Abstract
Objective
Although misperceptions about prognosis by surrogates in ICUs are common and influence treatment decisions, there is no validated, practical way to measure the effectiveness of prognostic communication. Surrogates' subjective ratings of quality of communication have been used in other domains as markers of effectiveness of communication. We sought to determine whether surrogates' subjective ratings of the quality of prognostic communication predicts accurate expectation about prognosis by surrogates.
Design
We performed a cross sectional cohort study. Surrogates rated the quality of prognostic communication by survey. Physicians and surrogates gave their percentage estimate of patient survival on ICU day 3 on a 0-100 probability scale. We defined discordance about prognosis as a difference in the physician's and surrogate's estimates of ≥ +/-20%. We used multi-level logistic regression modeling to account for clustering under physicians and patients and adjust for confounders.
Patients
275 patients with acute respiratory distress syndrome at high risk of death or severe functional impairment, their 546 surrogate decision makers, and their 150 physicians.
Measurements and Main Results
There was no predictive utility of surrogates' ratings of the quality of communication about prognosis to identify inaccurate expectations about prognosis. (OR 1.04 +/- 0.07, p 0.54). Surrogates' subjective ratings of the quality of communication about prognosis were high, as assessed with a variety of questions. Discordant prognostic estimates were present in 63.5% (95% CI: 59.0%-67.9%) of physician-surrogate pairs.
Conclusions
Although most surrogates rate the quality of prognostic communication highly, inaccurate expectations about prognosis are common among surrogates. Surrogates' ratings of the quality of prognostic communication do not reliably predict an accurate expectation about prognosis.
Key words for indexing: Communication; Decision making; Prognosis; Respiratory Distress Syndrome, Adult; Cohort Studies; Cross Sectional Studies
Introduction
Surrogate decision makers of critically ill patients often have inaccurate expectations about their loved one's prognosis. (1–4)This is problematic because prognostic information influences treatment decisions. Undue optimism in particular may lead to the use of invasive treatments that are inconsistent with patients' preferences. (5, 6)Misperceptions about prognosis may also leave surrogates unprepared for their loved ones' death.(7–9)
Despite the importance of effective prognostic communication, there is no practical way to assess whether a physician has effectively communicated prognostic information to a family. Audio recording is resource intensive, difficult to interpret, and not clinically practical. Directly asking surrogates to restate the information just delivered about prognosis in the conversation (e.g., a “teach back”(10)) may be interpersonally difficult for physicians and emotionally difficult for surrogates. A potentially practical and feasible way to evaluate the effectiveness of prognostic communication is to assesssurrogates' perceptions of the quality of prognostic communication. Literature suggests that for some types of communication, such ratings of quality are useful markers of actual effectiveness(11) but not in others(12–14). Thissuggests that the utility of subjective ratings of quality of communication as an actual marker of effective communication is context dependent. We are not aware of any efforts to examine if there is any predictive utility of surrogates' ratings of the quality of communication about prognosis to identify inaccurate expectations about prognosis.
We therefore conducted this analysis to determine whether simple questioning of surrogates' subjective perceptions of the quality of prognostic communication is a reliable predictor of surrogates' expectations about prognosis.
Materials and Methods
Design
We performed a secondary data analysis of a cross sectional cohort study of surrogate decision makers for critically ill patients in medical-surgical, trauma, cardiac, and neurologic ICUs of 5 U.S academic medical centered located in California, Pennsylvania, Washington, North Carolina, and Massachusetts between November 2010 and October 2012.
Participants
The cohort includes 251 patients with acute respiratory distress syndrome (ARDS), their 546 surrogate decision makers, and their 145 physicians.
Patients were eligible if they lacked decision making capacity and had respiratory failure requiring mechanical ventilation due to ARDS as defined by a PaO2:FO2 ratio less than 300 and bilateral infiltrates on chest radiography not due to left atrial hypertension. Patients had a 50% or greater risk of hospital mortality or long-term and severe functional impairment, estimated by an Acute Physiology and Chronic Health Evaluation (APACHE) II score of at least 25 or the attending physician's estimate for patients with neurologic diagnoses. We excluded patients who were awaiting organ transplantation, imminently dying, or had no surrogate available.
