Abstract
Bile acids (BAs) are endogenous agents capable of causing cancer throughout the gastrointestinal (GI) tract. To uncover the mechanism by which BAs exert carcinogenic effects, both human liver and colon cancer cells as well as mouse primary hepatocytes were treated with BAs and assayed for viability, genotoxic stress, and transcriptional response. BAs induced both Nur77 (NR4A1) and pro-inflammatory gene expression. The intracellular location of BA-induced Nur77 was time-dependent; short-term (1–3 h) exposure induced nuclear Nur77 whereas longer (1–2 days) exposure also increased cytosolic Nur77 expression and apoptosis. Inhibiting Nur77 nuclear export with leptomycin B decreased LCA-induced apoptosis. Extended (7 days) treatment with BA generated resistance to BA with increased nuclear Nur77, viability, and mobility. While, knockdown of Nur77 in BA-resistant cells increased cellular susceptibility to LCA-induced apoptosis. Moreover, in vivo mouse xenograft experiments demonstrated that BA-resistant cells form larger tumors with elevated Nur77 expression compared to parental controls. DNA-binding and gene expression assays identified multiple survival genes (CDK4, CCND2, MAP4K5, STAT5A, and RBBP8) and a pro-apoptosis gene (BID) as Nur77 targets. Consistently, BA-induced up-regulation of the aforementioned genes was abrogated by a lack of Nur77. Importantly, Nur77 was overexpressed in high percentage of human colon and liver cancer specimens and the intracellular location of Nur77 correlated with elevated serum total BA levels in colon cancer patients. These data show for the first time that BAs via Nur77 have a dual role in modulating cell survival and death.
Implications: These findings establish a direct link between Nur77 and the carcinogenic effect of bile acids.
Keywords: Nuclear receptor, gastrointestinal cancer, DNA damage, inflammation
Introduction
Bile acids (BAs) are synthesized and conjugated in the liver through cholesterol catabolism. Conjugation of bile acids increases their solubility, prevents their translocation across the intestinal epithelial barrier to damage tissue, and allows them to maintain the health of the GI tract as primary agents of lipid absorption. The detrimental effects of BAs over a lifetime of exposure vary depending on their solubility, conjugation status, and bioreactivity. Without the BA receptor farnesoid × receptor (FXR) regulation, chronic exposure to high concentrations of hydrophobic BAs can have carcinogenic consequences throughout the GI tract (1, 2). Deoxycholic acid (DCA) and lithocholic acid (LCA) are the most potent BAs associated to GI carcinogenesis (2, 3).
Dysregulated BA homeostasis is considered a common etiological factor for fat, viral, chemical, and immune-associated GI disease in the following contexts: (A) Obesity: Elevated BA pool size was observed in obese individuals with type II diabetes who carry increased liver and colon cancer risk (3). (B) Viral infections: BAs promoted HCV replication and HBV gene expression during viral hepatitis pathogenesis (4–6). (C) Chemical carcinogenesis: Ethanol increases the synthesis of toxic BAs while aflatoxin B1 induces cholestasis when excreted into bile (7, 8). (D) Immunity: BAs can also modulate inflammation and innate immunity in the gut-liver axis (9). All aforementioned diseases are associated with an elevated risk of GI cancer. Thus, it is critical to understand how BAs cause GI injury and promote carcinogenesis. Previous studies have implicated BAs in eliciting oxidative stress, DNA damage, and excessive inflammation (10). However, the mechanism accounting for GI carcinogenesis remains to be elucidated. The current study examines the effect of DCA and LCA in injuring and promoting compensatory proliferation in cells derived from the gut-liver axis, i.e. liver and colon, where BAs typically reside.
Orphan nuclear receptor Nur77 has a dual role in regulating cell survival or death depending on its intracellular location (11). The opposing effects of nuclear and cytosolic Nur77 in controlling cell fate have been established (11, 12). Nur77 and β-catenin crosstalk has been implicated in cancer formation (13). Epidermal growth factor (EGF) and other mitogens rapidly and potently induce the expression of nuclear Nur77, which serves as a transcription factor to enhance cell survival (14). The apoptotic effect of cytosolic Nur77 has also been studied using apoptosis inducers (15, 16). In the cytosol, Nur77 unmasks the BH-3 domain of Bcl-2, converting Bcl-2 into a pro-apoptotic molecule (12). Thus, the general consensus is that the opposing effects of nuclear and cytosolic Nur77 are chemical-dependent (11, 17). Because both Nur77 and BAs have a dual role in regulating apoptosis and proliferation, the current study tests the hypothesis that Nur77 mediates the effects of BAs.
Our data showed that hydrophobic DCA and LCA not only damaged DNA, but also increased the expression of pro-inflammatory genes in human liver and colon cancer cell lines as well as normal mouse primary hepatocytes (MPH). Both BAs effectively induced Nur77 expression with the intracellular location of Nur77 being time-dependent. Moreover, cells resistant to BA-induced apoptosis exhibited Nur77 overexpression along with increased cell viability and mobility. Nur77 target genes identified in BA-treated cells included proliferative genes CDK4, CCND2, BRE, RBBP8, MAP4K5, and STAT5A and unexpectedly, an apoptosis gene BID. Thus, for the first time, Nur77-mediated cell apoptosis and proliferation is shown to be regulated by BAs in a time-dependent manner. Moreover, Nur77 overexpression was observed in high percentages of liver and colon cancers implicating its significance in GI carcinogenesis. Taken together, hydrophobic BAs may promote liver and colon carcinogenesis though regulation of Nur77.
Materials and Methods
Reagents
All reagents were from Sigma-Aldrich (St. Louis, MO) unless otherwise noted. DCA, LCA, chenodeoxycholic acid (CDCA), and cholic acid (CA) were dissolved in DMSO as 150 mM or 20 mM stocks. Leptomycin B (LMB) was dissolved in ethanol as 100 µg/mL stocks.
Cell culture
Huh7 cells were obtained from Japanese Collection of Research Bioresources in 2009. Hep3B, HCT116, and HT29 cells were purchased from ATCC (American Type Culture Collection) in 2009 and 2013. ATCC authenticates all cell lines by DNA profiling via short tandem repeat (STR) analysis. Huh7 and Hep3B cells were maintained in Dulbecco’s Modified Eagle Medium (DMEM) (Gibco Grand Island, NY) with 10% fetal bovine serum (FBS) (Atlanta Biologicals Atlanta, GA). HCT116 and HT29 cells were maintained in McCoy’s 5α medium from Gibco with 10% FBS. Cells were treated with DMSO, DCA (20 or 150 µM), LCA (20 µM), CDCA (20 µM), or CA (20 µM) in serum-free media for indicated time. BA-resistant cells were selected from parental lines by exposure to increasing concentrations of LCA and DCA until 20 and 150 µM were reached, respectively.
Primary mouse hepatocyte isolation and culture
Following approved protocol from the Institutional Animal Care and Use Committee at University of California-Davis, wild type (WT) and Nur77 knockout (Nur77 KO) male mice (3–5 month, C57BL/6 from Jackson laboratory) were anesthetized and their livers perfused with Hank’s balanced salt solution, then HBSS with collagenase-A. Post isolation, 4 × 104 hepatocytes were seeded in six-well plates pre-coated with type-1 collagen and cultured in William's E medium containing 20% FBS. After overnight incubation, hepatocytes were treated with 20 µM LCA or 150 µM DCA in 2% FBS medium.
Human specimens
Formalin-fixed, archived human colon tumor and adjacent non-tumor specimens along with human liver tumor and normal specimens were obtained from the Second Affiliated Hospital of Guangzhou Medical University. Clinical data, i.e. patients’ medical records, included total serum BA (TBA), total cholesterol (TC), and triglyceride (TG), etc. with approval from the ethical committees of Guangzhou Medical University.
RNA preparation and qRT-PCR
RNA was extracted with TRIzol Reagent (Invitrogen, Carlsbad, CA). cDNA was made using High Capacity RNA-to-cDNA Kit (Applied Biosystems, Carlsbad, CA). qRT-PCR was done on ABI 7900HT Fast Real time PCR system using Power SYBR® Green PCR Master Mix (Applied Biosystems).
Nur77 shRNA plasmid transfection
shRNA constructs in lentiviral GFP vector against Nur77 were obtained from OriGene Technologies (Rockville, MD). For transient transfection, R-HCT116 and R-Huh7 cells were transfected with shRNA plasmids (1µg/1×105 Cells) using MegaTran 1.0 reagent (OriGene Technologies, Rockville, MD) according to the manufacturer's instruction.
