Abstract
Objective
To describe how mothers of preterm infants who are learning to nipple feed view their own and their infant’s role in the feeding process.
Design
Descriptive, comparative study.
Setting
Two neonatal intensive-care units (NICU) in the Midwest.
Participants
A convenience sample of 22 mothers of very-low-birth-weight infants.
Main Outcome Measures
Interviews were rated for mothers’ level of thinking about their co-regulatory role in their infants’ feeding on a 6-point scale. The higher the score the more flexible, contingent, adaptive, and reflective the mother’s thinking is regarding her infant’s and her own behavior during feeding. High and low scores were compared using paired t tests.
Results
The co-regulation scores ranged from 1 to 6, with a mean score of 3.3 (SD = 1.4). Mothers scoring higher on the co-regulation measure were significantly older and their infants were younger gestationally at birth. Their infants tended toward having been in the NICU for a longer period of time and spending more days on oxygen.
Conclusions
Understanding feeding from the parents’ perspective can guide clinicians as they support the development of parents’ feeding skills. Intervention, rather than beginning with how to feed, may need to begin with how to take the infant’s perspective, how to explore infant behavior that is novel, and ways of viewing the process of feeding as co-regulated.
Keywords: Co-regulation, Feeding, High-risk, Infant, Maternal, Preterm
“The biggest, biggest thing that scares me the most is that my whole life has changed from the way I looked at life in general to how I’m gonna feed my baby.”
Typically, learning to fully nipple feed is the final hurdle a preterm infant clears before leaving the neonatal nursery. In preparation for their infants’ discharge from the nursery, mothers are expected to learn to safely and adequately feed their infants. Little attention, however, has been paid to how caregivers think about their role in supporting and contributing to their infants’ feeding competencies. Clinicians recognize that infants’ feeding skills develop within the context of their physiologic and neurologic maturation. Often overlooked is the recognition that mothers of very-low-birth-weight (VLBW) infants are also in the process of developing their own feeding practice, adapted, in this case, within the context of a high-risk infant with unique vulnerabilities. Understanding feeding from the mother’s perspective will guide nurses as they support the development of mothers’ feeding practices with their high-risk infants.
Feeding is a context in which mothers learn to communicate with their infants, anticipate and respond to their infants’ agendas, and interpret feeding behaviors. They also are learning about themselves as parents as they engage in the practice of caregiving. During feeding, parents discover who they are as caregivers and how it feels to be needed and giving. They lay the foundation for who they will be for this child. As a primary task of early parenting, the act of feeding is a significant symbol of parenting to mothers of hospitalized preterm infants (Haase, 1992; Martin & Pridham, 1992; Thoyre & Pridham, 1994). In interviews with parents of preterm infants with bronchopulmonary dysplasia, Martin and Pridham (1992) found that early feeding experiences took on several meanings. Feeding was a way to be involved with their infants and feel connected to them, a means to provide nourishment and contribute to their child’s growth, and an opportunity to make their child happy through enjoyment of food.
Parents are expected to learn how to feed their infants safely and adequately, yet very little attention has been paid to mothers’ ideas about supporting their infants’ feeding competencies.
During the final weeks of their hospitalization in the neonatal intensive-care unit (NICU) preterm infants, particularly VLBW infants, are significantly challenged by the activity of nipple feeding (Guilleminault & Coons, 1984; Meier, 1988; Meier & Anderson, 1987; Rosen, Glaze, & Frost, 1984; Shiao, Brooker, & DiFiore, 1996; Shivpuri, Martin, Carlo, & Fanaroff, 1983). Mothers have the task of learning to feed an infant who is likely to fatigue easily (Medoff-Cooper, Weininger, & Zukowsky, 1989) and who may demonstrate feeding behaviors that are difficult to interpret, such as excessively long breathing pauses (Shiao et al., 1996; Thoyre & Carlson, 2000) and long pauses in sucking (Medoff-Cooper, Verklan, & Carlson, 1993). Physiologic studies have found that for some preterm infants significant oxygen desaturations continue to occur during feeding for several months after their discharge from the NICU (Rosen et al., 1984; Singer et al., 1992). Mothers report that feeding their VLBW infants is difficult, both while in the NICU and after hospital discharge (Martin & Pridham, 1992; Pridham, Martin, Sondel, & Tluczyk, 1989; Thoyre, in press; Thoyre & Pridham, 1994). At their infants’ 1-month postterm age, 28 of 52 mothers (54%) identified feeding problems with their VLBW infants who had a history of lung disease (Pridham, 1994). Difficult feeding often is unexpected by parents. In focus groups of parents of NICU graduates, parents expressed their surprise at finding how challenged they were by the complexity of nipple feeding their infants while in the NICU (Thoyre & Pridham, 1994).
From a dynamic systems perspective, the skill of feeding for a preterm infant emerges from the interaction of a number of components or subsystems, including the infant’s physiologic, state, and regulatory systems, as well as the caregiver’s co-regulatory feeding skills (Als, 1982, 1986; Fogel, 1993). However, the focus of preterm infant feeding research has been on components of feeding skill that reside solely within the infant rather than on the infant’s and feeder’s competence as a system. Mothers too often have been viewed as needing to understand their infant’s feeding skill rather than needing to understand that they are in fact a component of the infant’s skill.
During the preterm infant’s transition to self-regulated and coordinated feeding patterns, caregivers play a critical role in organizing the infant’s experience. This organization occurs as the parent co-regulates arousal, energy expended during the activity, respiratory adequacy, and the length of sucking bursts. For example, Rosen et al. (1984) noted that during feeding when infants had prolonged sucking at the expense of breathing, caregivers might interrupt the sucking and impose a breathing break. In these cases, maternal regulation of the length of the sucking, referred to as “pacing,” modified cardiorespiratory disturbances during feeding. The optimal degree and quality of guidance provided by the caregiver will vary, depending on the infant’s regulatory skills. Thus, in the case of an infant who sucks at the expense of respiration, the caregiver’s pacing actions are appropriate and supportive of the infant’s lack of skill at self-pacing. Together they co-regulate the feeding.
