Abstract
Aims
The levator ani muscle (LA) injury associated with vaginal birth occurs in a characteristic site of injury on the inner surface of the pubic bone to the pubovisceral portion of the levator ani muscle's origin. This study investigated the gross and microscopic anatomy of the pubic origin of the LA in this region.
Methods
Pubic origin of the levator ani muscle was examined in situ then harvested from nine female cadavers (35 - 98 years). A combination of targeted feature sampling and sequential sampling was used where each specimen was cut sequentially in approximately 5 mm thick slices apart in the area of known LA injury. Histological sections were stained with Masson's trichrome.
Results
The pubovisceral origin is transparent and thin as it attaches tangentially to the pubic periosteum, with its morphology changing from medial to lateral regions. Medially, fibers of the thick muscle belly coalesce towards multiple narrow points of bony attachment for individual fascicles. In the central portion there is an aponeurosis and the distance between muscle and periosteum is wider (~ 3 mm) than in the medial region. Laterally, the LA fibers attach to the levator arch where the transition from pubovisceral muscle to the iliococcygeal muscle occurs.
Conclusions
The morphology of the levator ani origin varies from the medial to lateral margin. The medial origin is a rather direct attachment of the muscle, while lateral origin is made through the levator arch.
Keywords: Vaginal birth injury, Levator ani muscle, Pubovisceral muscle, Pubococcygeal muscle, Aponeurosis, Enthesis, Histology
Introduction
Vaginal delivery is known to cause defects in the pelvic floor structures, including the levator ani muscle and the connective tissue around it.2-4 Due to tensile stretch during vaginal delivery that is twice the value tolerated by striated muscle in non-pregnant individuals,5 the levator ani muscle is subject to significant structural changes, including muscle tears or even avulsion.2 These injuries appear to occur in a characteristic “injury zone” on the inner surface of the pubic bone at the origin of the puboviscerala (PVM) but do not involve the puborectal muscle.2, 8-10 There are several constituent parts to the PVM origin. As can be seen in Fig. 1, the substructures in this anatomical region include the pubovisceral portion of the levator ani muscle, the levator arch (also known as arcus tendineus levator ani), and the fascial arch also known as arcus tendineus fascia pelvis). This raises the possibility of morphological differences in the pubovisceral muscle origin along the pelvic sidewall. Although a number of previous studies have been conducted on this region using histological slides,6, 11, 12 detailed morphological differences in the origins of the various sub-parts of the levator ani within this region are lacking.
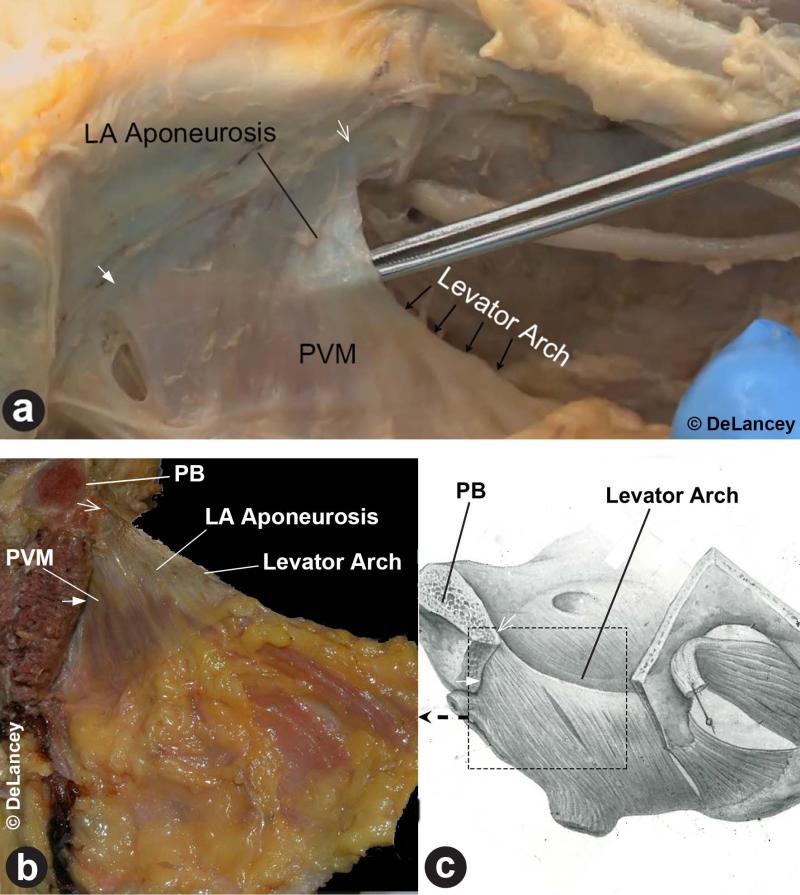
Figure 1.
