Abstract
Background
Texture analysis is a promising method of analyzing imaging data to potentially enhance diagnostic capability. This approach involves automated measurement of pixel intensity variation that may offer further insight into disease progression than standard imaging techniques alone. We postulate that postoperative liver insufficiency, a major source of morbidity and mortality, correlates with preoperative heterogeneous parenchymal enhancement that can be quantified with texture analysis of cross-sectional imaging.
Study Design
A retrospective case-matched study (waiver of informed consent and HIPAA authorization, approved by the institutional review board) was performed comparing patients who underwent major hepatic resection and developed liver insufficiency (n=12) to a matched group of patients with no postoperative liver insufficiency (n=24) by procedure, remnant volume, and year of procedure. Texture analysis (with gray-level co-occurrence matrices) was used to quantify the heterogeneity of liver parenchyma on preoperative computed tomography (CT) scans. Statistical significance was evaluated using Wilcoxon’s signed rank and Pearson’s chi-squared tests.
Results
No statistically significant differences were found between study groups for preoperative patient demographics and clinical characteristics, with the exception of gender (p<0.05). Two texture features differed significantly between the groups: correlation (linear dependency of gray levels on neighboring pixels) and entropy (randomness of brightness variation) (p<0.05).
Conclusions
In this preliminary study, the texture of liver parenchyma on preoperative CT, was significantly more varied, less symmetric, and less homogeneous in patients with postoperative liver insufficiency; thus texture analysis has the potential to provide an additional means of preoperative risk stratification.
Introduction
Partial hepatectomy is the most effective and the only potentially curative treatment for selected primary and secondary hepatic tumors. Despite significant improvements in perioperative outcome, postoperative liver insufficiency remains a source of morbidity and mortality, particularly for major resections [1, 2]. Complication rates increase directly with extent of resection, with one center reporting a 30% rate of severe hepatic insufficiency when five or more segments are resected [3]. Because postoperative hepatic insufficiency can delay chemotherapy, prolong hospital stay, and increase the overall risk of cancer recurrence, it is important to identify patients at risk prior to surgery.
Several studies have shown that the percentage of functional liver parenchyma remaining after surgery predicts postoperative hepatic insufficiency [3–5], but such analyses are far from perfect as they do not address the functional capacity of the parenchyma. Passive function tests such as biochemical parameters (bilirubin, albumin, and coagulation factor synthesis) and clinical grading systems (Child-Pugh and MELD), while capable of identifying severe hepatic parenchymal disease, are not useful predictors of perioperative outcome in candidates for resection [6]. Dynamic quantitative liver function tests, such as indocyanine green clearance and galactose elimination capacity, are thought to be more reliable, since the elimination/metabolization of these substances occurs almost exclusively in the liver [6]; however, several studies of these tests have shown no significant correlation with clinical outcome and histologic results [7, 8]. Cross-sectional imaging studies are typically used to assess liver volumetry and to detect steatosis or cirrhosis, but few metrics exist for quantifying liver functional capacity from images [9]. Very recently, gadoxetic acid uptake in MR imaging has shown promise for assessment of liver insufficiency by identifying 3 patients with liver insufficiency out of 73 who underwent liver resection [10]. Reliable prediction of postoperative liver insufficiency thus remains a difficult, inexact practice.
Texture analysis is an established technique that characterizes regions of interest in an image by spatial variations in pixel intensities. For example, a smooth or homogeneous image lacks pixel intensity variation, whereas an irregular or heterogeneous image has many pixel intensities and is richly textured. In the context of computed tomography (CT) images, texture analysis has the potential to quantify regional variations in enhancement that cannot be qualified by inspection. Recent studies describe texture analysis to augment lesion diagnosis and characterization [11], predict survival of colorectal cancer patients [12, 13], and classify hepatic tumors [14]. Texture analysis of liver parenchyma has been studied for fibrosis detection and correlated with postoperative pathologic findings [15] [16].
Texture analysis of preoperative CT images has not been used to predict post-hepatectomy liver insufficiency. Our hypothesis is that underlying liver insufficiency is correlated with heterogeneous parenchymal enhancement, which can be quantified by texture analysis. The purpose of our study is to determine if the preoperative CT texture of liver parenchyma differed between patients with and without postoperative liver insufficiency. By quantifying underlying parenchymal differences preoperatively, texture analysis has the potential to provide an additional, and potentially powerful, means of patient risk stratification.
Patients and Methods
Patients
A waiver of Health Insurance Portability and Accountability Act authorization and informed consent was obtained through Institutional Review Board approval. The prospectively maintained liver resection database was queried for all patients that underwent major hepatic resection (≥4 segments) between January 2006 and January 2012. Prospectively collected demographic, laboratory, histopathologic, operative, perioperative, and radiologic data were analyzed retrospectively. Preoperative evaluation, intraoperative management, and conduct of the operation have been described previously [2]. Morbidity was noted and graded using a scale consistent with the Common Terminology Criteria for Adverse Events from the National Cancer Institute [17].
