Abstract
Congenitally missing teeth (CMT), or as usually called hypodontia, is a highly prevalent and costly dental anomaly. Besides an unfavorable appearance, patients with missing teeth may suffer from malocclusion, periodontal damage, insufficient alveolar bone growth, reduced chewing ability, inarticulate pronunciation and other problems. Treatment might be usually expensive and multidisciplinary. This highly frequent and yet expensive anomaly is of interest to numerous clinical, basic science and public health fields such as orthodontics, pediatric dentistry, prosthodontics, periodontics, maxillofacial surgery, anatomy, anthropology and even the insurance industry. This essay reviews the findings on the etiology, prevalence, risk factors, occurrence patterns, skeletal changes and treatments of congenitally missing teeth. It seems that CMT usually appears in females and in the permanent dentition. It is not conclusive whether it tends to occur more in the maxilla or mandible and also in the anterior versus posterior segments. It can accompany various complications and should be attended by expert teams as soon as possible.
Keywords: Complications, etiology, hypodontia, prevalence, risk factors, tooth abnormalities, treatment
INTRODUCTION
Oral health plays a crucial role in public health. Dental treatments are rather expensive health services and the combination of different modalities such as orthodontic, prosthodontic and surgical treatments can put a heavy burden on the average family's health budget. Some frequent dental anomalies need quite expensive treatments. One of them is congenitally missing teeth (CMT), congenital absence of teeth, congenital dental aplasia, or dental agenesis. It is one of the most common dental anomalies.[1,2,3,4,5] It might negatively affect both the esthetics and function.[3,6,7,8] Esthetics itself is an important factor and its problems might affect patients’ self-esteem, communication behavior, professional performance and quality of life.[9,10,11] Patients with missing permanent teeth may suffer from complications such as malocclusion (which itself can lead to mastication problems),[12] periodontal damage, lack of alveolar bone growth, reduced chewing ability, inarticulate pronunciation, changes in skeletal relationships and an unfavorable appearance,[9,12,13,14,15,16] most of which need rather costly and challenging multidisciplinary treatments.[9,17,18,19]
ETIOLOGY OF DENTAL AGENESIS
CMT is a result of disturbances during the early stages of development[15] and is suggested as a mild dysplastic expression of the ectoderm.[20,21,22,23] When a primary tooth is congenitally absent, its permanent counterpart might also be missing.[22,24] Genetics plays a crucial role in congenital dental aplasia,[4] as confirmed by studies on monozygotic twins.[22,25,26,27] Interestingly, the pattern of CMT can differ between monozygotic twins, possibly pointing to additional underlying mechanisms,[25] such as epigenetic factors which might be implied by simultaneous occurrence of two anomalies.[4] This multifactorial etiology can include environmental factors as well, since a combination of environmental and genetic factors might contribute to the occurrence of dental agenesis.[4,8,14,19,28] These include infection, trauma and drugs, as well as genes associated with about 120 syndromes,[2,3,6,8,19,22,29,30,31,32,33,34,35] such as cleft lip, cleft palate or both,[36] ectodermal dysplasia[9,27,37] and Down, Rieger and Book syndromes.[9,22] A possible general explanation is that except in hereditary cases, CMT has greater occurrence likelihood when the dental germ is developing after the surrounding tissues have closed the space needed for the tooth development.[3,38] Other investigations demonstrated that delays in tooth development and reductions in tooth size correlate with advanced CMT.[3,39,40,41] Both of these might accord with the terminal reduction theory.[3,42] Furthermore, it is suggested that anterior agenesis may depend more on genes while posterior missing might be sporadic.[23]
The most supported etiological theory suggests a polygenic mode of inheritance, with epistatic genes and environmental factors exerting some influence on the phenotypic expression of the genes involved,[29,43,44] which this can disturb the tooth germ during the initial stages of formation, i.e., the initiation and proliferation.[22] The exact genetic mechanism is not known.[3,7,9,21] Separate mechanisms might as well account for missing of each tooth.[3]
CMT can form in isolation as well. Isolated cases are more common than syndromic type[17] and might be familiar or sporadic.[22] The isolated condition can follow autosomal dominant,[45,46,47] autosomal recessive[48,49] or X-linked[50] patterns of inheritance, with remarkable variation in both penetrance and expressivity.[17,20,22,51] Different subphenotypes of dental agenesis might be probably caused by various genes.[52,53,54,55,56,57] Mutations in genes such as MSX, PAX9 or TGFA might cause CMT in different racial groups.[9,14,30,31,47,56,58,59,60] Among the homeobox genes, MSX1 and MSX2 play an important role in mediating direct epithelial-mesenchymal interactions during craniofacial bone and tooth development.[14,17,61] The autosomal-dominant CMT might be correlated with a mutation in the MSX1 and PAX9 genes.[9,17,31,47,58,59,62] MSX1 mutations affect predominantly the second premolars and third molars, sometimes in combination with other types of teeth like the first molars.[17] On the other hand, in more common cases of incisor-premolar type of dental agenesis, MSX1 is less likely to play a role as the causative locus for this type of CMT.[17,53] In addition, PAX9 and TGFA are associated with congenital missing by interacting between MSX1 and PAX9.[14,56] A recent study showed a novel mutation in MSX1 gene responsible for CMT of the second premolars and third molars only.[63]
DIAGNOSIS AND CLASSIFICATION OF CONGENITALLY MISSING TEETH
Dental aplasia is classified based on the number of missing teeth.[22,35,64] Mild and moderate cases have usually less than three and less than six teeth missing, respectively.[35] The definitions of hypodontia, oligodontia and anodontia differ in the number of missing teeth, on which there is no clear agreement.[3,15,22,31,64] This can account for some of the variation observed.[64] An ideal CMT diagnosis requires radiographic, clinical and dental cast examinations,[65] but in any case, radiographic examination is a must.[3,8,66] Since radiographic evidence of tooth germs needs certain level of calcification to appear, inclusion of too young individuals might enter insufficiently calcified tooth buds into the sample, which can be mistakenly diagnosed as missing teeth on the radiograph.[64] It can be of a greater concern for the mandibular premolars[3,7,34,67,68] and boys, both with more delayed eruption odds.[8,65,69,70,71] Therefore scientists should take into consideration the late development of the lower second premolars in boys; and should not include subjects without the canines and premolars neither erupting nor fully erupted,[65] or at least under 6.[3] Some authors have recommended the exclusion of children younger than 9 or 10 or even 12 years old.[8,34,60,64,69,70,71,72] The third molar bud calcification begins at the age of about 7.5 only in very few people; however, the average age for the initiation of its calcification is about the age 9.5.[73,74] Therefore, by including patients younger than 9, or even 11 (as the 85th percentile for initiation of calcification),[74] researchers might considerably overestimate the third molar missing rate. This might explain the very high prevalence reported by some studies (34.8%).[60] It should be noted that even the initiation of calcification does not guarantee well detection in radiographs; and older ages might be needed for some cases, in order to make sure calcification has reached a detectable minimum.
THE PREVALENCE OF DENTAL AGENESIS
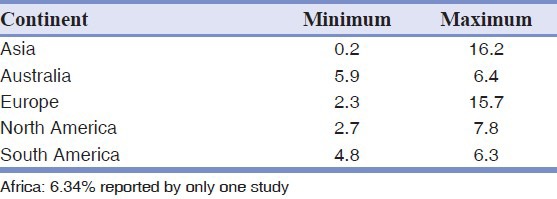
In the primary dentition, the CMT is not frequent, being between 0.1% and 2.4%.[30,33,35,75,76] However, primary dental aplasia is usually followed by permanent tooth missing.[8,19,34] The prevalence of CMT in the permanent dentition excluding the third molars ranges between 0.15% and 16.2% [Table 1] in studies varying in size from about 200 subjects to about +100,000 ones.[1,3,4,5,7,8,9,14,15,17,22,23,29,32,34,38,42,51,57,60,64,65,66,67,68,69,70,71,72,75,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156] Japanese people showed the highest rates both in deciduous and permanent dentitions.[17,30,35,64] The CMT prevalence was found to differ between continents and races, but unlikely over time.[34] The CMT prevalence in third molars has been reported over a rather broad range, between 5% and 37%.[22] For example, Ghaznawi et al.[134] reported 5.5% of wisdom tooth missing in Saudi Arabia, while Varela et al.[29] observed that 11.5% of a population from Spain had missing of third molars. Other rates might be much greater. For instance, Afify and Zawawi[155] and Silva Meza[141] reported 24% third molar absence rates in Saudi Arabia and Mexicans, respectively. Sheikhi et al.[60] have reported 34.8% missing prevalence of Iranians’ third molars. Australian aborigines and perhaps African Blacks might have a low chance of dental agenesis.[8,19] Indians have shown very small prevalence rates, as two out of three studies in India had rates less than 1% and the other one had about 4% prevalence.[77,151,152] The different rates reported could be explained by different measurement approaches or other methodologies[2,3,8,34,70] and ethnic backgrounds.[4,8,15,19,33,34,115] In contrast, X-ray is a carcinogen factor and cannot be prescribed without any treatment needs.[1,8,64,157,158,159] Thus, researchers need to use previously taken radiographic images. In very rare cases, such images have been taken from randomly selected subjects (epidemiological samples such as patients attending mandatory public health protocols that oblige periodic dental radiographs be taken from healthy people).[148] However, in almost all recent assessments, dental radiographs have been taken from dental patients. It is possible, however, that dental patients include more cases of dental anomalies which might bias the result.[64]
Table 1.
