Abstract
A 76-year-old woman with significant cardiovascular comorbidities was investigated under general surgery for weight loss and change in bowel habit. Endoscopic investigations revealed a large ulcer extending from the ileocaecal valve to the ascending colon. Histology of the biopsies from this site revealed chronic inflammation and reactive changes. However, considering the history and suspicious radiological and endoscopic findings, decision was made at a multidisciplinary meeting to offer laparoscopic right hemicolectomy. Owing to complications, the procedure was converted to an open surgery. Postoperatively, histology of resected bowel revealed chronic inflammation and no evidence of malignancy. In light of an 8-year history of nicorandil therapy, the histological changes were thought to represent nicorandil-induced colonic ulceration.
Background
Colonic ulceration is a rarely reported complication of nicorandil therapy. Few case reports in the literature have attempted to explore this link further. The purpose of this case report is to raise awareness of this under-reported complication, particularly as evidence shows that cessation of nicorandil therapy leads to mucosal healing and subsequently reversal of symptoms. As evident in the literature and this case report, patients tend to present with symptoms that would raise suspicions for malignancy. Therefore, it is important to consider this important differential to avoid potentially invasive investigations and treatments.
Case presentation
A 76-year-old woman presented in August 2012 with a history of unexplained significant weight loss and change in bowel habit. She was subsequently seen in clinic under general surgery for urgent investigations of her presenting symptoms. Her extensive medical history is as follows: paroxysmal atrial fibrillation, ischaemic heart disease and coronary artery bypass graft procedure 20 years ago with subsequent congestive cardiac failure, osteoporosis, chronic kidney disease and hypothyroidism. As an adjunct to treating angina, the patient was started on nicorandil in 2004 at an initial dose of 10 mg twice daily and was gradually increased to a dose of 30 mg twice daily following cardiology review in 2005. Her other regular medications included: glyceryl trinitrate, latanoprost, isosorbide mononitrate, simvastatin, co-dydramol, aspirin, candesartan, temazepam, gabapentin, calcichew, levothyroxine and folic acid.
Investigations
Prior to her clinic appointment, she had an urgent gastroscopy that showed widespread intramucosal haemorrhages. From clinic, an initial flexible sigmoidoscopy and later a colonoscopy was organised along with a CT scan of her chest, abdomen and pelvis. While the sigmoidoscopy revealed two sessile polyps in the sigmoid colon, a later colonoscopy revealed a suspicious large ulcer (figure 1) extending from the ileocaecal valve to distal ascending colon with adenomatous edges and a firm base: appearances thought to be in keeping with probable ulcerative tumour.
Figure 1.
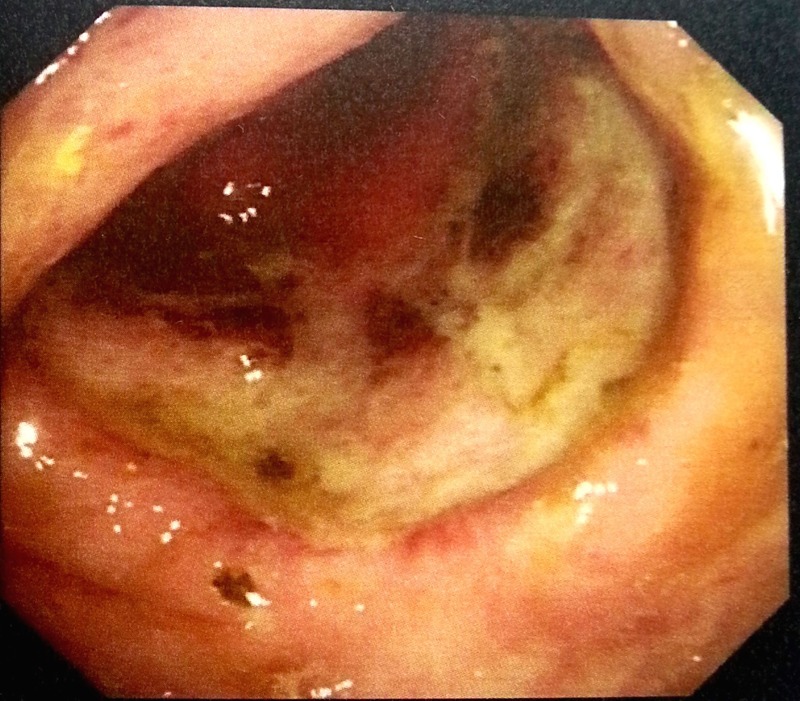
Colonoscopy showing large ulcer extending from ileocaecal valve to distal ascending colon.
The histology of biopsies revealed chronic inflammation with ulceration, ulcer slough and reactive changes. A rebiopsy was recommended although histology did not suggest convincing evidence of dysplasia or malignancy.
Finally, a suboptimal non-contrast staging CT was carried out due to chronic renal failure. This scan revealed an area of thickening around the caecum with stranding of pericolic fat and small lymph nodes. When weighed up with the suspicious endoscopic findings and the history of presenting problem, these findings were thought to likely represent malignancy. No distant metastatic disease was identified.
