Highlights
-
•
We present case of chronic traumatic diaphragmatic hernia.
-
•
Traumatic diaphragmatic hernia are rare and under diagnosed.
-
•
Chronic hernia may require complex abdominal reconstruction.
-
•
Computed tomography has diagnostic characteristics.
Keywords: Diaphragm hernia, Traumatic hernia, Hernia repair, Mesh
Abstract
Introduction
Traumatic diaphragmatic hernia is a rare and often under recognized complication of penetrating and blunt trauma. These injuries are often missed or there is a delay in diagnosis which can lead to enlargement of the defect and the development of abdominal or respiratory symptoms.
Presentation of case
We report a case of an otherwise healthy 37 year old male who was involved in a motor vehicle accident at age twelve. He presented 25 years later with vague lower abdominal symptoms and was found to have a large chronic left sided diaphragmatic hernia involving the majority of his intra-abdominal contents. Repair of the defect with a biologic mesh was undertaken and the patient also required complex abdominal wall reconstruction due to loss of intra-abdominal domain from the chronicity of the hernia. A staged closure of the abdomen was performed first with placement of a Wittmann patch. Medical management of intra-abdominal hypertension was successful and the midline fascia was sequentially approximated at the bedside for three days. The final closure was performed with a component separation and implantation of a fenestrated biologic fetal bovine mesh to reinforce the closure. In addition, a lightweight Ultrapro mesh was placed for additional lateral reinforcement. The patient recovered well and was discharged home.
Discussion
These injuries are rare and diagnosis is challenging. Mechanism and CT scan characteristics can aid clinicians.
Conclusion
Blunt diaphragmatic injury is rare and remains a diagnostic challenge. Depending on the chronicity of the injury, repair may require complex surgical decision making.
1. Introduction
Traumatic diaphragmatic hernia is a rare and often under recognized complication of penetrating and blunt trauma [1]. These injuries are often missed or there is a delay in diagnosis, which can lead to enlargement of the defect and the development of abdominal or respiratory symptoms [2,3]. We report a case of an otherwise healthy 37 year old male who was involved in a motor vehicle accident at age twelve. He presented 25 years later to us with vague lower abdominal symptoms and was found to have a large chronic left sided diaphragmatic hernia involving the majority of his intra-abdominal contents. Repair of the defect was undertaken and the patient also required complex abdominal wall reconstruction as a result. Blunt diaphragmatic injury is rare and remains a diagnostic challenge. Clinicians must have a high index of suspicion if patients have certain characteristics.
2. Presentation of case
A 37 year old man presented to our emergency department with complaints of lower left sided abdominal pain. He is an otherwise healthy man with no past medical or surgical history. He stated the pain started one day prior but he denied any nausea, vomiting, shortness of breath or fever. He is a field worker and denied any respiratory or abdominal symptoms in the past. After further questioning he did recall a motor vehicle accident when he was twelve years old, twenty-five years earlier. His vital signs on presentation were as follows: blood pressure 140/86 mmHg, heart rate 102 beats/min, respiratory rate 22 breaths/min, and oxygen saturation of 96% on room air. Laboratory findings were significant for white blood cell count 18.8. A chest X-ray followed by CT scan of the chest, abdomen and pelvis were performed which demonstrated a left sided diaphragmatic hernia with stomach, pancreas, omentum, colon, and small bowel within the left hemithorax (Fig. 1). Also noted were three left sided healed rib fractures. He was admitted to the surgical service and was taken for exploratory laparotomy which revealed a 7 cm × 10 cm defect in the left diaphragm. The hernia defect was located in the medial portion of the diaphragm abutting the GE junction. Though the majority of the intra-abdominal contents were within the chest, the GE junction remained in its usual anatomic location. Due to the size of the defect we were unable to perform a primary repair and elected to use a fetal bovine dermal biologic mesh after the reduction of contents (Fig. 2). We performed a staged abdominal wall reconstruction as the chronicity of the hernia led to loss of intra-abdominal domain. After reduction of the intrathoracic contents we were unable to primarily close the midline fascia. A Wittmann Patch was placed for serial advancement of the fascia and he was returned to the operating room for bilateral component separation, closure and reinforcement with biologic mesh (Figs. 3 and 4). Postoperatively he did have evidence of intra-abdominal hypertension and poor compliance of the abdominal wall due to loss of domain. He required prolonged mechanical ventilator support with sedation and neuromuscular blockade. He developed mild acute kidney injury which resolved and was nutritionally supported with parenteral nutrition due to distension and ileus. Ultimately he recovered well from the abdominal portion of the surgery but developed bronchiolitis obliterans organizing pneumonia (BOOP) of the left lung requiring a course of steroids.