The minimum and maximum prevalence of congenitally missing teeth/hypodontia in different continents
The CMT prevalence may be increasing, perhaps due to evolutionary changes,[2,8,15,70,160,161,162] or because of increases in the diagnosis,[2,8,163] not necessarily the evolution.[65,163] Nevertheless, some authors suggest that it might be evolutionary[1,152,161] to adapt with the gradually shrinking size of the jaws.[1,152,161] Some researchers state that evolution needs much more time to happen;[163] whereas some account for the rapid environmental changes as the causes of CMT.[160,163] However meta-analyses have not confirmed such an increase in the previous decades.[34,64,163]
THE ASSOCIATION OF CMT WITH OTHER DENTAL ANOMALIES
CMT can accompany other conditions such as delayed eruption of other teeth, reductions in coronal or radical dimensions, retained primary teeth, ectopic canine eruption and abnormal dental morphologies such as taurodontism and peg-shaped maxillary lateral incisors.[2,3,4,8,14,20,31,32,33] While some researchers have reported that the size of teeth and the width of the dental arch are not related to dental agenesis,[68] some others reported conflicting results indicating that CMT is associated with dental anomalies such as microdontia and decreases in the size of the incisors and canines as well as conical or tapered teeth such as peg lateral.[14,28,31,164,165] However, some investigators did not find a link between tooth agenesis and microdontia but with peg laterals.[14] They concluded that CMT was not associated with changes in the overall tooth size, while changes in tooth morphology especially in the maxillary lateral incisors might still be possible.[14] This might be in line with other studies finding correlations between severe CMT and taurodontism[57,166] especially in boys,[166] or between CMT and taurodontism;[31] It might also be in agreement with studies that could not associate CMT with microdontia of contralateral teeth.[57] Some authors found links between CMT with size anomalies and taurodontism.[31] Therefore, the literature is not conclusive. Both CMT and taurodontism seem to be a part of syndromes characterized by decreased mitotic cellular activity which might also affect dental germ development.[4] On the other hand, some other studies found clear associations between both mild and severe CMT and reduced tooth size,[21,32,160,165,167] especially in the upper laterals (in the mesiodistal dimension) and the lower canines (the labiolingual dimension).[165] The latter agrees with the synergism and allelism of major genes possibly affecting CMT.[21]
ASSOCIATIONS WITH SKELETAL CHANGES IN THE HORIZONTAL PLANE
The results pertaining to skeletal changes are controversial. Some authors did not find a significant correlation between malocclusions and CMT prevalence, although suggested a link between CMT and Class II division 2.[65] While according to others, there could be significant links. CMT might accompany reduced intercanine and intermolar widths.[147] Anterior missing can accompany retrognathic maxillae, prognathic mandibles and smaller lengths of posterior cranial base.[16] It also might be more common in the skeletal Class III malocclusion due to smaller or retrognathic maxillae.[14,22,30,71,168,169] In some studies, Class III was associated merely with severe CMT.[169,170] CMT might be also significantly less frequent in Class II cases,[147] although a study reported non-significant results for this decrease (possibly due to small sample of Class II cases).[65] On the contrary, Cua-Benward et al.[128] found the greatest prevalence of CMT in Class II patients and observed a significant number of missing maxillary teeth in Class III patients. However, it might depend on the most common missing teeth, as it appears that the missing tooth affects its own jaw. A study by Hirukawa et al.[135] concluded that Class III might be the most common malocclusion observed among the subjects who had missing teeth only in the maxilla, while when teeth were missing only in the mandible, it was frequently associated with Class II malocclusion.[135] Perhaps the tendency towards a Class III relationship is caused by decreased maxillary and mandibular angular prognathism and the effect might be greater on the maxilla than on the mandible.[170]
ASSOCIATIONS WITH VERTICAL SKELETAL CHANGES
According to some studies, dental aplasia is not correlated with the vertical relationship of the jaws.[14,147] However some investigators have found significant associations between the CMT ocurrence with reduced anterior lower facial height[16,30,168,171] and increased overbite,[22] which intensifies by increasing the severity of CMT,[169,170] or less severe deep bite in CMT patients[135] and decreased maxillary-to-mandibular-planes angle, which was clinically relevant only in severe CMT.[170] Furthermore anterior CMT might have a significant effect on the vertical skeletal relationships with increasing severity of CMT.[170] It also might contribute to a more acute mandibular angle and flatter chin.[16]
SEX DIMORPHISM
Gender might act as a dental agenesis risk factor.[8,33,34] Women are usually more affected[7,15,22,34,67,141,160] and the male-to-female ratio is about 2:3.[8,29,33,34,172] Some authors studied the teeth individually and found significant gender dimorphism only for certain teeth,[70,104,141] such as the upper incisors and upper first premolars, all on the right side only.[70] Of these teeth, only the missing of the upper right central incisor was more prevalent in males and the other ones were more prevalent in females. Silva Meza[141] have reported significant intersex differences only for the lateral incisors and third molars (without indicating the predominant gender). Eidelman et al.[104] reported significant differences only for the lateral incisor missing cases, being more common in females. Some studies found a non-significant predominance of CMT in males.[29,70,148,151] A very large study on six districts of Turkey showed that in five regions, females had a significantly higher CMT prevalence, while in one of them males had a significantly greater prevalence.[15] Male-to-female ratios were previously summarized as 1:1.37 and 1:1.4 in literature reviews.[8,33,34] The higher rates observed in females might be associated with biological differences such as smaller jaws which might trigger environmental factors. This might be confirmed by the suggestion that teeth might be absent also when the development of dental germs is delayed and thus the needed space has been compromised by the surrounding tissues.[78] As well, another factor can contribute to the higher rates of CMT in females: The existence of a probable higher orthodontic treatment need in females with the tooth missing due to their higher concern regarding the appearance[8] and the higher value that society gives to esthetics in females.[29] Nevertheless, the latter might not be the case, since most of studies on schoolchildren as well showed a higher rate in females. Moreover, some other studies did not find such a difference in orthodontic patients,[8,14] or even reported higher prevalence rates in male orthodontic patients[69,70] and male patients of the public health services.[148] Furthermore, since males tend to have lower rates of CMT, studies enrolling more males, might show lower total CMT prevalence rates.[64]
A possible reason for the controversies is that different teeth might vary in terms of sex dimorphism. Küchler et al.[57] showed that the M:F ratio of incisor agenesis was 1.4:1, while in the case of the upper lateral incisors, this ratio was 2:1 and for the lower incisors, the M:F ratio was 1:1. On the other hand, the M:F ratio of premolar missing was 0.5:1 (0.3:1 for the upper second premolar ratio and 0.5:1 for the lower second premolar ratio).[57] Thus a combination of various M:F ratios for different teeth can disallow to easily identify significant differences in the whole dentition. Based on the differences in sex ratios depending on the specific tooth types affected, Küchler et al.[57] suggested a continuous variable, “liability,” with a threshold value, beyond which individuals might be affected. This system is called multifactorial because both genetics and environmental factors determine liability.[57] Based on this concept, they concluded two possibilities: Either the same genetic model might have different thresholds for males and females, or each gender is influenced by an independent genetic model, each having its own threshold.[57] Another factor contributing to the controversy might be the ethnicity.
There is no consistent finding as to which sex is predominant in regard to having more missing teeth per child.[4,5,7,8,15,51,67,68,69,72,81,93,94,95,99,100,106,109,110,113,173] In one research, each male had an average of missing teeth per person higher than that of each female (2.32 compared to 1.40).[8] However, in another one, the average numbers of missing per person dentition were almost similar for both genders with a slight increase in boys (2.5 for boys, 2.4 for girls)[5] and in some others, girls had a higher chance for having more missing teeth per person.[15,23,68,109] From information reported in a study on Swedish schoolchildren,[4] these ratios were calculated and showed 1.46 missing teeth in each boy in comparison to 1.74/girl. Evaluation of six regions of Turkey showed that in five of them, females had a significantly greater chance of having more missing teeth per individual and in one of them, males had a greater chance of having more missing teeth in each person.[15] Some other studies as well showed that females might have oligodontia much more likely than males might do.[144,147,148] However, another study found the opposite[71] and another one found similarity between the two.[9]
THE MOST FREQUENTLY MISSING TEETH
Clinicians could be assisted by knowing the CMT risk factors and its pattern of occurrence.[6,8,141] As a general rule, if only a few teeth are missing, the absent tooth would be the most distal tooth of any given type.[8,22,70,162,174] This applies to the maxillary laterals and the mandibular second premolars. On the other hand, it is suggested that the permanent maxillary first premolars, canines and first molars, which are likely to be more stable, have a relatively greater rate of CMT in children with five or more teeth missing.[5,146]
UNILATERAL VERSUS BILATERAL DENTAL AGENESIS
Most authors observed predominance of bilateral CMT to extents such as about as twice as unilateral missing[1,4,5,8,15,51,67,69,81,95,99,110,112,141,144,161] or even as trice as unilateral missing.[1,3,141] Even Endo et al.[5] have reported that in 89% of patients, the teeth were bilaterally missing. However, few studies failed to find a significant difference[14,100,112,115,140] or reported non-significant[60] or significant predominance of unilateral missing.[60] In studies on Koreans and Iranians, these were almost similar.[65,146] Nevertheless, a careful examination of presented information by Kim[65] implied that that article has compared “patients” with bilateral or unilateral missing teeth, not the number of missing teeth. This author further evaluated the values and it was implied that many patients had more than only a pair of bilaterally missing teeth and that if the number of teeth was to be compared, bilateral missing would be as double as unilateral missing in their study. In another Korean study, 70.9% of sample had unilateral missing.[14] On this subject, a review shows that overall, unilateral missing is more common, but bilateral missing is seen mostly in the maxillary lateral incisors.[34] Furthermore, it is suggested that unilateral agenesis might be more common in the case of the upper and lower second premolars, whereas, bilateral missing might be more common in the maxillary laterals.[15] Except for the first molars in both jaws and the maxillary centrals, bilateral agenesis was significantly more common than unilateral aplasia.[15]
WHICH TEETH ARE MOSTLY SYMMETRICALLY MISSING?
