Abstract
Background
While limited evidence suggests that omega-3 supplementation may reduceantisocial behavior in children, studies have not reported on post-treatment follow-up and most treatment periods have been of short duration. This study tests the hypothesis that omega-3 supplementation over six months will reduce behavior problems in children both at the end of treatment and at six months post-treatment.
Methods
In this randomized, double-blind, placebo-controlled, stratified, parallel group trial, a community sample of 8-16 year old children were randomized into a treatment group (N = 100) and a placebo-control group (N = 100). The supplementation consisted of a fruit drink containing 1 gram/day of omega-3 or a placebo consisting of the same fruit drink without omega-3. Participants, care-givers, and research assistants were blinded to group assignment. The primary outcome measures of externalizing and internalizing behavior problems were reported by both caregivers and their children in a laboratory setting at 0 months (baseline), 6 months (end of treatment) and 12 months (6 months post-treatment), together with the secondary outcome measures of parental antisocial behavior. Data were analyzed on an intention-to-treat basis including all participants.
Results
Significant group × time interactions were observed with the treatment group showing long-term improvements in child behavior problems. The average post-treatment effect size was d = -.59. Effects were documented for parent-reports, but with theexception of proactive and reactive aggression,child-report data were non-significant.Parents whose children took omega-3showed significant post-treatment reductions in their own antisocial and aggressive behavior.Thisimprovementin caregiver behavior partly mediated the improvements observed in child behavior.
Conclusions
Findings provide initialevidence that omega-3 supplementation can produce sustained reductions in externalizing andinternalizing behavior problems. Results are the first to report improvements in caregiver behavior, and to establishthis improvement as a part-mechanism for the efficacy of omega-3.
Keywords: omega-3, externalizing, internalizing, aggression, randomized trial
Introduction
Poor nutritional status during pregnancy has been found to predispose to antisocial personality disorder in adulthood (Neugebauer, Hoek, & Susser, 1999), while poor nutrition in early childhood is associated with increased aggressive and conduct disordered behavior in childhood and adolescence(Liu, Raine, Venables, Dalais, & Mednick, 2004). Poor nutrition is hypothesized to negatively impact brain structure and function which in turn predisposes to risk factors for antisocial behavior(Liu, 2011; Raine, 2008). Brain abnormalities have been found to characterize not just adult offenders (Glenn & Raine, 2014), but also conduct disordered children and children with callous-unemotional traits (Viding et al., 2012; Fairchild et al., 2011). As such, poor nutrition is a plausible risk factor for the development of antisocial and aggressive behavior.
Given this nutrition – brain – antisocial behavior linkage, improving nutrition may help improve child behavior problems. Vitamin and mineral supplementation may reduce antisocial behavior, although evidence here is relatively sparse(Benton, 2007).Tryptophan supplementation (an essential amino acid) reduces aggression and agreeableness in some studies (Young, 2013). Another nutritional component coming under increasing scrutiny isomega-3. Fish consumption across the world is negatively correlated with cross-country homicide rates (Hibbeln, 2001). Two randomized controlled trials (RCTs) have shown that omega-3 supplementation reduces antisocial behavior in young prisoners in both England (35% reduction) and the Netherlands (34% reduction)(Gesch, Hammond, Hampson, Eves, & Crowder, 2002; Zaalberg, Nijman, Bulten, Stroosma, & van der Staak, 2010), and reduces aggression in male adultmen without a history of aggression (Long & Benton, 2013). Findings from RCTs in children and adolescents are mixed, with some finding limited evidence for efficacy (Gustafsson et al., 2010) while others do not (Milte et al., 2012). The latter study had 52% power to detect a significant effect, and consequently null results may be partly due to lack of adequate power.
Several factors may contribute to conflicting findings. Dosages of omega-3have varied across studies and are generally relatively low – with some as low as 124 mg of omega-3/ day (Gesch et al., 2002). Second, treatment length has been relatively short, with some as short as one month with a median of approximately three months(Sinn, Milte, & Howe, 2010). Third, because there appears to be no comprehensive meta-analysis of omega-3 supplementation on child antisocial behavior, there is a clear need for further RCTs on this behavior problem.Fourth, sample sizes are relatively small not just in studies on antisocial behavior, but also in clinical trials in general, with 50% having fewer than 70 participants (Califf et al., 2012).
There are also methodological limitations in prior studies. Some are correlational, yet RCTs are the building blocks of evidence-based practice (Maughan, 2013) and are critical for parsing causality. Second, no study on behavior problems has followed up children post-treatment to assess for long-term efficacy. Third, studies have not examined changes in caregiver behavior; improvements in the child’s behavior could plausibly improve the behavior of the parent, and this could further contribute to a delayed long-term improved child behavior. Fourth, it is unclear whether findings from the clinic and correctional settings generalize to the community. Fifth, while children with callous-unemotional traits have relatively poor treatment outcome(Frick, Ray, Thornton, & Kahn, 2014), we know of no attempts to reduce such traits using nutritional intervention.
To help address these issues, this study’s primary aimwas to test whether omega-3supplementation reduces child and adolescent antisocial /aggressive behavior. The main hypothesis was that omega-3 supplementation will reduce externalizing behavior problems both at the end of treatment and also six-month’s post-treatment. Secondary aims were to assess for reduction in internalizing behavior problems, and to examineany influence of nutritional supplementation to the child on theircaregiver’s antisocial behavior, and whether any such parental change could contribute to child behavior change.
Methods
Trial Design
The design consisted of a randomized, double-blind, placebo-controlled, stratified, parallel-group trial (1:1 ratio)of children in the community. Trial design remained unchanged throughout the study.
Study Setting
The study took place in interview rooms at the Joint Child Health Project headquarters in Quatre Bornes, Mauritius, from November 2009 to December 2011. Further details of this country and past research can be found in Raine, Liu, Venables, Mednick, & Dalais(2010). The study was registered in ClinicalTrials.gov under the title “Effect of Omega-3 Supplementation on Child Behavior Problems” at http://clinicaltrials.gov/ct2/show/NCT02016079?term=mauritius&rank=2
Participants
Participants consisted of 200 children of parents who themselves had participated in the Mauritius Child Health Project(Raine et al., 2010). Children had to be aged between 8 and 16 years old, willing to participate in an RCT, and residing in the community. Exclusion criteria consisted of: (1) allergy to fish or fish products, (2) use of fish oil supplementation in the past six months, (3) intellectual disability. Written informed consent was obtained from the parents, while assent was obtained from the child. During consenting, participants were informed of the study hypothesis that omega-3 may help improve child behavior. Ethical approval was obtained from IRB boards in Mauritius (Ministry of Health) and the US (University of Pennsylvania).
Reviews of RCTs have commented that median sample sizes in RCTs are relatively modest, with estimates of 46, 54, 65, and 80 from different reviews (Moher, 2010), and which also characterize omega-3 RCTs of psychopathology (Sinn et al., 2010). We consequently aimed for a somewhat larger study to detect a small-to-medium effect size. Our sample size of 200 had power to detect an effect size of d = .35 with power of .80, alpha = .05, one-tailed.