Mothers may need to support the feeding competencies of their preterm infant in novel ways, with means that may differ from their past experience or from their cultural norms. For example, sucking pauses that in a full-term infant might indicate diminished interest in feeding may, in a VLBW infant, indicate a need to regain adequate oxygen saturation levels (Thoyre & Carlson, 2000). It is likely to be challenging for mothers to create new ways of responding to their infants that remain sensitive to their needs and support their feeding competencies. Sensitive feeding of VLBW infants requires the mother to integrate and coordinate multiple feeding goals. A mother’s ability to adjust caregiving to the needs of a VLBW infant will vary, depending on how flexible and adaptive the mother is, her level of understanding of the infant’s capabilities, her ability to monitor the infant for behavioral cues and for responses to parental actions, her knowledge of feeding and of preterm infant feeding behavior, and her goals in caregiving (Bowlby, 1988; Bretherton, 1991; Pridham, 1993).
Examination of caregiver skill in feeding has largely focused on observation of maternal feeding behaviors. Maternal feeding skills, however, involve both observable behaviors and the thinking that frames and structures maternal action. Ainsworth and Bell (1969) found that mothers’ attitudes about patterning feedings influenced their infant feeding practices in the first 3 months of life. Mothers who sensitively paced and who were prompt in their responsiveness to their infants tended to have goals for feeding that included gratifying the infant, supporting regulation of the infant’s rhythms, and allowing the infant to be an active participant in the feeding. Pridham and colleagues (Martin & Pridham, 1992; Pridham et al., 1989) found that parents of VLBW children with bronchopulmonary dysplasia had as a primary feeding goal the child’s intake and, perhaps, growth. In the 1st year postdischarge, only 2 of the 11 families studied mentioned enjoyment or pleasure in feeding as one of their aims; none of the families mentioned the infant’s development of feeding competencies as a feeding goal.
Pridham developed the construct of “working model of feeding” to describe mothers’ beliefs, expectations, emotions, intentions, and motivations surrounding the activity of feeding (Pridham, 1993). “Working models” are defined as dynamic understandings of self, others, and the physical world that develop as individuals interact with others toward some aim (Bowlby, 1982). Working models serve to organize one’s experiences into a meaningful narrative and to assist in anticipation of the future. As such, a working model sets boundary conditions, directs perceptual cues, and constrains processes of interaction (Emde, 1994). Dimensions of mothers’ working models of feeding include (a) infant cues the mother monitors for decision making, (b) the importance to the mother of infant self-regulative behavior, (c) the mother’s view of her own role in supporting her infant in feeding, (d) the orientation of the mother’s action (e.g., toward adequate intake, infant feeding experience, time efficiency, or multiple aims), (e) criteria mothers use to evaluate the adequacy of a feeding, and (f) strategies mothers use to maintain or structure the feeding. Each working model dimension includes six ordinal categories that are given a score of 1 (low) to 6 (high). Higher scores on the working model measure as a whole represent more highly adaptive maternal expectations and intentions.
Studies exploring mothers’ working models of feeding preterm infants have focused on the postdischarge period (1 month through 1 year adjusted age). Overall, working model scores have varied across mothers and across the 1st year of the infant’s life (Pridham, Schroeder, & Brown, 1999), indicating that the working model measure may be a meaningful way to characterize the range of maternal thinking about infant feeding. Interactions of the adaptiveness of the working model with maternal personal resources have been found across the 1st year. The more education a mother had, the greater was the adaptiveness of her working model at 1, 8, and 12 months. The greater the mother’s depressive symptoms, the lower the adaptiveness of her working model at 8 months. Infant weight-for-age z score at 1, 8, and 12 months did not relate to the adaptiveness of the mother’s working model, whereas at 4 months, the lower the infant’s weight-for-age z score the more adaptive the mother’s working model. Links between the adaptiveness of mothers’ working models and maternal feeding actions also have been found. As working model scores increased, mothers’ sensitivity, responsiveness, and positive affect during feeding increased (Pridham, Schroeder, Brown, & Clark, 2000). At the assessment time nearest to the hospitalization period, at 1-month postterm age, mothers’ overall working model scores averaged 3.82 (SD = 1.13), indicating that, on the whole, mothers were primarily focused on feeding as a task, attending mainly to the amount of intake (Pridham, Schroeder, & Brown, 1999).
Mothers’ working models of feeding have not been described for VLBW infants at the transition to full oral feeding, a time when mothers are assuming the responsibility for feeding their preterm infants. This is a time when mothers’ working models may be open to information that contributes to an adaptive working model of feeding. The predischarge period offers multiple opportunities for building on mothers’ ideas about feeding. Parents are encouraged to plan visits around the task of feeding, a time when infants are most aroused and supported in interaction, to promote parent-child interaction and to learn feeding skills (Gill, Behnke, Conlon, McNeely, & Anderson, 1988; White-Traut & Nelson, 1988). In focus groups with parents of NICU graduates, mothers indicated that during the weeks before discharge they scheduled their visits around opportunities to feed their infants and they valued nurses’ knowledge about feeding (Thoyre & Pridham, 1994). Nurses can best engage a mother in development of her ideas if they have an understanding of ways mothers’ ideas may vary and how to explore these ideas. The purpose of the current study was to identify and describe how mothers of VLBW infants who are learning to nipple feed perceive their own and their infants’ role in the feeding process.
Method
This study was part of a larger study linking maternal thinking about feeding co-regulation, maternal and infant feeding behaviors, and infant physiology during VLBW infant nipple feeding (Thoyre, 1997). This article reports on maternal thinking about co-regulation, a dimension of a mother’s working model of feeding.