This question is not assessed thoroughly. Medina[172] stated that while symmetrical dental missing affects the maxilla, the mandible shows mostly unilateral agenesis. According to some other reports, the most common symmetric missing tooth could be the mandibular second premolar agenesis, followed by the absence of the maxillary second premolar or maxillary lateral incisor.[5,51,85,101,161] According to a meta-analysis, the maxillary lateral incisor might be the most common bilateral missing tooth.[34,60] Endo et al.[5] found a similar pattern in children other than those with two missing teeth. However, in children with two missing teeth, the mandibular lateral incisor agenesis had a higher prevalence rate.[5]
THE RIGHT VERSUS THE LEFT SIDES
No studies so far have found a significant difference between missing teeth located in the left and right sides.[5,8,22,57,60,70,78,130,141,142,147,175,176] For example, Sisman et al.[70] did not find any significant right-left differences for the whole CMT prevalence and for any of teeth assessed individually. Even a study on more than 100,000 dental patients showed that the number of missing teeth on the left and right sides was almost identical (1574 vs. 1573).[15] According to Fekonja,[22] the missing teeth were more commonly absent on the right side (26 teeth, 54.2%) than on the left side (22, 45.8%). However, their comparison was not statistically substantiated. Statistical comparison was carried out by this author using the Chi-square goodness-of-fit test, which did not detect a significant difference (P = 0.564).
THE OCCURRENCE OF CMT ACROSS THE ANTERIOR/POSTERIOR REGIONS
Few studies have evaluated the difference between CMT rates in the anterior and posterior segments[5,8,69,147] and this should be considered in future studies. Most studies showed higher prevalence in the anterior segment[8,71,147] and the few remaining researches found no significant differences.[5] Some investigators suggest that in mild cases of CMT, the anterior segment might be more involved while the posterior segment might be predominant in severe cases.[5] Many studies did not calculate or report the anterior versus posterior missing and many of them did not present raw data.[3,4,5,8,9,22,31,57,66,70,71,144,146,148,149,150,176,177] Their raw data were recovered from their tables, graphs and/or texts. The anterior/posterior occurrence was calculated and statistically analyzed using the Chi-square goodness-of-fit test, after making sure that the third molars were excluded. Some of these differences analyzed by this author were statistically significant (P < 0.01,[70] P < 0.01,[177] P < 0.01,[148] P < 0.01,[71] P < 0.01,[150] P < 0.01,[9] P = 0.000,[8] P = 0.003,[176] P = 0.000[4]) and some were non-significant (P > 0.05).[22,31,57,66,144,146,149] Galluccio and Pilotto[23] investigated the family trees of CMT patients. They identified two groups: Nine families exhibited dental missing seemingly as a function of autosomal dominant genetic transmission. In these families, CMT mainly involved the maxillary lateral incisors. Since other dental anomalies were present, CMT seemed one of the manifestations of an anomaly of the dental lamina. Six families had CMT as a sporadic condition. In this group, CMT was seen only in orthodontic patients and it most often involved the second molars and second premolars.[23]
THE OCCURRENCE OF CMT ACROSS THE ARCHES
The results as which arch is predominant are not conclusive.[5,8,34] Some investigators found that congenital tooth agenesis was more common in the maxilla,[8,15,22,70,147] and some others reported a higher rate of missing teeth in the mandible.[4,14,65,79,161] The following studies did not analyze/report maxillary/mandibular missing. However, their data were recovered and analyzed by this author. Some studies showed significant differences (P = 0.09,[66] P = 0.063,[146] P = 0.054,[31] which were only marginally significant, P = 0.000,[71] P = 0.000,[144] P = 0.003,[65] P = 0.000,[4] P = 0.000[70]) and some did not demonstrate significant or marginally significant differences (P > 0.1).[66,148,149,150,176]
TREATMENT OF CONGENITALLY MISSING TEETH
CMT has direct clinical implications. The treatment is comprehensive and expensive,[9] costing in some countries from about $3000 to $15,000/patient for minor prosthodontic interventions like a fixed partial denture in mild cases with only one or two missing permanent teeth, to $60,000 for comprehensive interdisciplinary treatments.[9,18] The treatment would be usually difficult.[137] It might represent an interdisciplinary challenge for specialists in oral and maxillofacial surgery, operative dentistry, pediatric dentistry, orthodontics and prosthodontics.[9,22,65,171,178,179,180,181] General or pediatric dentists can facilitate multidisciplinary treatments by diagnosing congenital absence of primary teeth and then through early referrals of patients; as the absence of primary teeth highly associates with missing of permanent successors.[8,19,34] They might also ensure the retention of reduced number of teeth,[8,19] in cases such as palatal impaction of the maxillary canines caused by the missing laterals, in which early extraction of deciduous canines might guide the eruption of the permanent ones into the correct position.[8,182] This necessitates the early evaluation of the number of missing teeth and the consideration of the CMT risk factors, as well as the size and number of teeth remaining in both arches in planning and managing treatment.[3,19,22] The type of malocclusion, severity of crowding and facial profile are of major concern in determining the final treatment plan.[22] Bone volume is related to facial esthetics such as smile, and should be considered in treatment planning as well.[65,183] During treatment planning, possible changes in the craniofacial morphology associated with CMT should be as well borne in mind.[14]
Another therapeutic challenge is the need to carry out treatment in the growing young patient.[9,179] While treatment should be initiated during adolescence,[9] interim treatment should begin in around 7-9 years of age before the affected children realize they are different from other children.[9,19,179]
The edentulous space can be either left open for prosthetic restoration, or closed by orthodontic means.[13,14,164] Other treatment modalities might include autotransplantation[14,184] or protraction[14,185] of the third molars, which are otherwise extracted, in order to substitute for the edentulous region or to increase the number of occluding teeth.[14] In prosthodontic treatments, transplantation is a better choice than implanting, since osseointegrated implants are contraindicated in the growing alveolar bone.[22] Successful autotransplantation of teeth ensures the stability of alveolar bone volume due to physiological stimulation of the periodontal ligament.[22] Implant treatment is postponed until the jaws have stopped growing in adolescence.[22,186,187,188] It is also possible to close the lateral space in crowded maxillae and recontour the canine into the lateral's shape. In an aligned maxillary arch, the distributed excess space can be localized and then restored using prosthetic approaches.[22] Absent lower incisors need esthetic and functional camouflage regarding the relationship between the maxillary and mandibular anterior teeth.[65] In crowded jaws, the missing premolar spaces can be used as one of the extraction spaces for arch alignment.[22] In uncrowded jaws with missing permanent premolars, the primary second molar might be left in situ. However, since, there is the risk of infra-occlusion or progressive root resorption, it might be eventually extracted and replaced with an implant or and autotransplanted tooth.[22] The treatment of severe cases is complex and should be performed in centers such as “Hypodontia Clinics”[65,189] with access to pediatric dentistry, orthodontics, prosthodontics and oral and maxillofacial surgery.[9,22,171,180,181] It should be noted that orthodontic/prosthodontic treatments might compromise esthetics and periodontal health.[22,190,191]
CONCLUSION
CMT is a prevalent multifactorial dental anomaly, usually appearing in females and in the permanent dentition. It is not conclusive whether it tends to occur more in the maxilla or mandible and also in the anterior versus posterior segments. It can accompany various dentoskeletal deformities, anomalies, or simply complications. Thus it should be attended by expert teams at the earliest possibility.