(for power cut)MTT assay
Parental and BA-resistant HCT116 and Huh7 cells were seeded in 24-well plates and treated with DCA or LCA for 24h and 48 h, respectively. Cells were stained with 3-(4,5-dimethylthiazol-2-l)-2,5-diphenyltetrazolium bromide (MTT, 0.05 mg/ml) and measured at 570 nm with Synergy HT multi-mode microplate reader (Biotek, Winooski, VT).
Wound healing assay
Parental and BA-resistant cells were cultured in 6-well plates. The 70–80% confluent monolayers were wounded in a line with a sterile 20-µl plastic pipette tip. After 24 h, cell migration, indicated by wound closure, was evaluated by comparing the width of the remaining cell-free area with that of the initial wound via bright field microscopy.
Alkaline comet assay
HCT116, Huh7 cells, and mouse primary hepatocytes derived from WT and Nur77 KO mice were treated with DMSO, DCA or LCA. Then, single cell gel electrophoresis was performed using OxiSelect Comet Assay Kit (Cell Biolabs, San Diego, CA). Procedure was done in dim lighting to avoid UV-induced DNA damage. Fifty randomly selected cells were analyzed under fluorescence microscopy. The percent of cells exhibiting DNA damage as indicated by tail DNA content was quantified for each treatment compared to DMSO control.
Immunostaining and confocal microscopy
Human colon and liver tissue sections were immunostained with anti-Nur77 antibody (1:100, Santa Cruz Biotechnology, Santa Cruz, CA) and counterstained with hematoxylin. Huh7 and HCT116 cells were grown on poly-L-lysine-coated, 1.5mm thick glass coverslips and treated with 150 µM DCA or 20 µM LCA for indicated time. Following treatment, cells were immunostained with anti-Nur77 (1:100, Abcam, Cambridge, MA) and anti-cleaved caspase 3 (1:50, Santa Cruz Biotechnology) antibodies followed by Alexa Fluor® 488 anti-rabbit IgG and Alexa Fluor® 594 anti-goat IgG (Cell Signaling, Beverly, MA). Cells were mounted in ProLong® Gold Antifade Reagent with DAPI (Life Technologies) and imaged under Keyence BZ-9000 microscope.
Terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assay
TUNEL assay was performed with In Situ Cell Death Detection Kit, TMR red (Roche, Indianapolis, IN) according to the manufacturer’s instruction to monitor apoptosis in LCA-treated HCT116 and Huh7 cells. Nuclei were counter-stained with 4',6-diamidino-2-phenylindole (DAPI, Invitrogen, Carlsbad, CA). The percentage of apoptotic cells in LCA-treated HCT116 and Huh7 cells were counted under fluorescence microscopy in at least 5 microscopic fields (40×).
Western blotting
Protein lysates (30 µg) were subjected to polyacrylamide gel electrophoresis under reducing conditions. Proteins separated from gels were transferred onto PVDF membranes. The membranes were blocked with 4% BSA and incubated with primary antibody specific for Nur77 and β-actin (Santa Cruz Biotechnology, Santa Cruz, CA). Membranes were then incubated with horseradish peroxidase (HRP)-conjugated secondary antibodies. The signal was detected using the ECL system SuperSignal West Pico Chemiluminescent Substrates (Pierce Protein Biology, Rockford, IL).
ChIP-qPCR
ChIP-qPCR was performed as described previously (18). Briefly, chromatin lysate was precleared before incubation with a ChIP-quality anti-Nur77 antibody (Abcam). Antibodies to IgG (Santa Cruz, CA) and RNA Polymerase II (Millipore, MA) were used as negative and positive controls, respectively. Samples were incubated with Dynase beads at 4°C overnight followed by de-crosslinking and purification. DNA fragments generated (n = 3) served as templates for qPCR using Power SYBR Green PCR Master Mix.
Subcutaneous nude mice tumor xenograft models
BALB/c Nude mice (5–6 weeks old) were obtained from the Guangdong Animal Center. Mice were inoculated of with parental or BA-resistant HCT116 cells (1×106 cells per mouse) in the left flank and killed 5 weeks later. Tumor size was measured and tumor volume was calculated using a formula: volume = W (Width)2×L(Length)/2. All experimental protocols were approved by Animal Care and Use Committee of Guangzhou Medical University.
Statistical analysis
Data is presented as mean ± SD. The difference between the two groups was analyzed with Student’s t-test. p<0.05 was considered statistically significant.
Results
Hydrophobic DCA and LCA induce Nur77, inflammatory genes, and DNA damage
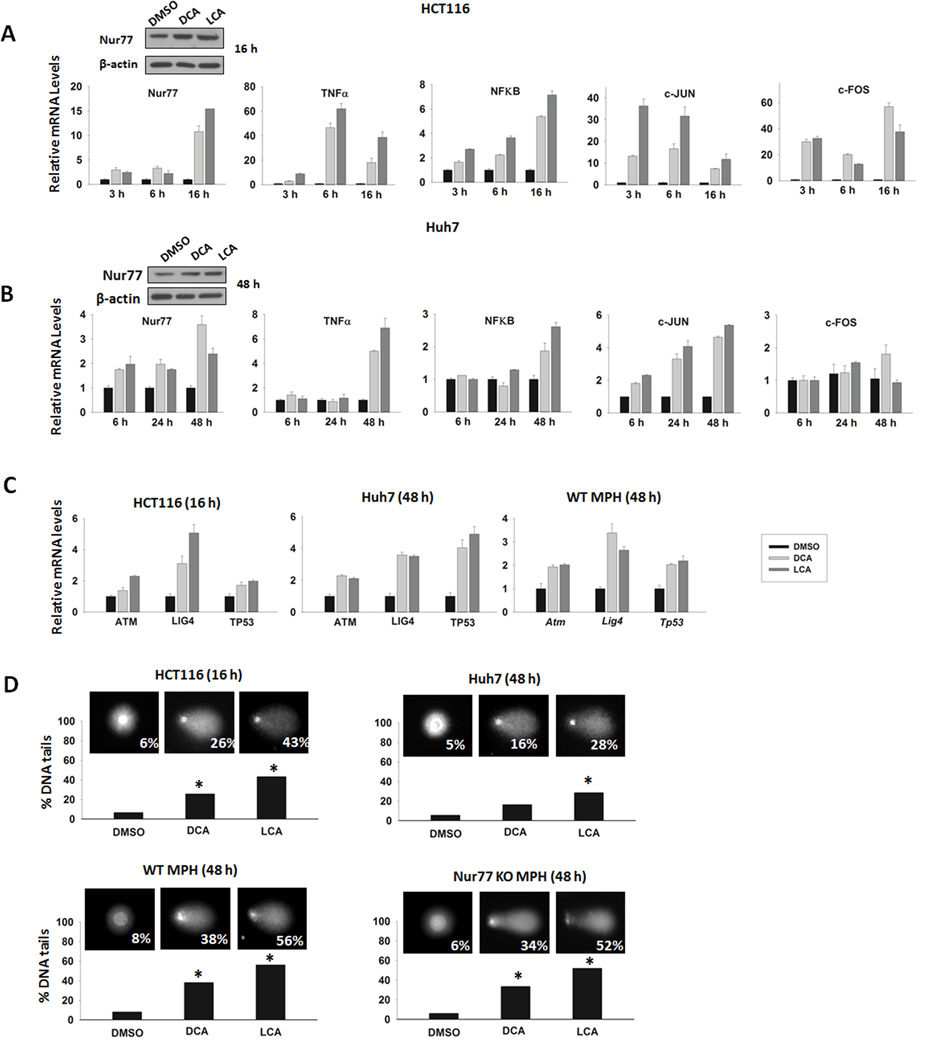
Human liver Huh7, Hep3B and colon HCT116, HT29 cell lines were treated with DCA, LCA, CDCA, or CA (20 µM) to determine whether BAs can induce Nur77 expression. All studied BAs induced Nur77 mRNA levels (2–15 fold induction, bar graphs not shown). LCA was the most potent Nur77 inducer for each studied cell line. DCA was able to increase Nur77 mRNA levels across all studied cell lines whereas CDCA failed to induce Nur77 in HT29 cells. CA only modestly increased Nur77 by 2-fold in Huh7 and HCT116 cells. Thus, the inducibility of Nur77 mRNA levels by BAs correlates with their hydrophobicity, which is LCA>DCA>CDCA>CA (19). Due to their effectiveness in inducing Nur77, DCA and LCA were used for subsequent studies in Huh7 and HCT116 cells. Because we hypothesized that BAs contribute to obesity-associated risks of GI cancer, we wanted to test BA concentrations found in obese patients. Therefore, the concentrations of 20 µM for LCA and 150 µM for DCA used were derived from fecal BA levels of individuals on a high-fat diet (20). Gene expression data showed that DCA and LCA increased Nur77, TNFα, and NFκB mRNA levels. Consistently, Nur77 protein levels were also increased by BA treatment in HCT116 and Huh7 cells (Fig. 1A and B). DCA and LCA also up-regulated the mRNA levels of c-FOS and c-JUN, upstream regulators of Nur77 (Fig. 1A and B). Moreover, DCA and LCA induced expression of DNA repair genes including ATM, LIG4, and TP53 in Huh7 and HCT116 cells as well as in WT MPH, suggesting the presence of DNA damage which was confirmed by COMET assay (Fig. 1C and D). DCA and LCA-treated HCT116 and Huh7 cells displayed significantly greater tail moments by 16 h and 48 h, respectively. Similarly, DCA and LCA-treated WT and Nur77 KO MPH also demonstrated DNA damage indicating BA-induced DNA damage was Nur77 independent. Taken together, DCA and LCA can damage DNA in both cancer and normal cells and potentially generate genomic instability.
