Abstract
Background:
The aim of this study was to evaluate the clinical lesions of human immunodeficiency virus (HIV)/acquired immune deficiency syndrome patients in the oral cavity, head and neck region and to determine their associations with level of immune suppression as measured by the CD4+ count.
Materials and Methods:
In a descriptive cross-sectional study, 50 patients with a proven HIV infection were evaluated. Based on the clinical findings and CD4+ counts, the relationships between oral lesions and CD4+ cell count were investigated.
Results:
The CD4+ count (cells/mm3) was <200, 200-500, and >500 in 32 cases (64%), 16 cases (32%) and 2 cases (4%) respectively, and the mean CD4+ count was 169.82 cells/mm3 in males and 142.8 cells/mm3 in females. All patients showed at least one oral manifestation. The most common oral lesion identified was pseudomembranous candidiasis accounting for 76% (38/50) followed by periodontal disease 34% (17/50), herpetic lesions and hairy leukoplakia 10% for each (5/50), gingivitis 8% (4/50), oral ulceration 8% (4/50), Kaposi’s sarcoma 6% (3/50), and Non-Hodgkin lymphoma 2% (1/50).
Conclusion:
The CD4+ count was decreasing the presence, and the severity of oral lesions was increasing in this study. The presence of oral lesions may lead to a positive diagnostic of HIV. Disease progression is characterized by increased prevalence of some oral lesions as candidiasis, hairy leukoplakia, and Kaposi sarcoma. The severity of oral lesions was more pronounced with a CD4+ count <200 cells/mm3.
Keywords: Acquired immune deficiency syndrome, CD4+, human immunodeficiency virus, oral lesions
Introduction
Acquired immune deficiency syndrome (AIDS) is a disease spectrum of the human immune system caused by infection with human immunodeficiency virus (HIV).1
HIV/AIDS is a global pandemic.1,2 As of 2012, approximately 35.3 million people have HIV worldwide with the number of new infections that year being about 2.3 million.3 This is down from 3.1 million new infections in 2001. Of these approximately, 16.8 million are women, and 3.4 million are less than 15-year-old. It resulted in about 1.6 million deaths in 2012, down from a peak of 2.2 million in 2005.3
HIV is a fatal infection, which compromises the body’s immune system and leaves the victim vulnerable to life-threatening opportunistic infections, neurologic disorders, or unusual malignancies.1 The key manifestation of HIV infection is a severe immunodeficiency state, which is principally caused by diminished CD4 T-lymphocytes.4
There are about 40 known oral manifestations of AIDS according to the classification by the European Economic Community.5-7
These oral lesions may cause considerable pain, discomfort, inability to swallow, and difficulty in eating and may compromise facial appearance. This may lead to malnourishment, emaciation, and stigmatization.
Early management of these oral lesions will improve the overall quality of life of the infected individuals.
Oral candidiasis is the most common feature of AIDS in the oral cavity, with a prevalence of 70-90%.8-11
Non-Hodgkin’s lymphoma and Kaposi sarcoma have a strong correlation with HIV infection and are described as the AIDS-defining conditions.12-14 Eventually, cystic enlargement of the parotid gland and Kaposi’s sarcoma are increasingly being encountered in the head and neck examination of HIV-infected patients.15-17
Apart from their diagnostic importance, oral manifestations may be of prognostic importance for the subsequent development of AIDS. They can also serve as clinical correlates with CD4+ counts.18-20
CD4+ T-cells are the primary target of HIV; their depletion severely limits the host response capacity.21
The ability of the immune system to mount a specific response against HIV is a key factor in the subsequent disease course.4
Eventually, when a significant number of CD4+ lymphocytes have been destroyed and when production of new CD4+ cells cannot match destruction, then failure of the immune system leads to the appearance of clinical AIDS.4,22,23
The measurement of CD4+ counts requires a blood sample and laboratory analysis, the identification of oral lesions can be made during the course of physical examination.
The aim of this study was to evaluate the clinical signs and symptoms of HIV/AIDS patients in the oral cavity, head and neck region and to determine the association of oral lesions with level of immune suppression as measured by the CD4+ count.
Materials and Methods
In a descriptive cross-sectional study conducted for a 2 years period, 50 patients with HIV infection were evaluated. The relationship between oral lesions and CD4+ cell count was investigated. Ethical clearance was obtained, and every participant gave informed consent.
Patient records, available at the Odontology Department of Saint-Antoine Hospital, were initially studied and then the patients were asked to visit the clinic for a further evaluation. A thorough medical history was taken and a physical examination of the oral cavity, head and neck area was performed on each patient. The variables studied, including medical history, physical examination, demographic data and laboratory tests, were reviewed. Based on the findings of a physical examination and laboratory tests, patients were prescribed essential medication and repeated examination, and follow-up visits were considered.