Although the CMT prevalence has been investigated thoroughly, no or few quasi-experimental (case-control or cohort) studies have assessed CMT risk factors. Besides, the number of studies assessing the severity of CMT is very small as well. It is recommended to evaluate within quasi-experimental designs the effect of gender on the prevalence of CMT and also its effect on the severity of CMT. Another problem which should be avoided in future research is the lack of proper report of every finding in many studies. Future studies are recommended to report not only the prevalence of CMT, but also the prevalence of cases with different numbers of missing teeth (for example how many subjects had two, three, or more missing teeth? etc.). This is valuable, since definitions of hypodontia might differ from study to study.[3,15,31,64] This approach would allow the standardization of the results. Another suggestion might be a global consensus on the definitions. Furthermore, it would be helpful if each study clearly defines hypodontia. Many studies have used the term hypodontia to refer to congenitally absent teeth in general. Perhaps it would be better to distinguish CMT and hypodontia in each report, by clearly defining the hypodontia (for example congenital missing of six teeth or more) or oligodontia terminologies (for example congenital missing of 10 teeth or more) in each study. Another limitation of most previous studies is that they have not reported the number of the affected patients with bilateral CMT, unilateral CMT and both simultaneously.[64]
Future studies are warranted to state the severity of CMT in both genders, both arches, both sides (left/right) and across other possible variable levels. The data can be simply summarized within a couple of tables and/or figures. Therefore, it is highly recommended to state all the numbers of all the missing teeth according to tooth types, jaws and sides, etc., in each study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Altug-Atac AT, Erdem D. Prevalence and distribution of dental anomalies in orthodontic patients. Am J Orthod Dentofacial Orthop. 2007;131:510–4. doi: 10.1016/j.ajodo.2005.06.027. [DOI] [PubMed] [Google Scholar]
- 2.De Coster PJ, Marks LA, Martens LC, Huysseune A. Dental agenesis: Genetic and clinical perspectives. J Oral Pathol Med. 2009;38:1–17. doi: 10.1111/j.1600-0714.2008.00699.x. [DOI] [PubMed] [Google Scholar]
- 3.Goya HA, Tanaka S, Maeda T, Akimoto Y. An orthopantomographic study of hypodontia in permanent teeth of Japanese pediatric patients. J Oral Sci. 2008;50:143–50. doi: 10.2334/josnusd.50.143. [DOI] [PubMed] [Google Scholar]
- 4.Bäckman B, Wahlin YB. Variations in number and morphology of permanent teeth in 7-year-old Swedish children. Int J Paediatr Dent. 2001;11:11–7. doi: 10.1046/j.1365-263x.2001.00205.x. [DOI] [PubMed] [Google Scholar]
- 5.Endo T, Ozoe R, Kubota M, Akiyama M, Shimooka S. A survey of hypodontia in Japanese orthodontic patients. Am J Orthod Dentofacial Orthop. 2006;129:29–35. doi: 10.1016/j.ajodo.2004.09.024. [DOI] [PubMed] [Google Scholar]
- 6.Pemberton TJ, Das P, Patel PI. Hypodontia: Genetics and future perspectives. Braz J Oral Sci. 2005;4:695–709. [Google Scholar]
- 7.Nik-Hussein NN. Hypodontia in the permanent dentition: A study of its prevalence in Malaysian children. Aust Orthod J. 1989;11:93–5. [PubMed] [Google Scholar]
- 8.Amini F, Rakhshan V, Babaei P. Prevalence and pattern of hypodontia in the permanent dentition of 3374 Iranian orthodontic patients. Dent Res J (Isfahan) 2012;9:245–50. [PMC free article] [PubMed] [Google Scholar]
- 9.Behr M, Proff P, Leitzmann M, Pretzel M, Handel G, Schmalz G, et al. Survey of congenitally missing teeth in orthodontic patients in Eastern Bavaria. Eur J Orthod. 2011;33:32–6. doi: 10.1093/ejo/cjq021. [DOI] [PubMed] [Google Scholar]
- 10.Meaney S, Anweigi L, Ziada H, Allen F. The impact of hypodontia: A qualitative study on the experiences of patients. Eur J Orthod. 2012;34:547–52. doi: 10.1093/ejo/cjr061. [DOI] [PubMed] [Google Scholar]
- 11.Oshagh M, Salehi P, Pakshir H, Bazyar L, Rakhshan V. Associations between normative and self-perceived orthodontic treatment needs in young-adult dental patients. Korean J Orthod. 2011;41:440–6. [Google Scholar]
- 12.Khosravanifard B, Ghanbari-Azarnir S, Rakhshan H, Sajjadi SH, Ehsan AM, Rakhshan V. Association between orthodontic treatment need and masticatory performance. Orthodontics (Chic) 2012;13:e20–8. [PubMed] [Google Scholar]
- 13.Kokich VG, Kokich VO. Congenitally missing mandibular second premolars: Clinical options. Am J Orthod Dentofacial Orthop. 2006;130:437–44. doi: 10.1016/j.ajodo.2006.05.025. [DOI] [PubMed] [Google Scholar]
- 14.Chung CJ, Han JH, Kim KH. The pattern and prevalence of hypodontia in Koreans. Oral Dis. 2008;14:620–5. doi: 10.1111/j.1601-0825.2007.01434.x. [DOI] [PubMed] [Google Scholar]
- 15.Aktan A, Kara I, Şener İ, Bereket C, Ay S, Çiftçi M. Radiographic study of tooth agenesis in the Turkish population. Oral Radiol. 2010;26:95–100. [Google Scholar]
- 16.Kumar SK, Lakshmi AV, Namita S, Elumalai M. Craniofacial morphologic variations and its association with hypodontia pattern (Anterior) in South Indian female population. Biosci Biotechnol Res Asia. 2013;10:325–8. [Google Scholar]
- 17.Shimizu T, Maeda T. Prevalence and genetic basis of tooth agenesis. Jpn Dent Sci Rev. 2009;45:52–8. [Google Scholar]
- 18.Murdock S, Lee JY, Guckes A, Wright JT. A costs analysis of dental treatment for ectodermal dysplasia. J Am Dent Assoc. 2005;136:1273–6. doi: 10.14219/jada.archive.2005.0343. [DOI] [PubMed] [Google Scholar]
- 19.Nunn JH, Carter NE, Gillgrass TJ, Hobson RS, Jepson NJ, Meechan JG, et al. The interdisciplinary management of hypodontia: Background and role of paediatric dentistry. Br Dent J. 2003;194:245–51. doi: 10.1038/sj.bdj.4809925. [DOI] [PubMed] [Google Scholar]
- 20.Graber LW. Congenital absence of teeth: A review with emphasis on inheritance patterns. J Am Dent Assoc. 1978;96:266–75. doi: 10.14219/jada.archive.1978.0054. [DOI] [PubMed] [Google Scholar]
- 21.Lyngstadaas SP, Nordbo H, Gedde-Dahl T, Jr, Thrane PS. On the genetics of hypodontia and microdontia: Synergism or allelism of major genes in a family with six affected members. J Med Genet. 1996;33:137–42. doi: 10.1136/jmg.33.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fekonja A. Hypodontia in orthodontically treated children. Eur J Orthod. 2005;27:457–60. doi: 10.1093/ejo/cji027. [DOI] [PubMed] [Google Scholar]
- 23.Galluccio G, Pilotto A. Genetics of dental agenesis: Anterior and posterior area of the arch. Eur Arch Paediatr Dent. 2008;9:41–5. doi: 10.1007/BF03321595. [DOI] [PubMed] [Google Scholar]
- 24.Hall RK. Congenitally missing teeth — A diagnostic feature in many syndromes of the head and neck. J Int Assoc Dent Child. 1983;14:69–75. [PubMed] [Google Scholar]
- 25.Varela M, Trujillo-Tiebas MJ, Garcia-Camba P. Case report: Identical twins revealing discordant hypodontia. The rationale of dental arch differences in monozygotic twins. Eur Arch Paediatr Dent. 2011;12:318–22. doi: 10.1007/BF03262831. [DOI] [PubMed] [Google Scholar]
- 26.Militi D, Militi A, Cutrupi MC, Portelli M, Rigoli L, Matarese G, et al. Genetic basis of non syndromic hypodontia: A DNA investigation performed on three couples of monozygotic twins about PAX9 mutation. Eur J Paediatr Dent. 2011;12:21–4. [PubMed] [Google Scholar]
- 27.Markovic M. Hypodontia in twins. Swed Dent J Suppl. 1982;15:153–62. [PubMed] [Google Scholar]
- 28.Forgie AH, Thind BS, Larmour CJ, Mossey PA, Stirrups DR. Management of hypodontia: Restorative considerations. Part III. Quintessence Int. 2005;36:437–45. [PubMed] [Google Scholar]
- 29.Varela M, Arrieta P, Ventureira C. Non-syndromic concomitant hypodontia and supernumerary teeth in an orthodontic population. Eur J Orthod. 2009;31:632–7. doi: 10.1093/ejo/cjp046. [DOI] [PubMed] [Google Scholar]
- 30.Larmour CJ, Mossey PA, Thind BS, Forgie AH, Stirrups DR. Hypodontia — A retrospective review of prevalence and etiology. Part I. Quintessence Int. 2005;36:263–70. [PubMed] [Google Scholar]
- 31.Gomes RR, da Fonseca JA, Paula LM, Faber J, Acevedo AC. Prevalence of hypodontia in orthodontic patients in Brasilia, Brazil. Eur J Orthod. 2010;32:302–6. doi: 10.1093/ejo/cjp107. [DOI] [PubMed] [Google Scholar]