Sample
The sample consisted of mothers of eligible infants admitted to two midwestern hospital NICUs over a 12-month period for one hospital and a 6-month period for the second hospital. Infants weighed 1,500 g or less at birth (VLBW), nipple fed 50% or more of their daily dietary intake, and were 40 weeks or less postconceptional age at the time of study; the mothers all spoke English (N = 22). Excluded were infants with significant anatomical or pathophysiologic problems that interfered with feeding ability or potentially made a difference in how an infant may feed (such as congenital heart disease, known intrauterine toxin exposure, small for gestational age, or with higher than Grade II intraventricular hemorrhage diagnosed by ultrasound). Twenty-seven infants were eligible and recruited for the study. Twenty-six families consented to the study, and 24 families completed data collection. Data from two of the mother-infant dyads were not incorporated into the analysis because of incomplete physiologic data. The final sample consisted of 22 mother-infant dyads. Characteristics of the participants are presented in Table 1.
TABLE 1.
Characteristics of the Participants
| Mothers (n = 22) | M ± SD | Range |
| Age (yrs) | 25.9 ± 6.7 | 15–39 |
| Education (yrs) | 13.8 ± 3.8 | 8–21 |
| Parity | 2 ± 1.8 | 1–9 |
| Income levela | 4 ± 2 | 1–7 |
| Experience feeding (number of bottle feedings)b | 14 ± 11 | 1–47 |
| Anticipation of feeding involvementc | 80% ± 16% | 50–100% |
| Infants (n = 22) | M ± SD | Range |
| Birth weight (g) | 1,155 ± 293 | 620–1,500 |
| Weight at time of study (g) | 2,192 ± 302 | 1,692–2,720 |
| Gender (% female) | 54.5 | |
| Race (% nonwhite) | 31.8 | |
| Gestational age at birth (wks) | 28.1 ± 2.1 | 25–32 |
| Postconceptional age at study | 36.5 ± 1.6 | 33.5–40 |
| Days nipple fed | 16 ± 6.5 | 6–30 |
| Bottle feedings before study | 62 ± 27 | 11–115 |
| Days prior to discharge | 5 ± 9 | 1–38 |
| Prescribed feeding volume ingested (%) | 95% ± 12% | 60–100% |
| Days on oxygen | 42 ± 34 | 1–97 |
| Receiving oxygen at study day (%) | 31.8% | |
| % requiring O2 at 36 weeks | 36.4% |
1 = ≤$10,000; 2 = 10,000–11,999; 3 = 12,000–14,999; 4 = 15,000–24,999; 5 = 25,000–34,999; 6 = 35,000–49,999; 7 = ≥50,000.
Number of nipple feedings mother has participated in.
Percent of feedings mother expects to participate in postdischarge.
Procedure
Informed consent was obtained from all participants after a full discussion of the study procedures. Mothers of eligible infants were informed that the investigator was seeking to learn more about VLBW infant feeding. Mothers bottle fed their infants in a quiet parent visitation room when they determined that their infant was ready to feed and at a time they found convenient within the time frame the nursery protocols allowed. The feeding was videotaped with a close-up view of the infant’s face and upper body. Upon completion of the feeding, mothers were interviewed about their understanding of the feeding process. An interview protocol, the Joint Exploration of a Parent’s Working Model of Feeding (Pridham, Schroeder, Van Riper, et al., 1999), was used as a focused interview designed as a dialogue with mothers to aid understanding of their story of a feeding. During the interview, selected portions of the just-completed videotaped feeding were replayed for the mother to aid recall, facilitate the telling of her story, and invite joint exploration of the feeding. Portions of the video were selected on the basis of a point of decision the mother may have made (e.g., mother removes nipple), a change in infant behavior (e.g., the infant appears to have fallen asleep or breathing has become very noisy), or a change in maternal behavior (e.g., mother begins to move the bottle nipple in and out of the infant’s mouth). Mothers were encouraged to reflect on what the feeding was like for them and for their infants, what they and their infants were trying to accomplish throughout the feeding, how they were going about it, and how they determined how well things were going during the feeding. Videotape playback has been shown to increase awareness of one’s own and of the other’s behavior (Berger, 1971; Kagan, Schauble, Resnikoff, Danish, & Krathwohl, 1969).
Interviews were transcribed and given a single-rated score for co-regulation on a 6-point scale. Pridham, Schroeder, Van Riper, et al. (1999) developed the coding system using a process consistent with the method of dimensional analysis (Schatzman, 1991) to identify dimensions of the mother’s working model of feeding. The dimension of co-regulation includes (a) how the mother views the infant’s and her own participation in the feeding; (b) the extent to which the mother shares responsibility for the feeding process and outcome with the infant; (c) the support the mother describes the infant as needing and the extent to which the mother aims to support her infant in becoming a fuller participant in the feeding process; and (d) how the mother views the relationship she is developing with her infant as having regulatory functions. The higher the score, the more the mother views feeding as a jointly regulated process of shared responsibility with the infant for the outcome. In addition, the more flexible, contingent, adaptive, and reflective is the mother’s thinking regarding her infant’s and her own behavior, the more she views development of a relationship with her infant as contributing to the creation of smooth and effective feeding. Table 2 summarizes the feeding coding manual for the co-regulation dimension of a mother’s working model of feeding. The complete coding instructions for the co-regulation dimension are included in the Coding Manual for Maternal Working Models of Feeding (Pridham, Schroeder, Van Riper, et al., 1999).
TABLE 2.
Summary of Co-Regulation Scoring Manual
|
Note. From Coding Manual of the Working Model of Feeding, by K. F. Pridham, M. Schroeder, M. Van Riper, S. Thoyre, R. Limbo, & S. Mlynarczyk, 1999. Adapted with permission.
Interrater reliability was examined with five randomly selected interview transcripts. Four independent coders rated three of the interviews, and two independent coders rated the final two transcripts. All coders were content experts and members of a feeding research team; they were blind to all other data about these participants. Interrater agreement on coding within one scale point was 93.3%.
Results
The co-regulation scores ranged from 1 to 6, with a mean score of 3.3 (SD = 1.4). Figure 1 displays the frequencies of each scale point. There was a full 6-point range of scores, with a median score of 4.
FIGURE 1.