Differential diagnosis
As we know, the differential diagnoses for an ulcerating colonic lesion include inflammatory bowel disease, infective causes like tuberculosis and amoebiasis and neoplasia—particularly in cases of solitary ulcers. In this case, there was no histological evidence to support the former two causes. A colorectal multidisciplinary team discussion took place and neoplasia was deemed to be the most likely cause in view of the history, suspicious colonoscopic appearances which were in line with non-contrast CT findings in the same region.
Treatment
Following on from a multidisciplinary team decision, the patient was then offered an elective laparoscopic right hemicolectomy in October 2012. As the patient developed fast atrial fibrillation during surgery, the procedure was converted to open hemicolectomy with primary anastomosis. A small lesion in the proximal ascending colon was seen with localised perforation and was tethered to the sidewall. Postoperatively, the patient was admitted to high dependency unit as a planned admission prior to surgery. She was stepped down to ward level care after 1 day where she developed localised cellulitis of her operative wound and loose bowels following start of antibiotics. Following a cardiology review for intraoperative fast atrial fibrillation and with microbiology advice, the patient was discharged home 20 days postoperatively for general surgery follow-up and community follow-up with the tissue viability team for a persistent wound infection.
Outcome and follow-up
Macroscopically, histology of the resected specimen showed a 35 mm×30 mm caecal ulcer. Microscopically, there was full thickness ulceration with acute inflammatory cells and necrotic debris. Beneath this necrosis was moderate to dense lymphoplasmacytic infiltrate which extends through the underlying thinned muscularis propria into the pericolic fatty tissue. The submucosa, muscularis propria and serosa in this area were congested. A total of 12 reactive lymph nodes were retrieved from the specimen. The histological appearances were in keeping with long-standing gastrointestinal ulceration and no evidence of malignancy or dysplasia was found.
After discussion at a colorectal multidisciplinary meeting, the above findings were thought to represent nicorandil-induced colonic ulceration in view of the patient's background of ischaemic heart disease and long history of nicorandil therapy (8 years). The patient has been stable following cessation of nicorandil and has recovered well following her surgery. She is under routine follow-up with the general surgical team.
Discussion
Nicorandil acts as a potassium channel activator with nitrate-like effects. It has a dual mechanism of relaxation of both arteriolar and venous smooth muscle, thus reducing cardiac preload and afterload while increasing coronary blood flow.1 Since its efficacy was proven in a landmark IONA trial, nicorandil has been used as an adjunct in treatment of ischaemic heart disease.1 Oral, anal, genital and ocular ulceration have been reported with nicorandil use.2–5 The pathophysiology may involve a vascular steal phenomenon or a direct toxic effect of nicorandil.3 Colonic ulceration is reported relatively rarely. Initial case reports postulated a link between nicorandil use and extensive colonic ulceration (figure 2).6 7
Figure 2.
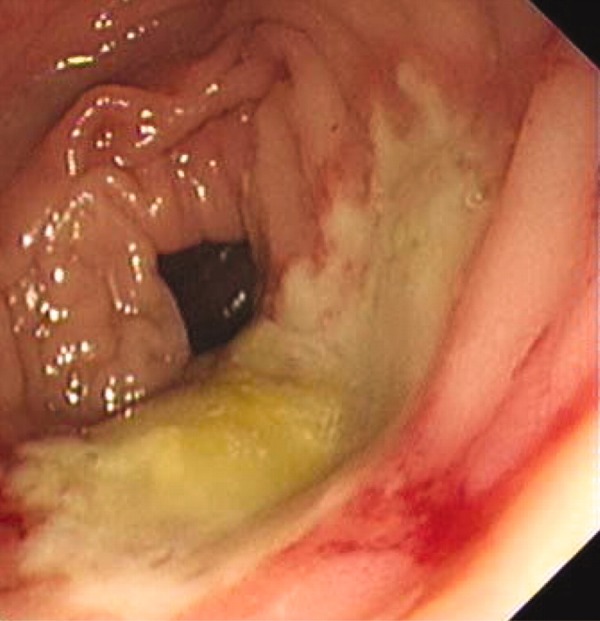
Brown and Warfare presenting a case of nicorandil-induced extensive ulceration of transverse and right colon revealed by colonoscopy6 (adapted with permission of BMJ Case Reports).
Recently, two case series have examined this link further. Titi et al8 report nicorandil-induced colonic ulceration in four patients. All patients presented with similar symptoms: abdominal pain, diarrhoea with or without bleeding. Three patients also had associated stomatitis and anal ulceration. Macroscopically, three patients had deep ulcers with a characteristic punched-out appearance and histology revealed non-specific chronic inflammation. Variation was noted in nicorandil doses that lead to ulceration and also with time to onset of symptoms from starting nicorandil. Titi et al8 observed a large variation of 6 weeks to 3 years for onset of symptoms from start of nicorandil. A similar pattern has also been described in another case series.9 Delay between starting nicorandil and presentation with significant symptoms in our case report was 8 years. Evidence from the aforementioned case reports imply that the threshold dose of nicorandil to trigger ulceration depends on the individual––particularly on the background of impaired perfusion due to deteriorating cardiac function in patients with significant cardiovascular comorbidities.8 9 Stronger evidence reviewing the link between individual risk factors and nicorandil dose to cause colonic ulceration is required to accurately diagnose and guide management of this condition.