- 32.Lai PY, Seow WK. A controlled study of the association of various dental anomalies with hypodontia of permanent teeth. Pediatr Dent. 1989;11:291–6. [PubMed] [Google Scholar]
- 33.Wu CC, Wong RW, Hägg U. A review of hypodontia: The possible etiologies and orthodontic, surgical and restorative treatment options-conventional and futuristic. Hong Kong Dent J. 2007;4:113–21. [Google Scholar]
- 34.Polder BJ, Van’t Hof MA, Van der Linden FP, Kuijpers-Jagtman AM. A meta-analysis of the prevalence of dental agenesis of permanent teeth. Community Dent Oral Epidemiol. 2004;32:217–26. doi: 10.1111/j.1600-0528.2004.00158.x. [DOI] [PubMed] [Google Scholar]
- 35.AlShahrani I, Togoo RA, AlQarni MA. A review of hypodontia: Classification, prevalence, etiology, associated anomalies, clinical implications and treatment options. World J Dent. 2013;4:117–25. [Google Scholar]
- 36.Shapira Y, Lubit E, Kuftinec MM. Hypodontia in children with various types of clefts. Angle Orthod. 2000;70:16–21. doi: 10.1043/0003-3219(2000)070<0016:HICWVT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 37.Karwetzky R, Homeyer H. About the ectodermal dysplasia from an orthodontic view [Über die ektodermale dysplasie aus kieferorthopädischer sicht] J Orofac Orthop. 1974;35:33–9. [Google Scholar]
- 38.Ishizuka K, Sasaki T, Imai R, Nakamura N, Yoshida T, Anabuki M, et al. Abnomalies of teeth which affects the orthodontic treatment. Nichidai Shigaku. 1988;62:584–95. [Google Scholar]
- 39.Schalk van der Weide Y, Prahl-Andersen B, Bosman F. Tooth formation in patients with oligodontia. Angle Orthod. 1993;63:31–7. doi: 10.1043/0003-3219(1993)063<0031:TFIPWO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 40.Schalk-van der Weide Y, Steen WH, Bosman F. Distribution of missing teeth and tooth morphology in patients with oligodontia. ASDC J Dent Child. 1992;59:133–40. [PubMed] [Google Scholar]
- 41.Rune B, Sarnäs KV. Tooth size and tooth formation in children with advanced hypodontia. Angle Orthod. 1974;44:316–21. doi: 10.1043/0003-3219(1974)044<0316:TSATFI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 42.Ma C. Statistical observation of morphological and numerical teeth anomalies in the teeth of Japanese. Shikagaku Zasshi. 1949;6:248–56. [Google Scholar]
- 43.Thesleff I. The genetic basis of tooth development and dental defects. Am J Med Genet A. 2006;140:2530–5. doi: 10.1002/ajmg.a.31360. [DOI] [PubMed] [Google Scholar]
- 44.Thesleff I. Genetic basis of tooth development and dental defects. Acta Odontol Scand. 2000;58:191–4. doi: 10.1080/000163500750051728. [DOI] [PubMed] [Google Scholar]
- 45.Goldenberg M, Das P, Messersmith M, Stockton DW, Patel PI, D’Souza RN. Clinical, radiographic, and genetic evaluation of a novel form of autosomal-dominant oligodontia. J Dent Res. 2000;79:1469–75. doi: 10.1177/00220345000790070701. [DOI] [PubMed] [Google Scholar]
- 46.Arte S, Nieminen P, Apajalahti S, Haavikko K, Thesleff I, Pirinen S. Characteristics of incisor-premolar hypodontia in families. J Dent Res. 2001;80:1445–50. doi: 10.1177/00220345010800051201. [DOI] [PubMed] [Google Scholar]
- 47.Vastardis H, Karimbux N, Guthua SW, Seidman JG, Seidman CE. A human MSX1 homeodomain missense mutation causes selective tooth agenesis. Nat Genet. 1996;13:417–21. doi: 10.1038/ng0896-417. [DOI] [PubMed] [Google Scholar]
- 48.Ahmad W, Brancolini V, ul Faiyaz MF, Lam H, ul Haque S, Haider M, et al. A locus for autosomal recessive hypodontia with associated dental anomalies maps to chromosome 16q12.1. Am J Hum Genet. 1998;62:987–91. doi: 10.1086/301799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pirinen S, Kentala A, Nieminen P, Varilo T, Thesleff I, Arte S. Recessively inherited lower incisor hypodontia. J Med Genet. 2001;38:551–6. doi: 10.1136/jmg.38.8.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Erpenstein H, Pfeiffer RA. Sex-linked-dominant hereditary reduction in number of teeth. Humangenetik. 1967;4:280–93. doi: 10.1007/BF00292201. [DOI] [PubMed] [Google Scholar]
- 51.Castaldi CR, Bodnarchuk A, MacRae PD, Zacherl WA. Incidence of congenital anomalies in permanent teeth of a group of Canadian children aged 6-9. J Can Dent Assoc (Tor) 1966;32:154–9. [PubMed] [Google Scholar]
- 52.Vieira AR. Oral clefts and syndromic forms of tooth agenesis as models for genetics of isolated tooth agenesis. J Dent Res. 2003;82:162–5. doi: 10.1177/154405910308200303. [DOI] [PubMed] [Google Scholar]
- 53.Nieminen P, Arte S, Pirinen S, Peltonen L, Thesleff I. Gene defect in hypodontia: Exclusion of MSX1 and MSX2 as candidate genes. Hum Genet. 1995;96:305–8. doi: 10.1007/BF00210412. [DOI] [PubMed] [Google Scholar]
- 54.Vastardis H. The genetics of human tooth agenesis: New discoveries for understanding dental anomalies. Am J Orthod Dentofacial Orthop. 2000;117:650–6. [PubMed] [Google Scholar]
- 55.Vieira AR, Modesto A, Meira R, Barbosa AR, Lidral AC, Murray JC. Interferon regulatory factor 6 (IRF6) and fibroblast growth factor receptor 1 (FGFR1) contribute to human tooth agenesis. Am J Med Genet A. 2007;143:538–45. doi: 10.1002/ajmg.a.31620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vieira AR, Meira R, Modesto A, Murray JC. MSX1, PAX9, and TGFA contribute to tooth agenesis in humans. J Dent Res. 2004;83:723–7. doi: 10.1177/154405910408300913. [DOI] [PubMed] [Google Scholar]
- 57.Küchler EC, Risso PA, Costa Mde C, Modesto A, Vieira AR. Studies of dental anomalies in a large group of school children. Arch Oral Biol. 2008;53:941–6. doi: 10.1016/j.archoralbio.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 58.Stockton DW, Das P, Goldenberg M, D’Souza RN, Patel PI. Mutation of PAX9 is associated with oligodontia. Nat Genet. 2000;24:18–9. doi: 10.1038/71634. [DOI] [PubMed] [Google Scholar]
- 59.Frazier-Bowers SA, Guo DC, Cavender A, Xue L, Evans B, King T, et al. A novel mutation in human PAX9 causes molar oligodontia. J Dent Res. 2002;81:129–33. [PubMed] [Google Scholar]
- 60.Sheikhi M, Sadeghi MA, Ghorbanizadeh S. Prevalence of congenitally missing permanent teeth in Iran. Dent Res J (Isfahan) 2012;9(Suppl 1):105–11. [PMC free article] [PubMed] [Google Scholar]
- 61.Jowett AK, Vainio S, Ferguson MW, Sharpe PT, Thesleff I. Epithelial-mesenchymal interactions are required for msx 1 and msx 2 gene expression in the developing murine molar tooth. Development. 1993;117:461–70. doi: 10.1242/dev.117.2.461. [DOI] [PubMed] [Google Scholar]
- 62.De Muynck S, Schollen E, Matthijs G, Verdonck A, Devriendt K, Carels C. A novel MSX1 mutation in hypodontia. Am J Med Genet A. 2004;128A:401–3. doi: 10.1002/ajmg.a.30181. [DOI] [PubMed] [Google Scholar]
- 63.Mostowska A, Biedziak B, Jagodzinski PP. Novel MSX1 mutation in a family with autosomal-dominant hypodontia of second premolars and third molars. Arch Oral Biol. 2012;57:790–5. doi: 10.1016/j.archoralbio.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 64.Rakhshan V. Meta-analysis and systematic review of factors biasing the observed prevalence of congenitally missing teeth in permanent dentition excluding third molars. Prog Orthod. 2013;14:33. doi: 10.1186/2196-1042-14-33. DOI: 10.1186/2196-1042-14-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kim YH. Investigation of hypodontia as clinically related dental anomaly: Prevalence and characteristics. ISRN Dent 2011. 2011 doi: 10.5402/2011/246135. 246135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Durrani OK, Zulfiqar K, Bashir U, Shamsher M. Prevalence of tooth agenesis in orthodontic patients at Islamic international dental hospital. Pak Orthod J. 2010;2:48–51. [Google Scholar]
- 67.Bergström K. An orthopantomographic study of hypodontia, supernumeraries and other anomalies in school children between the ages of 8-9 years. An epidemiological study. Swed Dent J. 1977;1:145–57. [PubMed] [Google Scholar]
- 68.Wisth PJ, Thunold K, Böe OE. Frequency of hypodontia in relation to tooth size and dental arch width. Acta Odontol Scand. 1974;32:201–6. doi: 10.3109/00016357409002548. [DOI] [PubMed] [Google Scholar]
- 69.Ng’ang’a RN, Ng’ang’a PM. Hypodontia of permanent teeth in a Kenyan population. East Afr Med J. 2001;78:200–3. doi: 10.4314/eamj.v78i4.9063. [DOI] [PubMed] [Google Scholar]