One qualified oral surgeon examined the patients taking into consideration the site and type of oral lesions present using the criteria established by the European Community Clearing-House/World Health Organization, 1993 on oral problems related to HIV.7 Where multiple lesions were seen in the same patient at the time of clinical evaluation, each lesion was considered independently for analysis.
CD4+ count level were analyzed by the flow cyto-metric method CD4+ cell counts ≥500 cells/mm3 was classified as “marginally immunodeficient,” CD4+ cell count of >201 to <499 cells/mm3 as “mildly immunodeficient” and CD4+ cell count of ≤200 cells/mm3 as “severely immunodeficient.”24
Other systemic conditions that could lead to low CD4+ count such as tuberculosis, autoimmune diseases and use of immunosuppressive medications were considered as co-morbidities for CD4+ evaluation.
Data obtained from the study were analyzed using the Statistical Package for Social Sciences (SPSS; version 16.0, Chicago, USA). The statistical variables and data analyzed were the bio data of the recruited population, the types of oral lesions present, the level of CD4+ count and its relationship with oral lesions.
Results
Fifty cases were enrolled in this study, with a mean age of 39.9 years (28-57). 45 (90%) cases were male and 5 (10%) were female.
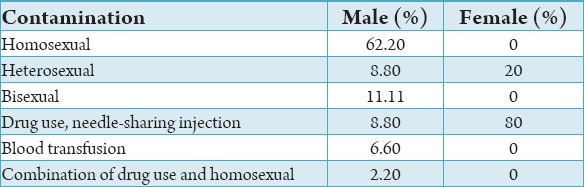
The contamination was related to homosexual relation for 28 cases, shared intravenous needles in 8 cases, bisexual relation in 5 cases, heterosexual relation in 5 cases, blood transfusion in 2 cases and 1 case of a combination of shared intravenous needles and homosexual (Table 1).
Table 1.
Distribution regarding the route of contamination and gender.
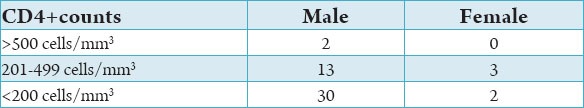
The CD4+ count (cells/mm3) was <200, 200-500, and >500 in 32 cases (64%), 16 cases (32%) and 2 cases (4%) respectively, and the mean CD4+ count was 169.82 in males and 142.8 in females (Table 2).
Table 2.
CD4+ counts and gender distribution.
All patients showed at least one oral manifestation. The most common oral lesion identified was pseudomembranous candidiasis accounting for 76% (38/50) followed by periodontal disease 34% (17/50), herpetic lesions and hairy leukoplakia 10% for each (5/50), gingivitis 8% (4/50), oral ulceration 8% (4/50), Kaposi’s sarcoma 6% (3/50) and non-Hodgkin lymphoma 2% (1/50) (Figure 1).
Figure 1.

Clinical appearance of the oral lesions. (a) Periodontal disease, (b) gingivitis, (c) herpetic lesion, (d) pseudomembranous candidiasis, (e) hairy leukoplakia, (f) ulceration, (g) Kaposi’s sarcoma, (h) non-Hodgkin lymphoma.
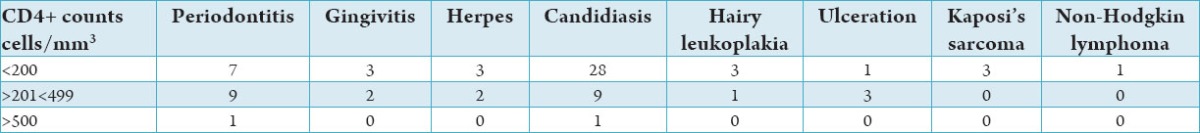
The distribution of oral lesions based on the CD4+ count of HIV infected patients showed that 62% of the oral lesions occurred at CD4+ count <200 cells/mm3, about 26% oral lesions were seen at CD4+ count of 201-499 cells/mm3, whereas 12% cases of oral lesions were seen at CD4+ count >500 cells/mm3 (Table 3).
Table 3.
Distribution of oral manifestations related to CD4+.
Discussion
Oral lesions are common findings in HIV infection. The main factor associated with the development of oral lesions is damage to the immune system, specifically loss of CD4+ lymphocytes, which are involved in cell-mediated immunity.20 The mean age of the participants in this study was approximately 39 years, demonstrating a trend for infection among the young population.
The mean age of males was significantly higher than that of females (40.7 vs. 32.4). The main route of HIV transmission was sexual contact (76% of cases) followed by shared intravenous needles (18%) and blood transfusion (6%). Shared intravenous needles infected the majority of females and males were infected through sexual contact. A predilection was observed in our study, which is a characteristic of the most common transmission route of HIV, followed by shared intravenous needles.