Fig. 1. DCA and LCA up-regulate Nur77, inflammatory genes, and induce DNA damage in HCT116, Huh7 cells, and MPH.
Fold induction in Nur77, TNFα, NFκB, c-FOS, and c-JUN mRNA levels in DMSO, DCA (150 µM) or LCA (20 µM)-treated HCT116 (A) and Huh7 (B) cells measured by qRT-PCR. Western blot of Nur77 protein levels in BA and DMSO-treated cells. (C) Fold induction in ATM, LIG4, and TP53 in DCA (150 µM) or LCA (20 µM)-treated cells relative to DMSO control was measured by qRT PCR. (D) HCT116, Huh7 cells, MPH derived from WT and Nur77 KO mice were treated with DMSO, DCA (150 µM) or LCA (20 µM) and subjected to COMET assay. The percentages of cells with DNA damage tail as indicated in the figure was quantified for each treatment with * indicating p <0.05 compared to DMSO control.
Induction and intracellular location of Nur77 correlate with the opposing effects on apoptosis and survival exerted by BAs
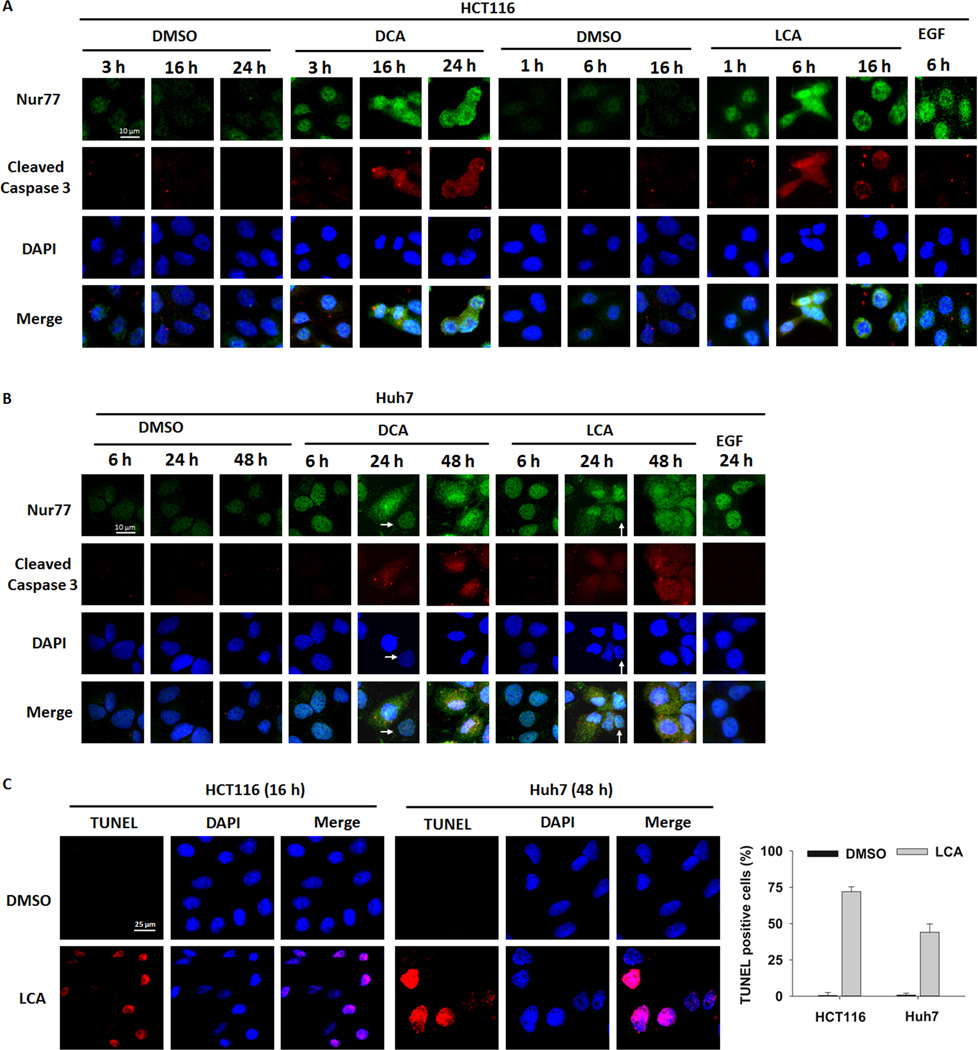
Because the induction and intracellular location of Nur77 dictate cell death and survival, the role of BA-induced Nur77 was studied by immunofluorescence microscopy. The data revealed that similar to EGF, DCA and LCA effectively induced Nur77 protein levels. Nur77 induction occurred shortly (1–3 h) after BA treatment in HCT116 cells; the induced Nur77 localized primarily in the nucleus while cleaved caspase 3 was undetectable (Fig. 2A). After prolonged treatment (6–24 h), diffuse Nur77 staining was noted in both the nucleus and cytosol, coinciding with positive detection of cleaved caspase 3. DCA and LCA similarly induced Nur77 in Huh7 cells with Nur77 intracellular location coinciding with cell survival and death (Fig. 2B). Consistent with cleaved caspase 3 staining data, TUNEL assay also showed extensive cell death after LCA treatment of HCT116 and Huh7 cells (Fig. 2C). Based on treatment time and BA concentrations, there was an apparent difference in susceptibility between HCT116 and Huh7 cells to the apoptotic effect of DCA and LCA. HCT116 cells were more sensitive to BA-induced apoptosis. Additionally, LCA was a more potent apoptotic agent than DCA. Intriguingly, after 24 h of DCA and LCA treatment, there were several Huh7 cells that lacked cleaved caspase 3 and had increased nuclear Nur77 suggesting the presence of BA-resistant cells (arrows, Fig. 2B). In conclusion, DCA and LCA modulated both survival and apoptosis in GI tract-derived cell lines and these opposing effects correlated with the induction and intracellular location of Nur77.
Fig. 2. BAs modulate cell proliferation and apoptosis through Nur77 nuclear export in a time-dependent manner.
Nur77 expression and location as visualized by immunofluorescence microscopy in DMSO, DCA (150 µM) or LCA (20 µM) treated HCT116 (A) and Huh7 cells (B) at indicated times. Cells were immunostained with anti-Nur77 and anti-cleaved caspase 3 antibodies followed by species appropriate Alexa Fluor secondary antibodies. Arrows showed Huh7 cells that lacked cleaved Caspase 3 and had increased nuclear Nur77. (C) TUNEL staining was performed in LCA-treated HCT116 and Huh7 cells. The percentages of apoptotic cells were counted with apoptotic cell staining in red while DAPI as nuclear staining in blue. Bar graph shows the number of apoptotic cells in 5 random fields (40×).