Omega-3 Intervention
Omega-3 supplementation
This consisted of a 200 ml drink (Smartfish Recharge).The base drinkin both treatment and control conditions consisted of fruit juice from apple, pear, pomegranate, aronia, and passion fruit. It also contained vitamin D (0.85 micrograms) and antioxidants(ferric reducing ability of plasma value of 0.71 mmol/100g). For the treatment condition only, a total of 1000 mg of omega-3 (300 mg of DHA, 200 mg of EPA, 400 mg of alpha-linolenic acid, and 100 mg of DPA) was added to the base drink. Placebo drinks were matched exactly with the fish-oil drink in terms of size, appearance, and flavor.
This drink was chosen because:(i) it contains an appreciably higher dosage of omega-3than standard capsules in a relatively small liquid quantity (60.6% of the size of a standard can of cola) suitable for child consumption, (ii) the fruit-flavored drink may be better tolerated and result in higher compliance with children than standard capsules.
Treatment duration and administration
Treatment duration was six months. This duration was chosen because prior treatment studies have usually been 2 - 4 months (Sinn et al., 2010), and a somewhat longer treatment period may be more effective in producing longer-term brain and behavioral change. The omega-3drink was administered by the parents to their children each dayat a suitable time.
Outcome Measures
The pre-defined primary outcome measures were externalizing behavior problems including aggressive behavior. Secondary outcomes included internalizing behavior problems and parental aggressive and psychopathic behavior.
Child Behavior Checklist (CBCL)and Youth Self Report (YSR)
The CBCL(parent-report) and YSR (child report) are well-standardized, extensively-used psychometric instruments with high reliability/validity in many countries (Achenbach & Rescorla, 2001).Measurement invariance of the CBCL has also been documented on this cohort in Mauritius (Yarnell et al., 2013). The CBCL/YSR contain two empirically derived broadband scales (externalizing / internalizing) and eight syndrome scales. Externalizing behavior consists of Aggressive Behavior and Rule-Breaking Behavior scales, while internalizing behavior domain consisted of Anxious/Depressed, Withdrawn/Depressed, and Somatic Complaints scales. Additionalsyndrome scales include Attention Problems, Social Problems, Thought, and Other Problems.
Reactive Proactive Aggression Questionnaire (RPQ)
Children completed this self-report instrument which yields scales or reactive, proactive, and total aggression (Raine et al., 2006). Reliability and validity have been documented in Baker, Raine, Liu, & Jacobson(2008),Fossati et al., (2009), andFung, Raine, & Gao(2009).
The Antisocial Personality Screening Device (APSD)
This 20-item scale assesses parent-reported child and adolescent psychopathic traits (Frick, Bodin, & Barry, 2000). It consists of three subscales to assess callous-unemotional traits, narcissism, and impulsivity.
Psychopathic Personality Inventory (PPI)
Parents completed the short version of the self-report Psychopathic Personality Inventory (PPI- Lilienfeld & Andrews, 1996). It yields a global psychopathy score, and eight sub-scales measuring social potency, cold-heartedness, fearlessness, impulsive nonconformity, stress immunity, Machiavellian egocentricity, blame externalization, and carefree non-planfulness. The PPI was designed for use in non-clinical settings and has been shown to be reliable and valid in community samples (Lilienfeld & Andrews, 1996).
Randomization and Stratification
After giving informed consent, participants were randomized into treatment and placebo groups with blocking on a 1:1 ratio (Suresh, 2011). Prior to initial group assignment, matched pairs of participants were created from the computer data-base, with matching on age band (8-10, 11-13, 14-16), gender (male / female), and ethnicity (Indian / Creole). This stratification procedure aims to balance groups on key demographic variables. Within each of the 100 pairs, restricted randomization to group was conducted using a computer-generated list of random numbers generated by SPSS.
Adherence to protocol
Adherence to the treatment regimen was assessed at the end of treatment by asking caregivers how often the drink had been consumed (number of drinks / week). Adherence was also assessed by assays of omega-6 and omega-3 from finger-prick blood taken at baseline and 6 months (end of treatment). For detailed methods seeLin, Loewke, Hyun, Leazer, & Hibbeln(2012).
Statistical Methods
An intention-to-treat (ITT) design using all randomly assigned participants (200) was employed for all data analyses. Data missing due to loss at follow-up were imputed using the last observation carried forward strategy (White, Horton, & Pocock, 2011). The ITT approach is considered a gold standard for RCTs, is endorsed by CONSORT, respects initial randomization, and provides unbiased estimates of the effect of treatment assignment on outcome measures (Shrier et al., 2014) as well as a more realistic estimate of treatment effects in the real world where people drop out of treatment (Del Re, Maisel, Blodgett, & Finney, 2013).
Analyses focused on documenting group × time interactions, with effect sizes calculated using partial eta2. Differences in baseline scores were compared using two-tailed independent t-test. Where differences were observed (only for child self-report RPQ), baseline scores were entered as covariates to equalize groups at baseline.
To assess whether any improvement in parental behavior may partly account for the treatment effect on child behavior, mediation analyses were performed using the PROCESS SPSS macro (Hayes, 2012). To test significance of the indirect effects (i.e. mediation), bias-corrected confidence intervals for the indirect effects were generated using 10,000 bootstrap samples. Bootstrapping was used because it constitutes a nonparametric resampling procedure that makes more realistic assumptions on the sampling distribution of the indirect effect(MacKinnon, Lockwood, & Williams, 2004)). To assess extent of mediation, the reduction in variance explained in treatment outcome by the intervention after controlling for improved parental behavior (the mediator) was calculated in a two-step regression. All analyses were conducted using SPSS (version 20).
Results
Participant flow and recruitment
Participant flow and recruitment details are outlined in the online supplementary Table S1. No participant loss was observed on baseline assessment after randomization. Of the 200 participants, 16(8%) were lost to follow-up at either 6 or 12 months (5 from omega-3, 11 from placebo – see Supplementary Table S1 for details of reasons for loss). Groups did not significantly differ in this attrition (chi-square = 2.51, df = 1, p = .11).
Demographics and adherence to protocol
Demographics
Demographic data are reported in Table 1. No significant group differences were observed, documenting that stratification procedures were successful.
Table 1.
Demographic and adherence data together with statistical comparisons for placebo and omega-3 groups.
| Placebo | Omega-3 | Statistic | P | ||
|---|---|---|---|---|---|
|
| |||||
| Demographics | |||||
|
| |||||
| Age (SD) | 11.57 (2.12) | 11.07 (2.21) | t = 1.62 | .11 | |
|
| |||||
| IQ (SD) | 99.94 (13.52) | 101.23 (14.54) | t = 0.65 | .52 | |
|
| |||||
| Sex | |||||
| Female (N) | 48 | 48 | Chi2 = 0.0 | 1.0 | |
| Male (N) | 52 | 52 | |||
|
| |||||
| Ethnicity | |||||
| Indian (N) | 59 | 57 | Chi2 = 0.08 | .77 | |
| Creole (N) | 41 | 43 | |||
|
| |||||
| Religion | Chi2 = 0.11 | .95 | |||
| Hindu (N) | 28 | 28 | |||
| Muslim (N) | 32 | 30 | |||
| Catholic (N) | 40 | 42 | |||
|
| |||||
| Adherence | |||||
|
| |||||
| N Drinks / week | 6.49 (1.04) | 6.54 (0.88) | t = 0.34 | .73 | |
|
| |||||
| Omega-3 blood level: | |||||
| Before | 21.49 (7.44) | 22.73 (7.55) | t = 1.16 | .25 | |
| After | 22.29 (7.12) | 26.39 (9.33) | t = 3.49 | .001 | |
Adherence to protocol
Average number of drinks taken per week for each group are provided online in Table 1. There was no significant group difference in compliance rates (p = .73).
