Abstract
Introduction
This study evaluated service-learning program’s impact on senior dental students’ attitude toward community service at Virginia Commonwealth University (VCU) School of Dentistry. Experience gained through service-learning in dental school may positively impact dental students’ attitude toward community service that will eventually lead into providing care to the underserved.
Materials and methods
Two surveys (pre and post-test) were administered to 105 senior dental students. For the first survey (post-test), seventy six students out of 105 responded and reported their attitude toward community service immediately after the service-learning program completion. Three weeks later, fifty six students out of the 76 responded to the second survey (retrospective pre-test) and reported their recalled attitude prior to the program retrospectively.
Results
A repeated-measure mixed-model analysis indicated that overall there was improvement between pre-test and post-test. Scales of connectedness, normative helping behavior, benefits1, career benefits, and intention showed a significant pre-test and post-test difference. An association between attitude toward community service and student characteristics such as age, gender, ethnicity, and volunteer activity was also examined. Only ethnicity showed an overall significant difference. White dental students appear to have a differing perception of the costs of community service.
Conclusions
The service-learning program at VCU School of Dentistry has positively impacted senior dental students’ attitude toward community service.
Keywords: Service-learning, attitude, community-based dental education
Introduction
Oral Health in America, the U.S. Surgeon General’s report in 2000, raised concerns about oral health disparities in the U.S. Certain segments of the population, such as the elderly, very young children, the poor, and people who are medically compromised, face significant barriers to access oral health care and are much more likely to have poorer oral health (1). An oral health workforce who are appropriately trained and willing to treat these vulnerable populations can help alleviate the barrier to access to care and eventually reduce oral health disparities. Dentists’ willingness to treat the underserved and their behavior can be shaped during dental school (2–6). More exposure and experience in providing care to the underserved, especially in community settings other than dental school (A.K.A. community-based dental education), can greatly improve dental students’ awareness of community needs, attitude toward community service, and willingness to provide care to those in need as part of the community service. The level of preparedness during dental school affects not only providers’ attitude for caring for the underserved but also their actual intention and behavior (2).
Service-learning, a form of community-based education, is a structured learning activity where community service and academic objectives are pursued concurrently. Balance between service and learning, integral involvement of community partners, and emphasis on reflection are important factors in service-learning (7–11). Service-learning activities establish a reciprocal relationship between community partners and campus instructors. In successful service-learning activities campus instructors ensure that the service experience is consistent with the course goals and objectives while community partners ensure that student activities are consistent with their goals and needs (12).
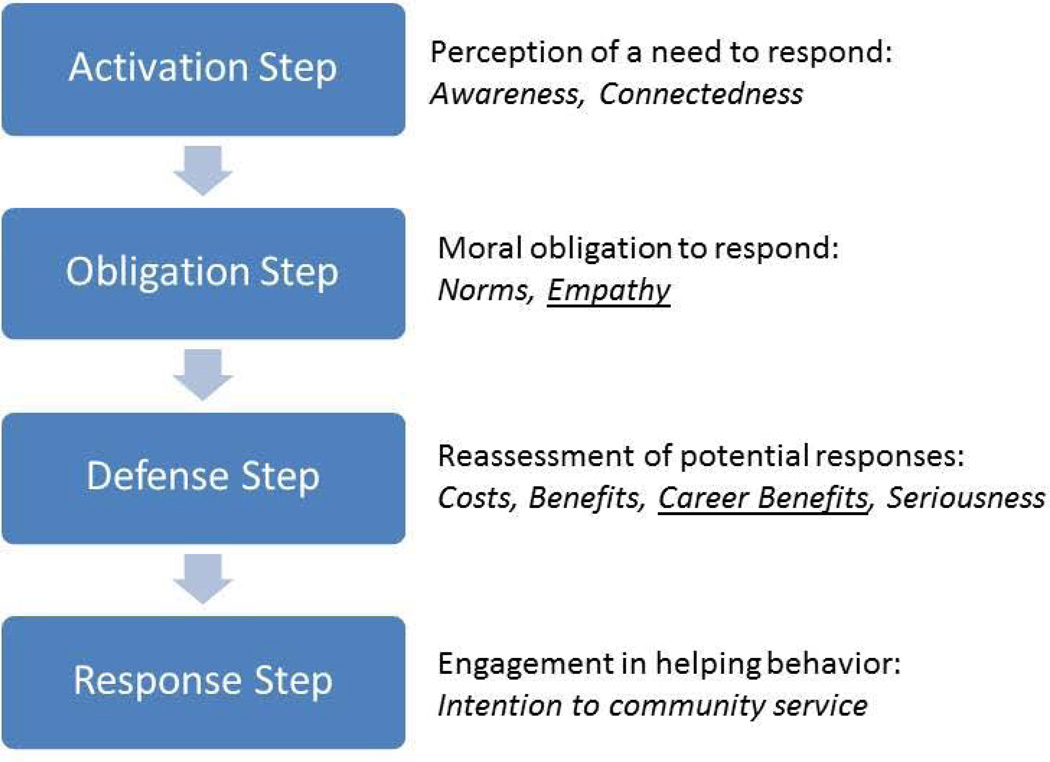
When examining relationships between service-learning and students’ helping behavior/attitude to help, Schwartz’s model is adopted as a theoretical foundation in this study. The model has four steps (Figure 1) (13,14). In Step I: Activation, potential volunteers perceive a need to respond in the form of awareness of the need and feeling connected to the people in need. In Step II: Obligation, they feel a moral obligation to respond to the need through a personal and situational norm and empathy. In Step III: Defense, they reconsider costs and benefits of helping then reassess the situation and become serious of the need to respond. In Step IV: Response, they develop intention to engage in the community service.
Figure 1.
Schwartz’s Model of Helping Behavior and CSAS (Community Service Attitudes Scale) Source: adapted and modified from Shiarella AH. Development and construct validity of scores on the community service attitudes scale. Educational and psychological measurement. 2000; 60(2):287.