Lee et al describe a similar history to our case: a 74-year-old woman who presents with iron deficiency anaemia and weight loss. Endoscopy revealed a large ulcer involving most of the caecal circumference with histology suggesting non-specific inflammation. CT of the abdomen showed a thickening of the affected bowel and reactive lymph nodes. Although malignancy was initially suspected, multidisciplinary team discussion raised the possibility of nicorandil-related ulceration. As a result of stopping the nicorandil, the lady recovered from her symptoms and a repeat colonoscopy showed healing of the ulcer.9
From the literature, nicorandil-induced colonic ulcers tend to be deep, can be solitary or multiple and can present with or without concomitant anal ulceration.8 9 There is a theoretical risk of perforation associated with deep ulcers, and studies have proposed a link between nicorandil use and ileal perforation. Nicorandil may also increase risk of fistulation in the presence of diverticular disease.10 11
Nicorandil-induced ulceration is a diagnosis of exclusion. All case studies so far have demonstrated reversal of inflammation and symptoms with cessation of nicorandil use. A wide variation in duration to resolution of symptoms has been reported: 3 weeks to 8 months.6 8 9 12
Careful co-ordination with the cardiology team is needed as many of these patients may have ischaemic heart disease refractory to first-line treatments. However, if recognised, it can prevent serious complications such as risk of perforation and prevent unnecessary invasive procedures such as bowel resection.
Learning points.
Nicorandil-induced colonic ulceration is an unrecognised complication. It can present with symptoms similar to inflammatory bowel disease or malignancy and therefore should be considered as a differential diagnosis.
With specialist cardiology input, cessation of nicorandil leads to mucosal healing and reversal of symptoms.
Early recognition prevents unnecessary investigations, perforation risk and, particularly considering this case, can avoid unnecessary surgery.
Acknowledgments
The author would like to thank Mr Sajal Rai (Consultant General Surgeon) for his continued supervision and support.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.IONA Study Group. Effect of nicorandil on coronary events in patients with stable angina: the Impact Of Nicorandil in Angina (IONA) randomised trial. Lancet 2002;359:1269–75. 10.1016/S0140-6736(02)08265-X [DOI] [PubMed] [Google Scholar]
- 2.Katory M, Davies B, Kelty C et al. Nicorandil and idiopathic anal ulceration. Dis Colon Rectum 2005;48:1442–6. 10.1007/s10350-005-0027-7 [DOI] [PubMed] [Google Scholar]
- 3.Watson A, Al-Ozairi O, Fraser A et al. Nicorandil associated anal ulceration. Lancet 2002;360:546–7. 10.1016/S0140-6736(02)09710-6 [DOI] [PubMed] [Google Scholar]
- 4.Trechot F, Batta B, Petitpain N et al. A case of nicorandil-induced unilateral corneal ulceration. Int Wound J 2014;11:238–9. 10.1111/iwj.12081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yap T, Philippou P, Perry M et al. Nicorandil-induced penile ulcerations: a case series. BJU Int 2011;107:268–71. 10.1111/j.1464-410X.2010.09463.x [DOI] [PubMed] [Google Scholar]
- 6.Brown R, Lee A, Welfare M. Nicorandil-induced colonic ulceration. BMJ Case Rep 2009;2009:bcr2007134379 10.1136/bcr.2007.134379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Egred M, Andron M, Morrison WL. Nicorandil may be associated with gastrointestinal ulceration. BMJ 2006;332:889 10.1136/bmj.332.7546.889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Titi MA, Seow C, Molloy RG. Nicorandil-induced colonic ulceration: a new cause of colonic ulceration. Report of four cases. Dis Colon Rectum 2008;51:1570–3. 10.1007/s10350-008-9218-3 [DOI] [PubMed] [Google Scholar]
- 9.Lee BC, Allen PB, Caddy GR et al. Nicorandil associated colonic ulceration: case series of an increasingly recognized complication. Dig Dis Sci 2011;56:2404–8. 10.1007/s10620-011-1634-x [DOI] [PubMed] [Google Scholar]
- 10.McDaid J, Reichl C, Hamzah I et al. Diverticular fistulation is associated with nicorandil usage. Ann R Coll Surg Engl 2010;92:463–5. 10.1308/003588410X12699663904673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.King PM, Suttie SA, Jansen JO et al. Perforation of the terminal ileum: a possible complication of nicorandil therapy. Surgeon 2004;2:56–7. 10.1016/S1479-666X(04)80140-9 [DOI] [PubMed] [Google Scholar]
- 12.Thrumurthy SG, Date RS, Owa OS et al. Nicorandil-induced colonic ulceration: an unusually delayed presentation of a rare complication. Int J Colorectal Dis 2011;26:1631–2. 10.1007/s00384-011-1184-x [DOI] [PubMed] [Google Scholar]