(a) Left mediolateral view of the anterior pelvic sidewall, with pelvic organs removed, showing the characteristic features of the origin of the pubovisceral muscle. The dotted quadrangle shows the anatomic area of study. (Reproduced from Halban and Tandler (1), Figure 2, p. 34) (b) A similar view of the right anterior pelvic sidewall of a 50 year old nulliparous fresh cadaver showing the pubovisceral attachments to the pubic bone. The fascial arch lies across the pubovisceral muscle, and the levator arch forms the lateral margin of the pubovisceral muscle as it attaches onto the pelvic sidewall.
The purpose of this study, therefore, was to establish the gross and microscopic anatomy of the pubic origin of the levator ani muscle as it relates to birth-induced injury.
Materials and Methods
Specimen acquisition and histochemical analysis were focused on the pubic origin of the levator ani muscle, which can span from approximately 1 cm lateral from the pubic symphysis to the origin of the levator arch that lies just ventral to the obturator canal (Fig. 2). Nine female cadavers, four of which were nulliparous, were collected with the support of the Anatomical Donations Program at the University of Michigan. The cadaveric specimens ranged from 35 to 98 years of age, with a mean age of 66 years old. The senior author (JOLD), who has extensive dissection and imaging experience in evaluating the levator ani muscle, assessed all the specimens and none showed signs of major pelvic floor muscle damage associated with maternal birth.
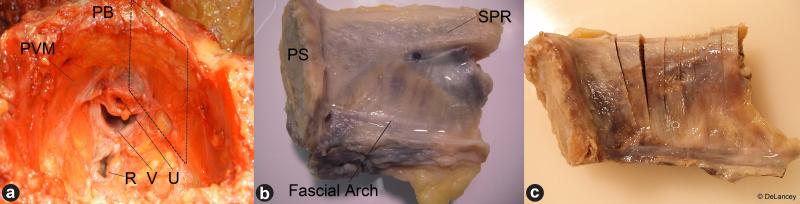
Figure 2.
(a) Superior view of the ventral pelvis after organ removal. The dotted quadrangle shows the area from which histological specimens were acquired. (b) An example of an excised specimen block which includes the right side of the pubovisceral muscle origin from the inter surface of the pubic bone showing the pubic symphysis at left. (c) Sectioning strategy of the pubovisceral muscle origin harvesting showing sequential cuts at ~ 5 mm intervals. (PB: pubic bone; PVM: pubovisceral muscle; U: urethra; V: vagina; R: rectum; PS: pubic symphysis; SPR: superior pelvis ramus).
Histological samples were acquired using targeted feature sequential sampling to obtain representative samples of the region of interest (ROI). The purpose of this acquisition strategy was to show the variation of the detailed morphological and structural relationships along the pubic origin of the PVM without losing important anatomical features, such as the origin of the levator archb and the fascial archc, the merging point of the both arches, and/or the muscle-bone interface of the PVM origin. Once a smaller portion of the sample was excised from the whole pelvis, the sequential precuts on the superior portion of the sample were made at an interval of approximately 5 mm, care being taken to keep the integrity of the structure intact. These were photographed for later reference. The detailed fiber orientation, as well as the enthesis or junction between the pubovisceral muscle and the pubic bone, were thoroughly examined using magnification when necessary before the pubic bones and the attached muscles were removed, so that the final sectioning was able to be made parallel to the fiber direction.