Note:
1. Empathy (underlined) exists in Schwartz’s model but was excluded in CSAS.
2. Career Benefits (underlined) was added to CSAS.
Service-learning’s conceptual foundation can be traced back to John Dewey (1859–1952) who believed that education should be concerned with developing students’ commitment and ability to contribute to society. Dewey also emphasized the importance of reflection (15,16). In 1995, the Health Professions Schools in Service to the Nation (HPSISN) initiated movement toward adopting this innovative educational method of service-learning in health care professional schools (17). Over the past fifteen years, more dental schools, especially those funded initially by the Robert Wood Johnson Foundation’s Pipeline program in 2001, started implementing service-learning in order to fulfill the profession’s obligation to meet the public’s oral healthcare needs (18). Service-learning is also intended to help students “internalize” their role as a healthcare provider in the context of a community and bring community engagement and educational objectives together (19,20).
There are many benefits of community service-learning. Community-based dental education using service-learning prepares students in cultural awareness, social responsibility, and communication skills (6,21). Potentially it can affect dental students’ values and behaviors to caring for the underserved in the community (6). Yoder stated that service-learning will create “a deeper understanding of the dynamics, the assets, and the challenges of the community and its relationship to oral and general health” (22).
The VCU School of Dentistry’s community-based service-learning program began in 2003–2004. In 2012, it became a required formal stand-alone course for senior dental students where they were assigned to rotate through a set of twelve different external sites, spending an average of 25 days throughout their senior year. At the time of this writing, VCU’s current curriculum does not afford any other formal community service-learning course for the first to third year dental students. Students’ service-learning is assessed and reinforced by self-reflection such as journal entries, blogging, and self-evaluation.
One of the objectives of service-learning is to improve students’ attitude toward community service so that they continue to volunteer to meet community needs after graduation. While there is limited data directly related to service-learning as an educational method and its impact on dental students’ attitude toward community service, several articles reported improved attitude, value, or intention to help the underserved after community-based dental education programs (2,23–25) which may or may not have adopted service-learning (emphasizing balance between service and learning and self-reflection) as an educational method. Brondani stated self-reflection may positively impact students’ attitude about service and community (26). Holtzman and Seirawan assessed impact of community-based oral health experiences on first year dental students’ attitudes toward caring for the underserved and did not find improvement in attitude toward community service after participating in the program (4). The purpose of this study was to evaluate the service-learning program at VCU School of Dentistry in the academic year 2011–2012 and to examine how the service-learning program has impacted senior dental students’ attitude toward community service. Association between students’ characteristics and attitude toward community service was also assessed.
Materials and methods
Study setting and data collection
This study describes community service attitude change of the VCU School of Dentistry class of 2012 (seniors) who were enrolled in Clinical Service-Learning course. The total class size was 105 including five students in the International Dentists Program (IDP) who joined the class of 2012 in their junior year. The questionnaire was a web-based sixty-question survey modified from the Community Service Attitudes Scales (CSAS) (27). Two surveys (pre and post-test) were sent to the 105 senior dental students. Seventy-six students responded to the first survey and 56 out of the 76 responded to both surveys: the post-test response rate was 72% and the pre-test response rate was 74%. The first survey (post-test) asked the students to report their attitude toward community service immediately after the service-learning program completion. Three weeks later, the second survey (retrospective pre-test) was sent only to the first survey respondents to report their attitude prior to the program retrospectively.
The CSAS was developed to measure college students’ attitude toward community service based on Schwartz’s model of helping behavior (27). CSAS scales and descriptions used in this study are available in Appendix A. This survey had forty six items assessing community service attitudes in eight scales: awareness, connectedness, normative helping behavior, costs, benefits, career benefits, seriousness, and intention to community service. These eight scales are consistent with scales in Schwartz’s model with slight differences (Figure 1).
Based on the factor analysis, CSAS was modified from Schwartz’s model to exclude empathy and add career benefits. Operational definitions of the CSAS scales are below.
Awareness is a measure of survey respondent’s perceived awareness to community needs.
Connectedness is a measure of survey respondent’s perceived connectedness to his or her community.
Normative helping behavior is a measure of survey respondent’s perceived personal or situational moral obligation to help his or her community.
Costs is a measure of survey respondent’s perceived costs in exchange for helping his or her community.
Benefits is a measure of survey respondent’s perceived benefits in exchange for helping his or her community.
Career benefits is a measure of survey respondent’s perceived benefits related to his or her career in exchange for helping his or her community.
Seriousness is a measure of survey respondent’s seriousness to help his or her community after considering costs and benefits.
Intentions to community service is a measure of survey respondent’s intention to help his or her community.
See Appendix A for the questions corresponding to each scale.
Two parallel questionnaires were developed for the pre-test and post-test. This study was approved by the VCU School of Dentistry Office of Research Subjects Protection. The data were collected during the months of March and April 2012 immediately following the completion of the service-learning rotations.
Questionnaire and scale
In the introduction of the questionnaire “community service” was defined as “a regular activity to meet community needs where one uses his or her skills in dentistry.” Questions measuring eight CSAS scales were distributed in the questionnaire in the same order as Shiarella et al.’s instrument. Questions 1 to 12 used seven point anchor scales of extremely likely: being 7, quite likely, slightly likely, neither likely nor unlikely, slightly unlikely, quite unlikely, and extremely unlikely: being 1 while questions 13 through 46 used seven point anchor scales of strongly agree: being 7, agree, slightly agree, neither agree nor disagree, slightly disagree, disagree, and strongly disagree: being 1. The rest of the questionnaire asked about demographics and student characteristics such as age, gender, ethnicity, volunteer activities, and whether or not being in the International Dentists Program.