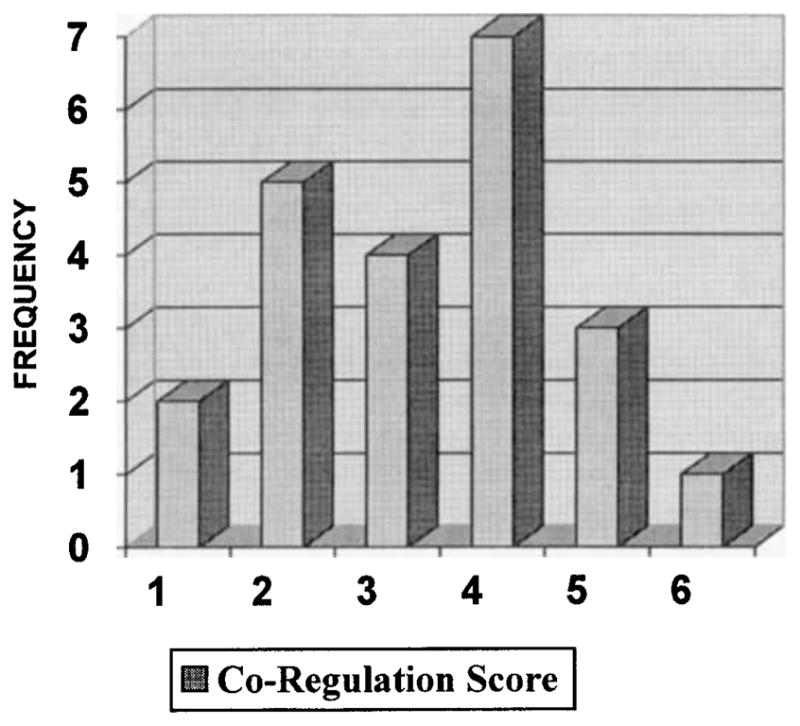
Frequency of each co-regulation score.
Scores were divided into high scores (4, 5, and 6) and low scores (1, 2, and 3) to compare specific group characteristics (see Table 3). There were no significant differences between groups of co-regulation scores by t tests on maternal years of education, parity (first time mother or not), family income level, number of feedings mother had participated in with her VLBW infant, infant birth weight, the number of days the infant had nipple feeding experience, gender, or whether the infant required oxygen on the day of the study. Mothers scoring higher on the co-regulation measure were significantly older (p < .05), and their infants were younger gestationally at birth (p < .05), tended to have been in the NICU for a longer period of time (p < .10), and tended toward having been on oxygen for more days (p < .10).
TABLE 3.
Comparison of High- and Low-Scoring Groups on Co-Regulation Measure
| Scores of 1, 2, 3 (2.2 ± .8) | Scores of 4, 5, 6 (4.5 ± .7) | ||
|---|---|---|---|
| Measurement | n = 11 | n = 11 | t |
| Mothers’ characteristics | |||
| Age | 22.8 ± 5.6 (15–34) | 28.5 ± 6.4 (17–39) | −2.26** |
| Education (yrs) | 14.2 ± 4.2 (8–20) | 13.5 ± 3.4 (9–21) | ns |
| Paritya | 1.45 ± .5 (1–2) | 1.63 ± .5 (1–2) | ns |
| Incomeb | 3.6 ± 2.0 (1–7) | 4.5 ± 1.8 (1–7) | ns |
| Feeding experiencec | 11.6 ± 7.5 (5–30) | 16.3 ± 13.8 (1–47) | ns |
| Infants’ characteristics | |||
| Birth weight (grams) | 1,255.9 ± 226 (817–1,463) | 1,053.4 ± 326 (620–1,500) | ns |
| Gestational age at birth (wks) | 29.3 ± 2.0 (25.5–32) | 26.9 ± 1.5 (25–29.5) | 3.25** |
| Weeks since birth | 7.3 ± 3.4 (3–14.5) | 9.6 ± 2.0 (6–14) | −1.76* |
| Experience nipple feeding (days) | 14.6 ± 6.6 (6–24) | 17.4 ± 6.6 (7–30) | ns |
| Days on oxygen | 28.3 ± 25.7 (1–65) | 55.5 ± 35.9 (1–97) | −2.05* |
| Oxygen at time of study (1 = yes, 2 = no) | 1.8 ± .4 (1–2) | 1.5 ± .7 (1–2) | ns |
1 = first infant, 2 = 2 or more children.
1 = ≤$10,000; 2 = 10,000–11,999; 3 = 12,000–14,999; 4 = 15,000–24,999; 5 = 25,000–34,999; 6 = 35,000–49,999; 7 = ≥50,000.
Number of nipple feedings mother has participated in.
p < .10,
p < .05; two-tailed t tests.
Mothers varied in the following: their view of the infant’s participation in feeding as valued and essential; their view of self as a co-regulator of feeding and sharing responsibility for the feeding; knowledge of specific infant behavior during feeding; integration of the goal of ensuring adequate feeding amount with goals for infant experience and development; and in whether they discussed their relationship with their infant as part of the context of the feeding. To illustrate maternal thinking about feeding, co-regulation profiles of mothers who rated high and low on the working model of feeding co-regulation score are presented. Quotes from the interviews are used to illustrate language used by mothers to describe their role in feeding near the time of discharge from the NICU.
Profile of Low Working Model of Feeding Co-Regulation Score
For mothers scoring 1, 2, or 3 (n = 11), infant participation in feeding may have been described and desired but was not viewed as a necessary condition of feeding. Mothers described how they redirected their infants’ agendas, ignored their infants’ communications, or “put on hold” the feedback they received from their infants in favor of accomplishing feedings. A common time for mothers to describe this type of thinking was at the onset of feeding, when they saw their role as getting the feeding started. Typically, mothers did not view their infants’ closed mouths, elevated tongues at the roof of their mouths, or heads moving away from the nipple either as having participatory meaning or as acceptable infant behavior. For example, one mother stated, “Sometimes I have to pull his mouth open, and sometimes he’ll have his tongue on top of his mouth and I’ll just have to pull his mouth down and shove the bottle in.” Mothers of this profile who recognized and spoke of their own behavior as directive did not wonder about how the infant might experience their actions. The infant’s perspective often was missing from their descriptions.