Adherence to the protocol was also assessed usingblood omega-3 fatty acid levels (see Table 1). A significant group × time interaction indicated that groups did not differ at baseline, but post-treatment (6 months) the omega-3 group had significantly higher omega-3levels than controls(p < .001), indicating increased omega-3 levels over treatment.
Child behavioral problems
Means and SDs on parent and child outcome measuresfor children at all three time points, group × trial interactions, effect sizes for interactions and post-treatment group differences are detailed in Table 2.
Table 2.
Means and standard deviations on child behavior outcome measures in placebo and omega-3 groups for the three assessment periods, together with statistical comparisons and effect sizes.
| Placebo Mean 0 Months (SD) | Omega-3 Mean 0 Months (SD) | Placebo Mean 6 Months (SD) | Omega-3 Mean 6 Months (SD) | Placebo Mean 12 Months (SD) | Omega-3 Mean 12 Months (SD) | Effect size for mean group difference at 12 months, Cohen’s d (95% C.I.) | Main group effect, F (df = 1) | Group × time interaction, F (df = 2) | Effect Size for Group × Time interaction, partial eta2 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Parent Report | ||||||||||
|
| ||||||||||
| Child Behavior Checklist | ||||||||||
| CBC Externalizing | 8.78 (8.44) | 8.33 (9.01) | 6.97 (8.79)a | 7.79 (8.17)a | 7.79 (8.95) | 5.05 (6.75) | -.35 (-.62, -.07) | .54 | 8.74** | .04 |
| CBC Internalizing | 8.88 (8.48) | 7.45 (7.84) | 5.22 (6.22)a | 4.94 (5.90)a | 6.72 (7.88)b | 3.14 (4.76)b | -.55 (-.83, -.27) | 4.59* | 6.33** | .03 |
| CBC Rule-Breaking | 1.58 (1.97) | 1.32 (2.27) | 1.29 (2.24)a | 1.36 (1.77) | 1.71 (2.41)b | .64 (1.67)b | -.52 (-.80, -.23) | 2.73 | 10.85** | .05 |
| CBC Aggression | 7.20 (6.93) | 7.01 (7.07) | 5.68 (6.90)a | 6.43 (6.82) | 6.08 (6.96) | 4.41 (5.45)b | -.33 (-.71, -.05) | .19 | 6.18** | .03 |
| CBC Attention Problems | 3.54 (3.72) | 3.53 (3.29) | 2.29 (3.00)a | 2.64 (2.95)a | 3.13 (3.09)b | 1.57 (1.93)b | -.61 (-.90, -.32) | 1.29 | 12.01** | .06 |
| CBC Withdrawn | 3.00 (2.84) | 2.28 (2.71) | 1.54 (1.96)a | 1.54 (2.07)a | 2.40 (2.70)b | 1.01 (1.67)b | -.62 (-.90, -.34) | 6.74* | 8.37** | .04 |
| CBC Somatic | 2.09 (2.69) | 1.60 (2.14) | 1.52 (2.34)a | 1.15 (2.00) | 1.07 (1.87) | .69 (1.43)b | -.23 (-.51, .05) | 3.05 | .09 | .00 |
| CBC Anxious/ Depressed | 3.97 (4.41) | 3.66 (4.47) | 2.27 (3.03)a | 2.30 (3.22)a | 3.26 (4.26)b | 1.44 (2.68)b | -.51 (-.79, -.23) | 2.58 | 7.10** | .04 |
| CBC Social Problems | 2.06 (2.41) | 1.80 (2.00) | 1.13 (1.79)a | 1.23 (1.63)a | 1.84 (2.11)b | .77 (1.34)b | -.61 (-.89, -.32) | 3.78 | 8.37** | .04 |
| CBC Thought Problems | .69 (1.22) | .75 (1.32) | .44 (1.02) | .36 (.80)a | .64 (1.26) | .13 (.51)b | -.53 (-.81, -.25) | 2.46 | 6.01** | .03 |
| CBC Other Problems | 5.13 (4.67) | 4.23 (4.35) | 3.35 (3.82)a | 3.30 (3.56)a | 4.02 (4.66) | 2.29 (2.62) | -.46 (-.74, -.18) | 3.41 | 5.37** | .03 |
| Antisocial Process Screening Device | ||||||||||
| APSD Callous-Unemotional | 4.60 (2.25) | 4.68 (2.22) | 3.06 (2.32)a | 3.55 (2.32)a | 3.96 (2.39)b | 2.58 (2.37)b | -.58 (-.86,-.30) | 1.22 | 13.69** | .07 |
| APSD Narcissism | 2.44 (2.84) | 2.70 (2.62) | 3.03 (3.36)a | 2.76 (3.12) | 2.39 (2.91)b | 2.38 (2.86) | -.00 (-.28, .28) | .00 | 1.05 | .01 |
| APSD Impulsivity | 2.68 (2.16) | 2.37 (1.98) | 2.98 (2.61) | 2.57 (2.27) | 2.24 (2.29)b | 1.99 (2.33)b | -.11 (-.39, .17) | 1.35 | .16 | .00 |
| APSD Total | 9.83 (5.53) | 9.75 (5.08) | 9.07 (7.04) | 8.88 (6.17) | 8.59 (6.14) | 6.95 (5.75)b | -.28 (-.55, .00) | .74 | 2.97 | .02 |
|
| ||||||||||
| Child Report | ||||||||||
|
| ||||||||||
| Youth Self-Report | ||||||||||
| YSR Externalizing | 8.81 (7.23) | 11.47 (6.49) | 7.59 (7.10)a | 10.17 (6.68)a | 7.60 (7.77) | 9.82 (6.87) | .30 (.02, .58) | .54 | .34 | .00 |
| YSR Internalizing | 13.70 (11.05) | 13.80 (10.45) | 12.38 (11.77) | 14.33 (11.37) | 10.62 (9.08)b | 13.27 (12.30) | .25 (-.03, .52) | 3.94* | 2.30 | .01 |