Study Design
Case-matched study design was used in an attempt to eliminate possible confounding effects of clinically established factors associated with postoperative hepatic insufficiency. Comparisons were performed between the patients who underwent major hepatic resection with postoperative liver insufficiency complications and a matched group of patients with no postoperative liver insufficiency. Patients were matched 2:1 by procedure (right lobectomy or right trisegmentectomy), remnant liver volume (RLV, defined as the ratio of the remaining functional liver volume to the preoperative functional liver volume, expressed as a percentage), and year of procedure.
Postoperative Liver Dysfunction and Failure Classification
Patients with postoperative liver insufficiency between 2006 and 2012 were identified from the database. Postoperative liver insufficiency was defined as the presence of the following: total bilirubin greater than 4.1 mg/dL without obstruction or bile leak, INR>2.5, ascites (drainage >500 mL/day), or encephalopathy with hyperbilirubinemia. The severity of liver insufficiency was assessed using the surgical events database scale [17].
Postoperative Staging and Follow-up
Steatosis was graded in the course of routine histopathologic assessment based on the Kleiner-Brunt histologic scoring system: mild (<33% of hepatocytes affected), moderate (33–66% of hepatocytes affected), or severe (>66% of hepatocytes affected) [18]. Fibrosis was graded based on the Rubbia-Brandt classification [19].
Computed Tomography Images
Patients with conventional portal venous phase contrast-enhanced CT imaging prior to surgery were included in the study. Post-contrast CT images were obtained following the administration of 150 mL iodinated contrast (Omnipaque 300, GE Healthcare, New Jersey) at 2.5 mL/sec, on multidetector CT (Lightspeed 16 and VCT, GE Healthcare, Wisconsin), as is the standard imaging protocol at our institution. The following scan parameters were used: pitch/table speed = 0.984–1.375/39.37–27.50 mm; autoMA 220–380; noise index 12–14; rotation time 0.7–0.8 ms; scan delay 80 s. Axial slices reconstructed at each 5 mm interval were used for the analysis. The entire liver was scanned on each CT.
Image Processing
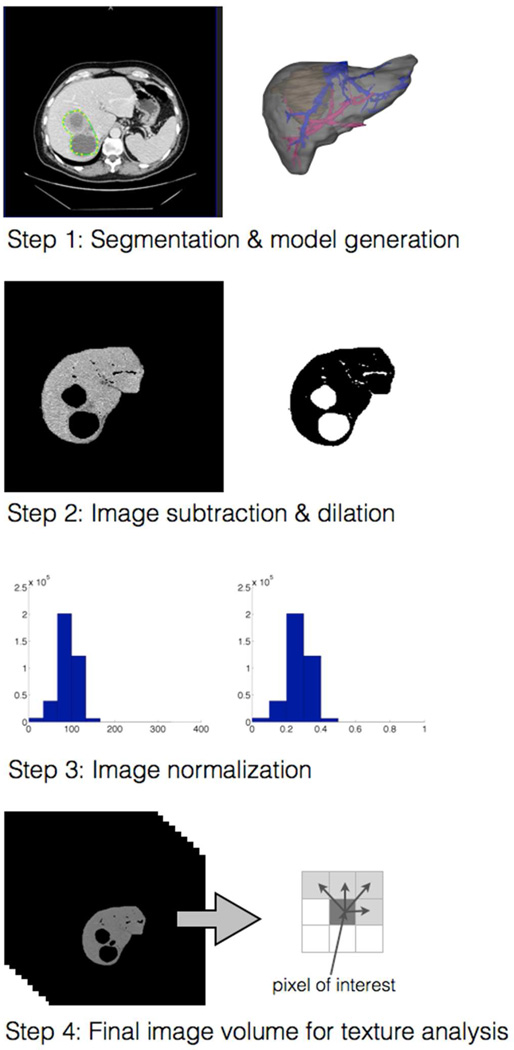
Standard image processing techniques were used to extract the liver parenchyma from surrounding structures (Fig. 1). Liver, tumors, vessels, and bile ducts were semi-automatically segmented from CT scans using Scout Liver (Pathfinder Technologies Inc., Tennessee). The remainder of the image processing was fully automated with software custom-developed for the study: parenchyma was separated from other structures using image subtraction, attenuation values outside of 0 and 300 threshold HU (corresponding to non-parenchymal regions, such as bulk fat and metal) were removed using image thresholding, image dilation and erosion operators slightly expanded the tumor and vessel boundaries to compensate for potential small inaccuracies in the segmentation. The final volume was scaled using conventional image normalization, which compensates for potential irregularities in the scale of pixel values across image volumes while conserving the appearance of the image [20].
Fig. 1.
Steps in the quantification of preoperative CT images for prediction of postoperative hepatic insufficiency, from image segmentation (step 1) to texture analysis (step 4).