Post-then-Retrospective Pre-test (RPT)
This study adopted the retrospective pre-test method where the post-test was followed by a separate pre-test. Although RPT may not have been commonly used in evaluating programs in dental education literature, RPT has been advocated to replace the traditional pre/post-test as a practical and valid way to evaluate programs in social sciences especially in educational program evaluation (28,29,29). The RPT is recommended especially when the goal of the evaluation is to assess students’ self-perception of change and reflection on personal growth related to the program is desired which was indicated in our study. Another advantage of the RPT is that it is known to reduce response-shift bias (common confounder of the traditional pre/post-test analysis) because survey respondents’ internal standard is not shifted by the program of interest itself (same criteria are used to rate pre- and post-test ratings) (26). The RPT can be used to establish a baseline when the pre-test result was not available (30). A potential criticism is the possibility of overestimating a program’s effect and recall bias of previous attitude or feelings (31,32).
RPT is found in a number of published studies in dental education (6) and other disciplines (29,33). Rubin et al. used RPT to measure dental students’ perceptions of cultural competence and social responsibility because RPT is known to reduce response-shift bias and better suited to measure subjective assessment. Skeff et al. evaluated a medical faculty development program using traditional pre/post and RPT and concluded that RPT revealed more significant changes in teaching performance and attitudes than traditional pre/post test. RPT results were also more consistent with house staff and student evaluations (33). Pelfrey and Pelfrey evaluated a Homeland Security Program using RPT to reduce a response-shift bias and concluded that “these data support the use of this innovative evaluation approach in the development of any discipline” (29). Because the present study’s interest was to describe service-learning’s impact as program participants experienced and subjectively reflected on using self-ratings, the RPT was deemed more suitable than the traditional pre-test.
In this study’s pre-test, to prompt survey respondents to reflect on their attitude before the service-learning program, the following instruction was given in the beginning of the pre-test.
“Now, pretend you are going to volunteer for a community service project sometime in the next year. Questions below ask you about possible outcomes of volunteering. Use the following scale to rate how likely you FELT or WOULD’VE FELT these outcomes are to occur BEFORE your service-learning rotations.”
Except this introductory paragraph, the post-test and RPT were parallel in attitude question items (Appendix B).
Statistical analysis
Descriptive statistics were obtained for all study variables. Outcome variables were pre-test and post-test attitude scores for all eight scales per student (respondents were tracked). Independent variables were age, gender, ethnicity, volunteering prior to dental school, volunteering during dental school, and two occasions (pre-test and post-test). The pre- versus post-test change across the eight scales was tested using a repeated-measures mixed-model ANOVA which accounted for the dependencies between the eight scales and across the two occasions as well as missing data points.
The following demographic characteristics were tested for differences on the post-test means: gender, ethnicity, age, and previous and present volunteer experience. Age was a continuous variable while all other variables were categorical variables. Ethnicity was categorized to White and non-White because the other specific race/ethnicity categories had small sample sizes. To test for differences by demographics, a repeated-measures mixed-model was used. The model included scale as an effect to account for the dependence between the scales and fixed effects for each of the demographic factors to test for the significance of that factor across all eight scales.
Results
The demographic characteristics of the respondents are summarized in Table 1. Out of 76 respondents, 33 (43%) were female and 43 (57%) were male. The average age of the respondents was 28.1 years and the age ranged from 25 to 38. Self-identified ethnicity was predominantly White: 53 of 76 (70%). Five students identified themselves to belong to the IDP. The distribution of age and gender for survey respondents was similar to that of the entire class (105 students who were invited) (P>0.05). For the entire class, 37% were female and 63% were male with the average age of 28.4 for the entire group.
Table 1.
Characteristics of the Post-test Respondents (N=76)
| Characteristic | Post-test Respondents (%) |
|---|---|
| Female | 33 (43%) |
| Male | 43 (57%) |
| White | 53 (70%) |
| Black | 2 (3%) |
| Hispanic | 1 (1%) |
| American Indian | 0 (0%) |
| Asian | 20 (26%) |
| no | 71 (93%) |
| yes | 5 (7%) |
| ≤ 25 | 10 (13%) |
| 26–29 | 46 (61%) |
| ≥ 30 | 19 (25%) |
| Regularly | 36 (47%) |
| Occasionally | 38 (50%) |
| No | 2 (3%) |
| Regularly | 22 (29%) |
| Occasionally | 48 (63%) |
| No | 6 (8%) |
Note: Questions regarding these characteristics were included only in the post-test.
When comparing those who completed both pre-test and post-test (n=56) to those who only completed the post-test (n=20), there was no significant difference in gender, age, or ethnicity (P > 0.3).
Forty seven percent (n=36) of the post-test respondents reported regular community or volunteer work prior to dental school while only 29% (n=22) of the post-test respondents regularly participated in volunteer community service activity (not assigned) outside the dental school curriculum during dental school. The percentages of those who volunteer occasionally was 50% (n=38) prior to dental school and 63% (n=48) during dental school. The percentage of regular volunteers decreased during dental school compared to prior to dental school. Only two respondents reported no volunteer work prior to dental school and only six respondents reported no participation in volunteer work during dental school.