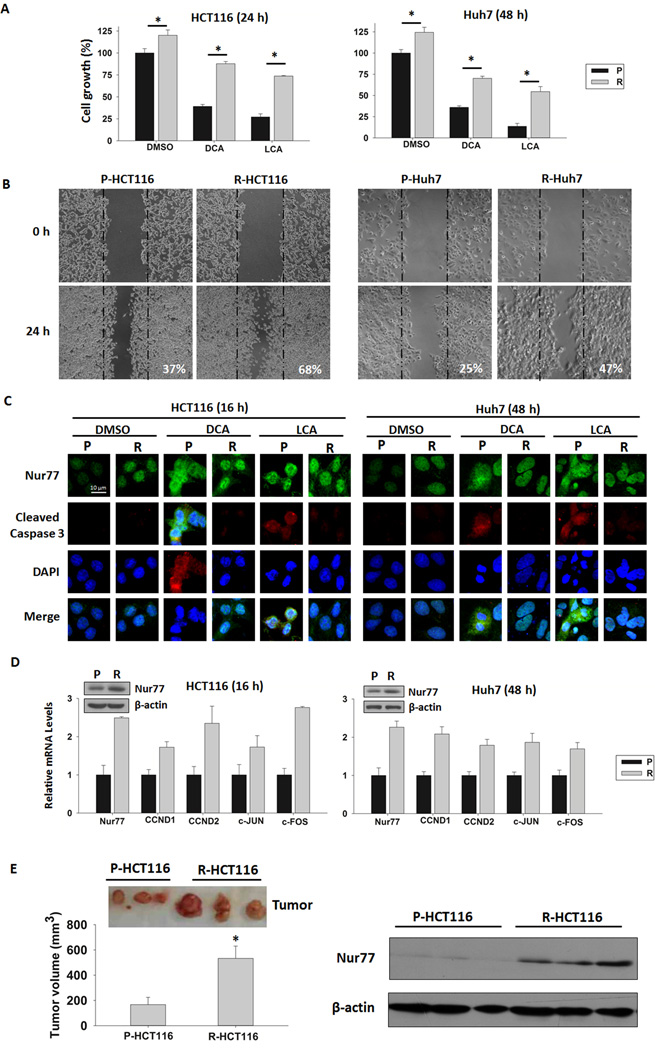
BA-resistant cells display increased viability and mobility as well as Nur77 overexpression
The potential role of Nur77 in BA-mediated carcinogenesis was studied by establishing BA-resistant cell lines. HCT116 and Huh7 cells were cultured under increasing concentrations of DCA and LCA over 7 days. Dead cells were removed daily and BA-containing media was replaced with normal media at the end of treatment to leave behind resistant cells. MTT assay showed that BA-resistant cells grew faster than parental lines at baseline and in response to DCA and LCA (Fig. 3A). Wound healing assay also revealed that BA-resistant cells migrated at least 2 times faster than parental counterparts (Fig. 3B). Moreover, BA-resistant cells displayed higher basal levels of nuclear Nur77 compared to parental cells as shown by qRT-PCR, Western blot, and immunostaining (Fig. 3C and D). DCA and LCA treatment further induced nuclear Nur77 levels in BA-resistant cells, which lacked cleaved caspase 3 (Fig. 3C). In contrast, identical treatment induced diffuse Nur77 throughout the entire cell as well as cleaved caspase 3 in parental Huh7 and HCT116 cells. Consistently, BA-resistant cell lines had elevated c-FOS, c-JUN, CCND1, and CCND2 mRNA levels suggesting that Nur77 overexpression promotes cell proliferation (Fig. 3D). To study the proliferative effect of BA-resistant cells in vivo, parental and BA-resistant HCT116 cells were injected subcutaneously into the flank of nude mice. Five weeks after the injection, the volume of tumors generated from R-HCT116 cells were about three times larger than that of P-HCT116 cells. Western blot analysis demonstrated that R-HCT116-generated tumors had elevated Nur77 level (Fig. 3E).
Fig. 3. BA-resistant HCT116 and Huh7 cells show enhanced proliferation, migration, and expression of nuclear Nur77 and cell cycle genes.
(A) Parental (P) and BA-resistant (R) HCT116 and Huh7 cells were treated with DMSO, DCA (150 µM) or LCA (20 µM) for indicated time and cell proliferation was measured by MTT assay. * indicates p <0.05 compared to P cells with corresponding treatment. (B) Migration of P- and R-HCT116 and P- and R-Huh7 cells was evaluated by wound healing assay 24h after wounding. The mean width of the gaps of nine wounds was measured and percentages of wound closure are indicated in the figure. (C) Nur77 expression and intracellular location as visualized by immunofluorescence microscopy in DMSO, DCA (150 µM) or LCA (20 µM) treated P- and R-HCT116 and Huh7 cells. The immunostaining was performed as same as mentioned in Fig. 2. (D) Fold induction in Nur77, CCND1, CCND2, c-FOS, and c-JUN mRNA levels in R-HCT116 and Huh7 cells relative to P cells as measured by qRT-PCR. Western blot shows Nur77 protein levels in P- and R-HCT116 and P- and R-Huh7 cells. (E) In vivo mouse xenograft study. Nude mice were injected with P-HCT116 or R-HCT116 cells and killed five weeks after the injection. Tumors size (left) and Nur77 protein level (right) were compared between the P and R-HCT116 cell-generated tumors. * p <0.05.
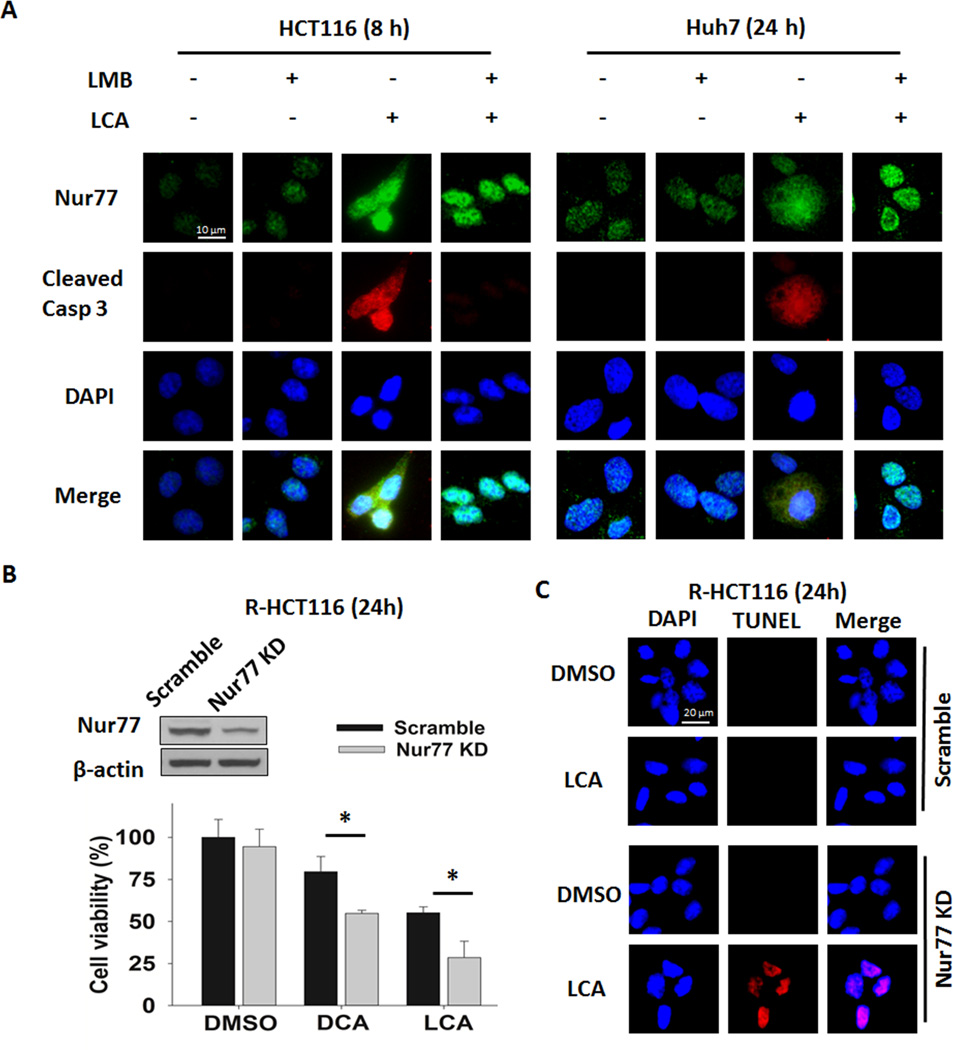
Nur77 expression and intracellular localization mediates BA-induced cell growth and apoptosis in HCT116 and Huh7
Leptomycin B (LMB), a specific inhibitor of protein nuclear export (21), was used to determine whether Nur77 intracellular location has a role in BA-induced apoptosis. Inhibition of Nur77 nuclear export by LMB decreased LCA-induced cleaved caspase-3 activity in HCT116 and Huh7 cells suggesting BA-induced apoptosis was dependent on Nur77 nuclear export (Fig. 4A). Because R-HCT116 cells had increased Nur77 basal level and cell viability, BA-resistant cells can be a model of Nur77 overexpression. Knockdown (KD) of Nur77 was performed in R-HCT116 cells to determine whether Nur77 mediates BA-induced HCT116 cell growth and apoptosis. Nur77 KD increased the sensitivity of cells to DCA and LCA-induced cell death (Fig 4B). Additionally, TUNEL assay showed increased apoptosis in LCA-treated R-HCT116 cells with Nur77 KD (Fig. 4C). Thus, reduction of Nur77 levels sensitized R-HCT116 cells to BA-induced apoptosis.