- 70.Sisman Y, Uysal T, Gelgor IE. Hypodontia. Does the prevalence and distribution pattern differ in orthodontic patients? Eur J Dent. 2007;1:167–73. [PMC free article] [PubMed] [Google Scholar]
- 71.Vahid-Dastjerdi E, Borzabadi-Farahani A, Mahdian M, Amini N. Non-syndromic hypodontia in an Iranian orthodontic population. J Oral Sci. 2010;52:455–61. doi: 10.2334/josnusd.52.455. [DOI] [PubMed] [Google Scholar]
- 72.Aasheim B, Ogaard B. Hypodontia in 9-year-old Norwegians related to need of orthodontic treatment. Scand J Dent Res. 1993;101:257–60. doi: 10.1111/j.1600-0722.1993.tb01115.x. [DOI] [PubMed] [Google Scholar]
- 73.Daito M, Tanaka T, Hieda T. Clinical observations on the development of third molars. J Osaka Dent Univ. 1992;26:91–104. [PubMed] [Google Scholar]
- 74.Garn SM, Lewis AB, Bonné B. Third molar formation and its development course. Angle Orthod. 1962;32:270–9. [Google Scholar]
- 75.Brook AH. Dental anomalies of number, form and size: Their prevalence in British schoolchildren. J Int Assoc Dent Child. 1974;5:37–53. [PubMed] [Google Scholar]
- 76.Daugaard-Jensen J, Nodal M, Skovgaard LT, Kjaer I. Comparison of the pattern of agenesis in the primary and permanent dentitions in a population characterized by agenesis in the primary dentition. Int J Paediatr Dent. 1997;7:143–8. doi: 10.1046/j.1365-263x.1997.00230.x. [DOI] [PubMed] [Google Scholar]
- 77.Guttal KS, Naikmasur VG, Bhargava P, Bathi RJ. Frequency of developmental dental anomalies in the Indian population. Eur J Dent. 2010;4:263–9. [PMC free article] [PubMed] [Google Scholar]
- 78.Yanagida I, Mori S. Statistical studies on numerical anomalies of teeth in children using orthopantomograms — Congenital hypodontia. Osaka Daigaku Shigaku Zasshi. 1990;35:580–93. [PubMed] [Google Scholar]
- 79.Dolder E. Deficient dentition. Dent Pract Dent Rec. 1936;57:142–3. [Google Scholar]
- 80.Werther R, Rothenberg F. Anodontia: A review of its etiology with presentation of a case. Am J Orthod. 1939;25:61–81. [Google Scholar]
- 81.Byrd ED. Incidence of supernumerary and congenitally missing teeth. J Dent Child. 1943;10:84–6. [Google Scholar]
- 82.Okamoto O, Mori O, Morimoto M, Nakao N, Miyakawa E. A statistical and genetic study related to congenital missing teeth. Shika Gakuho. 1951;5:8–10. [Google Scholar]
- 83.Terasaki T, Shiota K. Congenital absence of teeth. Nihon Kokyuki Gakkai Zasshi. 1954;3:88–93. [Google Scholar]
- 84.Tsutsui H, Yoshida Y. Clinical statistical study on supernumerary teeth and congenital absence of teeth. Kokubyo Gakkai Zasshi. 1955;22:44–8. [Google Scholar]
- 85.Grahnén H. Hypodontia in the permanent dentition. A clinical and genetical investigation. Odontol Revy. 1956;7:1–100. [Google Scholar]
- 86.Clayton JM. Congenital dental anomalies occurring in 3557 children. J Dent Child. 1956;23:206–8. [Google Scholar]
- 87.Lind V. Congenital number variations in the permanent dentition [Medfödda antalsvariationer i permanenta dentitionen] Odontol Revy. 1959;10:176–89. [PubMed] [Google Scholar]
- 88.Glenn F. Incidence of congenitally missing permanent teeth in a private pedodontic practice. ASDC J Dent Child. 1961;28:317–20. [Google Scholar]
- 89.Gimnes H. A frequency investigation of hypodontia in schoolchildren in Oslo, with a special regard to incidence of bilateral hypodontia of second Premolar in the lower jaw [En frekvensundersøkelse over hypodonti hos skolebarn i Oslo, med saerlig henblikk på forekomst av bilateral hypodonti av 2. premolar i underkjeven] Nor Tannlaegeforen Tid. 1963;73:141–8. [Google Scholar]
- 90.Volk A. About the frequency of occurrence of missing tooth systems [Über die häufigkeit des vorkommens von fehlenden zahnanlagen] Schweiz Monatsschr Zahnmed. 1963;73:320–34. [Google Scholar]
- 91.Niswander JD, Sujaku C. Congenital anomalies of teeth in Japanese children. Am J Phys Anthropol. 1963;21:569–74. doi: 10.1002/ajpa.1330210413. [DOI] [PubMed] [Google Scholar]
- 92.Glenn FB. A consecutive six-year study of the prevalence of congenitally missing teeth in private pedodontic practice of two geographically separated areas. J Dent Child. 1964;31:264–270. [Google Scholar]
- 93.Rosenzweig KA, Garbarski D. Numerical aberrations in the permanent teeth of grade school children in Jerusalem. Am J Phys Anthropol. 1965;23:277–83. doi: 10.1002/ajpa.1330230315. [DOI] [PubMed] [Google Scholar]
- 94.Rose JS. A survey of congenitally missing teeth, excluding third molars, in 6000 orthodontic patients. Dent Pract Dent Rec. 1966;17:107–14. [PubMed] [Google Scholar]
- 95.Horowitz JM. Aplasia and malocclusion: A survey and appraisal. Am J Orthod. 1966;52:440–53. doi: 10.1016/0002-9416(66)90122-9. [DOI] [PubMed] [Google Scholar]
- 96.Blayney J, Hill I. Congenitally missing teeth. J Am Dent Assoc. 1967;74:298–9. doi: 10.14219/jada.archive.1970.0151. [DOI] [PubMed] [Google Scholar]
- 97.Davies PL. Agenesis of teeth of the permanent dentition: A frequency study in Sydney schoolchildren. Aust Dent J. 1968;13:146–50. doi: 10.1111/j.1834-7819.1968.tb02254.x. [DOI] [PubMed] [Google Scholar]
- 98.Helm S. Malocclusion in Danish children with adolescent dentition: An epidemiologic study. Am J Orthod. 1968;54:352–66. doi: 10.1016/0002-9416(68)90304-7. [DOI] [PubMed] [Google Scholar]
- 99.Muller TP, Hill IN, Peterson AC, Blayney JR. A survey of congenitally missing permanent teeth. J Am Dent Assoc. 1970;81:101–7. doi: 10.14219/jada.archive.1970.0151. [DOI] [PubMed] [Google Scholar]
- 100.Haavikko K. Hypodontia of permanent teeth. An orthopantomographic study. Suom Hammaslaak Toim. 1971;67:219–25. [PubMed] [Google Scholar]
- 101.McKibben DR, Brearley LJ. Radiographic determination of the prevalence of selected dental anomalies in children. ASDC J Dent Child. 1971;28:390–8. [PubMed] [Google Scholar]
- 102.Egermark-Eriksson I, Lind V. Congenital numerical variation in the permanent dentition. D. Sex distribution of hypodontia and hyperodontia. Odontol Revy. 1971;22:309–15. [PubMed] [Google Scholar]
- 103.Hanaoka H, Yamauchi K, Kawasoko S, Imada Y. Anomalies in number of teeth of orthodontic patients. 3. Relationship to malocclusion. Nihon Kyosei Shika Gakkai Zasshi. 1972;31:162–7. [PubMed] [Google Scholar]
- 104.Eidelman E, Chosack A, Rosenzweig KA. Hypodontia: Prevalence amongst Jewish populations of different origin. Am J Phys Anthropol. 1973;39:129–33. doi: 10.1002/ajpa.1330390113. [DOI] [PubMed] [Google Scholar]
- 105.Ravn JJ, Nielsen LA. An orthopantomographic investigation of supernumerary teeth and aplasias in 1530 Copenhagen school children. Tandlaegebladet. 1973;77:12–22. [PubMed] [Google Scholar]
- 106.Hunstadbraten K. Hypodontia in the permanent dentition. ASDC J Dent Child. 1973;40:115–7. [PubMed] [Google Scholar]
- 107.Thilander B, Myrberg N. The prevalence of malocclusion in Swedish schoolchildren. Scand J Dent Res. 1973;81:12–21. doi: 10.1111/j.1600-0722.1973.tb01489.x. [DOI] [PubMed] [Google Scholar]
- 108.Bachmann H. Zürich: University of Zürich; 1974. The incidence of agenesis of permanent teeth (excluding wisdom teeth). Results of the analysis of 8694 panoramic radiographs of 9- to 10-year-old school children from Zurich [Die Häufigkeit von Nichtanlagen bleibender Zähne (ausgenommen der Weisheitszähne). Ergebnisse der Auswertung von 8694 Orthopantogrammen 9-10 Jährigen Schulkinder aus Zürich], Dissertation. [Google Scholar]
- 109.Thompson GW, Popovich F. Probability of congenitally missing teeth: Results in 1,191 children in the Burlington Growth centre in Toronto. Community Dent Oral Epidemiol. 1974;2:26–32. doi: 10.1111/j.1600-0528.1974.tb01790.x. [DOI] [PubMed] [Google Scholar]
- 110.Magnússon TE. An epidemiologic study of dental space anomalies in Icelandic schoolchildren. Community Dent Oral Epidemiol. 1977;5:292–300. doi: 10.1111/j.1600-0528.1977.tb01017.x. [DOI] [PubMed] [Google Scholar]
- 111.Nakahara M, Okada S, Tani H, Okada S, Tani H. A survey of congenitally missing permanent teeth in Hokkaido. Koku Eisei Gakkai Zasshi. 1977;27:21–3. doi: 10.5834/jdh.27.21. [DOI] [PubMed] [Google Scholar]
- 112.Maklin M, Dummett CO, Jr, Weinberg R. A study of oligodontia in a sample of New Orleans children. ASDC J Dent Child. 1979;46:478–82. [PubMed] [Google Scholar]