We enrolled family members who self-identified as being involved in surrogate decision-making for the patient. If multiple individuals identified themselves as the surrogate for a patient, we then enrolled those who rated their role in decision making to be significant. Therefore, each patient could have more than one surrogate enrolled. To be considered, surrogates needed to be at least 18 years old and speak and read English well enough to not require an interpreter.
Physicians were the treating attending physician of record or his or her designee, defined as any physician providing clinical care to the enrolled patient under the service of the attending physician. The eligible physician was approached for participation in the study prior to their participation in any study interventions.
The study coordinator at each site obtained a daily list of all ARDS patients identified through existing ARDS network screening mechanisms. The research coordinator then assessed whether the patient met enrollment criteria for the study. If so, the study investigator sought permission from the attending physician to approach the surrogate decision-maker regarding study participation. This study was approved by the University of Pittsburgh Institutional Review Board. All subjects provided written consent for all study procedures.
Predictor Variables
Patient, surrogate, and physician demographic variables were obtained via questionnaires. Surrogate trust in physicians was measured by the by the Wake Forest Trust Scale(15). Surrogate health literacy was measured by the Short Test of Functional Health Literacy in Adults (STOFHLA)(16). Surrogate numerical literacy was measured by the Lipkus score(17).
Surrogates' subjective perceptions of prognostic communication were assessed prior to the family conference on ICU day 3 by asking the following three questions: (1) “Overall, how well have the doctors communicated with you about your loved one's chances for surviving this hospitalization?” (2) “Overall, how much do you believe the information from the doctor about your loved one's chances for surviving this hospitalization?” and (3) “Overall, how satisfied are you with the doctor's bedside manner when he/she discussed your loved one's prognosis?” Subjective scales were measured on a 10 point Likert scale with 0 being “very poor” to 10 being “perfectly.”
Outcome Variables
The primary outcome measure was discordance between the physician's prognostic estimate and the surrogate's prognostic estimate of at least 20 points on a 0-100 probability scale. We assessed the surrogate's personal estimate of the patient's prognosis on ICU day 3 by asking the following question: “What do you think are the chances that your loved one will survive this hospitalization if the current plan of care stays the same?” We assessed the physician's prognostic estimate with the same question, replacing “loved one” with “patient.” All participants responded by marking on a 10cm long 0-100 probability scale, labeled on the left with “No chance of survival (0%),” on the right with “Will definitely survive (100%),” and “10%, 20%, …, 80%, and 90%” marked at every 1cm distance in between.
Statistical Analysis
Multilevel, mixed effect logistic regression modeling assessed for an association between surrogates' perceived quality of communication and discordance. Multilevel modeling was used to account for the hierarchical nature of the data where there can be multiple surrogates per patient and to describe those effects as fixed or random. Multilevel, multivariable, ordinal logistic regression modeling assessed for a trend between perceived quality of prognostic communication and surrogate prognostic estimates. Modeling controlled for demographic variables, Lipkus score, and APACHE score. All analyses were performed using STATA version 13 (Statcorp LP, College Station, TX) and two sided statistical significance was defined as a resultant P value of 0.05 or less.
Results
Characteristics of study participants
Table 1 shows the demographic characteristics of the patients, surrogates, and physicians who participated in the study. Of 546 surrogates in the original cohort, 464 completed the pre-family conference questionnaire. Because there was no physician enrolled for the patients of two surrogates, there are 462 physician-surrogate pairs available for analysis. The sample was diverse in terms of gender, religious affiliation, and level of education. Patients were admitted mostly from home, an outside hospital, or other acute care facility. At the time of enrollment, the patients had a mean APACHE II score of 32 (+/- 5). A majority of surrogates were the patient's spouse or child and had a least some college education with adequate health literacy. About half of surrogates had prior experience in medical decision-making. Responding surrogates were similar to non-responding surrogates except in their trust in physicians. Responders had higher trust in physicians than non-responders (20.8 +/-3.7 and 19.4 +/- 4.0, respectively; p=0.003).Clinicians were mostly attending physicians with an average of 8.7 years in practice.