Fig. 4. Nur77 expression and cytoplasmic localization are required for BA-induced apoptosis in HCT116 and Huh7 cells.
(A) Inhibition of Nur77 nuclear export by leptomycin B (LMB) (2 ng/mL) reduced cleaved caspase 3 levels in LCA-treated HCT116 and Huh7 cells. HCT116 and Huh7 cells were treated with LCA (20 µM) in the absence or presence of LMB and analyzed by immunofluorescence microscopy as described for Fig 2A. (B) Nur77 KD reduces cell viability following BA treatment in R-HCT116 cells. R-HCT116 cells were transfected with control (Scramble) or Nur77 shRNA plasmid (transfection efficiency >80%) and treated with DMSO, DCA (150µM), or LCA (20µM) for 24 h. Western blot of Nur77 was performed to assess knockdown efficiency. Cell viability was then measured by MTT assay, * p <0.05 compared to the scramble plasmid-transfected cells with corresponding treatment. (C) Nur77 KD induces apoptosis in R-HCT116 cells after LCA treatment. R-HCT116 cells were transfected with a Nur77 KD or a scramble GFP plasmid (transfection efficiency >80%) followed by DMSO or LCA treatment for 16 h. TUNEL staining was used to detect apoptotic cells. TUNEL positive cells were only found in Nur77 shRNA plasmid-transfected and LCA-treated cells.
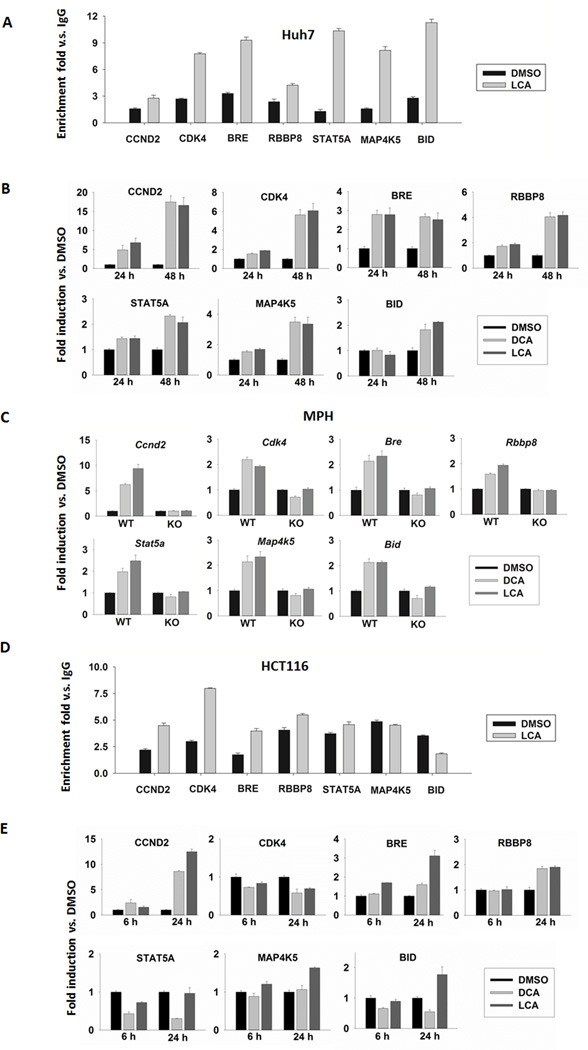
Nuclear Nur77 modulates the expression of survival and death genes by binding to the Nur77 response element
As a transcription factor, nuclear Nur77 regulates cell viability by modulating gene expression; however, very little is known about Nur77 target genes. Genes containing the Nur77 response element (NBRE; 5’AAAGGTCA3’) in their transcriptional regulatory regions with a role in cell viability, proliferation, or apoptosis were selected as potential Nur77 target genes (22). Nur77 binding to the NBRE of those genes at baseline and in response to BA treatment was studied by ChIP-qPCR. The results showed that Nur77 bound the NBRE of CCND2, CDK4, BRE, RBBP8, STAT5A, MAP4K5, and BID genes in vehicle-treated Huh7 cells while LCA treatment further increased the binding fold enrichment (Fig. 5A). Consistently, the mRNA levels of these genes were induced by DCA and LCA in Huh7 cells (Fig. 5B). To determine whether the regulation of those genes by BAs is Nur77-dependent, the effects of BAs in WT and Nur77 KO MPH were examined. BAs induced expression of Cdk4, Ccnd2, Bre, Rbbp8, Stat5a, Map4k5, and Bid genes in WT MPH, but such regulatory effect was completely abrogated in the absence of Nur77 (Fig. 5C). Nur77 also bound the NBRE of potential target genes in vehicle-treated HCT116 cells, but LCA treatment only altered the binding fold enrichment for CCND2, CDK4, BRE, and BID genes (Fig. 5D). Consistent with ChIP-qPCR binding data, BAs increased CCND2 and BRE mRNA levels. However, inconsistent with binding data, BAs induced BID but not CDK4 mRNA levels in HCT116 cells indicating that Nur77 binding does not necessarily alter gene expression (Fig. 5E).
Fig. 5. Nur77 up-regulates target genes by directly binding the NBRE in Huh7, HCT116 cells, and MPH.
(A) Enrichment fold of binding using anti-Nur77 in comparison with IgG in LCA (20 µM)-treated Huh7 cells as measured by ChIP-qPCR. (B) Fold induction of Nur77 target genes in DMSO, DCA (150 µM) or LCA (20 µM)-treated Huh7 cells measured by qRT-PCR. (C) Fold induction of Nur77 target genes in DCA (150 µM) or LCA (20 µM)-treated MPH from WT and Nur77 KO mice relative to DMSO control after 48 h treatment. (D) Enrichment fold of binding using anti-Nur77 in comparison with IgG in LCA (20 µM)-treated HCT116 as measured by ChIP-qPCR. (E) Fold induction of Nur77 target genes in DCA (150 µM) or LCA (20 µM)-treated HCT116 cells measured by qRT-PCR.
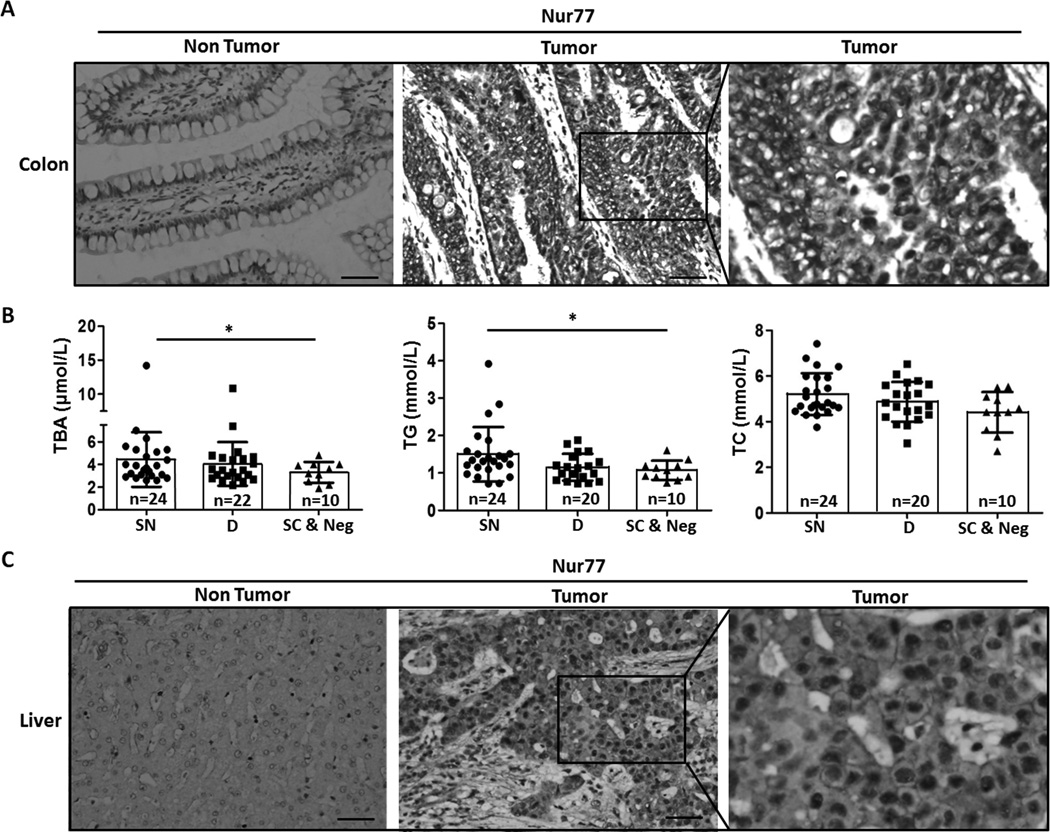
Nur77 is overexpressed in human colon and liver cancers and Nur77 intracellular location correlates with serum total BA levels
The expression of Nur77 was studied in human colon and liver cancers to determine the relevance of Nur77 in liver and colon carcinogenesis. Nur77 was overexpressed in 84% (59 out of 70 cases) of colon cancer specimens compared to paired normal adjacent specimens (Fig. 6A). Based on Nur77 intracellular location, colon tumor specimens were classified into three categories: (1) strong Nur77 staining in nucleus (SN, n=35), (2) diffuse Nur77 staining in both nucleus and cytosol (D, n=25), and (3) strong Nur77 staining in cytosol (SC, n=6) or negative Nur77 staining (Neg, n=4). The relationships between the intracellular distribution of Nur77 and clinical parameters were analyzed in colon cancer patients. Due to availability of clinical data, each analysis had a different sample size. In comparison with the normal fasting value of serum total bile acid (TBA, 3.1µmol/L), SN, D, and SC & Neg groups all had elevated TBA by 45%, 30%, and 6%, respectively. Serum TBA levels were significantly higher in SN than SC & Neg patients (Fig. 6B) (23). All patient groups had normal values for serum total triglyceride (TG, <1.7 mmol/L) and total cholesterol (TC, <5.2 mmol/L) (24). However, SN patients had statistically higher serum TG than SC & Neg patients. TC levels trended higher in SN and D than SC & Neg groups, but did not reach statistical significance (Fig. 6B). Significant correlation was not established with other available clinical findings, which included serum glucose, total bilirubin, and high density lipoprotein (not shown). Nur77 levels were also studied in liver cancer specimens (n=39) and normal liver controls (n=7). The data showed that 95% of examined liver cancer specimens displayed elevated Nur77 protein levels (Fig. 6C). Positive Nur77 staining was noted in both nucleus and cytosol with higher intensity in nucleus, but lack of clinical data prevented correlational studies.
