assessed by range of motion. Rasmussen reported that TMJ pain increased and jaw function was compromised progressively through the stages of DD but then improved with development of DJD. However, in Rasmussen’s study, 20% of subjects with DJD had persistent jaw muscle pain and 25% of subjects with DJD continued to have limited mouth opening (i.e., jaw function limitation). Thus, many subjects with DJD had jaw pain and limited function. Wilkes’s findings from a surgical case series have been broadly accepted by clinicians as supporting a biomedical model of DD progressing to a debilitating “end-stage” DJD accompanied by increased jaw pain and functional limitation. While some authors showed that condylar hypomobility was significantly associated with DDwoR (Campos et al. 2008), others reported only a small correlation between maximum condylar osseous change and range of motion (Palconet et al. 2012). Another study provided strong evidence against clinical relevance of ID stages for dysfunction (Schiffman et al. 1992), concluding that ID stages were not related to clinical signs of dysfunction.
Intra-articular Disorders and Disability
When the GCPS was used to assess disability in 37 chronic pain patients with MRI-depicted DDwR, patients had a disability score of zero points, but their oral health-related quality of life (OHRQoL) scores were worse compared with healthy controls (Karacayli et al. 2011). Also, OHRQoL scores were worse in patients with DDwoR with limited mouth opening than in patients with DDwR (Reissmann et al. 2007). Conversely, no differences were found between cases with DD and DJD using the Limitation of Daily Functions instrument (Kino et al. 2005) or the Pain Disability Index (Bush and Harkins 1995).
Study Limitations
Shortcomings of our findings are related to study design and population as well as the studied concepts and variables.
To interpret our results causally, the stages of intra-articular status needed to precede the pain and functional impairments. This seems plausible, but pain and its inflammatory process can also lead to TMJ changes (de Bont and Stegenga 1993; Zarb and Carlsson 1999). Our cross-sectional study design limits a causal interpretation.
Our study population is heterogeneous, which is advantageous for generalizability of findings but may have hampered detection of more subtle associations.
Our model of TMJ structural stages with equal distances between the 4 stages is simple. While numerous articles (Rasmussen 1981; Westesson and Lundh 1989; Wilkes 1989; de Leeuw et al. 1995a; de Leeuw et al. 1995b; Kurita et al. 2006) support this staging with DD as intermediate stages and DJD as the final stage, other more complex models may exist that explain TMJ intra-articular status.
Our model of TMD impact is also simple. Pain, function, and disability are essential domains of suffering for symptomatic TMD patients, but other components may also be important.
For a more detailed discussion of methodological considerations, see the Appendix.
Conclusion
This cross-sectional study found no association between TMJ intra-articular status and TMD impact represented by pain, jaw function, and disability. This suggests that TMJ intra-articular disorders have minimal impact on patients’ reported pain, function, and disability. This also suggests that treatments focusing on TMJ intra-articular disorders, such as surgery, may have limited impact on patient-reported outcomes (Schiffman et al. 2014). Validation of this finding in longitudinal studies is necessary, and models of TMJ intra-articular status other than ours (normal structure → DDwR → DDwoR → DJD) should be explored.
Author Contributions
P. Chantaracherd, M.T. John, J.S. Hodges, E.L. Schiffman, contributed to conception, design, and data analysis, drafted and critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Supplementary Material
Footnotes
The research was supported by National Institutes of Health/National Institute of Dental and Craniofacial Research grant U01-DE013331.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
A supplemental appendix to this article is published electronically only at http://jdr.sagepub.com/supplemental.
References
- Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove EL, John MT, Schiffman EL. 2009. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 107(6):844–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson GC, John MT, Ohrbach R, Nixdorf DR, Schiffman EL, Truelove ES, List T. 2011. Influence of headache frequency on clinical signs and symptoms of TMD in subjects with temple headache and TMD pain. Pain. 152(4):765–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertram S, Rudisch A, Innerhofer K, Pümpel E, Grubwieser G, Emshoff R. 2001. Diagnosing TMJ internal derangement and osteoarthritis with magnetic resonance imaging. J Am Dent Assoc. 132(6):753–761. [DOI] [PubMed] [Google Scholar]
- Boering G. 1966. Temporomandibular joint arthrosis: an analysis of 400 cases [dissertation]. Groningen, the Netherlands: University of Groningen. [Google Scholar]
- Brown TA. 2012. Confirmatory factor analysis for applied research. New York (NY): Guilford. [Google Scholar]
- Bush FM, Harkins SW. 1995. Pain-related limitation in activities of daily living in patients with chronic orofacial pain: psychometric properties of a disability index. J Orofac Pain. 9(1):57–63. [PubMed] [Google Scholar]
- Campos MI, Campos PS, Cangussu MC, Guimarães RC, Line SR. 2008. Analysis of magnetic resonance imaging characteristics and pain in temporomandibular joints with and without degenerative changes of the condyle. Int J Oral Maxillofac Surg. 37(6):529–534. [DOI] [PubMed] [Google Scholar]