Table 1. Characteristics of Study Participants.
| Characteristics | Surrogate (N=464) | Patient (N=251) | Clinician (N=145) | ||||
|---|---|---|---|---|---|---|---|
| Age | 49.5 | (14.0) | 58.1 | (16.6) | 38.9 | (10.1) | |
|
| |||||||
| Sex | Female | 301 | (65.7) | 115 | (45.8) | 44 | (30.3) |
| Male | 157 | (34.3) | 136 | (54.2) | 101 | (69.7) | |
|
| |||||||
| Race | White | 355 | (80.7) | 202 | (81.8) | 107 | (77.0) |
| African American | 49 | (11.1) | 30 | (12.2) | 4 | (2.9) | |
| Asian/Pacific Islander | 16 | (3.6) | 10 | (4.1) | 26 | (18.7) | |
| Native American/Alaskan Native | 3 | (0.7) | 2 | (0.8) | 0 | (0) | |
| Multiethnic | 17 | (3.9) | 3 | (1.2) | 2 | (1.4) | |
|
| |||||||
| Ethnicity | Non-Hispanic | 413 | (90.8) | 193 | (90.2) | 137 | (95.1) |
| Hispanic | 42 | (9.2) | 21 | (9.8) | 7 | (4.9) | |
|
| |||||||
| Relationship to patient | Spouse/partner | 100 | (21.9) | ||||
| Child | 165 | (36.1) | |||||
| Parent | 64 | (14.0) | |||||
| Sibling | 57 | (12.5) | |||||
| Other | 71 | (15.5) | |||||
|
| |||||||
| Level of education | High school or less | 157 | (34.4) | ||||
| Some college/college graduate | 217 | (47.5) | |||||
| Graduate school/degree | 83 | (18.2) | |||||
|
| |||||||
| Level of English comprehension | Poorly | 2 | (0.4) | ||||
| Fairly well | 10 | (2.2) | |||||
| Well | 33 | (7.2) | |||||
| Very well | 412 | (90.2) | |||||
|
| |||||||
| Lipkus et al. (2001) Numeracy Scale-Expanded, score 0-11, higher values indicating better numeracy | 6.8 | (3.2) | |||||
|
| |||||||
| Level of health literacy measured using STOFHLA: Reading Comprehension | Inadequate | 15 | (3.3) | ||||
| Marginal | 5 | (1.1) | |||||
| Adequate | 438 | (95.6) | |||||
|
| |||||||
| Religiosity (importance of religion in everyday life) | Not at all important | 35 | (7.7) | ||||
| Not too important | 66 | (14.5) | |||||
| Fairly important | 139 | (30.5) | |||||
| Very important | 216 | (47.4) | |||||
|
| |||||||
| Past experience as surrogate decision-maker | No | 236 | (52.0) | ||||
| Yes | 218 | (48.0) | |||||
|
| |||||||
| Wake Forest Trust Scale (short-form) measuring trust in physicians, score 5-25, higher values indicating more trust | 20.5 | (3.8) | |||||
|
| |||||||
| Patient prognosis estimation | 68.5 | (31.1) | 54.9 | (29.9) | |||
|
| |||||||
| APACHE II at time of questionnaire completion measuring disease severity, score 0-71, higher values indicating more severe disease and higher risk of death | 26.5 | (6.6) | |||||
|
| |||||||
| In-hospital death | 110 | (43.8) | |||||
|
| |||||||
| Staff position | Attending | 75 | (51.7) | ||||
| Fellow | 41 | (28.3) | |||||
| Resident | 27 | (18.6) | |||||
| Nurse practitioner | 2 | (1.4) | |||||
|
| |||||||
| Practice duration | 8.7 | (9.7) | |||||
Data given as mean (sd) or count (%); Percent may not add up to 100.0 due to rounding; 6 surrogates did not complete the Baseline Family Questionnaire and 1 clinician did not complete the Physician Questionnaire
Definitions of terms: STOFHLA = Short Test of Functional Health Literacy in Adults; APACHE = Acute Physiology and Chronic Health Evaluation
Surrogates perceive high quality of prognostic communication, yet discordance is common