Texture Analysis
Texture analysis was undertaken to characterize the statistical variation in the spatial relationships of pixels in these parenchymal regions using standard gray-level co-occurrence matrices (GLCM) [21–23]. The GLCM represents the number of neighboring pixel brightness values (gray levels) at specified distances in the image. Once the GLCM is constructed, standard features can be extracted using well-defined statistics. Five statistics were used: contrast (local variation), correlation (brightness interdependence on neighboring pixels), energy (local homogeneity), entropy (randomness in brightness variation), and homogeneity.
Statistical Analysis
Clinical variables were expressed as mean (with standard deviation) or median (with range), as appropriate. Texture features were expressed as mean (with 95% confidence interval). Differences between the matched groups with respect to the clinical variables and texture features were determined using Wilcoxon’s signed rank test for continuous variables and Pearson’s chi-squared test for categorical variables where p<0.05 defined statistical significance. All statistical analyses were performed with SPSS version 21 (IBM Corporation). The percentage difference between the texture features in the liver insufficiency (LI) and no liver insufficiency (NLI) study groups was expressed as: % difference = (mean LI – mean NLI) × (100/mean NLI) to show the relative differences between the two groups.
Results
Demographics
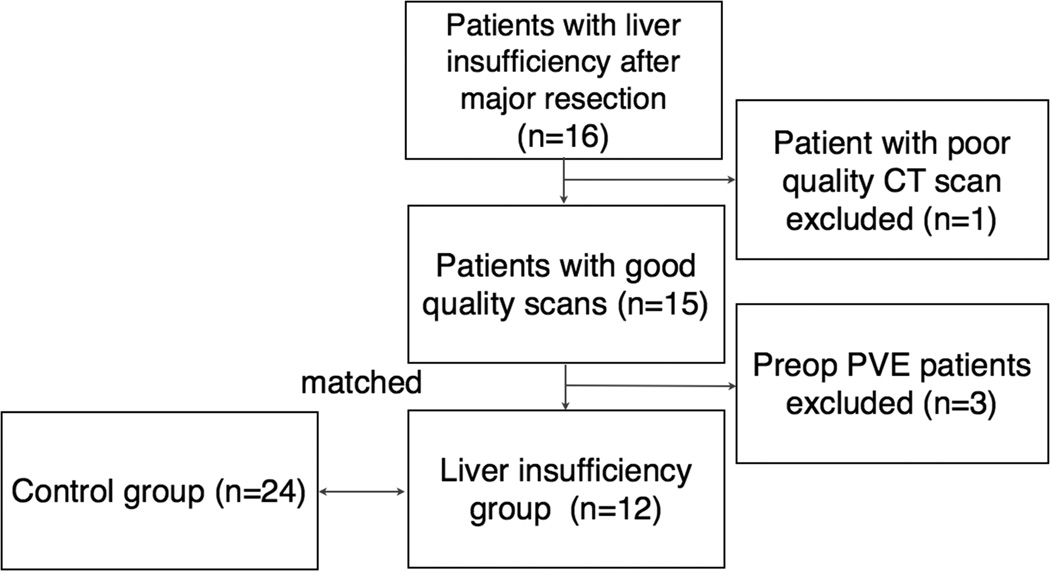
Sixteen patients with liver insufficiency following major hepatic resection from January 2006 to January 2012 were identified from the liver resection patient database of 1,721 resections (0.9%) and 467 major resections (3.4%). Three patients underwent preoperative portal vein embolization and were excluded due to the potential confounding influence of embolization-induced parenchymal changes on texture analysis. One additional patient was excluded based on a poor quality scan. All patients had undergone routine portal venous phase contrast-enhanced CT prior to surgery. The remaining 12 patients were matched to a control group of 24 patients, for a total cohort of 36 patients. The inclusion/exclusion flow diagram is summarized in Fig. 2.
Fig. 2.
Study profile demonstrating patient selection. PVE, portal vein embolization.
Patient demographics and clinicopathologic factors are presented in Table 1. Comparisons were made between the LI and the NLI groups to reveal potential biases in the study group selection. The median age, weight, height, and body mass index did not significantly differ between the two groups; however, patients in the LI group were more likely to be male (92%, p<0.05) with slightly larger body surface area (LI: 2.0 m2 vs. NLI: 1.8 m2, p<0.05). Preoperative bilirubin level, history of preoperative chemotherapy, and type of chemotherapy did not significantly differ between groups. The extent of resection did not significantly differ between the two groups: half of patients in each group underwent right hepatectomy and the other half underwent extended right hepatectomy, with mean RLV of 37.1% in the LI group vs. 41.5% in the NLI group (p=0.517).
Table 1.