Mothers in this category did not view themselves as co-regulators of the feeding. They may have acted on the infant (mother as regulator) or observed how the feeding unfolded (infant as regulator). For example, in response to a question about what her infant needed from her as the feeding got started, a mother described her limited role in feeding, “Just get the bottle in him. That’s all. I don’t usually have to force it in his mouth.” Mothers in this category did not view their own actions as affecting the feeding outcome, therefore they shared minimal responsibility for the feeding with the infant. Alternatively, the infant was viewed as having the greatest responsibility for the feeding outcome. For example, in response to a question about what made a difference for her infant during feeding, a mother described how her infant had full responsibility for how the feeding unfolded, “Like I said, it depends on the kid. Every kid is different. So, some feedings he inhales and some he doesn’t.” Another mother had a similar response with minimal sense of how she affected the feeding: “I’ll try to feed him. If he takes it he takes it. If he doesn’t, he doesn’t. Then I’ll worry.
Mothers scoring lower also had minimal understanding of specific infant behavior during feeding. They aimed to understand how to feed an infant in general rather than how to feed their individual infant. There was minimal exploration of novel aspects of the feeding, and rules were used to guide their feeding decisions rather than specific infant behaviors. Burping was an area where the use of rules was very evident. Rules such as “after half of the feeding,” or after a set time limit, such as “after 10 minutes” were specified, rather than their understanding of ways their infants communicate a need for a rest or a burp. Some mothers stated they never burped their infants because no one had ever told them to or they had decided that burping was not necessary, once again without mention of the infants’ communications as guiding their decisions. For example, “I don’t let ‘em drink some of it and then burp them and feed ‘em again then burp them again. I just burp ‘em after they feed.”
Mothers fitting this profile often focused on ensuring adequate intake and accomplishing feeding safely. One strategy used to ensure adequate intake was to avoid loss of interest in feeding through nipple removal, “Once you take it [nipple] out, it’s harder to get him going again. That’s why I’m afraid to take it out when it’s time to burp. I’m afraid he might not start again.” Another strategy to ensure adequate intake was manipulating the nipple to feed the prescribed amount regardless of infant behaviors: “Well, it’s like she’s not really awake or interested in it. You’ve got to keep wiggling her bottle, or I try to play with her face a lot and try to get her going again.” These mothers rarely described how feeding was experienced by their infants. When asked if their infant could talk what would they tell us feeding was like for them, the common response for these mothers was “I have no idea.” When encouraged to explore the meaning of infant behaviors during the playback of the videotape, these mothers often came to quick conclusions with limited exploration of ideas. They raised few questions or hypotheses about what they perceived their infants were communicating.
Profile of High Working Model of Feeding Co-Regulation Score
For mothers scoring a 4, 5, or 6 (n = 11), infant participation was described as a necessary, valued, and even essential condition for the feeding to proceed. Mothers provided opportunity and time for the infant to organize himself or herself to the challenge of feeding. They proactively structured the feeding for as much participation from the infant as they thought possible. For example, a mother discussed how she helped her infant to start feeding,
I was just kinda putting the bottle near his tongue and when he would go to grab onto it, I’d wait a minute so that when he did grab onto it he’d grab onto it and hold on … and so I just waited until he’d grab onto this nipple. I was kind of waiting for him to signal me to put it in.
This mother acknowledged her infant’s need to be a partner in the feeding and described her role in supporting her infant’s participation. Another mother stated, “He’s a good eater if you can get him to be awake. When he can actively participate in eating he seems to just really be very aggressive at his feeding.”
These mothers viewed themselves as co-regulators in the feeding process and shared responsibility for the feeding outcome. They valued and acknowledged their own contributions to the feeding. Each guided her infant’s pattern of eating; his or her state of arousal, level of energy, postural organization, and breathing regulation; and the pace of the feeding. At times, they wondered about whether they were making the right decisions during feeding and therefore remained open to additional information or feedback to further guide their actions. For example, burping decisions included infant feedback, context of the feeding, and mothers’ understanding of what being proactive may provide. A mother described how she determined when to burp her infant,
Like if he isn’t eating as fast, or if he’s squirming around. If he’s been eating for a while and if he just doesn’t let me know then I do it on my own …. to prevent a stomachache. I thought, I didn’t want him to eat as long after he had eaten so fast.
To co-regulate, these mothers worked at getting to know their infants’ capabilities and at putting their co-regulatory actions within this context. Maternal understanding of specific infant behavior was crucial for feeding to be accomplished in a manner that optimized feeding intake, ensured safety during feeding, developed infant feeding skill, and helped the infant feel supported during an activity that was perceived to be difficult. Two important strategies were used to accomplish these goals. First, mothers took the infants’ perspective during feeding, empathized with the challenge their infants faced, and tried to help their infants feel safe during feeding.
At the end you can just hear her breathing and then, of course, the gurgling and all of that and to me that makes me think that she’s having a hard time with that part of the feeding and so I try not … it’s like I push her more at the beginning. I think that’s why it goes long without that first burp because at the end you can just hear all the different things that she is going through just to suck and swallow it and then to breathe … so … I mean you always wonder if what you are doing is right.
Another mother’s statement illustrates how she viewed her infant as a person to be considered, “I don’t want to force it in her mouth if she really doesn’t want it. If she really won’t open her mouth, then I won’t give it to her.”
Second, they sought opportunities to explore their own feeding practices, wondered about the meaning of novel infant behaviors during feeding, and raised questions that would facilitate their learning about their infant and how to structure the feeding to meet their goals. For example, after viewing the videotape, one mother wondered if she had contributed to her infant’s fatigue:
I guess usually I just let her go until she gets to the point where she stops sucking and if I try to pull it out she is tonguing it out, like when I pull it out, instead of sucking it back in, she tongues it out, and that’s when I try to do the first burp. Maybe I give her too much and that’s why she gets sleepy.