Earlier studies have reported that HIV patients with a CD4+ count of <200 cells/ml had more oral lesions.18,20,23 A similar finding was recorded in this study in which 62% of the total HIV-related oral lesions were in the group of patients with CD4+ count of <200 cells/ml.
The inverse relationship between the CD4+ counts and the prevalence of oral mucosal lesions in HIV-infected patients has been previously reported.8,23,25 Similarly, this study observed a significant inverse relationship between CD4+ counts and the prevalence of oral lesions in HIV-infected patients.
These findings indicate that the occurrence of oral lesions in HIV patients could be a useful guide in determining the reduction in the immunological status of HIV patients. This agrees with reports that CD4+ depletion was strongly associated with a high level of viral load.20 Therefore, clinicians and researchers are advocating oral lesions as a useful tool for the diagnosis and detection of the progression of HIV infection.20,25
The main factor associated with the development of oral opportunistic lesions is the CD4+ count.20 The onset of oral candidiasis and oral hairy leukoplakia is heralded by a sustained reduction in the CD4+ blood cell count associated with a sharp increase in viral load.12 An earlier study8 observed that oral lesions found among a cohort of 737 persons in Italy infected with HIV were significantly associated with CD4+ count of <300 cells/mm3. In a study done on a population of 43 subjects in Greece9 oral hairy leukoplakia was found to be associated with CD4+ counts <200 cells/mm3. Analysis of oral lesions in 81 HIV-positive subjects and 31 HIV-negative subjects and their CD4+ counts in a study done at Oyo, Nigeria has shown that CD4+ counts <500 cells/mm3 were significantly associated with having pseudomembranous candidiasis and angular cheilitis.26
Similarly, this study revealed that the presence of oral candidiasis and hairy leukoplakia were associated with CD4+ counts <200 cells/ml.
Thus far, CD4+ cell count is recognized and widely used as a marker for HIV-related disease progression. Accordingly, the Centers for Disease Control and Prevention has proposed a revised classification system. Moreover, AIDS case surveillance definition that incorporates both clinical signs and symptoms as well as one laboratory marker, CD4+ cell count.7
Conclusion
Within the limitations of this study, the CD4+ count was decreasing the presence, and the severity of oral lesions was increasing in this study. The presence of oral lesions may lead to a positive diagnostic of HIV. Disease progression is characterized by increased prevalence of some oral lesions as candidiasis, hairy leukoplakia, and Kaposi sarcoma. The severity of oral lesions was more pronounced with a CD4+ count <200 cells/mm3.
Early management of these oral lesions will improve the overall quality of living of the infected individuals. Oral health specialists are the most appropriate personal to diagnose and manage the majority of these oral manifestations. Awareness’ still the best route to follow in the HIV infection.
Footnotes
Conflict of Interest: None
Source of Support: Nil
References
- 1.Sepkowitz KA. AIDS – The first 20 years. N Engl J Med. 2001;344(23):1764–72. doi: 10.1056/NEJM200106073442306. [DOI] [PubMed] [Google Scholar]
- 2.Cohen MS, Hellmann N, Levy JA, DeCock K, Lange J. The spread, treatment, and prevention of HIV-1: Evolution of a global pandemic. J Clin Invest. 2008;118(4):1244–54. doi: 10.1172/JCI34706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Geneva: World Health Organization; 2013. UNAIDS. WHO case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related disease in adults and childrens; pp. 6–16. [Google Scholar]
- 4.Phillips AN, Lundgren JD. The CD4 lymphocyte count and risk of clinical progression. Curr Opin HIV AIDS. 2006;1(1):43–9. doi: 10.1097/01.COH.0000194106.12816.b1. [DOI] [PubMed] [Google Scholar]
- 5.Pindborg JJ. Classification of oral lesions associated with HIV infection. Oral Surg Oral Med Oral Pathol. 1989;67(3):292–5. doi: 10.1016/0030-4220(89)90358-7. [DOI] [PubMed] [Google Scholar]
- 6.An update of the classification and diagnostic criteria of oral lesions in HIV infection. EEC-clearinghouse on oral problems related to HIV infection and WHO collaborating Centre on oral manifestations of the human immunodeficiency virus. J Oral Pathol Med. 1991;20:97–100. [PubMed] [Google Scholar]