Service-learning’s impact on students’ attitude change (pre-test and post-test)
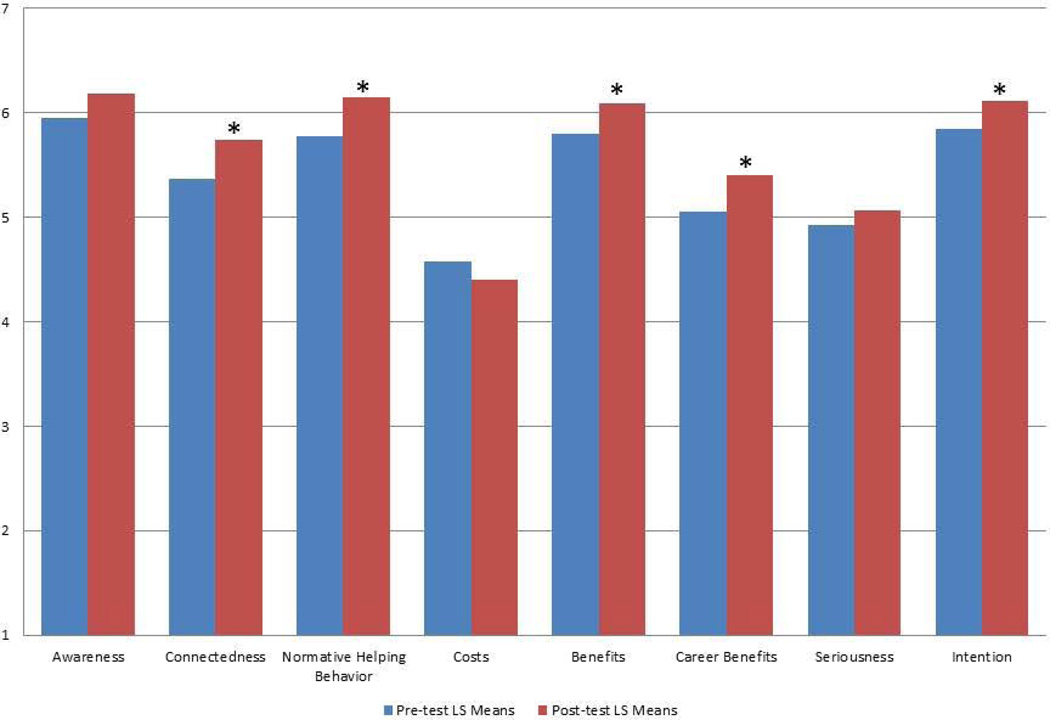
The repeated-measures mixed-model ANOVA using 56 responses (matched pre- and post-test) indicated the least-squared means (LS mean) for each occasion and the change score are summarized in Table 2. Overall, there was a change across the two occasions (p < 0.0001) in considering all variables simultaneously. The p-values in Table 2 show the test result for each of the eight scales. For example, awareness had a pre-test mean of 5.9 and it nominally increased to 6.2, a non-significant change of 0.23 (p = 0.0514). There were significant changes in connectedness, normative helping behaviors, benefits, career benefits, and intention but no evidence for a change in costs and seriousness. Figure 2 visually shows these findings. A possibility of only selected scales changing across time was tested using time*scale interaction. The p-value for time*scale interaction was 0.065 indicating there was not sufficient evidence that there was different amount of changes across scale: service-learning program’s impact did not depend on scale. All scales have changed after the service-learning.
Table 2.
Changes between Pre-test and Post-test
| Occasion | LS Mean | SE | 95% Confidence Interval | p-value | ||
|---|---|---|---|---|---|---|
|
Awareness | ||||||
| Pre-test | 5.954 | 0.096 | 5.766 | 6.142 | ||
| Post-test | 6.184 | 0.087 | 6.012 | 6.355 | ||
| Difference | 0.230 | 0.118 | −0.001 | 0.461 | 0.0514 | |
|
Connectedness | ||||||
| Pre-test | 5.363 | 0.130 | 5.108 | 5.618 | ||
| Post-test | 5.736 | 0.120 | 5.501 | 5.972 | ||
| Difference | 0.373 | 0.121 | 0.135 | 0.612 | 0.0022* | |
|
Normative Helping
Behavior | ||||||
| Pre-test | 5.775 | 0.094 | 5.590 | 5.960 | ||
| Post-test | 6.149 | 0.089 | 5.975 | 6.323 | ||
| Difference | 0.374 | 0.115 | 0.147 | 0.601 | 0.0013* | |
|
Costs | ||||||
| Pre-test | 4.573 | 0.148 | 4.283 | 4.864 | ||
| Post-test | 4.407 | 0.135 | 4.141 | 4.672 | ||
| Difference | −0.167 | 0.126 | −0.415 | 0.082 | 0.1875 | |
|
Benefits | ||||||
| Pre-test | 5.799 | 0.119 | 5.566 | 6.033 | ||
| Post-test | 6.086 | 0.107 | 5.875 | 6.296 | ||
| Difference | 0.286 | 0.122 | 0.046 | 0.526 | 0.0195* | |
|
Career Benefits | ||||||
| Pre-test | 5.057 | 0.135 | 4.792 | 5.323 | ||
| Post-test | 5.408 | 0.123 | 5.167 | 5.649 | ||
| Difference | 0.351 | 0.124 | 0.106 | 0.595 | 0.0050* | |
|
Seriousness | ||||||
| Pre-test | 4.931 | 0.140 | 4.657 | 5.205 | ||
| Post-test | 5.064 | 0.129 | 4.810 | 5.318 | ||
| Difference | 0.133 | 0.123 | −0.109 | 0.375 | 0.2810 | |
|
Intention | ||||||
| Pre-test | 5.849 | 0.106 | 5.640 | 6.058 | ||
| Post-test | 6.110 | 0.093 | 5.926 | 6.293 | ||
| Difference | 0.261 | 0.122 | 0.021 | 0.500 | 0.0328* | |
denotes p-value less than 0.05
Figure 2.
Pre-test and Post-test Change (Note: 1. * denotes pre-test and post-test changes with p-value less than 0.05 2. For scales of costs, benefits, and career benefits, the vertical axis numbers correspond to anchor scales as follows. 7: Extremely likely, 6:Quite likely, 5:Slightly likely, 4:Neither likely nor unlikely, 3:Slightly unlikely, 2:Quite unlikely, 1:Extremely unlikely 3. For all other scales, the vertical axis numbers correspond to anchor scales as follows. 7: Strongly agree, 6:Agree, 5:Slightly agree, 4:Neither agree nor disagree, 3:Slightly disagree, 2:Disagree, 1:Strongly disagree).