Figure 1 shows surrogates' mean scores to the three questions that assessed the quality of prognostic communication and the percent of discordant physician-surrogate prognostic estimates. 73% (337/464) of surrogates responded to the question asking how well the doctor communicated the prognosis and rated this question at mean score of 8 (+/- 2.4). 68% (316/464) of surrogates responded to the question asking regarding belief of prognostic information and rated this question at a mean of 8.4 (+/- 2.1). 75% (347/464) responded to the question regarding satisfaction with the doctor's bedside manner and rated this question at a mean of 9 (+/- 1.9). Overall, 63.5% (95% CI: 59.0% - 67.9%) of physician-surrogate pairs had prognostic estimates that were greater than 20% different (discordant).
Figure 1.

Discordance about prognosis is common despite highly rated quality of communication.
Perceived quality of prognostic communication does not predict inaccurate expectations about prognosis
Table 2 shows the multivariate model analyzing the relationship between our predictor variables of and discordance while controlling for age, gender, numerical literacy, minority status, APACHE score, and surrogate relationship. In this model, there was no predictive utility of the three candidate questions assessing perceived quality of prognostic communication to identify discordance, neither individually nor when placed in the model in combination (p= 0.661). A summary score that combines the scores from the individual questions and takes the average was also not predictive of discordance after controlling for the same variables (OR=1.01; p=0.857). This multivariate analysis also shows that as surrogates' numerical literacy increases, discordance decreases and as patients' severity of illness increases (OR=0.89, p=0.026), discordance increases (OR=1.06, p=0.013).Figure 2 shows additional analysis performed with a receiver operator curve which shows surrogates' quality ratings of the communication about prognosis predict accurate expectations about prognosis no better than chance (AUC=0.4481).
Table 2.
Multivariate analysis shows no association between surrogates' quality of communication ratings and inaccurate expectations about prognosis (n=276).
| Variables | Odds Ratio | P Value | 95% Confidence Interval |
|---|---|---|---|
| Believability of physician prognostication | 1.05 | 0.568 | 0.89 to 1.25 |
| Satisfaction with physician bedside manner | 1.06 | 0.620 | 0.84 to 1.35 |
| Perceived quality of prognostic communication | 1.02 | 0.831 | 0.85 to 1.23 |
|
|
|||
| Combine significance of all predictors of interest | 0.661 | ||
| APACHE II scorea | 1.06 | 0.013 | 1.01 to 1.12 |
| Lipkuset al. numeracyscorea | 0.89 | 0.026 | 0.80 to 0.99 |
| Spousal relationship with the patientb | 1.73 | 0.170 | 0.79 to 3.77 |
| Racial minority | 1.33 | 0.480 | 0.60 to 2.95 |
| Malec | 1.19 | 0.587 | 0.64 to 2.20 |
| Age in yearsa | 1.00 | 0.708 | 0.97 to 1.02 |
For every 1-unit increase;
vs. other types of relationship;
vs. female
Definitions of terms: APACHE = Acute Physiology and Chronic Health Evaluation; Racial minority = race/ethic group other than non-Hispanic white (i.e. blacks, Asians, Hispanic whites, Native Americans, etc.)
Figure 2.