Fig. 1.

Preoperative chest X-ray and CT scan.
Fig. 2.
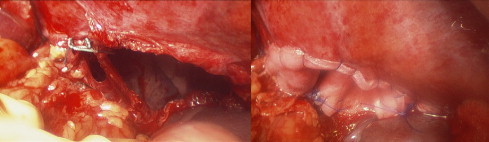
Diaphragm defect before and after repair.
Fig. 3.

Component separation and fascial closure.
Fig. 4.

Reinforcement with mesh overlay.
3. Discussion
Traumatic diaphragmatic hernia is an underappreciated injury in the acute setting and the majority of published literature is individual reported cases. Trauma accounts for approximately 0.8–8% of all diaphragmatic hernias [1]. These injuries are often missed or there is a delay in diagnosis because they are associated with other injuries, which require immediate attention; or the patient does not present with typical symptoms. If an injury goes undiagnosed, the hernia can grow in size over time but will often lead to the development of respiratory or abdominal symptoms [2–4]. As in our case, diagnosis of blunt diaphragmatic rupture can be challenging if it is initially small and the patient does not require laparotomy for an associated injury. Left sided tears are most common, as the liver tends to protect the right hemidiaphragm. The most common reported mechanism of injury is motor vehicle collisions, accounting for approximately 88% of blunt diaphragmatic injuries [5–9]. Tears in the diaphragm are usually more than ten centimeters in length, are radially orientated and occur at the weakest part of the diaphragm, the musculotendinous junction in a posterolateral location [10]. Our presented case was a defect of this size but located in a more medial position. Multiple studies have demonstrated reliable findings on computed tomography for the diagnosis of these injuries. Panda et al. demonstrated that discontinuous diaphragm sign was the most commonly identified finding occurring in 95.7% of patients, followed by thickening of the diaphragm in 66% [11]. Additional signs noted in many series include the dependent viscera sign where abdominal viscera are visualized against the posterior chest wall, and collar sign with visceral herniation with focal constriction of bowel or liver [10–12]. Reiff et al. described specific motor vehicle collision characteristics combined with patient injury patterns that are highly suggestive or diaphragmatic rupture. These included splenic injury, pelvic fracture, and high-speed accident and occupant compartment intrusion from any direction greater than 30 cm [13].
Operative closure and relocation of abdominal contents is mandatory for diaphragmatic injuries. Surgical treatment of traumatic diaphragmatic rupture includes reduction of the hernia contents, repair of the diaphragmatic defect and pleural drainage. Repair can be done through an abdominal approach, a transthoracic approach or a combination of the two depending on timing of repair and other associated injuries [3,14]. As minimally invasive techniques continue to gain popularity there is also a role for laparoscopy or thoracoscopy for the diagnosis and possible repair of these injuries when amenable [3,15]. Spann et al. evaluated the use of video-assisted thoracoscopy with laparoscopy versus with laparotomy and found the minimally invasive approach to be both safe and accurate at diagnosis [16]. Given the chronicity of our case and the degree of herniated contents we opted to start in the abdomen and enter the chest if necessary. Type of repair of the diaphragmatic defect depends on the size and ability to approximate without tension. Smaller defects can be closed primarily with nonabsorbable sutures in a continuous or interrupted fashion. Larger defects can be closed using either synthetic or biologic mesh depending on surgeon choice and presence of contamination.
4. Conclusion
Blunt diaphragmatic rupture is rare in trauma and in the absence of respiratory distress and massive visceral herniation; the diagnosis of blunt diaphragmatic injury can be difficult and often missed. Early repair is key to avoid the complications associated with herniation of intra-abdominal contents into the chest, however diagnosis can be challenging. Chronic loss of intra-abdominal domain can lead to the need for a complex abdominal wall closure. With the advent of the multi-slice helical CT scan and minimally invasive techniques, diagnosis is increasing even for the smallest of defects when evaluating for other associated injuries.
Conflicts of interest
RS declares conflict of interest not directly related to the submitted work. She receives personal fees from TEI Biosciences for lectures/speaker functions.
All other authors do not have any conflict of interest.
Sources of funding
There were no sources of funding for this case report.
Ethical approval
There was no ethics committee held for the preparation of this case report.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author’s contribution
Dr. Pakula contributed to study concept and design, and writing of the paper.
Dr. Jones helped with data collection and writing the paper.
Dr. Syed reviewed radiologic images and helped with writing the paper.
Dr. Skinner helped with study design and writing the paper.