- 113.Rølling S. Hypodontia of permanent teeth in Danish schoolchildren. Scand J Dent Res. 1980;88:365–9. doi: 10.1111/j.1600-0722.1980.tb01240.x. [DOI] [PubMed] [Google Scholar]
- 114.Locht S. Panoramic radiographic examination of 704 Danish children aged 9-10 years. Community Dent Oral Epidemiol. 1980;8:375–80. doi: 10.1111/j.1600-0528.1980.tb01311.x. [DOI] [PubMed] [Google Scholar]
- 115.Davis PJ. Hypodontia and hyperdontia of permanent teeth in Hong Kong schoolchildren. Community Dent Oral Epidemiol. 1987;15:218–20. doi: 10.1111/j.1600-0528.1987.tb00524.x. [DOI] [PubMed] [Google Scholar]
- 116.Lo Muzio L, Mignogna MD, Bucci P, Sorrentino F. Statistical study of the incidence of agenesis in a sample of 1529 subjects. Minerva Stomatol. 1989;38:1045–51. [PubMed] [Google Scholar]
- 117.Ignelzi MA, Jr, Fields HW, Vann WF., Jr Screening panoramic radiographs in children: Prevalence data and implications. Pediatr Dent. 1989;11:279–85. [PubMed] [Google Scholar]
- 118.Salem G. Prevalence of selected dental anomalies in Saudi children from Gizan region. Community Dent Oral Epidemiol. 1989;17:162–3. doi: 10.1111/j.1600-0528.1989.tb00014.x. [DOI] [PubMed] [Google Scholar]
- 119.Burden D, Connolly I. Radiographic study of hypodontia and other anomalies in orthodontic patients. J Dent Res. 1989;68:295. [Google Scholar]
- 120.Renkerová M, Badura S, Manicová H, Jambor J. A contribution to anomalous number of teeth in children in the Zilina District. Prakt Zubn Lek. 1989;37:12–8. [PubMed] [Google Scholar]
- 121.al-Emran S. Prevalence of hypodontia and developmental malformation of permanent teeth in Saudi Arabian schoolchildren. Br J Orthod. 1990;17:115–8. doi: 10.1179/bjo.17.2.115. [DOI] [PubMed] [Google Scholar]
- 122.Dechkunakorn S, Chaiwat J, Sawaengkit P. Congenital absence and loss of teeth in an orthodontic patient group. J Dent Assoc Thai. 1990;40:165–76. [PubMed] [Google Scholar]
- 123.Lynham A. Panoramic radiographic survey of hypodontia in Australian Defence Force recruits. Aust Dent J. 1990;35:19–22. doi: 10.1111/j.1834-7819.1990.tb03021.x. [DOI] [PubMed] [Google Scholar]
- 124.O’Dowling IB, McNamara TG. Congenital absence of permanent teeth among Irish school-children. J Ir Dent Assoc. 1990;36:136–8. [PubMed] [Google Scholar]
- 125.Legović M, Ceranić I, Cehich A. Anomalies in the number of permanent teeth in orthodontic patients in 2 localities in Croatia. Schweiz Monatsschr Zahnmed. 1990;100:286–90. [PubMed] [Google Scholar]
- 126.Polastri F, Cerato E, Gallesio C. The clinico-radiological assessment of dental anomalies with real and apparent numerical defects. Minerva Stomatol. 1991;40:415–23. [PubMed] [Google Scholar]
- 127.Watanabe K, Motoyoshi M, Fukui R, Chang K, Namba A, Mamura S. A study on incidence of congenital missing of teeth among orthodontics patients. Nichidai Shigaku (Nihon Univ Dent J) 1992;66:1029–33. [Google Scholar]
- 128.Cua-Benward GB, Dibaj S, Ghassemi B. The prevalence of congenitally missing teeth in class I, II, III malocclusions. J Clin Pediatr Dent. 1992;17:15–7. [PubMed] [Google Scholar]
- 129.Ogita S, Ogita M, Yamamoto T, Yanase H, Kondo Y, Yokoi K. The appearance of supernumerary teeth and congenitally missing teeth in 6299 Japanese pediatric patients. Aichi-Gakuin J Dent Sci. 1995;33:19–27. [Google Scholar]
- 130.Cuairán RV, Gaitan ZL, Hernández MA. Agenesia dental en una muestra de pacientes ortodónticos del Hospital Infantil de México. ADM. 1996;53:211–5. [Google Scholar]
- 131.Johannsdottir B, Wisth PJ, Magnusson TE. Prevalence of malocclusion in 6-year-old Icelandic children. Acta Odontol Scand. 1997;55:398–402. doi: 10.3109/00016359709059206. [DOI] [PubMed] [Google Scholar]
- 132.Peltola JS, Wolf J, Männik A, Russak S, Seedre T, Sirkel M, et al. Radiographic findings in the teeth and jaws of 14-to 17-year-old Estonian schoolchildren in Tartu and Tallinn. Acta Odontol Scand. 1997;55:31–5. doi: 10.3109/00016359709091938. [DOI] [PubMed] [Google Scholar]
- 133.Tsai SJ, King NM. A catalogue of anomalies and traits of the permanent dentition of southern Chinese. J Clin Pediatr Dent. 1998;22:185–94. [PubMed] [Google Scholar]
- 134.Ghaznawi HI, Daas H, Salako NO. A clinical and radiographic survey of selected dental anomalies and conditions in a Saudi Arabian population. Saudi Dent J. 1999;11:8–13. [Google Scholar]
- 135.Hirukawa K, Iwata R, Kurosawa M, Kondo T, Goto S. Statistical investigation about the prevalence of congenitally missing permanent teeth. Orthod Waves. 1999;58:49–56. [Google Scholar]
- 136.Gábris K, Tarján I, Csiki P, Konrád F, Szádeczky B, Rózsa N. Prevalence of congenital hypodontia in the permanent dentition and its treatment. Fogorv Sz. 2001;94:137–40. [PubMed] [Google Scholar]
- 137.Moon HS, Choi SC, Choung PH. Hypodontia and hyperdontia of permanent teeth in Korean schoolchildren. Cleft Lip Palate Assoc. 2001;4:19–27. [Google Scholar]
- 138.Nordgarden H, Jensen JL, Storhaug K. Reported prevalence of congenitally missing teeth in two Norwegian counties. Community Dent Health. 2002;19:258–61. [PubMed] [Google Scholar]
- 139.Al-Nakib LH, Younis WH. Orthopantomographic survey of hypodontia among Iraqi orthodontic patients. J Baghdad Coll Dent. 2002;4:74. [Google Scholar]
- 140.Osuji OO, Hardie J. Dental anomalies in a population of Saudi Arabian children in Tabuk. Saudi Dent J. 2002;14:11–4. [Google Scholar]
- 141.Silva Meza R. Radiographic assessment of congenitally missing teeth in orthodontic patients. Int J Paediatr Dent. 2003;13:112–6. doi: 10.1046/j.1365-263x.2003.00436.x. [DOI] [PubMed] [Google Scholar]
- 142.Albashaireh ZS, Khader YS. The prevalence and pattern of hypodontia of the permanent teeth and crown size and shape deformity affecting upper lateral incisors in a sample of Jordanian dental patients. Community Dent Health. 2006;23:239–43. [PubMed] [Google Scholar]
- 143.Gábris K, Fábián G, Kaán M, Rózsa N, Tarján I. Prevalence of hypodontia and hyperdontia in paedodontic and orthodontic patients in Budapest. Community Dent Health. 2006;23:80–2. [PubMed] [Google Scholar]
- 144.Peker I, Kaya E, Darendeliler-Yaman S. Clinic and radiographical evaluation of non-syndromic hypodontia and hyperdontia in permanent dentition. Med Oral Patol Oral Cir Bucal. 2009;14:e393–7. [PubMed] [Google Scholar]
- 145.Uslu O, Akcam MO, Evirgen S, Cebeci I. Prevalence of dental anomalies in various malocclusions. Am J Orthod Dentofacial Orthop. 2009;135:328–35. doi: 10.1016/j.ajodo.2007.03.030. [DOI] [PubMed] [Google Scholar]
- 146.Ajami B, Shab ZM, Afzal Aghaei M, Mehrjerdian MC. Prevalence and pattern of congenital missing teeth in a group of Iranian adolescents. J Dent (Shiraz) 2010;10:40–4. [Google Scholar]
- 147.Celikoglu M, Kazanci F, Miloglu O, Oztek O, Kamak H, Ceylan I. Frequency and characteristics of tooth agenesis among an orthodontic patient population. Med Oral Patol Oral Cir Bucal. 2010;15:e797–801. doi: 10.4317/medoral.15.e797. [DOI] [PubMed] [Google Scholar]
- 148.Tallón-Walton V, Nieminen P, Arte S, Carvalho-Lobato P, Ustrell-Torrent JM, Manzanares-Céspedes MC. An epidemiological study of dental agenesis in a primary health area in Spain: Estimated prevalence and associated factors. Med Oral Patol Oral Cir Bucal. 2010;15:e569–74. doi: 10.4317/medoral.15.e569. [DOI] [PubMed] [Google Scholar]
- 149.AlJabaa AH, Mohammad AA. Saudi Arabia: King Saud University; 2010. A study on dento/skeletal discrepancies and dental anomalies in a sample of saudi orthodontic patients [Dissertation] [Google Scholar]
- 150.Lee JH, Yang BH, Lee SM, Kim YH, Shim HW, Chung HS. A study on the prevalence of dental anomalies in Korean dental-patients. Korean J Orthod. 2011;41:346–53. [Google Scholar]
- 151.Gupta SK, Saxena P, Jain S, Jain D. Prevalence and distribution of selected developmental dental anomalies in an Indian population. J Oral Sci. 2011;53:231–8. doi: 10.2334/josnusd.53.231. [DOI] [PubMed] [Google Scholar]
- 152.Shetty P, Adyanthaya A, Adyanthaya S, Sreelatha SV. The prevalence of hypodontia and supernumerary teeth in 2469 school children of the Indian population: An epidemiological study. Indian J Stomatol. 2012;3:150–2. [Google Scholar]