Fig. 6. Nur77 is overexpressed in human colon and liver cancer and its intracellular location correlates with serum total BA levels in colon cancer patients.
(A) Representative images of Nur77 immunostaining in paired human colon tumor and adjacent non-tumor specimens (n=59). (B) Serum levels of total BA, TG and TC in colon cancer patients. Measurements were grouped as strong nuclear Nur77 staining (SN), diffuse Nur77 staining in both nuclear and cytosol (D), and strong cytosolic Nur77 or negative staining (SC & Neg) based on immunostaining. SC & Neg group included six of strong cytosol Nur77 staining samples and four of Nur77 negative staining samples. * indicating p <0.05 compared to SC & Neg group. Data sets were generated from available clinical data. (C) Representative images of Nur77 immunostaining in human liver tumor (n= 37) and normal liver (n=7). Scale bar, 100 µm.
Discussion
Chronic exposure to high levels of toxic hydrophobic BAs is a risk factor for colon and liver cancer. Our data showed that hydrophobic BAs induce DNA damage, inflammatory signaling, and cell death. To understand the underlying molecular mechanism by which BAs promote carcinogenesis, our novel data showed that BAs exert dual apoptotic and proliferative effects via Nur77. The dual roles of BA-regulated Nur77 are dependent on intracellular location. Short-term BA treatment induced nuclear Nur77, whereas longer treatment increased cytosolic Nur77 and cell death. The intracellular location of Nur77 regulated by BAs was time-dependent rather than chemical-dependent as proposed in previous studies (12, 25). Extended exposure to BAs also resulted in clonal selection and generated BA-resistant cells that had increased nuclear Nur77 and exhibited enhanced proliferative and migratory features. These results demonstrate that cellular exposure to DCA and LCA at concentrations associated with a high-fat diet not only promotes genomic instability, but also selects cells with malignant characteristics.
The overexpression of Nur77 in GI cancer cell lines is clinically relevant because immunostaining data showed that Nur77 protein levels were elevated in striking percentages of human colon and liver tumors versus non-tumor tissues. Regarding the intracellular location, the overexpressed Nur77 staining pattern differed between colon and liver tumors. Half (35 out of 70 cases) of studied colon tumor specimens showed strong nuclear Nur77 staining whereas liver tumor samples primarily displayed diffuse Nur77 staining in both the nucleus and cytosol. Additionally, the presence of three distinct Nur77 staining patterns in colon tumor specimens suggests a complexity of Nur77 regulation in vivo. This complexity can be explained by the heterogeneous characteristic of the tumor cells at the molecular level. In addition, the role of cytosolic Nur77 in established tumor cells remains to be characterized and may not be solely limited to the promotion of apoptosis by converting Bcl-2 into a death molecule. Moreover, variations in etiology such as viral hepatitis for liver cancer and familial adenomatous polyposis for colon cancer might also explain this difference in Nur77 intracellular location. In our study, etiological assessment was not possible due to limited available clinical data. Furthermore, Nur77 can be regulated by a wide variety of stress stimuli and chemicals in addition to BAs (11). Thus, case study does not allow us to establish a causal relationship between nuclear Nur77 overexpression and exposure to toxic BAs. Nevertheless, a marked 45% increase in serum TBA from normal fasting level was correlated with strong nuclear Nur77 staining in colon cancer patients; a 30% increase in serum TBA was also found in patients with diffuse Nur77 staining in both the nucleus and cytosol. Intriguingly, neither serum TG nor TC showed significant correlation with Nur77 intracellular location suggesting that disrupted BA homeostasis may play a larger role in Nur77-mediated GI carcinogenesis. These clinical findings support elevated BAs as a general feature of colon cancer; whether this correlation holds true for liver cancer remains to be determined. The knowledge gained from such studies would yield valuable insights into possible avenues to intercept the carcinogenic effects of dysregulated toxic BAs.
Because Nur77 and BAs have a dual role in regulating apoptosis and proliferation, a mechanistic investigation of a possible role of Nur77 in BA-enhanced GI carcinogenesis was necessary. Our data showed that exposure to toxic concentrations of LCA and DCA damaged DNA and up-regulated Nur77, TNFα, NFκB, c-FOS, and c-JUN mRNA expression. Our finding of DCA-induced NFκB up-regulation in liver and colon cancer cell lines is consistent with those in human hepatocytes and colon epithelial cells (26–28). It has been shown that the regulatory region of the Nur77 gene contains multiple highly conserved binding sites for AP1 (c-FOS/c-JUN) and NFκB and that NFκB is the principal regulator for lipopolysaccharide to induce Nur77 in macrophages (29). The induction of NFκB, c-FOS and c-JUN genes by BAs in both colon and liver cells shown in the current study further implicates the importance of these transcription factors in controlling Nur77 expression. Thus, the possible mechanism by which BAs induces Nur77 may be through activation of AP1 and NFκB.
Although previous studies have focused extensively on the apoptotic role of Nur77, few have considered the crucial role that Nur77 may play in carcinogenesis as a proliferative nuclear receptor. One study has implicated the involvement of Nur77 in DCA-stimulated proliferation of colon cancer cells, suggesting a link between Nur77 and BA-induced carcinogenesis (30). However, little is known about how Nur77 modulates cell proliferation due to limited evidence supporting its survival and proliferative function. Currently, only three putative Nur77 target genes have been identified as cell fate-regulators E2F1, BRE and RNF7 (31, 32). The remaining four target genes, G6PC, FBP1, FBP2, and ENO3, are involved in regulating skeletal muscle glucose homeostasis (33). In the present study, multiple survival genes CDK4, CCND2, RBBP8, STAT5A, and MAP4K5 were identified as direct Nur77 target genes following BA treatment. Surprisingly, a death gene BID could also be bound by Nur77 and was up-regulated by prolonged BA exposure in Huh7 and HCT116 cells. As a positive control, BRE showed expected induction at the mRNA level and Nur77 binding enrichment according to qRT-PCR and ChIP-qPCR results, respectively. Cdk4, Ccnd2, Bre, Rbbp8, Stat5a, Map4k5, and Bid were firmly established as Nur77 target genes when their up-regulation by BA was entirely abrogated in Nur77 KO MPH. The identification of these novel Nur77 target genes revealed for the first time that nuclear Nur77 can modulate both proliferative and apoptotic signaling pathways.