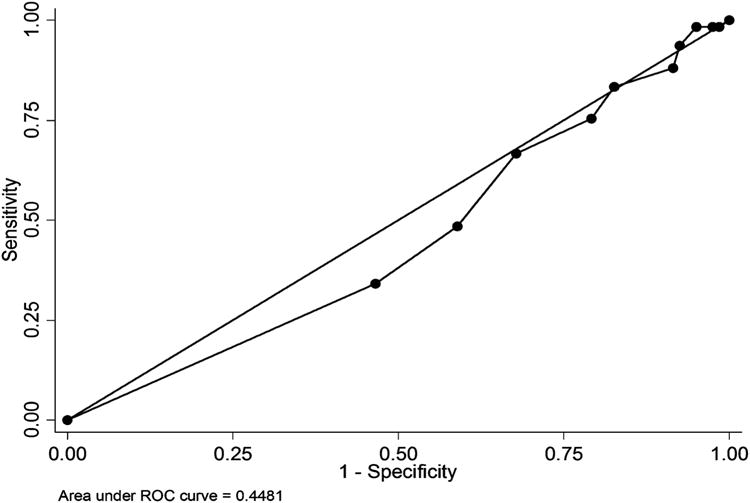
Analysis using receiver operator curve shows surrogates' communication quality ratings predict accurate expectations about prognosis no better than chance.
Surrogates who rate quality of communication the highest are also the most optimistic
Figure 3 shows the ratings of prognostic communication across three groups of surrogates: those with pessimistic estimates relative to physicians (13.5%), estimates concordant with physicians (36.5%), and optimistic estimates relative to physicians (50%). Surrogates who held more optimistic prognostic estimates relative to the physician tended to also ratethe quality of prognostic communication higher.
Figure 3.

Surrogates who rate quality of communication the highest are also the most optimistic.
Discussion
We found that although most surrogates positively evaluated physicians' prognostic communication, their prognostic expectations were discordant with physicians, typically being overly optimistic. Surrogates' ratings of the quality of prognostic communication do not reliably predict prognostic concordance with their physician.
We are not aware of other studies that address whether surrogate decision makers' subjective ratings of communication predict accurate expectations about prognosis by surrogates. However, several studies of the informed consent process reveal that participants often report high subjective quality of communication, but misunderstand key information central to truly informed consent.(18–22) For example, in one randomized controlled trial of 29 patients evaluating an intervention to improve informed consent comprehension, all participants were all highly satisfied with the consent process yet the percent of information understood in the control group was 39%.(18)Our study adds to this literature by showing that in the context of critical illness and surrogate decision making, subjective quality ratings about communication are not a reliable marker for effective communication about prognosis.
We also found surrogates' with higher quality of communication scores tend to hold overly optimistic prognostic estimates, which raises the possibility that surrogates' ratings of the quality of communication may actually worsen as they more clearly understand the patient's prognosis. Although no other studies have assessed this among surrogates, Weeks et al found a similar occurrence in a study of 1193 patients' expectations about effects of chemotherapy for advanced cancer.(23) They found that patients who reported higher scores for physician communication were also at higher risk for inaccurate expectations. This finding further strengthens the argument that subjective quality ratings are not likely to be useful proxies for effective communication about prognosis.
The study has two main strengths. First,we enrolled a large, diverse cohort, which enhances the study's generalizability. Second, we used multiple methods to assess our main result. We used both a model to calculate the predictive value of each individual question about prognostic communication as well as a composite score that combines the ratings of all three questions. We also used an ROC curve to examine the predictive accuracy. The fact that each analytic approach yielded qualitatively similar results lends support to our main finding.
Our study has several limitations. Although it is the largest study of its kind, there was not adequate power to meaningfully conduct subgroup analyses to examine whether the utility of the quality ratings varied across age or racial groups. Similarly, although our sample population was diverse, some groups for whom discussions of prognosis hold particular concern, such as Navajo Indians(24), were underrepresented. Finally, our study was conducted in the ICU environment and we cannot exclude the possibility that in other clinical contexts these types of quality ratings may be a reliable marker for effective communication.