Demographic and Clinicopathologic Factors
| All patients (n=36) |
NLI (n=24) | LI (n=12) | p Value | |
|---|---|---|---|---|
| Age, y (range) | 63 (54–73) | 62 (53–73) | 66 (56–75) | - |
| Sex, n (%) | < 0.05 | |||
| Male | 21 (58) | 10 (42) | 11 (92) | - |
| Female | 15 (42) | 14 (58) | 1 (8) | - |
| Weight, kg (range) | 80 (63–98) | 70 (61–92) | 92 (77–99) | - |
| Body mass index, kg/m2 (range) | 27.9 (23.1–31.2) | 26.7 (22.2–30.1) | 29.6 (26.3–32.4) | - |
| Preoperative bilirubin, mg/dL (mean ± SD) | 0.8 ± 0.6 | 0.7 ± 0.5 | 1.0 ± 0.6 | - |
| Preoperative chemotherapy, n (%) | 17 (47) | 13 (54) | 4 (33) | - |
| Type of preoperative chemotherapy, n (%) | ||||
| FOLFOX | 7 (19) | 6 (25) | 1 (8) | - |
| FUDR/Irinotecan | 2 (6) | 1 (4) | 1 (8) | - |
| Irinotecan | 1 (3) | - | 1 (8) | - |
| Bleomycin/Etoposide/Cisplatin | 1 (3) | 1 (4) | - | - |
| Cisplatin/Gemcitabine | 1 (3) | - | 1 (8) | - |
| Taxotere/Herceptin | 1 (3) | 1 (4) | - | - |
| Irinotecan/Cetuximab | 1 (3) | 1 (4) | - | |
| Gemcitabine/Taxotere; Doxorubicin/Decarbazine | 1 (3) | 1 (4) | - | |
| Procedure, n (%) | ||||
| Right lobectomy | 18 (50) | 12 (50) | 6 (50) | - |
| Right trisegmentectomy | 18 (50) | 12 (50) | 6 (50) | - |
| RLV (%), mean ± SD | 40.1 ± 13.7 | 41.5 ± 14.1 | 37.1 ± 13.1 | - |
| Mortality, n (%) | 6 (17) | - | 6 (50) | < 0.01 |
| Major complications, n (%) | 14 (39) | 6 (25) | 8 (67) | |
| Margin status, n (%) | ||||
| Negative | 35 (97) | 24 (100) | 11 (92) | - |
| Positive | 1 (3) | - | 1 (8) | - |
| Diagnosis, n (%) | ||||
| CRC | 20 (56) | 11 (46) | 9 (75) | - |
| Cholangiocarcinoma | 10 (28) | 7 (29) | 3 (25) | - |
| HCC | 3 (8) | 3 (13) | - | - |
| Other disease* | 3 (8) | 3 (13) | - | - |
| Steatosis, n (%) | 18 (50) | 12 (50) | 6 (50) | - |
| Fibrosis, n (%) | 4 (11) | 2 (8) | 2 (17) | - |
Testicular, breast, and duodenal.
NLI, no liver insufficiency; LI, liver insufficiency; RLV, remnant liver volume; CRC, colorectal cancer; HCC, hepatocellular carcinoma.
Major complications (≥grade 3) were observed in 14 patients for an overall complication rate of 39% with no differences between the two groups; however, the 90-day mortality rate was significantly higher in the LI group (50%, n=6) (p<0.01).
Pathologic characteristics were not statistically different between the two groups. Overall, the majority of patients were diagnosed with metastatic colorectal cancer (56%, n=20), followed by cholangiocarcinoma (28%, n=10), hepatocellular carcinoma (8%, n=3), and other metastatic disease [testicular (3%, n=1), breast (3%, n=1), duodenal (3%, n=1)]. Postoperative margin status was negative in all but one patient.