Association between student characteristics and post-test attitude
The repeated-measures mixed-model analysis to test differences by demographics revealed that with the exception of ethnicity demographic characteristics were not statistically significantly associated with any of the scales (p=0.0454). The comparisons between White and others are shown in Table 3. The p-values in Table 3 are not corrected for multiple comparisons due to the limited sample size but they do indicate that White dental students seem to have a differing perception of the costs of community service compared to non-White students.
Table 3.
Attitude Differences between White and non-White Respondents
| Race | n | Mean | SD | 95% Confidence Interval | p-value | |
|---|---|---|---|---|---|---|
|
Awareness | ||||||
| other | 23 | 6.06 | 0.67 | 5.77 | 6.35 | 0.246 |
| White | 53 | 6.24 | 0.57 | 6.08 | 6.39 | |
|
Connectedness | ||||||
| other | 23 | 5.68 | 0.94 | 5.28 | 6.09 | 0.749 |
| White | 53 | 5.76 | 0.93 | 5.50 | 6.02 | |
|
Normative Helping
Behavior | ||||||
| other | 23 | 6.06 | 0.58 | 5.81 | 6.31 | 0.326 |
| White | 53 | 6.19 | 0.51 | 6.05 | 6.33 | |
|
Costs | ||||||
| other | 23 | 3.84 | 1.18 | 3.33 | 4.35 | 0.003* |
| White | 53 | 4.65 | 1.01 | 4.37 | 4.93 | |
|
Benefits | ||||||
| other | 23 | 6.05 | 1.20 | 5.54 | 6.57 | 0.845 |
| White | 53 | 6.10 | 0.76 | 5.89 | 6.31 | |
|
Career Benefits | ||||||
| other | 23 | 5.70 | 1.07 | 5.23 | 6.16 | 0.082 |
| White | 53 | 5.28 | 0.87 | 5.04 | 5.52 | |
|
Seriousness | ||||||
| other | 23 | 5.13 | 1.36 | 4.55 | 5.72 | 0.711 |
| White | 53 | 5.03 | 0.91 | 4.78 | 5.28 | |
|
Intention | ||||||
| other | 23 | 5.93 | 0.67 | 5.64 | 6.22 | 0.147 |
| White | 53 | 6.19 | 0.73 | 5.99 | 6.39 | |
denotes p-value less than 0.05
Discussion
This study has provided information about the VCU School of Dentistry service-learning program’s impact on senior dental students’ attitude toward community service and the relationship between dental students’ characteristics and their attitude toward community service. To date, there have been limited published studies which have examined service-learning programs’ impact on senior dental students’ attitude toward community service using a validated scale. In healthcare professional education, one study found physical therapy students’ attitude toward older adults positively changed after service-learning (34), while there is ample evidence of service-learning’s positive impact on college students’ attitude towards service and social responsibility (35).
Several advantages of using the CSAS became evident during the process of determining whether a new survey instrument needed to be developed or a previously developed instrument could be adapted for the study. First of all, the CSAS is based on a conceptual framework of Schwartz’s helping behavior. Schwartz’s helping behavior model has been widely accepted and used to explain the cognitive and affective steps of changing behavior in a series of progressive steps from perception or awareness of needs to the intention to perform the actual helping behavior. Shiarella et al. developed questionnaire items corresponding to the Schwartz model’s sequential steps, tested those items, and conducted a factor analysis to develop the eight CSAS scales that includes 46 items (27). A separate analysis to examine CSAS’s applicability to dental education is planned for the present study once further data collection is completed. As part of this effort, only minimal modifications to Shiarella et al.’s original CSAS instrument were necessary.
In the repeated-measure mixed-model ANOVA, the overall F test was significant (p<0.0001) indicating that there was a change between pre and post-test. While LS means for all eight scales improved between pre and post-test, after adjusting for the scales effect, five scales showed statistically significant levels of change: connectedness, normative helping behavior, benefits, career benefits, and intention. This indicates that the overall community service attitude at the individual student level had changed after the service-learning. In other words, the service-learning program positively impacted dental students’ attitude toward community service and its impact did not depend on the scale (p-value for interaction time*scale (0.065) was not significant).
In general, the attitude scores were relatively high in pre-test -- LS pre-test means ranged from 4.573 to 5.954, with 1 being the least desirable and 7 being the most desirable attitude except for the costs scale, where is the scale was in the opposite direction. The post-test scores improved in all eight scales and the LS means changes ranged from 0.133 to 0.374. From the perspective of the magnitude of these changes, one might interpret these changes as “modest” and “not dramatic.” One possible reason for this “modest” change is that a mean score change for each scale was used rather than a total score for each scale, which would make the raw changes look larger. In addition, the high pre-test attitude scores may have contributed to make the changes appear smaller due to the ceiling effect – that is, only limited improvement was possible, given the high pre-test scores.
This study’s findings can be compared to those of Holtzman and Seirawan’s study where the authors found no evidence for a significant change in first year dental students’ attitude toward caring for the underserved before, during, and after participating in a community-based dental program (4) . One possible explanation is that in the Holtzman and Seirawan study, the study population was first year dental students who may have had idealistic attitude at the beginning, but become more realistic later, which may have resulted in lower attitude scores in the survey. It is also reasonable to speculate that their two-half-day clinical rotations, which were limited to examination, preventive treatment and delivering oral health education, would not be likely to change students’ attitude.