Despite significant progress in elucidating the location-dependent functions of Nur77, the mechanism by which Nur77 is targeted to the nucleus or cytosol remains unresolved. Nur77 post-translational modification studies have shown that ERK1/2 phosphorylation promoted nuclear localization of Nur77, whereas Chk2 phosphorylation led to nuclear export (16, 32). RXRα as well as RARβ also regulate Nur77-dependent apoptotic pathways by forming a complex with Nur77 (15, 25). Another study showed Nur77 protein stability and transcriptional activity are modulated via acetylation by p300 and HDAC1 (34). Furthermore, the differential binding of Nur77 to identified targets and susceptibility to apoptosis between Huh7 and HCT116 cells hint at tissue-specific regulation of Nur77 function by BAs. Inducible liver and intestine specific Nur77 KO mouse models should provide answers regarding how BA-induced and Nur77-mediated effects on cell fate might diverge between various cell populations in the gut-liver axis. Given the additional complexity of Nur77 regulation in vivo, it would also be pertinent to uncover the Nur77 target genes in human colon and liver cancer tissue. Thus, a clear understanding of the potentially organ-specific mechanisms dictating Nur77 localization and function is needed.
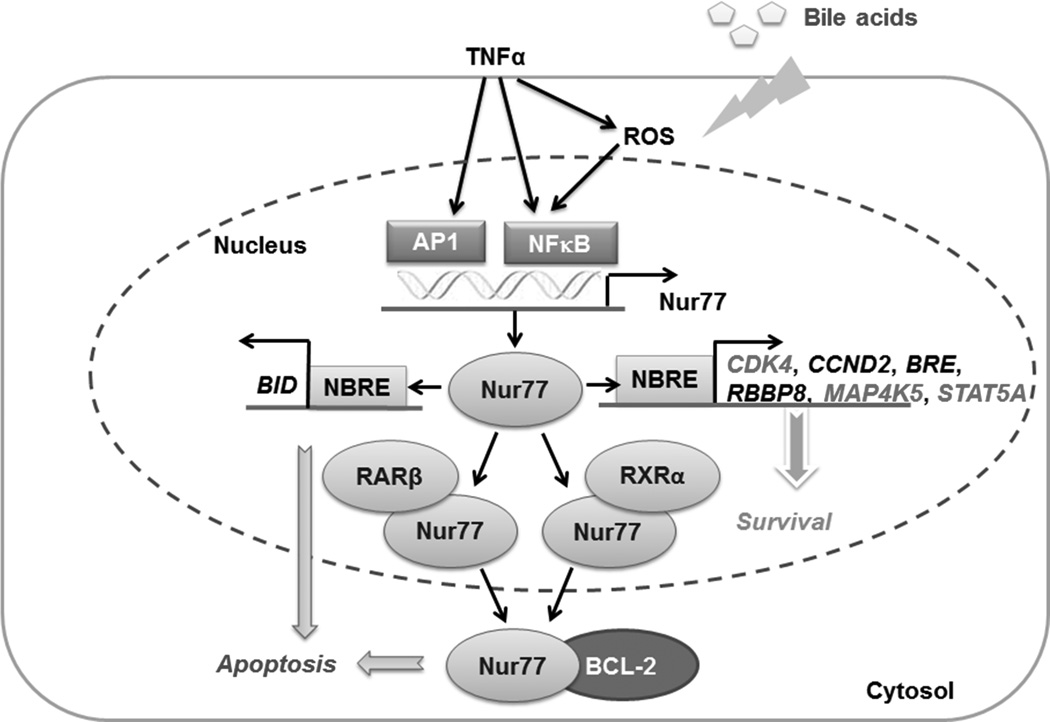
In conclusion, exposure to elevated levels of hydrophobic BAs can induce oxidative stress through ROS generation and activation of inflammatory TNFα-mediated signaling. TNFα activates AP1 and NFκB transcription factors, which subsequently enhance the transcription of Nur77. Increased levels of Nur77 permit its enrichment at the NBRE of its pro-survival targets genes CDK4, CCND2, BRE, RBBP8, STAT5A, and MAP4K5 to induce their expression and stimulate a Nur77-dependent survival pathway. However, after prolonged BA exposure, Nur77 also up-regulates the expression of BID, which inhibits the anti-apoptotic function of Bcl2. Additionally, cytosolic Nur77 interacts with and converts Bcl2 to a death molecule, triggering cytochrome C release and apoptosis. This suggests that a balance between Nur77-modulated expression of pro-survival and pro-apoptotic genes plays an important role in BA-regulated cell turnover. Our proposed Nur77-dependent mechanism by which toxic BAs elicit cell death, survival, and ultimately carcinogenesis is summarized in Fig. 7. Our data for the first time showed that LCA and DCA exert a dual role in modulating cell proliferation as well as apoptosis and both effects are mediated through Nur77. The subcellular localization of BA-induced Nur77 was time-dependent rather than chemical-dependent. CDK4, CCND2, RBBP8, MAP4K5, STAT5A, and BID were identified as direct Nur77 targets that carry out the time-dependent proliferative and apoptotic effects of DCA and LCA.
Fig. 7. Schematic representation for how BAs regulate apoptosis and survival in colon and liver cells.
Exposure to hydrophobic BAs induces oxidative stress through ROS generation and further activates TNFα-mediated signaling. BA-induced TNFα activates AP1 (c-FOS/c-JUN) and NFκB, which sequentially enhance Nur77 expression. Up-regulated Nur77 enriches at the NBRE of pro-survival targets genes (CDK4, CCND2, BRE, RBBP8, MAP4K5, and STAT5A) to induce their expression, thereby promoting a Nur77-dependent survival pathway. Conversely, Nur77 also up-regulates BID expression which likely contributes to BA-induced cell death. Additionally, RXRα and RARβ regulate Nur7 nuclear export by forming a complex with Nur77. Cytosolic Nur77 interacts with and converts Bcl2 into a death molecule, inducing apoptosis. These pathways are based on data generated in the present study and previously published data (Ref 12, 15, 25, 29, and 30). Genes that showed induction in Huh7, but not in HCT116 cells are indicated in grey.
Acknowledgement
The authors thank Lisa Teixeira for her assistance in preparation of this manuscript.
Grant Support
This study is supported by grants funded by National Institutes of Health (CA53596 and DK092100 to Y.J.Y.W.); the National Natural Science Foundation of China (81372634 to H.Y.); Guangdong Natural Science Funds for Distinguished Young Scholar (S2013050014121 to H.Y.) and the Research Award Fund for Outstanding Young Teachers in Guangdong Provincial Higher Education Institutions (Yq2013133 to H.Y.).
Abbreviations
- BA
bile acid
- GI
Gastrointestinal
- DCA
deoxycholic acid
- LCA
lithocholic acid
- CDCA
chenodeoxycholic acid
- CA
cholic acid
- NBRE
Nur77 response element
- WT
wild type
- Nur77 KO
Nur77 Knockout
- Nur77 KD
Nur77 Knockdown
- TC
total cholesterol
- TG
triglyceride.
Footnotes
Disclosure
The authors declare that there is no known conflict of interest associated with this publication
Authors' Contributions
Y.H.: Study concept and design, acquisition of data, analysis and interpretation of data, statistical analysis, drafting of the manuscript.
T.C.: Acquisition of data, analysis and interpretation of data, statistical analysis, drafting of the manuscript.
H.X.L.: Acquisition of data, analysis and interpretation of data.
R.K.: Acquisition of data, analysis and interpretation of data.
D.G.L. and Y.Q.N.: technical or material support, clinical samples and the relevant clinical information collection:
H.Y.: Acquisition of data, analysis and interpretation of data, obtained funding.
Y.J.Y.W.: Study concept and design, critical revision of the manuscript for important intellectual content, and obtained funding.