| YSR Rule-Breaking | 1.64 (1.97) | 2.65 (2.02) | 1.64 (2.01) | 1.89 (2.02)a | 1.63 (1.93) | 2.05 (2.12) | .21 (-.07, .49) | 1.39 | 1.24 | .01 |
| YSR Aggression | 7.17 (5.76) | 8.82 (5.19) | 5.95 (5.65)a | 8.28 (5.26) | 5.97 (6.31) | 7.77 (5.54) | .30 (.02, .58) | 7.29** | .68 | .00 |
| YSR Attention Problems | 3.38 (3.07) | 4.38 (2.61) | 2.91 (2.93) | 3.81 (2.74)a | 2.58 (2.83) | 3.77 (3.26) | .39 (.11, .67) | 2.30 | 1.48 | .01 |
| YSR Withdrawn | 2.60 (2.19) | 2.73 (2.10) | 2.54 (2.46) | 2.41 (1.97) | 2.06 (1.90) b | 2.46 (2.18) | .20 (-.08, .47) | .12 | 1.97 | .01 |
| YSR Somatic | 1.16 (1.33) | 1.25 (1.75) | .90 (1.31) | 1.26 (1.56) | .98 (1.59) | 1.18 (1.67) | .12 (-.15, .40) | 2.20 | 1.24 | .01 |
| YSR Anxious/ Depressed | 4.97 (4.49) | 4.91 (4.05) | 4.47 (4.48) | 5.33 (4.65) | 3.79 (3.51) b | 4.80 (4.93) | .24 (-.04, .51) | 4.40* | 2.48 | .01 |
| YSR Social Problems | 3.32 (2.42) | 3.09 (2.03) | 2.86 (2.32)a | 3.62 (2.52) | 2.30 (1.97)b | 3.07 (2.28)b | .36 (.08, .64) | 11.79** | 5.55** | .03 |
| YSR Thought Problems | 1.47 (2.14) | 1.25 (1.56) | 1.47 (1.91) | 1.71 (2.07)a | 1.52 (1.89) | 1.82 (2.18) | .15 (-.13, .42) | 3.64 | 1.77 | .01 |
| YSR Other Problems | 7.17 (5.76) | 8.82 (5.19) | 5.44 (4.72)a | 5.98 (3.16)a | 5.15 (3.93) | 6.48 (3.94) | .33 (.06, .62) | 5.03* | 1.59 | .01 |
| Reactive-Proactive Aggression Questionnaire | ||||||||||
| RPQ Proactive Aggression | .67 (1.28) | 1.52 (2.12) | .96 (2.09) | .67 (1.30)a | .83 (2.03) | 1.27 (2.37)b | .20 (-.08, .48) | 2.81 | 4.02* | .02 |
| RPQ Reactive Aggression | 3.91 (3.85) | 6.05 (3.40) | 4.61 (4.34) | 3.96 (3.02)a | 4.17 (4.14) | 5.13 (3.35) b | .25 (-.02, .53) | 4.58* | 7.88** | .04 |
| RPQ Total Aggression | 4.58 (4.67) | 7.57 (4.95) | 5.57 (5.99) | 4.63 (3.87)a | 5.00 (5.72) | 6.40 (5.16)b | .26 (-.02, .54) | 5.76* | 8.58** | .04 |
indicates statistically significant (p < .05) within group behavior change from 0 to 6 months.
indicates statistically significant (p < .05) within group behavior change from 6 to 12 months.
Parent Report
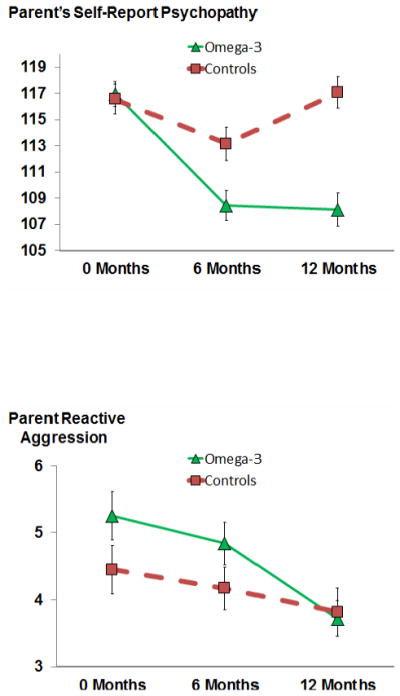
Significant group × time interactions were observed for all internalizing and externalizing subscales, except for somatic complaints. A significant interaction was also obtained for callous-unemotional traits. All other results were non-significant. Interactions for externalizing, internalizing, and callous-unemotional behavior are illustrated in Figure 1. The effect size for group differences at 12 months for all CBCL behavior problem scales was d = - .59 (95% C.I. = -.84 to -.35).
Figure 1.
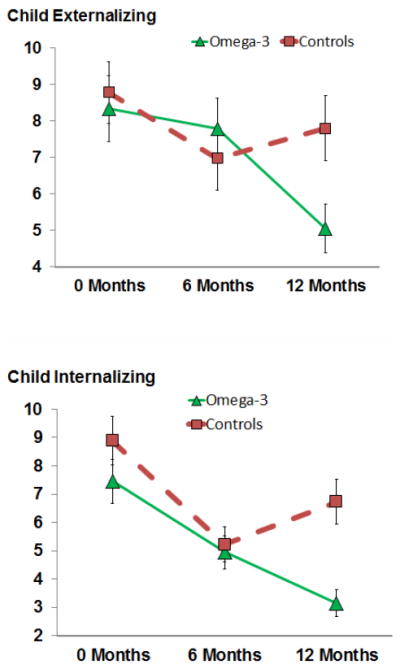
Significant group × time interactions (with standard error bars) for parents’ reports of child externalizing behavior, child internalizing behavior, and child callous-unemotional traits.
Child Report
In contrast to parent reports,for most self-report measures no group × trial interactions were observed. Significant interactions were however observed for self-report reactive (p < .0001) and proactive (p = .02) aggression, as well as total aggression (p < .0001). Both forms of aggression showed significant intervention declines only in the omega-3 group by the end of treatment at 6 months (average d = - .80, 95% C.I. = -1.08 to -.52) (see online supplementary Figure S1).
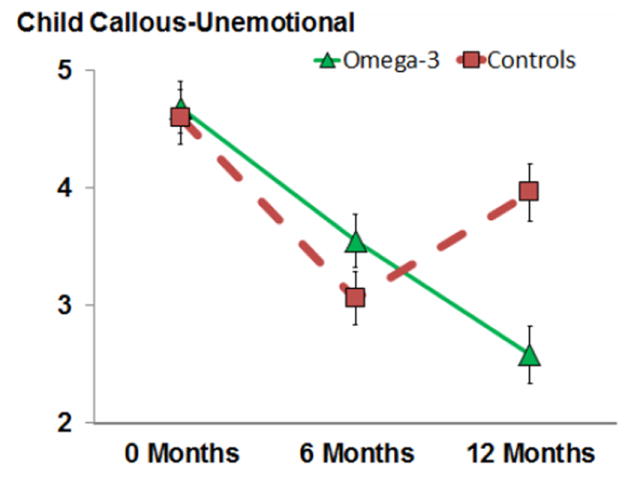
Parental Antisocial Behavior
Means, SDs, group × time interactions, and post-treatment effect sizes are shown in Table 3. Significant group × time interactions were observed for total PPI scores, six of the eight PPI subscales, and reactive (but not proactive) aggression. As indicated Figure 2, total psychopathy scores declined at 6 months in both groups during treatment, but while scores for placebo parents returned to baseline at follow-up, the reduction in parents of the omega-3 group was maintained 6 months post-treatment at the 12 month time-point.
Table 3.