- Cohen J. 1988. Statistical power analyses for the behavioral sciences. 2nd ed. Hillsdale (NJ): Lawrence Erlbaum. [Google Scholar]
- de Bont LG, Stegenga B. 1993. Pathology of temporomandibular joint internal derangement and osteoarthrosis. Int J Oral Maxillofac Surg. 22(2):71–74. [DOI] [PubMed] [Google Scholar]
- de Leeuw R, Boering G, Stegenga B, de Bont LG. 1995a. Radiographic signs of temporomandibular joint osteoarthrosis and internal derangement 30 years after nonsurgical treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 79(3):382–392. [DOI] [PubMed] [Google Scholar]
- de Leeuw R, Boering G, Stegenga B, de Bont LG. 1995b. TMJ articular disc position and configuration 30 years after initial diagnosis of internal derangement. J Oral Maxillofac Surg. 53(3):234–241; discussion 241–242. [DOI] [PubMed] [Google Scholar]
- Emshoff R, Brandlmaier I, Gerhard S, Strobl H, Bertram S, Rudisch A. 2003. Magnetic resonance imaging predictors of temporomandibular joint pain. J Am Dent Assoc. 134(6):705–714. [DOI] [PubMed] [Google Scholar]
- Emshoff R, Rudisch A, Innerhofer K, Bosch R, Bertram S. 2001. Temporomandibular joint internal derangement type III: relationship to magnetic resonance imaging findings of internal derangement and osteoarthrosis. An intraindividual approach. Int J Oral Maxillofac Surg. 30(5):390–396. [DOI] [PubMed] [Google Scholar]
- Karacayli U, Mumcu G, Cimilli H, Sisman N, Sur H, Gunaydin Y. 2011. The effects of chronic pain on oral health related quality of life in patients with anterior disc displacement with reduction. Community Dent Health. 28(3):211–215. [PubMed] [Google Scholar]
- Kino K, Sugisaki M, Haketa T, Amemori Y, Ishikawa T, Shibuya T, Sato F, Amagasa T, Shibuya T, Tanabe H, et al. 2005. The comparison between pains, difficulties in function, and associating factors of patients in subtypes of temporomandibular disorders. J Oral Rehabil. 32(5):315–325. [DOI] [PubMed] [Google Scholar]
- Kurita H, Uehara S, Yokochi M, Nakatsuka A, Kobayashi H, Kurashina K. 2006. A long-term follow-up study of radiographically evident degenerative changes in the temporomandibular joint with different conditions of disk displacement. Int J Oral Maxillofac Surg. 35(1):49–54. [DOI] [PubMed] [Google Scholar]
- Kurita K, Westesson PL, Yuasa H, Toyama M, Machida J, Ogi N. 1998. Natural course of untreated symptomatic temporomandibular joint disc displacement without reduction. J Dent Res. 77(2):361–365. [DOI] [PubMed] [Google Scholar]
- Laskin DM. 1994. Current controversies in surgery for internal derangements of the temporomandibular joint: etiology and pathogenesis of internal derangement of the temporomandibular joint. Oral Maxillofac Surg Clin North Am. 6:217–222. [Google Scholar]
- Ohlmann B, Rammelsberg P, Henschel V, Kress B, Gabbert O, Schmitter M. 2006. Prediction of TMJ arthralgia according to clinical diagnosis and MRI findings. Int J Prosthodont. 19(4):333–338. [PubMed] [Google Scholar]
- Ohrbach R, Larsson P, List T. 2008. The jaw functional limitation scale: development, reliability, and validity of 8-item and 20-item versions. J Orofac Pain. 22(3):219–230. [PubMed] [Google Scholar]
- Palconet G, Ludlow JB, Tyndall DA, Lim PF. 2012. Correlating cone beam CT results with temporomandibular joint pain of osteoarthritic origin. Dentomaxillofac Radiol. 41(2):126–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen OC. 1981. Description of population and progress of symptoms in a longitudinal study of temporomandibular arthropathy. Scand J Dent Res. 89(2):196–203. [DOI] [PubMed] [Google Scholar]
- Reissmann DR, John MT, Schierz O, Wassell RW. 2007. Functional and psychosocial impact related to specific temporomandibular disorder diagnoses. J Dent. 35(8):643–650. [DOI] [PubMed] [Google Scholar]
- Salé H, Bryndahl F, Isberg A. 2013. Temporomandibular joints in asymptomatic and symptomatic nonpatient volunteers: a prospective 15-year follow-up clinical and MR imaging study. Radiology. 267(1):183–194. [DOI] [PubMed] [Google Scholar]
- Schiffman EL, Anderson GC, Fricton JR, Lindgren BR. 1992. The relationship between level of mandibular pain and dysfunction and stage of temporomandibular joint internal derangement. J Dent Res. 71(11):1812–1815. [DOI] [PubMed] [Google Scholar]
- Schiffman EL, Ohrbach R, Truelove EL, Tai F, Anderson GC, Pan W, Gonzalez YM, John MT, Sommers E, List T, et al. 2010. The research diagnostic criteria for temporomandibular disorders, V: methods used to establish and validate revised Axis I diagnostic algorithms. J Orofac Pain. 24(1):63–78. [PMC free article] [PubMed] [Google Scholar]
- Schiffman EL, Velly AM, Look JO, Hodges JS, Swift JQ, Decker KL, Anderson QN, Templeton RB, Lenton PA, Kang W, et al. 2014. Effects of four treatment strategies for temporomandibular joint closed lock. Int J Oral Maxillofac Surg. 43(2):217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VonKorff M, Ormel J, Keefe FJ, Dworkin SF. 1992. Grading the severity of chronic pain. Pain. 50(2):133–149. [DOI] [PubMed] [Google Scholar]
- Westesson PL, Lundh H. 1989. Arthrographic and clinical characteristics patients with disk displacement who progressed to closed lock during a 6-month period. Oral Surg Oral Med Oral Pathol. 67(6):654–657. [DOI] [PubMed] [Google Scholar]
- Wilkes CH. 1989. Internal derangement of the temporomandibular joint: pathologic variations. Arch Otolaryngol Head Neck Surg. 115(4):469–477. [DOI] [PubMed] [Google Scholar]
- Zarb GA, Carlsson GE. 1999. Temporomandibular disorders: osteoarthritis. J Orofac Pain. 13(4):295–306. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.