Samples were removed for histochemical processing by cutting them parallel to the PVM fiber direction. The samples were fixed in 10 % neutral buffered formalin, decalcified in 10% formic acid for 10-30 days depending on the size of the original specimen, and then stored in 70 % ethanol. Paraffin embedding was then applied followed by serial sectioning of samples less than 7 μm in thickness. Masson's trichrome staining was applied in order to effectively distinguish muscular cells from connective tissue. Finally, digital conversion of the stained slide was conducted using a Super COOLSCAN 5000 ED film scanner (Nikon, Shinjuku, Tokyo, Japan).
Results
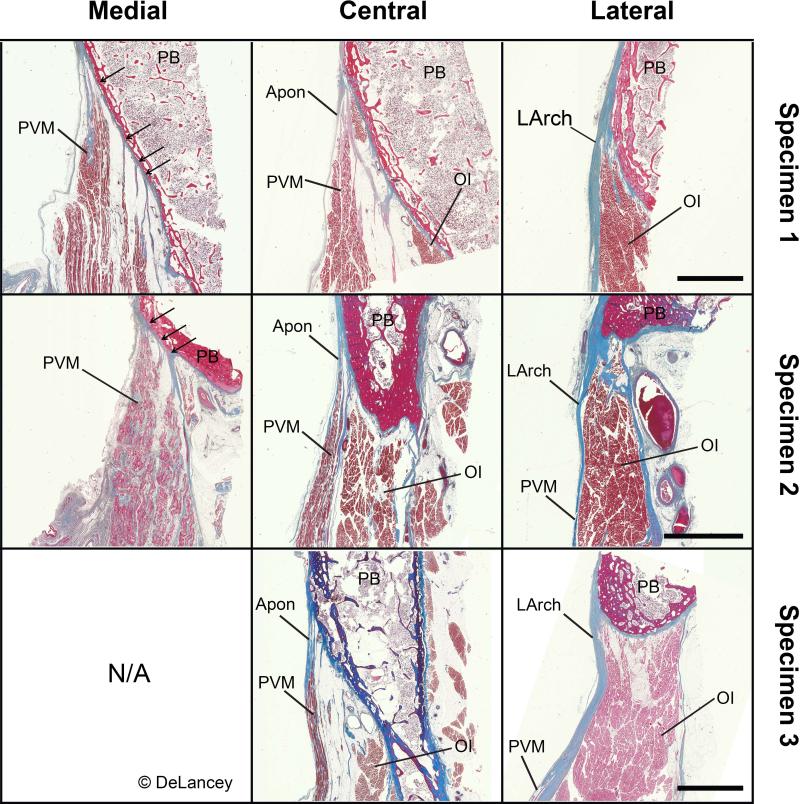
The PVM originates tangentially from the periosteum covering the pubic bone and the nature of this attachment changes from the medial to lateral regions and can be divided into three regions: medial, central, and lateral. Figure 3a shows the inner surface of the muscle seen from inside the pelvis. Panel b is a view of the outer surface of the muscle seen from outside the pelvis after the anterior pubic bone and obturator internus were removed to provide visual access to the lateral PVM surface as shown diagrammatically in Panel c.
Figure 3.
(a) A view of the inner surface of the right pubic origin of the PVM similar in orientation with Figure 2b. Note how thin the semitransparent levator ani (LA) aponeurosis is (i.e. tips of a clamp being visible through the aponeurosis) as it attaches to the superior pubic ramus. This aponeurosis poses a smooth transition from the muscular area of the PVM to the periosteum of the pubic bone. Medially the muscle can be seen to extend closer to the bone than it is laterally where the aponeurosis widens. (b & c) Left lateromedial view of the left PVM origin area seen from outside the pelvis after the lateral pelvic bone was removed to reveal the outside of the aponeurotic levator ani muscle. Note that the medial portion of the left PVM extends to the bone while the more lateral portion has a wide aponeurosis between the muscle and bone. The rectangle shows the view shown in Figure 3b. (Panel c reproduced by permission from Anson (13), p. 474). In this and succeeding figures, closed arrows designate medial origin, and open arrows designate lateral LArch attachment that form the origin of the PVM.