Texture
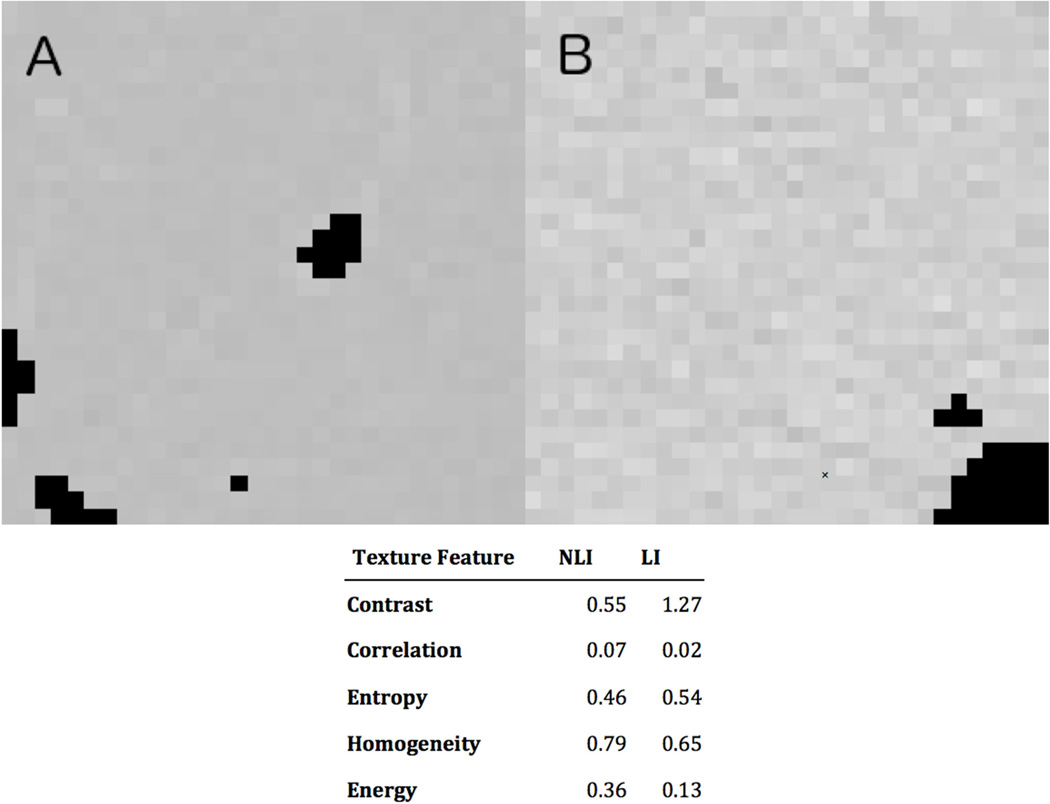
Two texture features in the control group (n=24) were significantly different (p<0.05) from those in the LI group (n=12). Compared to features in the control group, the contrast and entropy features increased in the patients with liver insufficiency, whereas the correlation, energy, and homogeneity features decreased in value (Table 2). Contrast, a measure of local variation in the image, showed greater range in values in the LI group than in the control group. Correlation is a measure of the linear dependency of gray levels on neighboring pixels, with higher values indicating greater similarity in gray-level regions; the control group had much less variation than the LI group (p<0.05). Entropy, a measure of randomness in brightness variation, was greater in the LI group (p<0.05). Homogeneity was somewhat lower in the LI group, but this difference was not statistically significant.
Table 2.
Comparison of CT Texture Features (Mean, 95% Confidence Interval) for Patients with No Postoperative Liver Insufficiency and Patients with Liver Insufficiency
| Texture Feature | NLI (n=24) | LI (n=12) | % Difference | p Value |
|---|---|---|---|---|
| Contrast | 0.65 (0.47, 0.82) | 0.97 (0.54, 1.40) | 49 | 0.098 |
| Correlation | 0.04 (0.03, 0.05) | 0.02 (0.00, 0.03) | −50 | <0.05* |
| Energy | 0.40 (0.27, 0.53) | 0.37 (0.12, 0.62) | −8 | 0.106 |
| Entropy | 0.50 (0.45, 0.55) | 0.58 (0.51, 0.65) | 16 | <0.05* |
| Homogeneity | 0.79 (0.74, 0.83) | 0.75 (0.64, 0.85) | −5 | 0.091 |
Significant.
NLI, no liver insufficiency; LI, liver insufficiency; % Difference = (mean LI − mean NLI) × (100/mean NLI).
To summarize, the texture of the liver parenchyma from preoperative CT images of patients with postoperative liver insufficiency was significantly more varied and less homogeneous than that of the control group (Fig. 3).
Fig. 3.
Comparison of 32 × 32 preoperative CT textures (pixel distance = 24). (A) Patient with no postoperative liver insufficiency and (B) Patient with postoperative liver insufficiency. Black areas indicate non-parenchymal regions (vessels, tumors, cysts) excluded from analysis. NLI, no liver insufficiency; LI, liver insufficiency.
Discussion
Partial hepatic resection remains an effective and relatively safe procedure for carefully selected patients. Over the last two decades, increased use of parenchymal-sparing techniques in resections has reduced perioperative morbidity and mortality [2]. However, postoperative liver insufficiency remains a grave concern, since up to 75% of postoperative mortalities are related to postoperative liver insufficiency [24]. In addition to human factors, one study reported a three-fold increase in the total costs associated with the clinical management of postoperative liver failure patients [25]. Preventing liver insufficiency is the dominant theme of liver surgery, since treatment options for this condition are limited and associated mortality rates are high; however, an objective measure of parenchymal quality remains elusive.
The principal finding of this study is that preoperative CT texture of liver parenchyma of patients who experience liver insufficiency postoperatively differs significantly from the preoperative CT texture of patients who do not. Preoperative patient characteristics in the study groups were similar, highlighting the potential role of texture analysis to stratify risk groups prior to surgery. Although the basic definition of postoperative liver insufficiency is debated [24], six of twelve patients (50%) in the LI group died within 90 days of surgery. These six patients developed liver insufficiency as the initial event in the cascade of events that ultimately led to their deaths. Therefore, the definition applied in this study clearly identified the population at high risk for poor perioperative outcome.