Means and standard deviations (in parentheses) for parent self-report on outcome measures in placebo and omega-3 groups for the three time periods, together with statistical comparisons and effect sizes.
| Placebo Mean 0 Months (SD) | Omega-3 Mean 0 Months (SD) | Placebo Mean 6 Months (SD) | Omega-3 Mean 6 Months (SD) | Placebo Mean 12 Months (SD) | Omega-3 Mean 12 Months (SD) | Effect size for mean group difference at 12 Months, Cohen’s d (95% C.I.) | Main group effect, F (df = 1) | Group × time interaction, F (df = 2) | Effect Size for Group × Time interaction, partial eta2 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Parent Self-Report | ||||||||||
| Psychopathic Personality Inventory (PPI) | ||||||||||
| PPI Total | 116.55 (11.36) | 116.95 (9.68) | 113.16 (12.67)a | 108.44 (11.60)a | 117.07 (12.14)b | 108.11 (12.81) | -.72 (-1.00, -.43) | 11.38** | 13.97** | .07 |
| PPI Social Potency | 19.32 (3.79) | 19.42 (3.77) | 17.13 (4.29)a | 17.67 (4.85)a | 18.31 (4.70)b | 17.08 (4.43) | -.27 (-.55, .01) | .14 | 5.98** | .03 |
| PPI Coldheartedness | 15.04 (3.84) | 15.66 (3.08) | 13.76 (3.76)a | 14.27 (4.02)a | 15.52 (4.28)b | 15.39 (4.23)b | -.03 (-.31, .25) | .51 | 1.32 | .01 |
| PPI Carefree Nonplanfulness | 11.30 (3.33) | 12.93 (3.17) | 10.16 (3.12)a | 10.22 (2.89)a | 11.57 (4.03)b | 10.46 (3.18) | -.31 (-.58, -.03) | .30 | 13.29** | .06 |
| PPI Fearlessness | 12.17 (3.94) | 12.07 (3.12) | 12.54 (5.32) | 9.90 (3.33)a | 12.95 (3.38) | 11.07 (3.14)b | -.58 (-.86, -.29) | 11.40** | 14.43** | .07 |
| PPI Blame Externalization | 16.15 (6.70) | 15.78 (6.07) | 15.67 (7.25) | 16.21 (6.70) | 15.69 (6.73) | 14.03 (6.82)b | -.25 (-.52, .03) | .32 | 7.21** | .04 |
| PPI Stress Immunity | 18.30 (3.37) | 17.72 (2.67) | 19.57 (3.89)a | 17.60 (3.61)a | 19.06 (3.46) | 18.58 (3.26)b | -.14 (-.42, .13) | 6.57* | 6.13** | .03 |
| PPI Impulsive Nonconformity | 11.92 (3.17) | 11.51 (2.84) | 11.26 (3.42)a | 10.14 (3.07)a | 11.84 (3.28) | 10.07 (3.09) | -.56 (-.84, -.27) | 9.39** | 4.41* | .02 |
| PPI Machiavellian Egocentricity | 12.35 (3.80) | 11.89 (3.30) | 13.07 (4.28) | 12.43 (3.93) | 12.12 (3.97)b | 11.43 (3.40)b | -.19 (-.46, .09) | 1.70 | .12 | .00 |
| Reactive-Proactive Aggression Questionnaire | ||||||||||
| RPQ Proactive | .68 (1.41) | .54 (1.03) | .66 (1.26) | .39 (1.13) | .54 (2.08) | .37 (.65) | -.11 (-.39, .17) | 1.52 | .28 | .00 |
| RPQ Reactive | 4.45 (3.62) | 5.25 (3.60) | 4.17 (3.22) | 4.84 (3.21) | 3.82 (3.55) | 3.72 (2.73)b | -.03 (-.31, .25) | 1.21 | 3.15* | .02 |
| RPQ Total | 5.13 (4.48) | 5.79 (4.18) | 4.83 (4.13) | 5.23 (3.81)a | 4.36 (5.11) | 4.09 (3.09)b | -.06 (-.03, .21) | .25 | 2.21 | .01 |
indicates within group behavior change from 0 to 6 months was statistically significant (p< .05).
indicates within group behavior change from 6 to 12 months was statistically significant (p< .05).
Figure 2.
Significant group × time interactions (with standard error bars) for parents’ self-reports of their own psychopathy and reactive aggression.
For reactive aggression, all groups showed declines over time, but the within-group post-treatment decline was greater in the omega-3 group than in controls with respect to both 6-12 months within-group change scores (t = 2.15, df = 198, p = .04, d = -.30, CI = -.03 to -.58) and also 0 – 12 month change scores (t = 2.12, df = 198, p = .04, d = -.30, CI = -.02 to - .58). Groups did not differ from each other at the end point (12 months).
Influence of placebo effects
Becausethe above results documented a short-term placebo effect for parent reports of child behavior, groups were examined for differences in their belief in group assignment, and whether this could explain group differences in child behavior. By the end of treatment at 6 months, caregivers withchildrenrandomizedinto the treatment groupwere more likely to believe their children were receiving omega-3 (97%) compared to the placebo group (53%) (chi2 = 51.63, df = 1, p < .0001, eta = .51)
To assess if this belief influenced parental perception of their child’s behavior, this measure was entered as a covariate in all previously significant analyses. After controlling for parental belief in treatment allocation, the group × time interaction for parental reports remained significant for externalizing behavior (F[2,394] = 7.59, p = .001, eta2 = .04) and internalizing behavior (F[2,394] = 6.44, p = .002, eta2 = .03). All other previously significant findings remained significant (p < .05). One previously non-significant interaction for narcissism became significant after controlling for parental belief (F[2,195] = 8.44, p = .048, eta2 = .02).
Factors influencing improvement in parental behavior
We tested whether improvements in the child’s behavior at 12 months partly accounted for improvement in their parent’s behavior at 12 months. Improvement in child callous-unemotional traits (indirect effect: β = .04, p< .05), reactive aggression (indirect effect: β = .02, p< .05), and total RPQ aggression (indirect effect: β = .02, p< .05) all separately mediated improvement in parental psychopathy, but not parental reactive aggression. No other child improvements were found to mediate improved parental behavior (p > .05). In total, improvement in child behavior following treatment accounted for 38.7% of the improvement in parental antisocial behavior.
Factors accounting for improvementin child behavior
Omega-3treatment of the child was associated with improvements in their parent’s behavior. Improved parental behaviormay therefore partly account for the treatment effect on child behavior.
Testing this hypothesis, changes in parental psychopathy partly mediated child treatment outcomes for callous-unemotional traits (indirect effect: β = .06, p< .05), reactive aggression (indirect effect: β = .06, p< .05), and total RPQ aggression (indirect effect: β = .06, p< .05). Changes in parental reactive aggression partly mediated child treatment effects for anxious-depressed (indirect effect: β = .02, p< .05). No other parental improvement mediated improved child behavior (p > .05). In total, improvement in parental behavior accounted for 60.9% of the improvement in child antisocial behavior and 40.0% of the improvement in child anxious-depressed behavior.
Adverse events
No major adverse events were reported. Minor adverse events during the six month treatment period were reported by 17 parents (8.5%) and 6 children (3%) (see Supplementary Table S2).There were no significant group differences for parent-reports (chi2 = 1.61, df = 1, p = .21) or child-reports (chi2 = 0.69, df = 1, p = .41). No participant withdrew due to these minor events.