As for the relationship between student characteristics and attitude toward community service, age, gender, and previous or current volunteer activities did not impact dental students’ attitude in this study population across all scales; however, the ethnicity variable (White vs. non-White) which had a p-value of 0.0454. Ethnicity differences tested on all eight scales were significance only for the costs scale. White respondents were found to be more cognizant to the costs related to community service. One possible explanation is that White students may be more likely to have larger student loans than non-White students (mainly Asian students which comprised 26 of 30 non-White respondents) (36). White students with large loans would be more likely to be more cognizant of costs. However, even for the White and non-White comparison in the costs scale, the p-value was 0.0139 which can be considered significant at a=0.05 level but would not be considered significant after Bonferroni adjustment for multiple comparisons. This finding is consistent with other study’s finding of no significant differences in students’ attitude by age, gender, or volunteer experience (3,4). A lower percentage of respondents indicated that they volunteered regularly during dental school compared to those who regularly volunteered before dental school. The tight schedule and intense requirement coupled with less “need” to volunteer than for dental school admission may have attributed to fewer students volunteering during dental school.
There are some limitations of this study that are worth mentioning. First, the small sample size (57 for the pre-test and 76 for the post-test out of 105 students) did not allow us to perform multiple comparisons with confidence, nor to fully assess the application of Shiarella et al.’s CSAS to dental education by comparing our findings to Shiarella et al.’s findings. A larger sample size would have allowed us to assess CSAS’s application to dental education and evaluate its use in dental educational settings. With an emerging trend of emphasizing inter-professional education, CSAS can help educators across disciplines to evaluate their program using the same scale. Second, this study adopted RTP (retrospective pre-test) where the overestimation of the program effect is possible (31). Third, this study examined the service-learning program at a particular dental school. Differently structured service-learning programs would have different impacts on students’ attitude. Future research can examine how different service-learning/community-based dental education programs impact dental students’ attitude and may allow for development of a gold standard or “best practice” that would maximize students’ learning outcomes. Fourth, even if students’ attitude toward community service is believed to be a predictor for their actual behavior, it would be inappropriate to conclude that a service-learning program impacts community service behavior after graduation. Future research can follow up with these dentists to assess the impact of the service-learning program related to community service activities after graduation.
Conclusions
The main findings of this study can be summarized as follows. The service-learning program at VCU School of Dentistry during 2011–2012 positively impacted senior dental students’ attitude toward community service as measured with CSAS. More specifically, scales such as connectedness, normative helping behavior, benefits, career benefits, and intention showed significant pre and post-test differences. Relationships between student characteristics such as age, gender, ethnicity, and previous and current volunteer activities and students’ attitude toward community service were examined but were not found to be statistically significant.
Educators and administrators of service-learning programs in higher education, especially in health professional schools, can use this study’s findings as an example of one of the service-learning program’s potential outcomes: improving students’ attitude toward community service. They can also apply the CSAS tool to evaluate their service-learning program’s impact and to make students’ experience with service-learning better and to compare their findings to this study’s findings or between different programs. This will be useful to meet the trend of emphasis on inter-professional education.
ACKNOWLEDGMENT
The project described was partially supported by CTSA award No. UL1TR000058 from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
APPENDIX A: CSAS (Community Service Attitude Scale) and Questions
| Scales | Question No. |
Description |
|---|---|---|
| Awareness | 14 | Community groups need our help. |
| 19 | There are people in the community who need help. | |
| 31 | When I meet people who are having a difficult time,
I wonder how I would feel if I were in their shoes. |
|
| 33 | I feel bad that some community members are suffering
from a lack of resources. |
|
| 34 | I feel bad about the disparity among community members. | |
| 36 | There are needs in the community. | |
| 44 | There are people who have needs which are not being met. | |
| Connectedness | 25 | I am responsible for doing something about improving
the community. |
| 27 | It is my responsibility to take some real measures
to help others in need. |
|
| 28 | It is important to provide a useful service to the
community through community service. |
|
| 29 | It is important to me to have a sense of
contribution and helpfulness through participating in community service. |
|
| 30 | It is important to me to gain an increased sense of
responsibility from participating in community service. |
|
| 35 | I feel an obligation to contribute to the community. | |
| 39 | Other people deserve my help. | |
| 41 | It is critical that citizens become involved in
helping their communities. |
|
|
Normative Helping Behavior |
15 | In general, it is important to help people. |
| 16 | Improving communities is important to maintaining a
quality society. |
|
| 17 | I can make a difference in the community. | |
| 18 | Our community needs good volunteers. | |
| 20 | All communities need good volunteers. | |
| 21 | Volunteer work at community agencies helps solve
social problems. |
|
| 22 | Volunteers in community agencies make a difference,
if only a small difference. |
|
| 23 | College student volunteers can help improve the
local community. |
|
| 24 | Volunteering in community projects can greatly
enhance the community's resources. |
|
| 26 | Contributing my skills will make the community a better place. | |
| 45 | My contribution to the community will make a real difference. | |
| Costs | 7 | I would have less time for my work. |
| 8 | I would have forgone the opportunity to make money
in a paid position. |
|
| 9 | I would have less energy. | |
| 10 | I would have less time to work. | |
| 11 | I would have less free time. | |
| 12 | I would have less time to spend with my family. | |
| Benefits | 1 | I would be contributing to the betterment of the community. |
| 2 | I would experience personal satisfaction knowing
that I am helping others. |
|
| 3 | I would be meeting other people who enjoy community service. | |
| 4 | I would be developing new skills. | |
|
Career Benefits |
5 | I would make valuable contacts for my professional career. |
| 6 | I would gain valuable experience for my resume. | |
| Seriousness | 37 | Lack of participation in community service will
cause severe damage to our society. |
| 38 | Without community service, today's
disadvantaged citizens have no hope. |
|
| 40 | Community service is necessary to making our
communities better. |
|
| 42 | Community service is a crucial component of the
solution to community problems. |
|
| 43 | The more people who help, the better things will get. | |
| Intention | 13 | I want to do this activity. |
| 32 | I will participate in a community service project in the next year. | |
| 46 | Would you seek out an opportunity to do community
service in the next year? |
|
Source: adapted and modified from Bringle RG, Phillips MA, Hudson M. The measure of service learning. Washington D.C. U.S.A. American Psychological Association; 2004:180–182.