Textural differences between livers of patients with and without insufficiency may arise from a combination of factors beyond intrinsic liver parenchymal properties. A limitation of using routine portal venous phase CT for liver texture analysis is the arbitrary and fixed time point at which these abdominal CTs are performed. At our institution, a fixed delay of 80 s is used for the portal venous phase, but certain patient variables may affect the degree of liver parenchymal enhancement, such as cardiac output, or hepatic venous congestion. Normalizing the histogram of pixel intensities before performing texture analysis will reduce the effect of differences in the magnitude of liver enhancement given our fixed dose of contrast, but may not eliminate the textural differences due to extrahepatic patient factors. This limitation also raises the possibility that performing similar analyses at multiple time points after contrast injection may help define an optimal time point to distinguish between patients with high or low risk for postoperative liver insufficiency by parenchymal texture analysis.
We chose to quantify CT images via texture analysis with GLCM methods for several reasons. First, texture analysis with GLCM is well defined and has been studied for more than three decades, with numerous applications supporting their use [20, 25]. Second, perceptual studies have shown this method to correspond to some level of human perception [26]. Third, GLCM continue to outperform other methods of texture classification [27]. Fourth, these quantitative imaging features have been shown to improve tumor diagnosis [11, 14], and to provide measures of response assessment [28, 29] and radiation-induced gland injury [30], and are reproducible across multiple imaging units [31]. Lastly, and perhaps most relevant to the present study, recent investigations have shown that CT texture relates to fibrosis staging [15, 16] so the extension to liver insufficiency is not unexpected.
Our methods differ from those in prior studies of hepatic texture. Instead of the GLCM methods employed here, many studies utilize edge detection techniques [12, 13], which rely on analysis of abrupt brightness changes rather than on statistical variation of brightness in a neighborhood. Brightness variation in liver parenchymal regions on CT represents subtle changes in uptake of intravenous contrast. Analysis of brightness variation, as described in this paper, may provide a better assessment of underlying parenchymal health. In contrast, edge detection techniques may be more suitable for tumor detection. In the present study, non-parenchymal regions (vessels, cysts, etc.) were excluded from analysis: including these high-contrast regions could potentially bias measurement of brightness variation. For example, contrast-to-noise ratios calculated between the most hyper- and hypo-intense regions of the liver have been correlated with fibrosis [32] but the effect of the presence of vascular structures on texture features is unstudied.
Analysis of patient and treatment factors determined that only texture features appear to predict liver insufficiency in this cohort. Other studies of hepatic texture do not report analysis of these patient and treatment factors [12, 13] that may represent surrogates of hepatic texture values. To our knowledge, this is the first study to relate texture features to postoperative outcome. The ability to predict hepatic behavior prior to treatment has the potential to inform risk stratification for patients under consideration for resection and possibly to assess the risk of liver injury in patients undergoing initial treatment with chemotherapy. Although new imaging protocols and contrast agents are in development, CT remains the primary imaging modality for oncology patients and CT images are potentially rich with additional useful information beyond anatomic data.
The underlying mechanism as to why preoperative analysis of liver texture can inform postoperative liver failure risk remains to be elucidated. The proposed method provides a quantitative approach to measuring the heterogeneity of liver parenchymal enhancement. Differences in parenchymal heterogeneity are a reflection of the variability in the distribution of intravenously administered contrast. This variability likely reflects a combination of factors, including changes to the microvasculature that often occur from the presence of metastatic disease as well as the chemotherapy used to treat it. Since our two patient groups did not substantially differ in type of malignancies or chemotherapies used, our texture analysis may reflect the accumulated microvascular injury, not appreciated on routine histology, but possibly associated with high risk of liver insufficiency after resection.
The major limitations of this study were the retrospective design and also the low number of patients in the LI group (n=12) for analysis because liver insufficiency is a relatively rare event at our institution due to careful preoperative patient selection. Further analysis of patient factors that may influence parenchymal changes such as steatosis and fibrosis in a large series of patients undergoing liver resection is needed to identify the effect of parenchymal changes on texture. Patients with preoperative portal vein embolization were excluded in this study due to the unstudied effects of these treatment strategies on parenchymal texture. Analysis could be performed on pre-treatment scans, provided that these scans were timed sufficiently; however, this is for future work and not addressed in this preliminary study. Despite these limitations, the data show that analysis of texture is a promising predictor of postoperative hepatic insufficiency; a comprehensive, prospective, and well-powered study is needed to confirm these results. The increasing use of preoperative chemotherapy suggests that post-hepatectomy liver insufficiency will likely remain a major problem. In tumor types with higher risk of liver insufficiency, such as hilar cholangiocarcinoma [33], the proposed technique may show much broader applicability in a larger prospective study.