Discussion
The study’s main finding was that omega-3 supplementation for 6 months resulted in a 41.6% reduction in parent-rated child externalizing behavior half-a-year after treatment ended. A similar long-term reduction (68.4%) was observed for internalizing behavior.Results could not easily be attributed to placebo expectations. Findings are mitigated by the failure to observe similar effects for child self-reports, with the exception of significant short-term reductions in self-report child reactive (58.9% reduction) and proactive (49.7%) aggression. In the parents of treated children, significantreductions were also observed in parental psychopathy and reactive aggression. Improvement in parental behavior accounted for 60.9% of the improvement in child antisocial behavior. To our knowledge, this is the first study to document support for the longer-term post-treatment efficacy of omega-3 in reducing child and adolescent externalizing and internalizing behavior, and to document reduced antisocial behavior in caregivers.
Improvements in child behavior problems
In addition to significant improvements in aggressive and antisocial behaviors, the medium effect size (d = -.58) for long-term improvement in callous-unemotional traits is notable given the recent addition of this trait as a specifier in DSM-V (American Psychiatry Association, 2013) and the increasing interest in child psychopathic-like behavior (Frick et al., 2014). This finding might be expected as low omega-3 has been associated with high callous-unemotional traits in children with ADHD(Gow et al., 2013). In contrast, 18 out of 20 treatment studies report poorer outcomes in antisocial adolescents with callous-unemotional traits compared to those without these traits (Frick et al., 2014). Furthermore there is very little research focused on callous-unemotional traits themselves (Frick et al., 2014). In this context, omega-3 interventions may be an option in tackling this particular treatment challenge.
While the primary focus of this study was on antisocial and aggressive behavior, positive treatment effects were also observed for almost all internalizing behavior problems. While omega-3 supplementation has been shown in some studies to reduce childhood depression(Nemets, Nemets, Apter, Bracha, & Belmaker, 2006), overall the evidence from RCTs of omega-3 on depression is mixed (Giles, Mahoney, & Kanarek, 2013). Similar mixed conclusions have been drawn for omega-3 RCTs on ADHD, with some reviews suggesting small positive effects (Bloch & Qawasmi, 2011)while others suggest null results(Gillies, Sinn, Lad, Leach, & Ross, 2012). Clearly the current findings on internalizing behavior must be treated with caution, while also suggestingthat efficacy for internalizing behavior problems is worthy of further investigation.
Mechanisms of action
While study cannot identify proximal neurobiological mechanisms whereby omega-3results in long-term reductions externalizing behavior problems, callous-unemotional traits, and reactive / proactive aggression,this long-chain fatty acid plays a critical role in brain structure and function, making up approximately 35% of the cell membrane, enhancing neurite outgrowth, and regulating both neurotransmitter functioning and gene expression (McNamara & Carlson, 2006).In this context an RCT of omega-3 in children has been shown to enhance dorsolateral prefrontal functioning(McNamara & Carlson, 2006), a brain area found to be impaired in antisocial individuals(Fairchild et al., 2013; Yang & Raine, 2009; Seguin, Nagin, Assaad, & Tremblay, 2004). Future studies could therefore test the mediating hypothesis that omega-3 reduce antisocial behavior by enhancing prefrontal functioning.
Despite this study limitation, we were able to assess the mediating role of parental behavior on treatment efficacy. Giving children omega-3 resulted in improvements in their caregivers’ antisocial behavior compared to controls. This parental improvementpartly mediated improvements in child behavior produced by omega-3supplementation. Specifically, reductions in parental psychopathy accounted for 60.9% of the improvement in child antisocial behavior. Because caregiversand their children have reciprocal effects on one another (Dodge & Pettit, 2003), it is not surprising to anticipate improvements in child behavior evoking improvement in parental behavior that further improves child behavior. Surprising however, no prior study of omega-3 on any child behavior has, to our knowledge, tested this reciprocity hypothesis. While initial, this finding highlights an intermediary parental behavioral mechanism for improved child behavior following omega-3 supplementation that requires further investigation.
Placebo effects
Improvements in child behavior were not explained by parent’s belief in treatment allocation, with the group × time interaction effects remaining significant after controlling for this belief. On the contrary, effects for the narcissism component of the child psychopathy measure became significant after controlling for this confound. These findings dictate against a placebo effect as an explanation for the sustained improvement in child behavior over time.
Nevertheless, the placebo group did show improvements during the initial test period up to 6 months on several outcomes. While expectation of improvement with treatment enrollment likely contributed to this effect, it is also conceivable that the antioxidants and vitamin D contained in the placebo drink may have contributed to this transient change given some evidence suggesting potential efficacy of micronutrient supplementation for antisocial behavior(Benton, 2007).
Reporter Effects
Improvement in child behavior following omega-3 consumption was observed for parent reports, but with the exception of proactive and reactive aggression, no effects were observed with child self-reports. Similar results have been observed in other studies. The only two RCTs of omega-3 conducted in prison which documented behavioral improvement as monitored by others either failed to observe effects for self-reports (Zaalberg et al., 2010) or did not report findings beyond baseline data (Gesch et al., 2002). SimilarlyLong & Benton (2013) found no effect of omega-3 on self-report aggression, but did find reduced aggression on a laboratory behavioral measure of aggression.
The fact that effects were nevertheless obtained for child self-reported proactive and reactive aggression may be due to the fact that in the construction of this self-report measure, it was argued that children know better than their parents the underlying motive for aggressive behavior, a factor critical for distinguishing goal-oriented proactive aggression from aggression in reaction to a provocation (Raine et al., 2006). While the null results for other self-report should be viewed as a limitation, from a clinical perspective the very large majority of clinicreferrals for behavioral problems are from parents, not children. Consequently the current findings for parental reportsmay have clinical relevance.
Study limitations and generalizability
Regarding limitations, the ITT approach which analyzed all participants irrespective of treatment completion is viewed as an important defense against selection bias (White et al., 2011) and is viewed as the primary approach to data analysis in RCTs(Hernan & Hernandez-Diaz, 2012). It is nevertheless believed to underestimate treatment effects on placebo-controlled RCTs (Hernan & Hernandez-Diaz, 2012). The sample size of 200 is not large, although given that more than 50% of all registered RCTs have fewer than 70 participants by design (Califf et al., 2012), the completed sample and associated statistical power compares favorably to other trials. While long-term post-treatment improvement was observed, we caution that this time period is six months and findings may or may not extend for longer. Furthermore, long-term effects were not observed for proactive and reactive aggression.
Caveats are also needed on generalizability of findings. While Mauritius is a developed country, future generalization to other countries and other ethnic groups is required. Furthermore, the research staff reported unusually strong enthusiasm to participate in this treatment study compared to the risk research normally conducted at the Joint Child Health Project. This again cautions against generalization of findings from this RCT to other international settings.
Conclusions
In conclusion, this RCT shows that six months of omega-3 supplementation in fruit juice drink form results in a 42-68% reduction in parent-reported externalizing and internalizing behavior problems in community-residing children and adolescents, with improvement continuing six months after treatment cessation. While replication and generalization to other countries is critical, the potential clinical promise is that these nutrients can shift the distribution of behavior problems to a lower level in the general population and that more severe behavioral problems that are significant risk factors for serious adult violence and psychopathology may be ameliorated.
Supplementary Material
Table S1. CONSORT flow diagram.