The medial portion of the PVM origin has a relatively direct connection between muscle and bone. In the central portion, the ends of the muscle fibers are attached to the periosteum by a thin semitransparent aponeurotic membrane. The distance from the end of the muscle fascicles to periosteal attachment in this area is approximately 3 to 5 mm. This region lies on the inner surface of the obturator internus muscle, but no fusion between the two muscles was found as they were able to be separated easily by blunt dissection. The lateral portion of the PVM pubic origin attaches to the levator arch that runs from the pubic bone to the ischial spine at a point where the PVM blends into the iliococcygeal muscle. The muscle fibers were oriented radially from the levator arch origin.
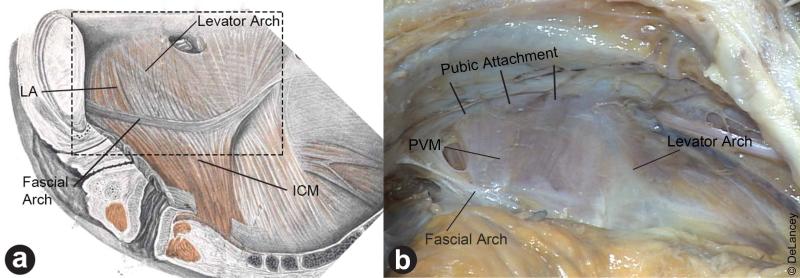
Histological cross-sections of the pubic interface of the PVM acquired from cadaveric specimens are shown in Figure 4. Each column of images shows one of the three regions while the different rows are examples from different individuals. In the medial region, the relatively thick muscle fascicles attach to the pubic bone by means of several short fibrous attachments. In the medial section there is an aponeurosis that bridges a widening distance between the end of the muscle fascicles and the periosteum. Laterally, the dense connective tissue band of the levator arch is seen. An angled interface between the muscle and the bone is also evident, especially in the medial region. The aponeurotic PVM widens in the central region resulting in a larger distance between the pubic bone and the ends of the muscle fascicles. The thickness of the PVM muscle belly thins as one moves laterally.
Figure 4.
Examples of medial, central and lateral region histology of the pubic origin of the PVM. Each row is from a different donor. Histological images showing the pubic origin of the levator ani from medial (column 1), central (column 2), and lateral (column 3) areas with the orientation picture below. All samples shown are stained in Masson's trichrome, and the scale bars are 5 mm for each row of images. Medial: The medial LA fibers originate from multiple slips attaching in an enthesis to the pubis; oblique interface between the pubic bone (PB) and the levator ani muscle (LA) can also be observed. The thickness of the LA is greater than in other areas. N/A denotes missing data due to a technical issue during harvesting process. Central: The central portion originates from the PB in a single aponeurotic attachment, which is noticeably thinner than medial portion. The obturator internus muscle (OI) can be seen lateral to the LA. Lateral: The levator arch (LArch) appears as dense blue connective tissue attaching to the PB and forming the lateral margin of the pubic origin of the LA. Note that relative preponderance of the three portions varies by individual.
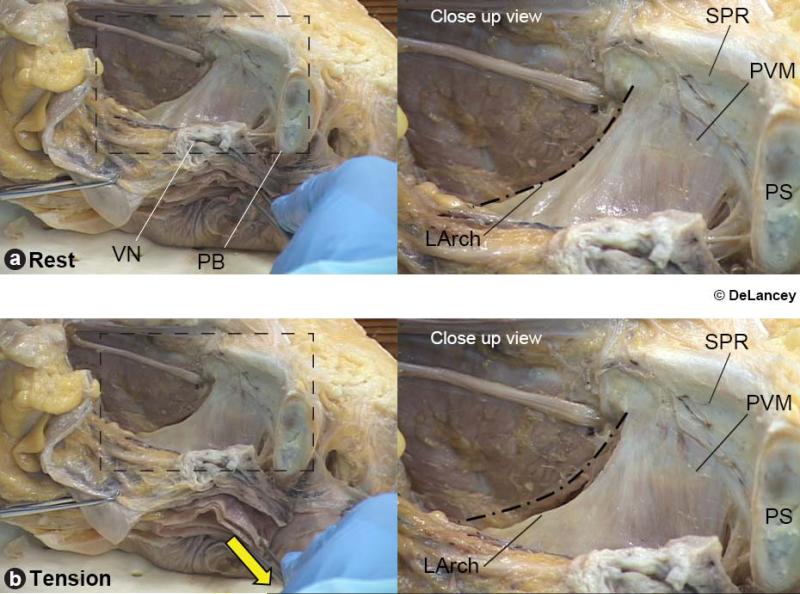
When repeated inferior traction forces were placed on the perineal tissues, in the direction typical of the loading late in a vaginal delivery, visible tension could be seen where the PVM originates from the pubic bone (Figure 5). This traction did not affect the obturator internus muscle. Although tension could be seen all along the muscle origin, it was concentrated most at the point where levator arch attached to the pubic bone.