Guarantor
Dr. Andrea Pakula accepts full responsibility for this work.
References
- 1.Hood R.M. Traumatic diaphragmatic hernia. Ann. Thorac. Surg. 1971;12:311–324. doi: 10.1016/s0003-4975(10)65131-4. [DOI] [PubMed] [Google Scholar]
- 2.Shailesh K., Santosh K., Shubhendu B., Sumit M., Priyadarshi D. An undiagnosed left sided traumatic diaphragmatic hernia presenting as small intestinal strangulation: a case report. Int. J. Surg. Case Rep. 2013;4:446–448. doi: 10.1016/j.ijscr.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rashid F., Chakrabarty M.M., Singh R., Iftikhar S.Y. A review on delayed presentation of diaphragmatic rupture. World J. Emerg. Surg. 2009;4:32. doi: 10.1186/1749-7922-4-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gali B.M., Bakari A.A., Wadinga D.W., Nganjiwa U.S. Missed diagnosis of a delayed diaphragmatic hernia as intestinal obstruction: a case report. Niger. J. Med. 2014;23:83–85. [PubMed] [Google Scholar]
- 5.Chughtai T., Ali S., Sharkey P., Lins M., Rizoli S. Update on managing diaphragmatic rupture in blunt trauma: a review of 208 consecutive cases. Can. J. Surg. 2009;52:177–181. [PMC free article] [PubMed] [Google Scholar]
- 6.Wardi G., Lasoff D., Cobb A., Hayden S. Traumatic diaphragmatic hernia. J. Emerg. Med. 2014;46(1):80–82. doi: 10.1016/j.jemermed.2013.08.032. [DOI] [PubMed] [Google Scholar]
- 7.Boulanger B.R., Milzman D.P., Rosati C. A comparison of right and left blunt traumatic diaphragmatic rupture. J. Trauma. 1993;35:255–260. doi: 10.1097/00005373-199308000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Vermillion J.M., Wilson E.B., Smith R.W. Traumatic diaphragmatic hernia presenting as a tension fecopneumothorax. Hernia. 2001;5:158–160. doi: 10.1007/s100290100022. [DOI] [PubMed] [Google Scholar]
- 9.Guth A.A., Pachter H.L., Kim U. Pitfalls in the diagnosis of blunt diaphragmatic injury. Am. J. Surg. 1995;170:5–9. doi: 10.1016/s0002-9610(99)80242-6. [DOI] [PubMed] [Google Scholar]
- 10.Scaglione M., Pinto F., Grassi R., Romano S., Giovine S., Sacco M., Forner A.L., Romano L. Diagnostic sensitivity of computerized tomography in closed trauma of the diaphragm. Radiol Med. 2000;99:46–50. [PubMed] [Google Scholar]
- 11.Panda A., Kumar A., Gamanagatti S., Patil A., Kumar S., Gupta A. Traumatic diaphragmatic injury: a review of CT signs and the difference between blunt and penetrating injury. Diagn. Interv. Radiol. 2014;20:121–128. doi: 10.5152/dir.2013.13248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bergin D., Ennis R., Keogh C. The ‘dependent viscera’ sign in CT diagnosis of blunt traumatic diaphragmatic rupture. AJR Am. J. Roentgenol. 2001;177:1137–1140. doi: 10.2214/ajr.177.5.1771137. [DOI] [PubMed] [Google Scholar]
- 13.Reiff D.A., McGwin G., Jr., Metzger J. Identifying injuries and motor vehicle collision characteristics that together are suggestive of diaphragmatic rupture. J. Trauma. 2002;53:1139–1145. doi: 10.1097/00005373-200212000-00018. [DOI] [PubMed] [Google Scholar]
- 14.DeBlasio R., Maione P., Avallone U., Rossi M., Pigna F., Napolitano C. Late posttraumatic diaphragmatic hernia. A clinical case report. Minerva Chir. 1994;49:481–487. [PubMed] [Google Scholar]
- 15.Pross M., Manger T., Mirow L., Wolff S., Lippert H. Laparoscopic management of a late-diagnosed major diaphragmatic rupture. Laparoendosc. Adv. Surg. Tech. 2000;10(2):111–114. doi: 10.1089/lap.2000.10.111. [DOI] [PubMed] [Google Scholar]
- 16.Spann J.C., Nwariaku F.E., Wait M. Evaluation of video-assisted thoracoscopic surgery in the diagnosis of diaphragmatic injuries. Am. J. Surg. 1995;170:628–631. doi: 10.1016/s0002-9610(99)80030-0. [DOI] [PubMed] [Google Scholar]