Table S2. Minor adverse events
Figure S1. Child proactive and reactive aggression.
Key Points.
-
▪
It is unclear whether omega-3 supplementation can reduced externalizing and internalizing behavior problems in child and adolescent populations
-
▪
This RCT showed that six months of omega-3supplementation in fruit juice form produced long-term post-treatment reductions in parent-reported externalizing behavior problems (41.6%) and internalizing behavior problems (68.4%).
-
▪
Caregivers of children receiving omega-3 also showed significant reductions in their own antisocial behavior)
-
▪
Improvements in parental behavior accounted for 60.9% of the improvement in child behavior
-
▪
This is the first study to report not just post-treatment reductions in child antisocial behavior, but also to document improvements in parental behavior that in part explain treatment efficacy.
Acknowledgments
This study was supported in part by the Intramural Research Program of the National Institute on Alcohol Abuse and Alcoholism, Rockville, MD, the University of Pennsylvania, and Smartfish AS, Oslo, Norway. The authors wish to thank Shameem Oomur, Shameemah Golamnobee, and Joelle Rawoteea for their assistance in data collection.
Acronyms
- CBC
Child Behavior Checklist
- RPQ
Reactive-Proactive Aggression Questionnaire
- RCT
Randomized controlled trial
Footnotes
Additional supporting information can be found in the online version of this article:
Declaration of interest. This study was made possible in part by funding from Smartfish AA, Oslo, Norway, who produced the omega-3 supplementand placebo drink used in this study.
Reference List
- Achenbach TM, Rescorla L. Manual for the ASEBA School-age forms & profiles. Burlington: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- American Psychiatry Association. Diagnostic and statistical manual of mental disorders. 5. Wshington, D.C.: American Psychiatric Association; 2013. [Google Scholar]
- Baker LA, Raine A, Liu JH, Jacobson KC. Differential Genetic and Environmental Influences on Reactive and Proactive Aggression in Children. Journal of Abnormal Child Psychology. 2008;36:1265–1278. doi: 10.1007/s10802-008-9249-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benton D. The impact of diet on anti-social, violent and criminal behaviour. Neuroscience and Biobehavioral Reviews. 2007;31:752–774. doi: 10.1016/j.neubiorev.2007.02.002. [DOI] [PubMed] [Google Scholar]
- Bloch MH, Qawasmi A. Omega-3 Fatty Acid Supplementation for the Treatment of Children With Attention-Deficit/Hyperactivity Disorder Symptomatology: Systematic Review and Meta-Analysis. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:991–1000. doi: 10.1016/j.jaac.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Califf RM, Zarin DA, Kramer JM, Sherman RE, Aberle LH, Tasneem A. Characteristics of Clinical Trials Registered in ClinicalTrials.gov, 2007-2010. Jama-Journal of the American Medical Association. 2012;307:1838–1847. doi: 10.1001/jama.2012.3424. [DOI] [PubMed] [Google Scholar]
- Del Re AC, Maisel NC, Blodgett JC, Finney JW. Intention-to-treat analyses and missing data approaches in pharmacotherapy trials for alcohol use disorders. BMJ Open. 2013;3:e003464. doi: 10.1136/bmjopen-2013-003464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge KA, Pettit GS. A biopsychosocial model of the development of chronic conduct problems in adolescence. Developmental Psychology. 2003;39:349–371. doi: 10.1037//0012-1649.39.2.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairchild G, Hagan CC, Walsh ND, Passamonti L, Calder AJ, Goodyer IM. Brain structure abnormalities in adolescent girls with conduct disorder. Journal of Child Psychology and Psychiatry. 2013;54:86–95. doi: 10.1111/j.1469-7610.2012.02617.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairchild G, Passamonti L, Hurford G, Hagan CC, von dem Hagen EAH, Van Goozen SHM, et al. Brain Structure Abnormalities in Early-Onset and Adolescent-Onset Conduct Disorder. American Journal of Psychiatry. 2011;168:624–633. doi: 10.1176/appi.ajp.2010.10081184. [DOI] [PubMed] [Google Scholar]
- Fossati A, Raine A, Borroni S, Bizzozero A, Volpi E, Santalucia I, et al. A Cross-Cultural Study of the Psychometric Properties of the Reactive-Proactive Aggression Questionnaire Among Italian Nonclinical Adolescents. Psychological Assessment. 2009;21:131–135. doi: 10.1037/a0014743. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Bodin SD, Barry CT. Psychopathic traits and conduct problems in community and clinic-referred samples of children: Further development of the psychopathy screening device. Psychological Assessment. 2000;12:382–393. [PubMed] [Google Scholar]
- Frick PJ, Ray JV, Thornton LC, Kahn RE. Can Callous-Unemotional Traits Enhance the Understanding, Diagnosis, and Treatment of Serious Conduct Problems in Children and Adolescents? A Comprehensive Review. Psychological Bulletin. 2014;140:1–57. doi: 10.1037/a0033076. [DOI] [PubMed] [Google Scholar]
- Fung ALC, Raine A, Gao Y. Cross-Cultural Generalizability of the Reactive-Proactive Aggression Questionnaire (RPQ) Journal of Personality Assessment. 2009;91:473–479. doi: 10.1080/00223890903088420. [DOI] [PubMed] [Google Scholar]
- Gesch CB, Hammond SM, Hampson SE, Eves A, Crowder MJ. Influence of supplementary vitamins, minerals and essential fatty acids on the antisocial behaviour of young adult prisoners: Randomised, placebo- controlled trial. British Journal of Psychiatry. 2002;181:22–28. doi: 10.1192/bjp.181.1.22. [DOI] [PubMed] [Google Scholar]
- Giles GE, Mahoney CR, Kanarek RB. Omega-3 fatty acids influence mood in healthy and depressed individuals. Nutrition Reviews. 2013;71:727–741. doi: 10.1111/nure.12066. [DOI] [PubMed] [Google Scholar]
- Gillies D, Sinn JKH, Lad SS, Leach MJ, Ross MJ. Polyunsaturated fatty acids (PUFA) for attention deficit hyperactivity disorder (ADHD) in children and adolescents. Cochrane Database of Systematic Reviews. 2012 doi: 10.1002/14651858.CD007986.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn AL, Raine A. Psychopathy: An introduction to biological findings and their implications. New York: New York University Press; 2014. [Google Scholar]
- Gow RV, Vallee-Tourangeau F, Crawford MA, Taylor E, Ghebremeskel K, Bueno AA, et al. Omega-3 fatty acids are inversely related to callous and unemotional traits in adolescent boys with attention deficit hyperactivity disorder. Prostaglandins Leukotrienes and Essential Fatty Acids. 2013;88:411–418. doi: 10.1016/j.plefa.2013.03.009. [DOI] [PubMed] [Google Scholar]
- Gustafsson PA, Birberg-Thornberg U, Duchen K, Landgren M, Malmberg K, Pelling H, et al. EPA supplementation improves teacher-rated behaviour and oppositional symptoms in children with ADHD. Acta Paediatrica. 2010;99:1540–1549. doi: 10.1111/j.1651-2227.2010.01871.x. [DOI] [PubMed] [Google Scholar]
- Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. White Paper [On-line] 2012 Available: http://www.afhayes.com/public/process2012.pdf.