Figure 5.
Three-quarter view taken from Video 1 of the inside of the left anterior pelvis of a fresh cadaveric specimen sectioned in the mid-sagittal plane. The views demonstrate how the PVM origin deforms in response to a downward force (yellow arrow) placed on the perineal structures. Resting position (a) and deformed position (b) are compared. Tension increases over the pubic origin of the levator ani and the attachment of the levator arch to the pubic bone as the perineal body area is pulled in the direction of loading typical late in a vaginal birth. (VN denotes vesical neck: PB: perineal body; SPR: superior pubic ramus; PVM: pubovisceral muscle; PS: pubic symphysis; LArch: levator arch)
Discussion
We have found characteristic features of the anatomy of the origin of the PVM in the region where both imaging studies and computer simulations have shown that birth-induced stretch injury can occur (see Introduction). The lateral margin of this region, which is formed with the levator arch, is a thick collagenous bundle connecting to the pelvic sidewall and the ischial spine with a catenary structure. This attachment pattern contrasts with the medial margin of the PVM attachment where the muscle is directly attached to the pubic bone via a fibrous enthesis.14 The medial portion that lies between these extremes was a thin semitransparent aponeurosis. Video 1 shows that when pelvic floor stretch similar to that occurring late in vaginal birth is applied, tension was placed on these attachments and concentrated at the lateral margin in the region of the levator arch.
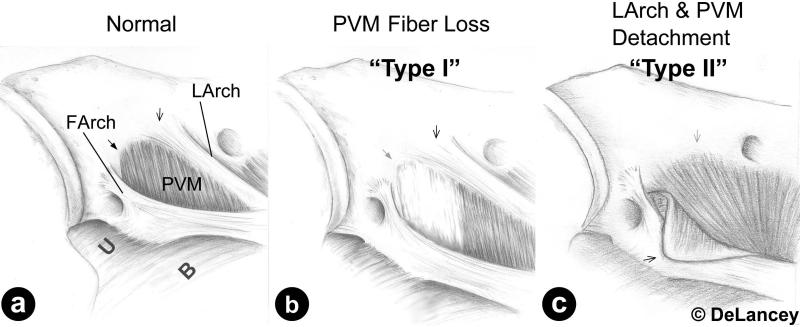
MRI studies of levator ani muscle injuries seen in this region have revealed two patterns; one that involves gross architectural distortion of the anatomy and one that reveals loss of muscle substance, but maintenance of the overall architecture.16 The result of our anatomical studies suggests a conceptual framework for these two types of maternal PVM injury (Figure 6). In “Type I” injury the injury is confined to individual portions of the PVM in which the portions of the muscle is missing. In this defect the levator arch remains intact but some substance of the muscle is lost. Histological study reveals this attachment to be a 'scarf enthesis',17 since it is an enthesis where the two heterogeneous materials - the PVM and the pubic bone - meet at an oblique angle. (An oblique junction is often referred to as a scarf joint in the engineering field.) In a computer simulation study that was conducted to examine how traction on the PVM affects the strain energy distribution at its origin, an oblique connection to the pubic bone, the results demonstrated a significant strain energy concentration appearing at the inferior margin of the scarf enthesis.17 This suggests a possible location for the initiation of the birth-related injury which we have designated a “Type I” injury.
Figure 6.