Another mother viewed the videotape of a time when she was wiggling the bottle to direct her infant’s attention back to the feeding. She listened carefully to her infant’s amplified breathing during this segment. The pattern of breathing was rapid and labored. She asked for the segment of tape to be replayed and then responded in a way that demonstrated her ability to reflect on her feeding practice and to empathize with her infant: “No one ever said anything about breathing breaks. Poor kid, you were just trying to catch up, we’re trying to force you to suck some more.”
Feeding, for these mothers, also offered an opportunity to engage in the multifaceted task of parenting. Multiple goals that were considered included ensuring feeding adequacy, providing a positive experience for their infants, expanding infant feeding skills, and developing a feeling of closeness between mothers and their infants. Mothers worked to integrate conflicting agendas, such as their perception of their infants’ need to take a break from feeding before achieving the prescribed intake. Enhancing the infant’s experience and helping him or her to develop an effective and pleasurable way of feeding moved to the foreground of their decision making. For example, a mother said when she ended a feeding, “It’s been a lot of work for her and it hasn’t been real rhythmic, and so I think at this point it’s give up … kind of like not worth it. It just seems like it is so much work for her. It’s like I’m forcing it into her more than anything else.” These mothers discussed the need for their infants to like to eat, to look forward to feeding, and to feel close during feeding. For example, a goal for one mother was that her infant was “… enjoying being awake with me.” Mothers perceived that the relationship they worked to create with their infants supported feeding and alerted them to their infants’ needs. A mother stated, “You have to pay a lot of attention. They’ll notice that you are paying attention to them. They’ll know, ‘Mommy’s watching and she wants to know if I am hungry or not. It’s time to tell her.’ If you are close to them like that, they will tell you.”
Discussion
The average score on the rated dimension of co-regulation was 3 on the 6-point scale, indicating that mothers varied in their thinking about their role in feeding their high-risk infants. The mean score was slightly lower than that reported by Pridham, Schroeder, and Brown (1999) for the overall working model score. This may suggest growth in mothers’ working models as they gain experience with feeding their infants. Mothers’ scores found in this study are consistent with the findings of Martin and Pridham (1992) and Pridham et al. (1989). Mothers primarily viewed their role as that of ensuring feeding intake and reacting to compelling cues that arise during feeding (e.g., crying, coughing, choking). Ensuring intake is a prime concern of the clinicians with whom mothers come into contact in the NICU. Therefore, it is not surprising that mothers say intake is a major goal in feeding. Adequate intake is essential for the growth and development of high-risk infants, especially during this time. However, growth occurs within a social framework that includes being fed in a supportive, calming, and responsive environment. Adequate intake may be ensured when the infant is fed with multiple goals in mind, including preventing fatigue, minimizing energy expenditure, maintaining adequate oxygenation, responding to infant communications, and creating a loving time. Being proactive during feeding to prevent distress and fatigue was rarely described as a maternal feeding action by this group of mothers.
Mothers primarily viewed their role as one who ensures feeding intake and reacts to compelling cues that arise during feeding (e.g., crying, coughing, choking).
Most mothers wanted their infants to participate in the feeding but did not stop feeding if their infants were giving subtle cues of disinterest, including cues of fatigue or distress. In particular, deciding when to start a feeding and when to end it or to offer a break varied among the mothers. In addition, mothers who were actively exploring how to make feedings smoother focused primarily on these issues.
Being proactive during feeding to prevent distress and fatigue was rarely described as a maternal feeding action by this group of mothers.
The mother’s evaluation of the feeding was beginning to include the infant’s experience of feeding. This would be expected during a time when mothers are coming to know their infants, particularly their infants’ feeding skills. Feeding is clearly a time when mothers learn about their infants’ behaviors as well as their infants’ responses to the actions of others. Working with mothers who are feeding their infants can provide many opportunities for clinicians to support the development of mothers’ ideas.
Higher scoring mothers were older and had more experience with their infants. Their infants had been born at an earlier gestational age and required oxygen for a longer period of time than did infants of mothers with lower scores. Contrary to the Pridham, Schroeder, and Brown study (1999), no significant relationship was found between a mother’s education or the birth weight of the infant with the scores on the co-regulation dimension. However, the relationship between high score and infants having an earlier gestational age at birth may be consistent with Pridham et al.’s finding of higher scores with lower weight-for-age z scores at 4 months of age. Mothers may view the smaller infant as more vulnerable and may expect to be more explorative and reflective in their thinking about feeding issues. Their working model may be more adaptive as a result.
Several hypotheses derived from the findings of this study warrant further research. One hypothesis is that mothers who have the opportunity to know their infants for a longer period of time begin to take their infants’ perspective, learn their subtle behaviors, and experience their own effect on their infants’ behavior in other venues, which then translates to their feeding practice. A second hypothesis is that these mothers view their infants as vulnerable. They then increase their monitoring of their infants and their care to protect them from further distress. A final hypothesis is that mothers of more vulnerable infants spend more time with clinicians, particularly the NICU nurses, or receive more individualized guidance in caring for their infants.
Limitations
Limitations of the current study include a small sample size, no control group comparison, a single data collection time point, and lack of descriptive data on the three women who either refused to participate or did not follow through with the study. In addition, reliability on a 6-point ordinal scale within one scale point may be an insufficient measure of reliability. It may be more useful to collapse the categories to achieve higher exact agreement reliability.
Nursing Implications
Very little attention has been paid to how parents and other caregivers contribute to infants’ feeding competencies. For example, parents have too often been viewed as needing to understand their infant’s feeding skill rather than needing to understand that they are in fact a component of the infant’s skill. Understanding how a mother views her role in feeding is an important starting point in teaching her about infant feeding skills. In working with mothers during the early development of their infant feeding practices, clinicians build on mothers’ ideas.