The clinical implication of our finding is that surrogates' perceptions about the quality of prognostic communication do not reliably predict prognostic concordance with their physician. The “teach back” method(10) is an evidence based tool clinicians use to assess accurate understanding of information. A large body of research shows this technique is well liked by patients and is an effective way to assess for misunderstandings.(25–28) Because surrogates may experience emotional discomfort when verbalizing their loved one's poor prognosis, clinicians may consider a modified version of the “teach back” method where the surrogate is asked to verbalize what they are going to tell other family members about their loved one's prognosis. For example, rather than saying, “can you please tell me what I just told you about your father's prognosis”, clinicians could say, “We've talked about a lot of complicated medical things and I imagine you are going to talk with other family/friends about this after our meetings. What are you going to tell them about what the future might hold for your father?”
Conclusion
Surrogates' perceptions about the quality of prognostic communication do not reliably predict prognostic concordance with their physician. Future research is needed to develop and empirically test an approach that will promote shared understanding between physicians and surrogates regarding prognostic information.
Acknowledgments
Supported by: National Institutes of Health National Heart, Lung, and Blood Institute grant 5R01HL094553-02
Copyright form disclosures: Drs. Chiarchiaro, Buddadhumaruk, and White received support for article research from the National Institutes of Health (NIH) (5R01HL094553). Dr. Arnold received royalties from Cambridge University and JHU University, served as a board member, and received support for article research from the NIH (5R01HL094553). His institution received grant support from, consulted for, and lectured for the University of Pittsburgh. His institution received grant support from the JHF Foundation and AV Davis Foundations.
References
- 1.Covinsky KE, Fuller JD, Yaffe K, et al. Communication and decision-making in seriously ill patients: findings of the SUPPORT project.The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc. 2000;48:S187–93. doi: 10.1111/j.1532-5415.2000.tb03131.x. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez RM, Navarrete E, Schwaber J, et al. A prospective study of primary surrogate decision makers' knowledge of intensive care. Crit Care Med. 2008;36:1633–6. doi: 10.1097/CCM.0b013e31816a0784. [DOI] [PubMed] [Google Scholar]
- 3.Azoulay E, Chevret S, Leleu G, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med. 2000;28:3044–3049. doi: 10.1097/00003246-200008000-00061. [DOI] [PubMed] [Google Scholar]
- 4.Cox CE, Martinu T, Sathy SJ, et al. Expectations and outcomes of prolonged mechanical ventilation. Crit Care Med. 2009;37:2888–94. doi: 10.1097/CCM.0b013e3181ab86ed. quiz 2904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy DJ, Burrows D, Santilli S, et al. The influence of the probability of survival on patients' preferences regarding cardiopulmonary resuscitation. N Engl J Med. 1994;330:545–549. doi: 10.1056/NEJM199402243300807. [DOI] [PubMed] [Google Scholar]
- 6.Lloyd CB, Nietert PJ, Silvestri GA. Intensive care decision making in the seriously ill and elderly. Crit Care Med. 2004;32:649–654. doi: 10.1097/01.ccm.0000115636.29294.2f. [DOI] [PubMed] [Google Scholar]
- 7.Weeks JC, Cook EF, O'Day SJ, et al. Relationship between cancer patients' predictions of prognosis and their treatment preferences. JAMA. 1998;279:1709–1714. doi: 10.1001/jama.279.21.1709. [DOI] [PubMed] [Google Scholar]
- 8.Fried TR, Bradley EH, Towle VR, et al. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346:1061–1066. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]
- 9.Apatira L, Boyd EA, Malvar G, et al. Hope, truth, and preparing for death: perspectives of surrogate decision makers. Ann Intern Med. 2008;149:861–868. doi: 10.7326/0003-4819-149-12-200812160-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Care H. “What Did the Doctor Say?:” Improving Health Literacy to Protect Patient Safety Another in the series of Health Care. Jt Comm Public Policy Initiat. 2007 [Google Scholar]