References
- 1.Gadaleta RM, van Mil SWC, Oldenburg B, Siersema PD, Klomp LWJ, van Erpecum KJ. Bile acids and their nuclear receptor FXR: Relevance for hepatobiliary and gastrointestinal disease. BBA-Mol Cell Bio L. 2010;1801:683–692. doi: 10.1016/j.bbalip.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 2.Bernstein H, Bernstein C, Payne CM, Dvorak K. Bile acids as endogenous etiologic agents in gastrointestinal cancer. World J Gastroentero. 2009;15:3329–3340. doi: 10.3748/wjg.15.3329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Graessler J, Qin Y, Zhong H, Zhang J, Licinio J, Wong ML, et al. Metagenomic sequencing of the human gut microbiome before and after bariatric surgery in obese patients with type 2 diabetes: correlation with inflammatory and metabolic parameters. Pharmacogenomics J. 2013;13:514–522. doi: 10.1038/tpj.2012.43. [DOI] [PubMed] [Google Scholar]
- 4.Bar-Yishay I, Shaul Y, Shlomai A. Hepatocyte metabolic signalling pathways and regulation of hepatitis B virus expression. Liver Int. 2011;31:282–290. doi: 10.1111/j.1478-3231.2010.02423.x. [DOI] [PubMed] [Google Scholar]
- 5.Chhatwal P, Bankwitz D, Gentzsch J, Frentzen A, Schult P, Lohmann V, et al. Bile Acids Specifically Increase Hepatitis C Virus RNA-Replication. PloS one. 2012;7 doi: 10.1371/journal.pone.0036029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reese VC, Oropeza CE, McLachlan A. Independent activation of hepatitis B virus biosynthesis by retinoids, peroxisome proliferators, and bile acids. J Virol. 2013;87:991–997. doi: 10.1128/JVI.01562-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Muller N, Petzinger E. Hepatocellular uptake of aflatoxin B1 by non-ionic diffusion. Inhibition of bile acid transport by interference with membrane lipids. Biochim Biophys Acta. 1988;938:334–344. doi: 10.1016/0005-2736(88)90131-9. [DOI] [PubMed] [Google Scholar]
- 8.Beyoglu D, Idle JR. The metabolomic window into hepatobiliary disease. J Hepatol. 2013;59:842–858. doi: 10.1016/j.jhep.2013.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poupon R. Ursodeoxycholic acid and bile-acid mimetics as therapeutic agents for cholestatic liver diseases: An overview of their mechanisms of action. Clin Res Hepatol Gas. 2012;36:S3–S12. doi: 10.1016/S2210-7401(12)70015-3. [DOI] [PubMed] [Google Scholar]
- 10.Allen K, Jaeschke H, Copple BL. Bile acids induce inflammatory genes in hepatocytes: a novel mechanism of inflammation during obstructive cholestasis. Am J Pathol. 2011;178:175–186. doi: 10.1016/j.ajpath.2010.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moll UM, Marchenko N, Zhang XK. p53 and Nur77/TR3 - transcription factors that directly target mitochondria for cell death induction. Oncogene. 2006;25:4725–4743. doi: 10.1038/sj.onc.1209601. [DOI] [PubMed] [Google Scholar]
- 12.Lin B, Kolluri SK, Lin F, Liu W, Han YH, Cao X, et al. Conversion of Bcl-2 from protector to killer by interaction with nuclear orphan receptor Nur77/TR3. Cell. 2004;116:527–540. doi: 10.1016/s0092-8674(04)00162-x. [DOI] [PubMed] [Google Scholar]
- 13.To SK, Zeng WJ, Zeng JZ, Wong AS. Hypoxia triggers a Nur77-β-catenin feed-forward loop to promote the invasive growth of colon cancer cells. Br J Cancer. 2014 doi: 10.1038/bjc.2013.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kolluri SK, Bruey-Sedano N, Cao X, Lin B, Lin F, Han YH, et al. Mitogenic effect of orphan receptor TR3 and its regulation by MEKK1 in lung cancer cells. Mol Cell Biol. 2003;23:8651–8667. doi: 10.1128/MCB.23.23.8651-8667.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang H, Zhan Q, Wan YJ. Enrichment of Nur77 mediated by retinoic acid receptor beta leads to apoptosis of human hepatocellular carcinoma cells induced by fenretinide and histone deacetylase inhibitors. Hepatology. 2011;53:865–874. doi: 10.1002/hep.24101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang H, Nie Y, Li Y, Wan YJ. ERK1/2 deactivation enhances cytoplasmic Nur77 expression level and improves the apoptotic effect of fenretinide in human liver cancer cells. Biochem Pharmacol. 2011;81:910–916. doi: 10.1016/j.bcp.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hsu HC, Zhou T, Mountz JD. Nur77 family of nuclear hormone receptors. Curr Drug Targets Inflamm Allergy. 2004;3:413–423. doi: 10.2174/1568010042634523. [DOI] [PubMed] [Google Scholar]
- 18.Hu Y, Liu HX, He Y, Fang Y, Fang J, Wan YJ. Transcriptome profiling and genome-wide DNA binding define the differential role of fenretinide and all-trans RA in regulating the death and survival of human hepatocellular carcinoma Huh7 cells. Biochem Pharmacol. 2013;85:1007–1017. doi: 10.1016/j.bcp.2013.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Song PZ, Zhang YC, Klaassen CD. Dose-Response of Five Bile Acids on Serum and Liver Bile Acid Concentrations and Hepatotoxicty in Mice. Toxicol Sci. 2011;123:359–367. doi: 10.1093/toxsci/kfr177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bernstein H, Bernstein C, Payne CM, Dvorakova K, Garewal H. Bile acids as carcinogens in human gastrointestinal cancers. Mutat Res-Rev Mutat. 2005;589:47–65. doi: 10.1016/j.mrrev.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 21.Kudo N, Matsumori N, Taoka H, Fujiwara D, Schreiner EP, Wolff B, et al. Leptomycin B inactivates CRM1/exportin 1 by covalent modification at a cysteine residue in the central conserved region. P Natl Acad Sci USA. 1999;96:9112–9117. doi: 10.1073/pnas.96.16.9112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao YG, Liu YX, Zheng DX. Alpha 1-antichymotrypsin/SerpinA3 is a novel target of orphan nuclear receptor Nur77. FEBS J. 2008;275:1025–1038. doi: 10.1111/j.1742-4658.2008.06269.x. [DOI] [PubMed] [Google Scholar]
- 23.Neale G, Lewis B, Weaver V, Panveliwalla D. Serum bile acids in liver disease. Gut. 1971;12:145–152. doi: 10.1136/gut.12.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 25.Cao XH, Liu W, Lin F, Li H, Kolluri SK, Lin BZ, et al. Retinoid × receptor regulates Nur77/thyroid hormone receptor 3-dependent apoptosis by modulating its nuclear export and mitochondrial targeting. Mol Cell Biol. 2004;24:9705–9725. doi: 10.1128/MCB.24.22.9705-9725.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Payne CM, Crowley C, Washo-Stultz D, Briehl M, Bernstein H, Bernstein C, et al. The stress-response proteins poly(ADP-ribose) polymerase and NF-κB protect against bile salt-induced apoptosis. Cell Death Differ. 1998;5:623–636. doi: 10.1038/sj.cdd.4400395. [DOI] [PubMed] [Google Scholar]
- 27.Washo-Stultz D, Crowley-Weber CL, Dvorakova K, Bernstein C, Bernstein H, Kunke K, et al. Role of mitochondrial complexes I and II, reactive oxygen species and arachidonic acid metabolism in deoxycholate-induced apoptosis. Cancer Lett. 2002;177:129–144. doi: 10.1016/s0304-3835(01)00786-8. [DOI] [PubMed] [Google Scholar]
- 28.Payne CM, Weber C, Crowley-Skillicorn C, Dvorak K, Bernstein H, Bernstein C, et al. Deoxycholate induces mitochondrial oxidative stress and activates NF-κB through multiple mechanisms in HCT-116 colon epithelial cells. Carcinogenesis. 2007;28:215–222. doi: 10.1093/carcin/bgl139. [DOI] [PubMed] [Google Scholar]
- 29.Pei LM, Castrillo A, Chen MY, Hoffmann A, Tontonoz P. Induction of NR4A orphan nuclear receptor expression in macrophages in response to inflammatory stimuli. J Biol Chem. 2005;280:29256–29262. doi: 10.1074/jbc.M502606200. [DOI] [PubMed] [Google Scholar]
- 30.Wu H, Lin Y, Li W, Sun Z, Gao W, Zhang H, et al. Regulation of Nur77 expression by beta-catenin and its mitogenic effect in colon cancer cells. FEBS J. 2011;25:192–205. doi: 10.1096/fj.10-166462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mu XM, Chang CS. TR3 orphan nuclear receptor mediates apoptosis through up-regulating E2F1 in human prostate cancer LNCaP cells. J Biol Chem. 2003;278:42840–42845. doi: 10.1074/jbc.M305594200. [DOI] [PubMed] [Google Scholar]
- 32.Yao LM, He JP, Chen HZ, Wang Y, Wang WJ, Wu R, et al. Orphan receptor TR3 participates in cisplatin-induced apoptosis via Chk2 phosphorylation to repress intestinal tumorigenesis. Carcinogenesis. 2012;33:301–311. doi: 10.1093/carcin/bgr287. [DOI] [PubMed] [Google Scholar]
- 33.Pei L, Waki H, Vaitheesvaran B, Wilpitz DC, Kurland IJ, Tontonoz P. NR4A orphan nuclear receptors are transcriptional regulators of hepatic glucose metabolism. Nat Med. 2006;12:1048–1055. doi: 10.1038/nm1471. [DOI] [PubMed] [Google Scholar]
- 34.Kang SA, Na H, Kang HJ, Kim SH, Lee MH, Lee MO. Regulation of Nur77 protein turnover through acetylation and deacetylation induced by p300 and HDAC1. Biochem Pharmacol. 2010;80:867–873. doi: 10.1016/j.bcp.2010.04.026. [DOI] [PubMed] [Google Scholar]