Highlights
-
•
The case study details a patient's multiple admissions with aseptic pneumoperitoneum.
-
•
Rough description of his management course is provided.
-
•
The fact that no cause for his pneumoperitoneum is clearly illustrated.
-
•
The patient's last presentation was managed conservatively with success.
-
•
This supports the idea that aseptic pneumoperitoneum can be treated conservatively.
Keywords: Spontaneous pneumoperitoneum, Pneumatosis cystoides intestinalis, Air under diaphragm
Abstract
INTRODUCTION
Pneumoperitoneum, observed by radiography, is typically associated with the perforation of hollow viscous. More than 90% of all cases of pneumoperitoneum are the result of a gastrointestinal tract perforation. These patients usually present with signs of acute peritonitis and require immediate surgical exploration and intervention. However, rare cases of idiopathic spontaneous pneumoperitoneum do occur without any indication of visceral perforation and other known causes of the free intraperitoneal gas.
PRESENTATION OF CASE
A 66-year-old male presented to the emergency department on three separate occasions with similar episodes six months apart. Upon physical examination and subsequent testing, chest radiography revealed the presence of free intraperitoneal gas. A computerized tomography (CT) was performed in which pneumatosis and pneumoperitoneum was reported with the first two admissions and both laparotomies were negative. This patient continues to be followed for prostate cancer and bony metastases. All subsequent CT scans (last performed 01/2014) have shown no acute or chronic abdominal pathology and no obstructions. He also had upper and lower endoscopies in 2011, which were negative.
DISCUSSION
This case revealed very different finding than anticipated. The patient presented to the emergency department with symptoms unrelated to the CT findings of free intraperitoneal gas. On two separate occasions, the patient underwent a laparotomy with negative findings. The conventional course of treatment for pneumoperitoneum was followed, but was it necessary? Though the presentation of pneumoperitoneum is most often associated with significant pathology requiring surgical intervention, a more conservative approach may be applicable in cases similar to the one presented here.
1. Introduction
Pneumoperitoneum is a condition typically identified through radiological studies. In more than 90% of all cases, the aetiology is known to be associated with perforation of a hollow viscera such as the gastrointestinal tract (GI). The most common type of perforation is caused by a peptic ulcer in the stomach or duodenum.2,3 In rare cases, pneumoperitoneum is not caused by visceral perforation. It may be caused by intra-abdonimal, intra-thoracic, gynaecological or iatrogenic origins.4 When these causes are all ruled out, we are left with an undetermined origin. In the case presented here, the spontaneous idiopathic pneumoperitoneum was recurrent and the diagnosis of pneumoperitoneum was discovered secondary to presenting with an unrelated chief complaint. The most common abdominal causes of spontaneous pneumoperitoneum are perforated pneumatosis cystoides intestinalis, infection by gas-producing organisms such as clostridium and penetrating wound in the abdomen.
2. Case report
In July 2011, this 66-year-old male presented to the emergency department with abdominal pain and distention following an outpatient chest radiograph revealing free intraperitoneal gas (Fig. 1). He complained of gradual bloating and abdominal distention. Upon examination, the patient was afebrile. His abdomen was soft and denied any pain with palpation. His white blood cell count was within normal limits at 4.7. Surgical notes indicated it as a “difficult diagnosis with a patient that presents clinically well”.
Fig. 1.

Chest radiography July, 2011. Aseptic spontaneous pneumoperitoneum of unknown origin discovered during routine physical examination.
The patient was observed overnight and scheduled for repeat radiography in the morning. Physical examination on day two showed no new symptoms, however the computed tomography (CT) was positive for pneumatosis and pneumoperitoneum with undetermined source (Fig. 2). It was the determination of the surgical team to proceed with a laparotomy. Intra-operatively, the bowel and stomach was extensively examined and no evidence of perforation was found. The abdominal wall was closed and the patient was returned to the surgical ward for post-operative care.
Fig. 2.
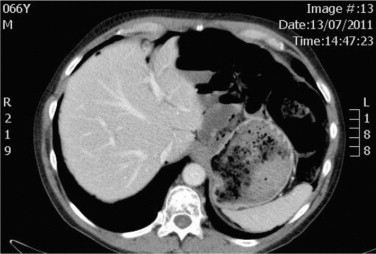
Abdominal CT scan July 2011 confirming pneumoperitoneum.
Two days post laparotomy, the patient was tolerating clear liquids. He remained afebrile with no abdominal distension, no pain other than some tenderness about the incision and had good bowel sounds. He was discharged on post-operative day five, after tolerating a normal diet and restoration of bowel function. Follow-up outpatient CT scans were unremarkable for any free air.
This same male patient then presented to the emergency department in March 2012. This time he was admitted with right leg cellulitis. Upon history taking and physical examination he also noted gradual abdominal distension over the past few weeks. He was not experiencing any nausea, vomiting or abdominal pain. The clinical findings following examination were once again negative for any signs of perforation or peritonitis. A chest radiograph was completed as part of the patient work-up and it revealed free air under the diaphragm (Fig. 3), similar to the previous episode six months earlier. It should be noted that the patient had both lower and upper gastrointestinal endoscopies in October, 2011 that were unremarkable.
Fig. 3.

Chest radiography completed March 2012 during emergency department work-up. Results determined free intraperitoneal gas.
He underwent a CT scan that further confirmed the diagnosis of pneumoperitoneum. The patient was informed of the CT findings and the need to have a laparotomy. He was reluctant to agree to surgery due to the fact that his previous procedure, for the same pathology, was negative. However, he did agree to a plan of watchful waiting and observation for the night.
A repeat CT scan showed a large amount of free intraperitoneal gas with associated pneumatosis of the small bowel (Fig. 4). It was also noted that the findings of pneumatosis and the free air had actually worsened compared to the CT performed earlier.
Fig. 4.