Illustrations of the right inner pelvic sidewall showing the fascial and levator arches originating from the pubic bone. (a) Two different types of the PVM origin can be identified: One being direct aponeurotic attachment in anteromedial portion (open arrow), the other being indirect catenary attachment through the levator arch (LArch) in posterolateral region (closed arrow). Morphological and functional variation in these locations may account for how injury might occur and progress. (b) Type I injury: PVM can locally be damaged, which then leads to PVM atrophy (semitransparent closed arrow). (c) Type II injury: Detachment of the LArch origin from the pubic bone (semitransparent open arrow) observed in 32 year old patient with stress urinary incontinence and history of a traumatic birth (3rd degree laceration). Since there is only a single point of pubic origin at the LArch for the lateral margin of the PVM, detachment of that point will result in complete offloading of that region of the PVM. (Modified from Fig. 2a of Delancey (15))
The second type of injury (“Type II”) would involve detachment of the catenary-like levator arch from the pubic bone by excessive tension created in this region during vaginal birth. This “Type II” injury would involve a loss of the normal architecture of the pelvic sidewall due to loss of this critical attachment. This is consistent with the characteristic abnormal appearance of the vagina in the same region where damage to the PVM is seen and involves changes on the overall architecture of this region.18 MR images of women with the architectural distortion showed significant alteration in the levator arch anatomy along with lateral or posterior spill of the vagina from its normal position.16 It is also consistent with the downward displacement in the levator arch seen in these individuals.18 Unlike the Type I injury, where there is only a loss of muscle substance, the Type II injury results in a change in the architecture of the supportive tissues and may be responsible for the additional risk of prolapse seen in these women.16, 18 It seems likely as well that the Type I injuries seen after first birth may place women at increased risk for Type II in subsequent births. This hypothesis remains to be tested.
The differences between these two types of injury may have implications for treatment. A muscle injury in which there are small portions of the muscle that are injured (Type I injury), but in which the overall attachments of the muscle remain intact, may certainly benefit from exercise that might help with reinnervation of injured fibers and could hypertrophy adjacent muscle to compensate for injury. On the other hand, a complete muscle detachment (Type II injury) would not benefit and early exercise might exacerbate the separation between the muscle and its origin. Also, the thin and almost transparent origin of the muscle makes it unlikely that this attachment would be amenable to surgical re-attachment. These clinical issues, however, require further study before definitive conclusions can be drawn.
Disruption of the catenary structure of the levator arch can be understood in mechanical terms. Engineering studies of catenary structures also indicate that extra care is needed in designing the cable itself because, as the main load-carrying pathway, failure can lead to catastrophic collapse when it is damaged.19, 20 Findings from anatomical and histological observations combined with imaging techniques allow the refinement of biomechanical models to investigate and simulate mechanical effects during delivery and test hypotheses relating to regions of the pelvic floor that are vulnerable to injury.
Our methodological approach has several limitations. First, the sample size was small, so generalization of the results should be made with care until the results are corroborated by others, and the possible variations with age, parity and/or ethnicity have been checked. The availability of four nulliparous cadavers; a rarity in anatomical donation programs, is a strength of this study. Second, the observations of this study were based on cadaveric specimens whose topography is altered by death and the fixation process. We were able to minimize this effect by harvesting the entire pelvis fresh and then fixing via flotation so that the integrity of the structure was maintained as much as possible. Third, histological descriptions of the study region were focused on geometrical comparisons. More detailed histological descriptions are needed that include different types of collagen, decorin, biglycan, aggrecan and other possible constituents that may form this particular enthesis.21 Investigation of the nerve supply to this region might also be worthwhile, since pudendal nerve damage has been noted in women with pelvic floor dysfunction.22, 23 Finally, a traction force was applied to the top of the perineal body of a cadaveric hemipelvis in an attempt to show deformed pattern of the levator ani by increased intra-abdominal pressure. While we acknowledge that there is no existing data to support the applied traction being similar to that applied during labor, we were seeking to simulate tissue deformations rather than quantifying the magnitude of the loading.
The present study has provided a detailed morphologic description of the region of birth-related injury near the PVM origin. This may be valuable for a better understanding of the injury mechanism during vaginal delivery.24 The pubic origin of the PVM was examined in terms of three sub-regions or its pubic origin: medial, central, and lateral. Based on the understanding the structure through cadaver dissections, an analogy to simpler load bearing mechanical elements was made and a hypothetical injury mechanism and injury sequence are offered in the form of the Type I and II injury patterns.