APPENDIX B: Survey 1 (post-test) and Survey 2 (RPT) first pages
Service-learning: Survey 1
We are trying to understand your willingness to donate your time regularly to community service after graduation. By community service, we mean a project in which you would volunteer regularly and use your skills and knowledge in dentistry. These types of community service require a commitment and offer you the opportunity to share your skills as well as develop new ones. Examples include participating in MOM (Missions of Mercy) projects, Give Kids a Smile, and/or providing uncompensated care to underserved populations.
Please answer the following questions about your feelings regarding community service projects using the definition above. Some of the questions might appear similar, but please answer all of them. If a question does not apply to you, please skip the question.
Now, pretend you are going to volunteer for a community service project sometime in the next year. Questions below ask you about possible outcomes of volunteering. Use the following scale to rate how likely you feel these outcomes are to occur.
| 1) | I would be contributing to the betterment of the community. |
| □ Extremely unlikely | |
| □ Quite unlikely | |
| □ Slightly unlikely | |
| □ Neither likely nor unlikely | |
| □ Slightly likely | |
| □ Quite likely | |
| □ Extremely likely | |
| 2) | I would experience personal satisfaction knowing that I am helping others. |
| □ Extremely unlikely | |
| □ Quite unlikely | |
| □ Slightly unlikely | |
| □ Neither likely nor unlikely | |
| □ Slightly likely | |
| □ Quite likely | |
| □ Extremely likely | |
| 3) | I would be meeting other people who enjoy community service. |
| □ Extremely unlikely | |
| □ Quite unlikely | |
| □ Slightly unlikely | |
| □ Neither likely nor unlikely | |
| □ Slightly likely | |
| □ Quite likely | |
| □ Extremely likely | |
| 4) | I would be developing new skills. |
| □ Extremely unlikely | |
| □ Quite unlikely | |
| □ Slightly unlikely | |
| □ Neither likely nor unlikely | |
| □ Slightly likely | |
| □ Quite likely | |
| □ Extremely likely |
Service-learning: Survey 2
We are trying to understand your willingness to donate your time regularly to community service after graduation. By community service, we mean a project in which you would volunteer regularly and use your skills and knowledge in dentistry. These types of community service require a commitment and offer you the opportunity to share your skills as well as develop new ones. Examples include participating in MOM (Missions of Mercy) projects, Give Kids a Smile, and/or providing uncompensated care to underserved populations.
Please answer the following questions about your feelings regarding community service BEFORE the service-learning rotations using the definition above. Some of the questions might appear similar, but please answer all of them.
Now, pretend you are going to volunteer for a community service project sometime in the next year. Questions below ask you about possible outcomes of volunteering. Use the following scale to rate how likely you FELT or WOULD'VE FELT these outcomes are to occur BEFORE your service-learning rotations.
| 1) | I would be contributing to the betterment of the community. |
| □ Extremely unlikely | |
| □ Quite unlikely | |
| □ Slightly unlikely | |
| □ Neither likely nor unlikely | |
| □ Slightly likely | |
| □ Quite likely | |
| □ Extremely likely | |
| 2) | I would experience personal satisfaction knowing that I am helping others. |
| □ Extremely unlikely | |
| □ Quite unlikely | |
| □ Slightly unlikely | |
| □ Neither likely nor unlikely | |
| □ Slightly likely | |
| □ Quite likely | |
| □ Extremely likely | |
| 3) | I would be meeting other people who enjoy community service. |
| □ Extremely unlikely | |
| □ Quite unlikely | |
| □ Slightly unlikely | |
| □ Neither likely nor unlikely | |
| □ Slightly likely | |
| □ Quite likely | |
| □ Extremely likely | |
| 4) | I would be developing new skills. |
| □ Extremely unlikely | |
| □ Quite unlikely | |
| □ Slightly unlikely | |
| □ Neither likely nor unlikely | |
| □ Slightly likely | |
| □ Quite likely | |
| □ Extremely likely |
Footnotes
The scale of benefits refers to general personal benefits compared to career benefits being more directly related to career.
The authors disclaim no conflicts of interest.
References
- 1.U.S. Department of Health and Human Services. Oral Health in America: a report of the surgeon general. 2000. [Google Scholar]
- 2.Smith CS, Ester TV, Inglehart MR. Dental education and care for underserved patients: an analysis of students' intentions and alumni behavior. J Dent Educ. 2006 Apr;70(4):398–408. [PubMed] [Google Scholar]
- 3.Kuthy RA, Heller KE, Riniker KJ, McQuistan MR, Qian F. Students' opinions about treating vulnerable populations immediately after completing community-based clinical experiences. J Dent Educ. 2007 May;71(5):646–654. [PubMed] [Google Scholar]
- 4.Holtzman JS, Seirawan H. Impact of community-based oral health experiences on dental students' attitudes towards caring for the underserved. J Dent Educ. 2009 Mar;73(3):303–310. [PubMed] [Google Scholar]
- 5.Davidson PL, Nakazono TT, Carreon DC, Bai J, Afifi A. Practice Plans of Dental School Graduating Seniors: Effects of the Pipeline Program. J Dent Educ. 2009 Feb;73(2):S283–S296. [PubMed] [Google Scholar]
- 6.Rubin RW, Rustveld LO, Weyant RJ, Close JM. Exploring Dental Students' Perceptions of Cultural Competence and Social Responsibility. J Dent Educ. 2008 Oct;72(10):1114–1121. [PubMed] [Google Scholar]
- 7.Bringle RG, Phillips MA, Hudson M. The Measure of Service Learning. n/a ed. Washington D.C. U.S.A.: American Psychological Association; 2004. [Google Scholar]
- 8.Furco A. Service-learning: A balanced approach to experiential education. Expanding boundaries: Serving and learning. 1996;1:1–6. [Google Scholar]
- 9.Hood JG. Service-Learning in Dental Education: Meeting Needs and Challenges. J Dent Educ. 2009 Apr;73(4):454–463. [PubMed] [Google Scholar]
- 10.Jacoby B. Service-learning in higher education. San Francisco, U.S.A.: Jossey-Bass Publisher; 1996. [Google Scholar]
- 11.Learn and Serve America’s National Service-Learning Clearinghouse. [Accessed: October 16, 2011];Service-learning is …. Available at: www.servicelearning.org/what_is_service-learning/service-learning_is/index.php.