Abdominal CT March 2012. Confirming pneumoperitoneum and pneumatosis of small bowel.
The decision was made at that time to perform a diagnostic laparoscopy which progressed to a laparotomy. Once again, even though a laparotomy was indicated, there was no hollow viscera perforation or any other changes that could determine the origin of the pneumoperitoneum. Severe pneumatosis was present with no obvious perforation (Fig. 5). The patient was discharged seven days later following a course of antibiotics to treat the cellulitis.
Fig. 5.

Photograph taken during March 2012 laparotomy.
Approximately three month later, this patient presented to the emergency department for the third time for a similar occurrence. Once again, a CT scan had revealed the presence of free air under the diaphragm. After presenting this information to the patient, he declined surgery and the surgical team did not push for a procedure to be performed. It was determined to admit him for observation and proceed with IV antibiotics. Upon the third day of admission, the patient remained clinically well and made a decision to self-discharge.
This patient continues to be followed in an outpatient setting for unrelated medical conditions and has been admitted through the emergency department on several occasions. The unique findings of this case are that subsequent CT studies (four since his last laparotomy) and admissions have not revealed any additional episodes of pneumoperitoneum. All scans have also been negative for acute abdominal pathology and obstructions.
3. Discussion
The term pneumoperitoneum refers to the presence of air within the peritoneal cavity. The most common cause is a perforation of the abdominal viscera such as a perforated ulcer. Although, a pneumoperitoneum may occur as a result of perforation of any part of the bowel. Other causes include a benign ulcer, a tumour, or trauma.5 The exception is a perforated appendix, which seldom causes a pneumoperitoneum.
The presence of a pneumoperitoneum does not, however, always imply a perforation. This is because a number of other (mostly non surgical) conditions that is associated with pneumoperitoneum. Likewise, not every bowel perforation results in a pneumoperitoneum. Some perforations heal over, sealing themselves and allowing just a small amount of gas to escape.
Traditional medicine teaches us that a pneumoperitoneum usually indicates a surgical intervention because of visceral perforation (in more than 90% of all cases) and that spontaneous pneumoperitoneum without peritonitis is a rare phenomenon. However, in more recent case studies, the evidence supports that it can be managed conservatively.6 For the surgeon evaluating the case, this causes a surgical dilemma. It requires proper assessment by thorough history and physical examination (including radiography).
Although radiographic studies associated with this patient did not indicate pneumatosis cystoides intestinalis, it is reported to be the most common cause of spontaneous pneumoperitoneum, and possibly the cause in this case.7 In the case report presented here, there is a lesson for surgeons who are inexperienced with or unaware of this condition. Pneumoperitoneum, preceded by a reasonable clinical history in a patient with an adequate abdominal examination, may warrant continued observation and thus avoiding an unnecessary laparotomy.8,9
4. Conclusion
The conventional course of treatment for pneumoperitoneum has been historically favoured, but not always necessary. Although the presentation of pneumoperitoneum is most often associated with significant pathology requiring surgical intervention, a more conservative approach is applicable in cases similar to the one presented here.1,3,4
Conflict of interest statement
None declared.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
The principal author has been involved in the design, data collection, writing the manuscript. No other parties have been involved in the mentioned case report.
References
- 1.Mann C.M., Bhati C.S., Gemmell D., Doyle P., Gupta V., Gorman D.F. Spontaneous pneumoperitoneum: diagnostic and management difficulties. Emerg Med Aust. 2010;6:568–570. doi: 10.1111/j.1742-6723.2010.01357.x. [DOI] [PubMed] [Google Scholar]
- 2.Pitiakoudis M., Zezos P., Oikonomou A., Kirmanidis M., Kouklakis G., Simopoulos C. Spontaneous idiopathic pneumoperitoneum presenting as an acute abdomen: a case report. J Med Case Rep. 2011;5:86. doi: 10.1186/1752-1947-5-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Derveaux K., Penninckx F. Recurrent “spontaneous” Pneumoperitoneum: a diagnostic and therapeutic dilemma. Acta Chir Belg. 2003;103:490–492. doi: 10.1080/00015458.2003.11679473. [DOI] [PubMed] [Google Scholar]
- 4.van Gelder H.M., Allen K.B., Renz B., Sherman R. Spontaneous pneumoperitoneum. A surgical dilemma. Am J Surg. 1991;57(March (3)):151–156. [PubMed] [Google Scholar]
- 5.Wlliams N.M.A., Watkin D.F.L. Spontaneous pneumoperitoneum and other non-surgical causes of intraperitoneal free gas. Postgrad Med J. 1997;73:531–537. doi: 10.1136/pgmj.73.863.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marwah S., Gupta R., Dhall J.C. Non-surgical spontaneous pneumoperitoneum, a case report. Indian Pract. 2002;55:122–124. [Google Scholar]
- 7.Mularski R.A., Ciccolo M.L., Rappaport W.D. Non-surgical causes of pneumoperitoneum. West J Med. 1999;170:41–46. [PMC free article] [PubMed] [Google Scholar]
- 8.McLaren O. Spontaneous idiopathic recurrent pneumoperitoneum. J Surg Case Rep. 2013;8 doi: 10.1093/jscr/rjt071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DeGrinder W.L., Nacol M., Walzel J. Chronic aseptic spontaneous pneumoperitoneum without a serious complication in 8 years. Arch Surg. 1995;130:557–559. doi: 10.1001/archsurg.1995.01430050107019. [DOI] [PubMed] [Google Scholar]