Conclusion
The morphology of the origin of the levator ani near the pubic bone shows a changing pattern from medial to lateral margin. Unlike the medial area with its direct junction between the pubic bone and levator ani muscle, the central and lateral origins are thin and aponeurotic. What forms the most lateral margin is the levator arch in the form of a relatively thick collagenous bundle. Vaginal loading seems to be transferred mainly through the thick, direct medial attachment as well as the levator arch attachment.
Supplementary Material
The material can also be found in the following URL:http://vimeo.com/102735080.
Acknowledgements
The authors gratefully acknowledge the support of Dean Mueller, Director of the Anatomical Donation Program at the University of Michigan. We would also like to thank the histology core facility at the University of Michigan, School of Dentistry for the histological services. Digital conversion of the slides was performed in the Microscopy and Image-analysis Laboratory (MIL), Department of Cell & Developmental with the assistance of Shelley Almburg.
Funding
Support for this work was provided by National Institutes of Health, Office of Research on Women's Health (ORWH) grant, “Specialized Center of Research (SCOR) on Sex and Gender Factors Affecting Women's Health,” P50 HD044406. One of the authors (CB) received a postdoctoral mobility grant from the Swiss National Science Foundation.
Footnotes
Conferences
This study was presented at the 37th Annual Scientific Meeting of the International Urogynecological Association, Brisbane, Australia, September 2012 and the 33rd Annual Scientific Meeting of the American Urogynecologic Society, Chicago, IL, USA, October 2012.
We use the term ‘pubovisceral’6 in favor of the more common term ‘pubococcygeal’7 because the former term more accurately describes the anatomic sites of its origin and insertion in humans.
This term is used in lieu of the longer ‘arcus tendineus levator ani’
This term is used in lieu of the longer ‘arcus tendineus fascia pelvis’
Conflict of Interest
The University of Michigan received research grants providing partial salary support for Dr. DeLancey and Dr. Ashton-Miller from Johnson & Johnson and Proctor & Gamble, Inc., and from Boston Scientific for Dr. Ashton-Miller. The other authors have no disclosures to report.
References
- 1.Halban J, Tandler J. Anatomie und aetiologie der genitalprolapse beim weibe. Braumüller; 1907. [Google Scholar]
- 2.DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003;101(1):46–53. doi: 10.1016/s0029-7844(02)02465-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leijonhufvud A, Lundholm C, Cnattingius S, Granath F, Andolf E, Altman D. Risks of stress urinary incontinence and pelvic organ prolapse surgery in relation to mode of childbirth. Am J Obstet Gynecol. 2011;204(1):70, e1–7. doi: 10.1016/j.ajog.2010.08.034. [DOI] [PubMed] [Google Scholar]
- 4.Schwertner-Tiepelmann N, Thakar R, Sultan AH, Tunn R. Obstetric levator ani muscle injuries: current status. Ultrasound Obstet Gynecol. 2012;39(4):372–83. doi: 10.1002/uog.11080. [DOI] [PubMed] [Google Scholar]
- 5.Lien KC, Mooney B, DeLancey JO, Ashton-Miller JA. Levator ani muscle stretch induced by simulated vaginal birth. Obstet Gynecol. 2004;103(1):31–40. doi: 10.1097/01.AOG.0000109207.22354.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lawson JO. Pelvic anatomy. I. Pelvic floor muscles. Ann R Coll Surg Engl. 1974;54(5):244–52. [PMC free article] [PubMed] [Google Scholar]
- 7.Federative Committee on Anatomical Terminology . Stuttgart. Thieme; New York: 1998. Terminologia anatomica: international anatomical terminology. [Google Scholar]
- 8.Dietz HP, Gillespie AV, Phadke P. Avulsion of the pubovisceral muscle associated with large vaginal tear after normal vaginal delivery at term. Aust N Z J Obstet Gynaecol. 2007;47(4):341–4. doi: 10.1111/j.1479-828X.2007.00748.x. [DOI] [PubMed] [Google Scholar]