- 11.Jha AK, Orav EJ, Zheng J, et al. Patients' perception of hospital care in the United States. N Engl J Med. 2008;359:1921–1931. doi: 10.1056/NEJMsa0804116. [DOI] [PubMed] [Google Scholar]
- 12.Chang JT, Hays RD, Shekelle PG, et al. Patients' global ratings of their health care are not associated with the technical quality of their care. Ann Intern Med. 2006;144:665–672. doi: 10.7326/0003-4819-144-9-200605020-00010. [DOI] [PubMed] [Google Scholar]
- 13.Sequist TD, Schneider EC, Anastario M, et al. Quality monitoring of physicians: linking patients' experiences of care to clinical quality and outcomes. J Gen Intern Med. 2008;23:1784–1790. doi: 10.1007/s11606-008-0760-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schneider EC, Zaslavsky AM, Landon BE, et al. National quality monitoring of Medicare health plans: the relationship between enrollees' reports and the quality of clinical care. Med Care. 2001;39:1313–1325. doi: 10.1097/00005650-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Dugan E, Trachtenberg F, Hall MA. Development of abbreviated measures to assess patient trust in a physician, a health insurer, and the medical profession. BMC Health Serv Res. 2005;5:64. doi: 10.1186/1472-6963-5-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baker DW, Williams MV, Parker RM, et al. Development of a brief test to measure functional health literacy. Patient Education and Counseling. 1999:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 17.Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 18.Bickmore TW, Pfeifer LM, Paasche-Orlow MK. Using computer agents to explain medical documents to patients with low health literacy. Patient Educ Couns. 2009;75:315–20. doi: 10.1016/j.pec.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davis TC, Holcombe RF, Berkel HJ, et al. Informed consent for clinical trials: a comparative study of standard versus simplified forms. J Natl Cancer Inst. 1998;90:668–74. doi: 10.1093/jnci/90.9.668. [DOI] [PubMed] [Google Scholar]
- 20.Karunaratne AS, Korenman SG, Thomas SL, et al. Improving communication when seeking informed consent: a randomised controlled study of a computer-based method for providing information to prospective clinical trial participants. Med J Aust. 2010;192:388–92. doi: 10.5694/j.1326-5377.2010.tb03561.x. [DOI] [PubMed] [Google Scholar]
- 21.Tait AR, Voepel-Lewis T, Zikmund-Fisher BJ, et al. The effect of format on parents' understanding of the risks and benefits of clinical research: a comparison between text, tables, and graphics. J Health Commun. 2010;15:487–501. doi: 10.1080/10810730.2010.492560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aaronson NK, Visser-Pol E, Leenhouts GH, et al. Telephone-based nursing intervention improves the effectiveness of the informed consent process in cancer clinical trials. 1996 doi: 10.1200/JCO.1996.14.3.984. [DOI] [PubMed] [Google Scholar]
- 23.Weeks JC, Catalano PJ, Cronin A, et al. Patients' Expectations about Effects of Chemotherapy for Advanced Cancer. N Engl J Med. 2012;367:1616–1625. doi: 10.1056/NEJMoa1204410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carrese JA, Rhodes LA. Western bioethics on the Navajo reservation. Benefit or harm? JAMA. 1995;274:826–9. [PubMed] [Google Scholar]
- 25.White M, Garbez R, Carroll M, et al. Is “teach-back” associated with knowledge retention and hospital readmission in hospitalized heart failure patients? J Cardiovasc Nurs. 28:137–46. doi: 10.1097/JCN.0b013e31824987bd. [DOI] [PubMed] [Google Scholar]
- 26.Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163:83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 27.Burkhart JA. Training nurses to be teachers. J Contin Educ Nurs. 2008;39:503–10. doi: 10.3928/00220124-20081101-02. [DOI] [PubMed] [Google Scholar]
- 28.Kemp EC, Floyd MR, McCord-Duncan E, et al. Patients prefer the method of “tell back-collaborative inquiry” to assess understanding of medical information. J Am Board Fam Med. 21:24–30. doi: 10.3122/jabfm.2008.01.070093. [DOI] [PubMed] [Google Scholar]