- 7.1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Recomm Rep. 1992;41(RR-17):1–19. [PubMed] [Google Scholar]
- 8.Moniaci D, Greco D, Flecchia G, Raiteri R, Sinicco A. Epidemiology, clinical features and prognostic value of HIV-1 related oral lesions. J Oral Pathol Med. 1990;19(10):477–81. doi: 10.1111/j.1600-0714.1990.tb00790.x. [DOI] [PubMed] [Google Scholar]
- 9.Kolokotronis A, Kioses V, Antoniades D, Mandraveli K, Doutsos I, Papanayotou P. Immunologic status in patients infected with HIV with oral candidiasis and hairy leukoplakia. Oral Surg Oral Med Oral Pathol. 1994;78(1):41–6. doi: 10.1016/0030-4220(94)90115-5. [DOI] [PubMed] [Google Scholar]
- 10.Berberi A. Doctorate thesis. France: university of Champagne-Ardenne; 1994. Oral Pathology of AIDS: Clinical observations about 50 patients. [Google Scholar]
- 11.Berberi A. Oral candidiasis associated with HIV infection. Rev Odontostomatol. 1996;2:139–44. [Google Scholar]
- 12.Ramírez-Amador V, Esquivel-Pedraza L, Sierra-Madero J, Anaya-Saavedra G, González-Ramírez I, Ponce-de-León S. The changing clinical spectrum of human immunodeficiency virus (HIV)-related oral lesions in 1,000 consecutive patients: A 12-year study in a referral center in Mexico. Medicine (Baltimore) 2003;82(1):39–50. doi: 10.1097/00005792-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Berberi A, Mokhbat J, Nasseh I, Zeinoun T. Non-Hodgkin's lymphoma of the maxilla as a first clinical manifestation of HIV infection. Report of a case. Bull Group Int Rech Sci Stomatol Odontol. 1995;38:77–80. [PubMed] [Google Scholar]
- 14.Berberi A, Khairalah S, el Sahili N. Non-Hodgkin lymphoma associated with HIV infection: Report of two cases. Rev Odontostomatol. 2000;1:23–7. [Google Scholar]
- 15.Prasad HK, Bhojwani KM, Shenoy V, Prasad SC. HIV manifestations in otolaryngology. Am J Otolaryngol. 2006;27(3):179–85. doi: 10.1016/j.amjoto.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 16.Kim MK, Alvi A. Common head and neck manifestations of AIDS. AIDS Patient Care STDS. 1999;13(11):641–4. doi: 10.1089/apc.1999.13.641. [DOI] [PubMed] [Google Scholar]
- 17.Reisacher WR, Finn DG, Stern J, Zeifer B, Cocker R. Manifestations of AIDS in the head and neck. South Med J. 1999;92(7):684–97. doi: 10.1097/00007611-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Begg MD, Lamster IB, Panageas KS, Mitchell-Lewis D, Phelan JA, Grbic JT. A prospective study of oral lesions and their predictive value for progression of HIV disease. Oral Dis. 1997;3(3):176–83. doi: 10.1111/j.1601-0825.1997.tb00032.x. [DOI] [PubMed] [Google Scholar]
- 19.Bravo IM, Correnti M, Escalona L, Perrone M, Brito A, Tovar V, et al. Prevalence of oral lesions in HIV patients related to CD4 cell count and viral load in a Venezuelan population. Med Oral Patol Oral Cir Bucal. 2006;11(1):E33–9. [PubMed] [Google Scholar]
- 20.Margiotta V, Campisi G, Mancuso S, Accurso V, Abbadessa V. HIV infection: Oral lesions, CD4+cell count and viral load in an Italian study population. J Oral Pathol Med. 1999;28(4):173–7. doi: 10.1111/j.1600-0714.1999.tb02019.x. [DOI] [PubMed] [Google Scholar]
- 21.Chinen J, Shearer WT. Molecular virology and immunology of HIV infection. J Allergy Clin Immunol. 2002;110(2):189–98. doi: 10.1067/mai.2002.126226. [DOI] [PubMed] [Google Scholar]
- 22.Onakewhor JUE, Unuigbe AA. Determination of maternal immune status of HIV positive women using CD4 count level: Implications for the Nigeria PMTCT program. Sahel Med J. 2006;9:117–23. [Google Scholar]
- 23.Taiwo OO, Hassan Z. HIV-related oral lesions as markers of immunosuppression in HIV sero-positive Nigerian patients. J Med Med Sci. 2010;1:166–70. [Google Scholar]
- 24.Taiwo OO, Hassan Z. The impact of Highly Active Antiretroviral Therapy (HAART) on the clinical features of HIV - related oral lesions in Nigeria. AIDS Res Ther. 2010;7:19. doi: 10.1186/1742-6405-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tappuni AR, Fleming GJ. The effect of antiretroviral therapy on the prevalence of oral manifestations in HIV-infected patients: A UK study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92(6):623–8. doi: 10.1067/moe.2001.118902. [DOI] [PubMed] [Google Scholar]
- 26.Adurogbangba MI, Aderinokun GA, Odaibo GN, Olaleye OD, Lawoyin TO. Oro-facial lesions and CD4 counts associated with HIV/AIDS in an adult population in Oyo State, Nigeria. Oral Dis. 2004;10(6):319–26. doi: 10.1111/j.1601-0825.2004.01036.x. [DOI] [PubMed] [Google Scholar]