- 9.Margulies RU, Huebner M, DeLancey JO. Origin and insertion points involved in levator ani muscle defects. Am J Obstet Gynecol. 2007;196(3):251, e1–5. doi: 10.1016/j.ajog.2006.10.894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeLancey JO, Sorensen HC, Lewicky-Gaupp C, Smith TM. Comparison of the puborectal muscle on MRI in women with POP and levator ani defects with those with normal support and no defect. Int Urogynecol J. 2012;23(1):73–7. doi: 10.1007/s00192-011-1527-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Albright TS, Gehrich AP, Davis GD, Sabi FL, Buller JL. Arcus tendineus fascia pelvis: a further understanding. Am J Obstet Gynecol. 2005;193(3 Pt 1):677–81. doi: 10.1016/j.ajog.2005.02.129. [DOI] [PubMed] [Google Scholar]
- 12.Grigorescu B, Lazarou G, Olson T, Downie S, Powers K, Greston W, et al. Innervation of the levator ani muscles: description of the nerve branches to the pubococcygeus, iliococcygeus, and puborectalis muscles. Int Urogynecol J. 2008;19(1):107–16. doi: 10.1007/s00192-007-0395-8. [DOI] [PubMed] [Google Scholar]
- 13.Anson BJ. An atlas of human anatomy. Saunders; Philadelphia: 1963. [Google Scholar]
- 14.Benjamin M, Kumai T, Milz S, Boszczyk BM, Boszczyk AA, Ralphs JR. The skeletal attachment of tendons--tendon “entheses”. Comp Biochem Physiol A-Mol Integr Physiol. 2002;133(4):931–45. doi: 10.1016/s1095-6433(02)00138-1. [DOI] [PubMed] [Google Scholar]
- 15.Delancey JO. Fascial and muscular abnormalities in women with urethral hypermobility and anterior vaginal wall prolapse. Am J Obstet Gynecol. 2002;187(1):93–8. doi: 10.1067/mob.2002.125733. [DOI] [PubMed] [Google Scholar]
- 16.Huebner M, Margulies RU, DeLancey JO. Pelvic architectural distortion is associated with pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(6):863–7. doi: 10.1007/s00192-007-0546-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim J, DeLancey JO, Ashton-Miller JA. Why does the pubovisceral muscle fail at its enthesis, and not elsewhere, during the second stage of labor? A computational study.. 35th Annual Meeting of the American Society of Biomechanics; Long Beach, CA. 2011. [Google Scholar]
- 18.Larson KA, Luo J, Yousuf A, Ashton-Miller JA, Delancey JO. Measurement of the 3D geometry of the fascial arches in women with a unilateral levator defect and “architectural distortion”. Int Urogynecol J. 2012;23(1):57–63. doi: 10.1007/s00192-011-1528-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Averill W. Collapse of the Tacoma Narrows Bridge. Pacific Builder and Design. 1940;46:12. [Google Scholar]
- 20.Plaut RH. Snap loads and torsional oscillations of the original Tacoma Narrows Bridge. J Sound Vibr. 2008;309(3–5):613–36. [Google Scholar]
- 21.Liu Y, Birman V, Chen C, Thomopoulos S, Genin GM. Mechanisms of Bimaterial Attachment at the Interface of Tendon to Bone. J Eng Mater Technol. 2011;133(1) doi: 10.1115/1.4002641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith AR, Hosker GL, Warrell DW. The role of partial denervation of the pelvic floor in the aetiology of genitourinary prolapse and stress incontinence of urine. A neurophysiological study. Br J Obstet Gynaecol. 1989;96(1):24–8. doi: 10.1111/j.1471-0528.1989.tb01571.x. [DOI] [PubMed] [Google Scholar]
- 23.Kenton K, Mueller E, Brubaker L. Continent women have better urethral neuromuscular function than those with stress incontinence. Int Urogynecol J. 2011;22(12):1479–84. doi: 10.1007/s00192-011-1447-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim J, Ramanah R, DeLancey JO, Ashton-Miller JA. On the anatomy and histology of the pubovisceral muscle enthesis in women. Neurourol Urodyn. 2011;30(7):1366–70. doi: 10.1002/nau.21032. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The material can also be found in the following URL:http://vimeo.com/102735080.