Clinicians’ support of a mother who is developing her ideas about feeding her infant will have important effects on how she structures feedings and responds to her infant’s feeding cues. Mothers need to learn to interpret infant feeding behavior within the context of the infant’s health status and often to respond to feeding cues in ways that are novel to them (Shaker, 1999). For example, behaviors that in a full-term infant might indicate satiety or lost interest in feeding may, in a VLBW infant, indicate a need for a pause in feeding to rest and reregulate breathing. Appropriate parental feeding behaviors will vary, depending on the meaning of the infant’s behavior. Thus, feeding will require a high level of attention and commitment to learning about the infant.
It is likely that with experience and getting to know their infants mothers grow toward a more developed understanding of their co-regulatory role in feeding. If clinicians view maternal thinking about feeding as a developmental process then their role in supporting mothers will expand to include facilitating development of maternal thinking about infant feeding. Intervention, rather than beginning with how to feed (such as how to position the infant, how much to feed, time frame to feed within), may need to begin with how to take the infant’s perspective, how to explore infant behavior that is novel, and ways of viewing the process of feeding as co-regulated. Clinical goals for maternal thinking may include (a) thinks of feeding as a joint process that she and her infant create together, (b) works to balance and weigh multiple goals in her decision making, (c) is flexible and less rule-bound in her plans for decision making about feeding, (d) aims to look at feeding from the infant’s perspective, (e) watches the infant for guidance on how to feed, and (f) considers whether her infant is coming to view feeding as positive, enjoyable, and relational.
In talking with many mothers about feeding their infants, I have learned that it takes very little time to assess how a mother is thinking about herself and her infant in the activity of feeding. Several questions have been found to be particularly useful in exploring how a mother approaches the feeding of her high-risk infant (see Table 4). These questions can assist the clinician in understanding how mothers view the process of feeding, their perception of their infants’ need for support, their primary goals during feeding, how they problem-solve novel or poorly understood issues, and the effect they believe they or others can have on creating smooth infant feeding.
TABLE 4.
Target Questions for Clinician Assessment of Maternal Thinking
| Target Questions |
|---|
| How would you like feedings to be for your infant? |
| If I had to feed your newborn for the first time what would I need to know about him or her? |
| What have you found gets in the way of your infant eating? |
| What have you found helps when this occurs? |
| What part do you play in how a feeding might go? |
As can be learned from the comparison of the high- and low-scoring mothers, focusing nursing interventions on categories of mothers such as low income or primiparae or mothers of infants who are extremely young gestationally at birth will not meet the need to help all mothers develop a safe, effective, supportive, and relational feeding practice. In particular, mothers of infants who have been in the nursery for a short time but who are now learning to nipple feed will not have had as many opportunities to come to know their infants. These mothers will need nursing support in providing care that is responsive to their particular infant.
In assessing mothers’ working models of co-regulation several “red flags” can be identified that can alert clinicians to the need for more in-depth feeding intervention. These indicators for targeted intervention include difficulty thinking about what feeding might be like for the infant; inability to describe what they contribute to the feeding; difficulty wondering what would make feeding go more smoothly; difficulty exploring new ideas such as the meaning of dribbling milk or noisy breathing; difficulty exploring alternative feeding strategies, such as what stopping the feeding to help the infant reorganize might do for the infant’s experience of feeding; or having limited criteria for a “good” feeding.
In conclusion, mothers’ thinking about their function as a co-regulator of infant feeding varies. The degree to which mothers understand themselves as co-regulators of their infants’ feeding will draw on mothers’ skill at taking their infants’ perspective, their view of their infants’ skill at expressing a participatory agenda, the mothers’ relational skills, how adept mothers are at having multiple and sometimes conflicting goals, and how well they can accomplish these goals while keeping their infants’ experience during feeding in the foreground. How the infant experiences feeding will lay a foundation for how the infant views feeding as he or she develops. Mothers’ notions of self as co-regulator of infant feeding will likely propel them to guide their infants’ development of an effective working model of feeding.
Acknowledgments
This study was supported by the National Institute of Nursing Research, Fellowship NR07052-02, and by the University of Wisconsin–Madison, School of Nursing.
References
- Ainsworth MDS, Bell SM. Some contemporary patterns of mother-infant interaction in the feeding situation. In: Anthony A, editor. Stimulation in early infancy. New York: Academic Press; 1969. [Google Scholar]
- Als H. Toward a synactive theory of development: Promise for the assessment and support of infant individuality. Infant Mental Health Journal. 1982;3:229–243. [Google Scholar]
- Als H. A synactive model of neonatal behavioral organization: Framework for the assessment of neurobehavioral development in the premature infant and support for infants and parents in the neonatal intensive care environment. Physical and Occupational Therapy in Pediatrics. 1986;3(4):3–53. [Google Scholar]
- Berger MM. Self-confrontation through video. American Journal of Psychoanalysis. 1971;31:48–58. doi: 10.1007/BF01872309. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss. 2. New York: Basic Books; 1982. Attachment. [Google Scholar]