Conclusions
Differences in enhancement in hepatic parenchyma can be quantified by texture analysis from underlying pixel variations on portal venous phase CT scans. These parenchymal differences in preoperative CT scans appear to correlate with postoperative insufficiency following major hepatic resections. These results have the potential to improve preoperative risk stratification by adding a measure of liver parenchymal quality to the standard assessments of liver remnant volume.
Acknowledgments
Ms Parada received a consulting fee from Pathfinder Technologies, Inc. and was previously employed by them; Dr Miga received payments for patents and licensing fees from Pathfinder Therapeutics Inc. and holds less than 1% equity in the company.
Support: The National Cancer Institute grant number R01 CA162477 supports Drs Simpson and Miga.
Abbreviations & Acronyms
- CT
computed tomography
- GLCM
gray-level co-occurrence matrix
- LI
liver insufficiency
- NLI
no liver insufficiency
- RLV
remnant liver volume
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Information: All other authors have nothing to disclose.
Presented at the Annual Meeting for the Society of Abdominal Radiology, Boca Raton, FL, March 2014.
References
- 1.Dokmak S, Fteriche FS, Borscheid R, et al. 2012 Liver resections in the 21st century: we are far from zero mortality. HPB. 2013;15:908–915. doi: 10.1111/hpb.12069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jarnagin WR, Gonen M, Fong Y, et al. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg. 2002;236:397–406. doi: 10.1097/01.SLA.0000029003.66466.B3. discussion -407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schindl MJ, Redhead DN, Fearon KCH, et al. The value of residual liver volume as a predictor of hepatic dysfunction and infection after major liver resection. Gut. 2005;54:289–296. doi: 10.1136/gut.2004.046524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kishi Y, Abdalla EK, Chun YS, et al. Three hundred and one consecutive extended right hepatectomies: evaluation of outcome based on systematic liver volumetry. Ann Surg. 2009;250:540–548. doi: 10.1097/SLA.0b013e3181b674df. [DOI] [PubMed] [Google Scholar]
- 5.Shoup M, Gonen M, D'Angelica M, et al. Volumetric analysis predicts hepatic dysfunction in patients undergoing major liver resection. J Gastrointest Surg. 2003;7:325–330. doi: 10.1016/s1091-255x(02)00370-0. [DOI] [PubMed] [Google Scholar]
- 6.Hoekstra LT, de Graaf W, Nibourg GA, et al. Physiological and biochemical basis of clinical liver function tests: a review. Ann Surg. 2013;257:27–36. doi: 10.1097/SLA.0b013e31825d5d47. [DOI] [PubMed] [Google Scholar]
- 7.Lam CM, Fan ST, Lo CM, Wong J. Major hepatectomy for hepatocellular carcinoma in patients with an unsatisfactory indocyanine green clearance test. Br J Surg. 1999;86:1012–1017. doi: 10.1046/j.1365-2168.1999.01204.x. [DOI] [PubMed] [Google Scholar]
- 8.Wong JSW, Wong GLH, Chan AWH, et al. Liver stiffness measurement by transient elastography as a predictor on posthepatectomy outcomes. Ann Surg. 2013;257:922–928. doi: 10.1097/SLA.0b013e318269d2ec. [DOI] [PubMed] [Google Scholar]
- 9.Marsman HA, van der Pool AE, Verheij J, et al. Hepatic steatosis assessment with CT or MRI in patients with colorectal liver metastases after neoadjuvant chemotherapy. J Surg Oncol. 2011;104:10–16. doi: 10.1002/jso.21874. [DOI] [PubMed] [Google Scholar]
- 10.Wibmer A, Prusa AM, Nolz R, et al. Liver failure after major liver resection: risk assessment by using preoperative gadoxetic acid-enhanced 3-T MR imaging. Radiology. 2013;269:777–786. doi: 10.1148/radiol.13130210. [DOI] [PubMed] [Google Scholar]
- 11.Davnall F, Yip CS, Ljungqvist G, et al. Assessment of tumor heterogeneity: an emerging imaging tool for clinical practice? Insights into Imaging. 2012;3:573–589. doi: 10.1007/s13244-012-0196-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miles KA, Ganeshan B, Griffiths MR, et al. Colorectal cancer: texture analysis of portal phase hepatic CT images as a potential marker of survival. Radiology. 2009;250:444–452. doi: 10.1148/radiol.2502071879. [DOI] [PubMed] [Google Scholar]
- 13.Ganeshan B, Burnand K, Young R, et al. Dynamic contrast-enhanced texture analysis of the liver: initial assessment in colorectal cancer. Investigative Radiol. 2011;46:160–168. doi: 10.1097/RLI.0b013e3181f8e8a2. [DOI] [PubMed] [Google Scholar]