- 153.Cantekin K, Dane A, Miloglu O, Kazanci F, Bayrakdar S, Celikoglu M. Prevalence and intra-oral distribution of agenesis of permanent teeth among Eastern Turkish children. Eur J Paediatr Dent. 2012;13:53–6. [PubMed] [Google Scholar]
- 154.González-Allo A, Campoy MD, Moreira J, Ustrell J, Pinho T. Tooth agenesis in a Portuguese population. Int Orthod. 2012;10:198–210. doi: 10.1016/j.ortho.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 155.Afify AR, Zawawi KH. The prevalence of dental anomalies in the Western region of Saudi Arabia. ISRN Dent 2012. 2012 doi: 10.5402/2012/837270. 837270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Ajami BA, Shabzendedar M, Mehrjerdian M. Prevalence of hypodontia in nine-to fourteen-year-old children who attended the Mashhad School of Dentistry. Indian J Dent Res. 2010;21:549–51. doi: 10.4103/0970-9290.74215. [DOI] [PubMed] [Google Scholar]
- 157.Khosravanifard B, Rakhshan V, Raeesi E. Factors influencing attractiveness of soft tissue profile. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:29–37. doi: 10.1016/j.oooo.2012.03.021. [DOI] [PubMed] [Google Scholar]
- 158.Esenlik E, Sayin MO, Atilla AO, Ozen T, Altun C, Başak F. Supernumerary teeth in a Turkish population. Am J Orthod Dentofacial Orthop. 2009;136:848–52. doi: 10.1016/j.ajodo.2007.10.055. [DOI] [PubMed] [Google Scholar]
- 159.Amini F, Rakhshan V, Jamalzadeh S. Prevalence and pattern of accessory teeth (hyperdontia) in permanent dentition of Iranian orthodontic patients. Iran J Public Health. 2013;42:1259–65. [PMC free article] [PubMed] [Google Scholar]
- 160.Brook AH. A unifying aetiological explanation for anomalies of human tooth number and size. Arch Oral Biol. 1984;29:373–8. doi: 10.1016/0003-9969(84)90163-8. [DOI] [PubMed] [Google Scholar]
- 161.Silverman NE, Ackerman JL. Oligodontia: A study of its prevalence and variation in 4032 children. ASDC J Dent Child. 1979;46:470–7. [PubMed] [Google Scholar]
- 162.Jorgenson RJ. Clinician's view of hypodontia. J Am Dent Assoc. 1980;101:283–6. doi: 10.14219/jada.archive.1980.0186. [DOI] [PubMed] [Google Scholar]
- 163.Mattheeuws N, Dermaut L, Martens G. Has hypodontia increased in Caucasians during the 20th century? A meta-analysis. Eur J Orthod. 2004;26:99–103. doi: 10.1093/ejo/26.1.99. [DOI] [PubMed] [Google Scholar]
- 164.Zhu JF, Marcushamer M, King DL, Henry RJ. Supernumerary and congenitally absent teeth: A literature review. J Clin Pediatr Dent. 1996;20:87–95. [PubMed] [Google Scholar]
- 165.Gungor AY, Turkkahraman H. Tooth sizes in nonsyndromic hypodontia patients. Angle Orthod. 2013;83:16–21. doi: 10.2319/011112-23.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Kan WY, Seow WK, Holcombe T. Taurodontism in children with hypodontia and supernumerary teeth: A case control study. Pediatr Dent. 2010;32:134–40. [PubMed] [Google Scholar]
- 167.Alvesalo L, Portin P. The inheritance pattern of missing, peg-shaped, and strongly mesio-distally reduced upper lateral incisors. Acta Odontol Scand. 1969;27:563–75. doi: 10.3109/00016356909026309. [DOI] [PubMed] [Google Scholar]
- 168.Woodworth DA, Sinclair PM, Alexander RG. Bilateral congenital absence of maxillary lateral incisors: A craniofacial and dental cast analysis. Am J Orthod. 1985;87:280–93. doi: 10.1016/0002-9416(85)90003-x. [DOI] [PubMed] [Google Scholar]
- 169.Chung LK, Hobson RS, Nunn JH, Gordon PH, Carter NE. An analysis of the skeletal relationships in a group of young people with hypodontia. J Orthod. 2000;27:315–8. doi: 10.1093/ortho/27.4.315. [DOI] [PubMed] [Google Scholar]
- 170.Acharya PN, Jones SP, Moles D, Gill D, Hunt NP. A cephalometric study to investigate the skeletal relationships in patients with increasing severity of hypodontia. Angle Orthod. 2010;80:511–8. doi: 10.2319/072309-411.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Ogaard B, Krogstad O. Craniofacial structure and soft tissue profile in patients with severe hypodontia. Am J Orthod Dentofacial Orthop. 1995;108:472–7. doi: 10.1016/s0889-5406(95)70047-1. [DOI] [PubMed] [Google Scholar]
- 172.Medina AC. Radiographic study of prevalence and distribution of hypodontia in a pediatric orthodontic population in Venezuela. Pediatr Dent. 2012;34:113–6. [PubMed] [Google Scholar]
- 173.Ringqvist M, Thilander B. The frequency of hypodontia in an orthodontic material. Sven Tandlak Tidskr. 1969;62:535–41. [PubMed] [Google Scholar]
- 174.Schalk-van der Weide Y, Beemer FA, Faber JA, Bosman F. Symptomatology of patients with oligodontia. J Oral Rehabil. 1994;21:247–61. doi: 10.1111/j.1365-2842.1994.tb01141.x. [DOI] [PubMed] [Google Scholar]
- 175.Kirzioğlu Z, Köseler Sentut T, Ozay Ertürk MS, Karayilmaz H. Clinical features of hypodontia and associated dental anomalies: A retrospective study. Oral Dis. 2005;11:399–404. doi: 10.1111/j.1601-0825.2005.01138.x. [DOI] [PubMed] [Google Scholar]
- 176.Kositbowornchai S. Prevalence and distribution of dental anomalies in pretreatment orthodontic Thai patients. Khon Kaen Univ Dent J. 2011;13:92–100. [Google Scholar]
- 177.Al-Ajwadi SA. An orthopantomographic study of hypodontia in permanent teeth of Iraqi patients. Med Dent J. 2009;6:139–4. [Google Scholar]
- 178.Wong AT, McMillan AS, McGrath C. Oral health-related quality of life and severe hypodontia. J Oral Rehabil. 2006;33:869–73. doi: 10.1111/j.1365-2842.2006.01654.x. [DOI] [PubMed] [Google Scholar]
- 179.Behr M, Driemel O, Mertins V, Gerlach T, Kolbeck C, Rohr N, et al. Concepts for the treatment of adolescent patients with missing permanent teeth. Oral Maxillofac Surg. 2008;12:49–60. doi: 10.1007/s10006-008-0109-5. [DOI] [PubMed] [Google Scholar]
- 180.Tuverson DL. Anterior interocclusal relations. Part II. Am J Orthod. 1980;78:371–93. doi: 10.1016/0002-9416(80)90019-6. [DOI] [PubMed] [Google Scholar]
- 181.Tuverson DL. Anterior interocclusal relations. Part I. Am J Orthod. 1980;78:361–70. doi: 10.1016/0002-9416(80)90018-4. [DOI] [PubMed] [Google Scholar]
- 182.Jacobs SG. The impacted maxillary canine. Further observations on aetiology, radiographic localization, prevention/interception of impaction, and when to suspect impaction. Aust Dent J. 1996;41:310–6. doi: 10.1111/j.1834-7819.1996.tb03139.x. [DOI] [PubMed] [Google Scholar]
- 183.Isler SL. Smile-maxilla, maxilla in the mouth, and other interdisciplinary design guidelines: Helpful hints for the esthetic dental team. Alpha Omegan. 2000;93:26–33. [PubMed] [Google Scholar]
- 184.Bauss O, Sadat-Khonsari R, Engelke W, Kahl-Nieke B. Results of transplanting developing third molars as part of orthodontic space management. Part 1: Clinical and radiographic results. J Orofac Orthop. 2002;63:483–92. doi: 10.1007/s00056-002-0131-4. [DOI] [PubMed] [Google Scholar]
- 185.Chung KR, Cho JH, Kim SH, Kook YA, Cozzani M. Unusual extraction treatment in Class II division 1 using C-orthodontic mini-implants. Angle Orthod. 2007;77:155–66. doi: 10.2319/020106-35R.1. [DOI] [PubMed] [Google Scholar]
- 186.Nordquist GG, McNeill RW. Orthodontic vs. restorative treatment of the congenitally absent lateral incisor — Long term periodontal and occlusal evaluation. J Periodontol. 1975;46:139–43. doi: 10.1902/jop.1975.46.3.139. [DOI] [PubMed] [Google Scholar]
- 187.Robertsson S, Mohlin B. The congenitally missing upper lateral incisor. A retrospective study of orthodontic space closure versus restorative treatment. Eur J Orthod. 2000;22:697–710. doi: 10.1093/ejo/22.6.697. [DOI] [PubMed] [Google Scholar]
- 188.Rosa M, Zachrisson BU. Integrating esthetic dentistry and space closure in patients with missing maxillary lateral incisors. J Clin Orthod. 2001;35:221–34. [PubMed] [Google Scholar]
- 189.Hobkirk JA, Goodman JR, Jones SP. Presenting complaints and findings in a group of patients attending a hypodontia clinic. Br Dent J. 1994;177:337–9. doi: 10.1038/sj.bdj.4808606. [DOI] [PubMed] [Google Scholar]
- 190.Kristerson L, Lagerström L. Autotransplantation of teeth in cases with agenesis or traumatic loss of maxillary incisors. Eur J Orthod. 1991;13:486–92. doi: 10.1093/ejo/13.6.486. [DOI] [PubMed] [Google Scholar]
- 191.Botelho MG, Nor LC, Kwong HW, Kuen BS. Two-unit cantilevered resin-bonded fixed partial dentures - A retrospective, preliminary clinical investigation. Int J Prosthodont. 2000;13:25–8. [PubMed] [Google Scholar]