- Bowlby J. A secure base. New York: Basic Books; 1988. [Google Scholar]
- Bretherton I. Pouring old wine into new bottles: The social self as internal working model. In: Gunnar MR, Sroufe LA, editors. Self processes and development; Minnesota symposia on child psychology; Hillside, NJ: Lawrence Erlbaum; 1991. pp. 1–41. [Google Scholar]
- Emde RN. Three roads intersecting: Changing view-points in the psychoanalytic story of Oedipus. In: Ammaniti M, Stern DN, editors. Psychoanalysis and development: Representations and narratives. New York: New York University Press; 1994. [Google Scholar]
- Fogel A. Developing through relationships. Chicago: University of Chicago Press; 1993. [Google Scholar]
- Gill NE, Behnke M, Conlon M, McNeely JB, Anderson GC. Effect of nonnutritive sucking on behavioral state in preterm infants before feeding. Nursing Research. 1988;37:347–350. [PubMed] [Google Scholar]
- Guilleminault C, Coons S. Apnea and bradycardia during feeding in infants weighing > 2000 grams. Journal of Pediatrics. 1984;104:932–934. doi: 10.1016/s0022-3476(84)80502-8. [DOI] [PubMed] [Google Scholar]
- Haase B. Unpublished master’s thesis. University of Wisconsin-Madison; 1992. Mothers’ internal working models of feeding infants with pulmonary disease. [Google Scholar]
- Kagan N, Schauble P, Resnikoff A, Danish SJ, Krathwohl DR. Interpersonal process recall. Journal of Nervous and Mental Disorders. 1969;148:365–374. doi: 10.1097/00005053-196904000-00004. [DOI] [PubMed] [Google Scholar]
- Martin R, Pridham KF. Early experiences of parents feeding their infants with bronchopulmonary dysplasia. Neonatal Network. 1992;11:23–29. [PubMed] [Google Scholar]
- Medoff-Cooper B, Verklan T, Carlson S. The development of sucking patterns and physiologic correlates in very-low-birth-weight infants. Nursing Research. 1993;42:100–105. [PubMed] [Google Scholar]
- Medoff-Cooper B, Weininger S, Zukowsky K. Neonatal sucking as a clinical assessment tool: Preliminary findings. Nursing Research. 1989;38:162–165. [PubMed] [Google Scholar]
- Meier PP. Bottle and breastfeeding: Effects on transcutaneous oxygen pressure and temperature in preterm infants. Nursing Research. 1988;37:36–41. [PubMed] [Google Scholar]
- Meier PP, Anderson GC. Responses of preterm infants to bottle and breastfeeding. MCN: American Journal of Maternal Child Nursing. 1987;12:420–423. doi: 10.1097/00005721-198703000-00006. [DOI] [PubMed] [Google Scholar]
- Pridham KF. Anticipatory guidance of parents of new infants: Potential contribution of the internal working model construct. Image: Journal of Nursing Scholarship. 1993;25:49–56. doi: 10.1111/j.1547-5069.1993.tb00753.x. [DOI] [PubMed] [Google Scholar]
- Pridham KF. Unpublished raw data. Research project funded by the National Institute of Nursing Research, NR02348–02. 1994. Correlates of preterm and term infant feeding outcomes. [Google Scholar]
- Pridham KF, Martin R, Sondel S, Tluczyk A. Parental issues in feeding young children with bronchopulmonary dysplasia. Journal of Pediatric Nursing. 1989;4:177–185. [PubMed] [Google Scholar]
- Pridham KF, Schroeder M, Brown R. The adaptiveness of mothers’ working models of caregiving through the first year: Infant and mother contributions. Research in Nursing and Health. 1999;22:471–485. doi: 10.1002/(sici)1098-240x(199912)22:6<471::aid-nur5>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Pridham KF, Schroeder M, Brown R, Clark R. The relationship to feeding behavior of a mother’s working model of caregiving in the context of infant and mother conditions. 2000. Manuscript submitted for publication. [Google Scholar]
- Pridham KF, Schroeder M, Van Riper M, Thoyre S, Limbo R, Mlynarczyk S. Unpublished manuscript. University of Wisconsin-Madison School of Nursing; 1999. Working model of feeding: An interview protocol and coding manual. [Google Scholar]
- Rosen CL, Glaze DG, Frost JD. Hypoxemia associated with feeding in the preterm infant and full-term neonate. American Journal of Diseases of Children. 1984;138:623–628. doi: 10.1001/archpedi.1984.02140450005002. [DOI] [PubMed] [Google Scholar]
- Schatzman L. Dimensional analysis: Notes on an alternative approach to the grounding of theory in qualitative research. In: Maines DR, editor. Social organization and social process: Essays in honor of Anselm Strauss. New York: Aldine De Gruyier; 1991. pp. 303–314. [Google Scholar]
- Shaker CS. Nipple feeding preterm infants: An individualized, developmentally supportive approach. Neonatal Network. 1999;18(3):15–22. doi: 10.1891/0730-0832.18.3.15. [DOI] [PubMed] [Google Scholar]
- Shiao SPK, Brooker J, DiFiore T. Desaturation events during oral feedings with and without a naso-gastric tube in very low birth weight infants. Heart and Lung. 1996;25:236–245. doi: 10.1016/s0147-9563(96)80034-3. [DOI] [PubMed] [Google Scholar]
- Shivpuri CR, Martin RJ, Carlo WA, Fanaroff AA. Decreased ventilation in preterm infants during oral feeding. Journal of Pediatrics. 1983;103:285–289. doi: 10.1016/s0022-3476(83)80368-0. [DOI] [PubMed] [Google Scholar]
- Singer L, Martin RJ, Hawkins SW, Benson-Szekely LJ, Yamashita TS, Carlo WA. Oxygen desaturation complicates feeding in infants with bronchopulmonary dysplasia after discharge. Pediatrics. 1992;90:380–384. [PMC free article] [PubMed] [Google Scholar]
- Thoyre S. Challenges mothers identify in bottle feeding their preterm infants. Neonatal Network. doi: 10.1891/0730-0832.20.1.45. (in press) [DOI] [PubMed] [Google Scholar]
- Thoyre S. Unpublished doctoral dissertation. University of Wisconsin-Madison; 1997. Co-regulation of very low birthweight infant feeding. [Google Scholar]
- Thoyre S, Carlson J. Preterm infant behaviors during bottle-feeding oxygen desaturation events. Paper presented at the annual meeting of the Southern Nursing Research Society; Little Rock, AR. 2000. Feb, [Google Scholar]
- Thoyre S, Pridham KF. Learning to feed preterm infants in the NICU: Parents’ perspectives. Poster presented at the Midwest Nursing Research Society Conference; Milwaukee, WI. 1994. Apr, [Google Scholar]
- White-Traut RC, Nelson MN. Maternally administered tactile, auditory, visual, and vestibular stimulation: Relationship to later interactions between mothers and premature infants. Research in Nursing and Health. 1988;11:31–39. doi: 10.1002/nur.4770110106. [DOI] [PubMed] [Google Scholar]