- 14.Huang YL, Chen JH, Shen WC. Diagnosis of hepatic tumors with texture analysis in nonenhanced computed tomography images. Acad Radiol. 2006;13:713–720. doi: 10.1016/j.acra.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 15.Romero-Gomez M, Gomez-Gonzalez E, Madrazo A, et al. Optical analysis of computed tomography images of the liver predicts fibrosis stage and distribution in chronic hepatitis C. Hepatology. 2008;47:810–816. doi: 10.1002/hep.22112. [DOI] [PubMed] [Google Scholar]
- 16.Barry B, Buch K, Soto JA, et al. Quantifying liver fibrosis through the application of texture analysis to diffusion weighted imaging. Magnetic Resonance Imaging. 2014;32:84–90. doi: 10.1016/j.mri.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 17.Martin RC, Jaques DP, Brennan MF, Karpeh M. Achieving RO resection for locally advanced gastric cancer: is it worth the risk of multiorgan resection? J Am Coll Surg. 2002;194:568–577. doi: 10.1016/s1072-7515(02)01116-x. [DOI] [PubMed] [Google Scholar]
- 18.Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–1321. doi: 10.1002/hep.20701. [DOI] [PubMed] [Google Scholar]
- 19.Rubbia-Brandt L, Audard V, Sartoretti P, et al. Severe hepatic sinusoidal obstruction associated with oxaliplatin-based chemotherapy in patients with metastatic colorectal cancer. Ann Oncol. 2004;15:460–466. doi: 10.1093/annonc/mdh095. [DOI] [PubMed] [Google Scholar]
- 20.Russ JC. The image processing handbook. 6th ed. Boca Raton: CRC Press; 2011. p. xviii.p. 867. [Google Scholar]
- 21.Haralick RM, Shanmugam K, Dinstein IH. Textural Features for Image Classification. Systems, Man and Cybernetics, IEEE Transactions on. 1973;SMC-3(6):610–621. [Google Scholar]
- 22.Haralick RM. Statistical and structural approaches to texture. Proceedings of the IEEE. 1979;67:786–804. [Google Scholar]
- 23.Soh LK, Tsatsoulis C. Texture analysis of SAR sea ice imagery using gray level co-occurrence matrices. Geoscience and Remote Sensing, IEEE Transactions on. 1999;37:780–795. [Google Scholar]
- 24.van den Broek MA, Olde Damink SW, Dejong CH, et al. Liver failure after partial hepatic resection: definition, pathophysiology, risk factors and treatment. Liver Int. 2008;28:767–780. doi: 10.1111/j.1478-3231.2008.01777.x. [DOI] [PubMed] [Google Scholar]
- 25.Tuceryan M, Jain AK. Texture Analysis. In: Chen CH, Pau LF, Wang PSP, editors. Handbook of pattern recognition & computer vision. 2nd ed. River Edge, NJ: World Scientific; 1998. pp. 207–248. [Google Scholar]
- 26.Julesz B, Gilbert EN, Shepp LA, Frisch HL. Inability of humans to discriminate between visual textures that agree in second-order statistics-revisited. Perception. 1973;2:391–405. doi: 10.1068/p020391. [DOI] [PubMed] [Google Scholar]
- 27.Ohanian PP, Dubes RC. Performance evaluation for four classes of textural features. Pattern Recognition. 1992;25:819–833. [Google Scholar]
- 28.Harrison LC, Luukkaala T, Pertovaara H, et al. Non-Hodgkin lymphoma response evaluation with MRI texture classification. J Experiment Clin Cancer Res. 2009;28:87. doi: 10.1186/1756-9966-28-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O'Connor JP, Rose CJ, Jackson A, et al. DCE-MRI biomarkers of tumour heterogeneity predict CRC liver metastasis shrinkage following bevacizumab and FOLFOX-6. Br J Cancer. 2011;105:139–145. doi: 10.1038/bjc.2011.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang X, Tridandapani S, Beitler JJ, et al. Ultrasound GLCM texture analysis of radiation-induced parotid-gland injury in head-and-neck cancer radiotherapy: an in vivo study of late toxicity. Med Phys. 2012;39:5732–5739. doi: 10.1118/1.4747526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hunter LA, Krafft S, Stingo F, et al. High quality machine-robust image features: Identification in nonsmall cell lung cancer computed tomography images. Med Phys. 2013;40:121–916. doi: 10.1118/1.4829514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aguirre DA, Behling CA, Alpert E, et al. Liver fibrosis: noninvasive diagnosis with double contrast material–enhanced MR imaging. Radiology. 2006;239:45–37. doi: 10.1148/radiol.2392050505. [DOI] [PubMed] [Google Scholar]
- 33.Ratti F, Cipriani F, Ferla F, et al. Hilar cholangiocarcinoma: preoperative liver optimization with multidisciplinary approach. Toward a better outcome. World J Surg. 2013;37:1388–1396. doi: 10.1007/s00268-013-1980-2. [DOI] [PubMed] [Google Scholar]