- Hernan MA, Hernandez-Diaz S. Beyond the intention-to-treat in comparative effectiveness research. Clinical Trials. 2012;9:48–55. doi: 10.1177/1740774511420743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbeln JR. Homicide mortality rates and seafood consumption: A cross-national analysis. World Review of Human Nutrition. 2001;88:41–46. doi: 10.1159/000059747. [DOI] [PubMed] [Google Scholar]
- Lilienfeld SO, Andrews BP. Development and preliminary validation of a self-report measure of psychopathic personality traits in noncriminal populations. Journal of Personality Assessment. 1996;66:488–524. doi: 10.1207/s15327752jpa6603_3. [DOI] [PubMed] [Google Scholar]
- Lin YH, Loewke JD, Hyun DY, Leazer J, Hibbeln JR. Fast Transmethylation of Serum Lipids Using Microwave Irradiation. Lipids. 2012;47:1109–1117. doi: 10.1007/s11745-012-3714-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JH. Early health risk factors for violence: Conceptualization, evidence, and implications. Aggression and Violent Behavior. 2011;16:63–73. doi: 10.1016/j.avb.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JH, Raine A, Venables PH, Dalais C, Mednick SA. Malnutrition at age 3 years and externalizing behavior problems at ages 8, 11 and 17 years. American Journal of Psychiatry. 2004;161:2005–2013. doi: 10.1176/appi.ajp.161.11.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long SJ, Benton D. A double-blind trial of the effect of docosahexaenoic acid and vitamin and mineral supplementation on aggression, impulsivity, and stress. Human Psychopharmacology-Clinical and Experimental. 2013;28:238–247. doi: 10.1002/hup.2313. [DOI] [PubMed] [Google Scholar]
- Long SJ, Benton D. A double-blind trial of the effect of docosahexaenoic acid and vitamin and mineral supplementation on aggression, impulsivity, and stress. Human Psychopharmacology-Clinical and Experimental. 2013;28:238–247. doi: 10.1002/hup.2313. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maughan B. Editorial: “Better by design” why randomized controlled trials are the building blocks of evidence-based practice. Journal of Child Psychology and Psychiatry. 2013;54:225–226. doi: 10.1111/jcpp.12051. [DOI] [PubMed] [Google Scholar]
- McNamara RK, Carlson SE. Role of omega-3 fatty acids in brain development and function: Potential implications for the pathogenesis and prevention of psychopathology. Prostaglandins Leukotrienes and Essential Fatty Acids. 2006;75:329–349. doi: 10.1016/j.plefa.2006.07.010. [DOI] [PubMed] [Google Scholar]
- Milte CM, Parletta N, Buckley JD, Coates AM, Young RM, Howe PR. Eicosapentaenoic and docosahexaenoic acids, cognition, and behavior in children with attention-deficit/hyperactivity disorder: A randomized controlled trial. Nutrition. 2012;28:670–677. doi: 10.1016/j.nut.2011.12.009. [DOI] [PubMed] [Google Scholar]
- Moher D. CONSORT 2010 Explanation and Elaboration: updated guidelines for reporting parallel group randomised trials. British Medical Journal. 2010;343:c869. doi: 10.1136/bmj.c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemets H, Nemets B, Apter A, Bracha Z, Belmaker RH. Omega-3 treatment of childhood depression: A controlled, double-blind pilot study. American Journal of Psychiatry. 2006;163:1098–1100. doi: 10.1176/ajp.2006.163.6.1098. [DOI] [PubMed] [Google Scholar]
- Neugebauer R, Hoek HW, Susser E. Prenatal exposure to wartime famine and development of antisocial personality disorder in early adulthood. JAMA: Journal of the American Medical Association. 1999;282:455–462. doi: 10.1001/jama.282.5.455. [DOI] [PubMed] [Google Scholar]
- Raine A. From Genes to Brain to Antisocial Behavior. Current Directions in Psychological Science. 2008;17:323–328. [Google Scholar]
- Raine A, Dodge K, Loeber R, Gatzke-Kopp L, Lynam D, Reynolds C, et al. The reactive-proactive aggression questionnaire: Differential correlates of reactive and proactive aggression in adolescent boys. Aggressive Behavior. 2006;32:159–171. doi: 10.1002/ab.20115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raine A, Liu JH, Venables PH, Mednick SA, Dalais C. Cohort Profile: The Mauritius Child Health Project. International Journal of Epidemiology. 2010;39:1441–1451. doi: 10.1093/ije/dyp341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seguin JR, Nagin D, Assaad JM, Tremblay RE. Cognitive-neuropsychological function in chronic physical aggression and hyperactivity. Journal of Abnormal Psychology. 2004;113:603–613. doi: 10.1037/0021-843X.113.4.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrier I, Steele RJ, Verhagen E, Herbert R, Riddell CA, Kaufman JS. Beyond intention to treat: What is the right question? Clinical Trials. 2014;11:28–37. doi: 10.1177/1740774513504151. [DOI] [PubMed] [Google Scholar]
- Sinn N, Milte C, Howe PR. Oiling the Brain: A Review of Randomized Controlled Trials of Omega-3 Fatty Acids in Psychopathology across the Lifespan. Nutrients. 2010;2:128–170. doi: 10.3390/nu2020128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suresh K. An overview of randomization techniques: An unbiased assessment of outcome in clinical research. Journal of Human Reproductive Sciences. 2011;4:8–11. doi: 10.4103/0974-1208.82352. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Viding E, Sebastian CL, Dadds MR, Lockwood PL, Cecil CA, De Brito SA, et al. Amygdala Response to Preattentive Masked Fear in Children With Conduct Problems: The Role of Callous-Unemotional Traits. American Journal of Psychiatry. 2012;169:1109–1116. doi: 10.1176/appi.ajp.2012.12020191. [DOI] [PubMed] [Google Scholar]
- White I, Horton NJ, Pocock SJ. Strategy for intention to treat analysis in randomised trials with missing outcome data. British Medical Journal. 2011;342:d40. doi: 10.1136/bmj.d40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang YL, Raine A. Prefrontal structural and functional brain imaging findings in antisocial, violent, and psychopathic individuals: A meta-analysis. Psychiatry Research-Neuroimaging. 2009;174:81–88. doi: 10.1016/j.pscychresns.2009.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarnell LM, Sargeant MN, Prescott CA, Tilley JL, Farver JA, Mednick SA, et al. Measurement Invariance of Internalizing and Externalizing Behavioral Syndrome Factors in a Non-Western Sample. Assessment. 2013;20:642–655. doi: 10.1177/1073191113498114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young SN. The effect of raising and lowering tryptophan levels on human mood and social behaviour. Philosophical Transactions of the Royal Society B-Biological Sciences. 2013;368 doi: 10.1098/rstb.2011.0375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaalberg A, Nijman H, Bulten E, Stroosma L, van der Staak C. Effects of Nutritional Supplements on Aggression, Rule-Breaking, and Psychopathology Among Young Adult Prisoners. Aggressive Behavior. 2010;36:117–126. doi: 10.1002/ab.20335. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. CONSORT flow diagram.
Table S2. Minor adverse events
Figure S1. Child proactive and reactive aggression.