- 12.Zlotkowski E. Pedagogy and engagement. Colleges and universities as citizens. 1999:96–120. [Google Scholar]
- 13.Schwartz JE. The value of education & certification in the dental office. Dent Assist. 2002 Sep-Oct;71(5):26–27. [PubMed] [Google Scholar]
- 14.Schwartz SH. Normative Influences on Altruism1. Advances in experimental social psychology. 1977;10:221–279. [Google Scholar]
- 15.Dewey J. Experience and education. The Educational forum. 1986;50(3):241. [Google Scholar]
- 16.Dewey J. Democracy and Education : An Introduction to the Philosophy of Education. Boston: MobileReference.com; 1916. [Google Scholar]
- 17.Seifer SD. Service-learning: Community-campus partnerships for health professions education. Academic medicine. 1998;73(3):273. doi: 10.1097/00001888-199803000-00015. [DOI] [PubMed] [Google Scholar]
- 18.Formicola AJ. Dental school clinics as patient care delivery centers: a paradigm shift in dental education. J Dent Educ. 2008 Feb;72(2 Suppl):18–20. [PubMed] [Google Scholar]
- 19.Brondani MA, Clark C, Rossoff L, Aleksejūnienė J. An evolving community-based dental course on professionalism and community service. J Dent Educ. 2008;72(10):1160–1168. [PubMed] [Google Scholar]
- 20.Bailit H. Community-based clinical education programs. Major findings and recommendations. J Dent Educ. 1999 Dec;63(12):981–989. [PubMed] [Google Scholar]
- 21.Brondani MA. Teaching Social Responsibility Through Community Service-Learning in Predoctoral Dental Education. J Dent Educ. 2012;76(5):609–619. [PubMed] [Google Scholar]
- 22.Yoder KM. A framework for service-learning in dental education. J Dent Educ. 2006;70(2):115. [PubMed] [Google Scholar]
- 23.Strauss RP, Stein MB, Edwards J, Nies KC. The Impact of Community-Based Dental Education on Students. J Dent Educ. 2010 Oct;74(10):S42–S55. [PubMed] [Google Scholar]
- 24.Davidson PL, Carreon DC, Baumeister SE, Nakazono TT, Gutierrez JJ, Afifi AA, et al. Influence of contextual environment and community-based dental education on practice plans of graduating seniors. J Dent Educ. 2007 Mar;71(3):403–418. [PubMed] [Google Scholar]
- 25.McQuistan MR, Kuthy RA, Qian F, Riniker-Pins KJ, Heller KE. Dentists' treatment of underserved populations following participation in community-based clinical rotations as dental students. J Public Health Dent. 2010;70(4):276–284. doi: 10.1111/j.1752-7325.2010.00182.x. [DOI] [PubMed] [Google Scholar]
- 26.Brondani MA. Students’ reflective learning within a community service-learning dental module. J Dent Educ. 2010;74(6):628–636. [PubMed] [Google Scholar]
- 27.Shiarella A, McCarthy A, Tucker M. Development and construct validity of scores on the Community Service Attitudes Scale. Educational and Psychological Measurement. 2000 Apr;60(2):286–300. [Google Scholar]
- 28.Nimon K, Zigarmi D, Allen J. Measures of Program Effectiveness Based on Retrospective Pretest Data: Are All Created Equal? American Journal of Evaluation. 2011 Mar;32(1):8–28. [Google Scholar]
- 29.Pelfrey WV, Sr, Pelfrey WV., Jr Curriculum Evaluation and Revision in a Nascent Field The Utility of the Retrospective Pretest-Posttest Model in a Homeland Security Program of Study. Eval Rev. 2009 Feb;33(1):54–82. doi: 10.1177/0193841X08327578. [DOI] [PubMed] [Google Scholar]
- 30.Campbell DT, Stanley JC, Gage NL. Experimental and quasi-experimental designs for research. Houghton Mifflin Boston: 1963. [Google Scholar]
- 31.Hill L, Betz D. Revisiting the retrospective pretest. American Journal of Evaluation. 2005 Dec;26(4):501–517. [Google Scholar]
- 32.Redelmeier DA, Kahneman D. Patients' memories of painful medical treatments: real-time and retrospective evaluations of two minimally invasive procedures. Pain. 1996;66(1):3–8. doi: 10.1016/0304-3959(96)02994-6. [DOI] [PubMed] [Google Scholar]
- 33.Skeff KM, Stratos GA, Bergen MR. Evaluation of a Medical Faculty Development Program A Comparison of Traditional Pre/Post and Retrospective Pre/Post Self-Assessment Ratings. Eval Health Prof. 1992;15(3):350–366. [Google Scholar]
- 34.Beling J. Impact of Service Learning on Physical Therapist Students' Knowledge of and Attitudes Toward Older Adults and on Their Critical Thinking Ability. Journal of Physical Therapy Education. 2004;18(1) [Google Scholar]
- 35.Eyler Janet, Giles Dwight, Stenson Christine, Gray Charlene J. At a Glance: What We Know About the Effects of Service Learning on College Students, Faculty, Institutions, and Communities, 1993–2000. [Google Scholar]
- 36.Jolly P. Medical school tuition and young physicians’ indebtedness. Health Aff. 2005;24(2):527–535. doi: 10.1377/hlthaff.24.2.527. [DOI] [PubMed] [Google Scholar]