Abstract
Background:
Impaired quality of life (QOL) is an issue considered in patients with multiple sclerosis (MS). There are limited studies evaluated poor sleep and impaired QOL in these cases. The aim of this study was to evaluate quality of sleep and poor sleep in Iranian patients with MS and the relationship between Pittsburgh Sleep Quality Index (PSQI) score and QOL subscales.
Methods:
One-hundred and fourteen cases with definite MS due to MC Donald criteria enrolled who referred to MS clinic of Sina and Imam Hospitals were enrolled. Patients asked to fill valid and reliable Persian versions of PSQI and MSQOL-54 questionnaires. Demographic data (sex, age), duration of the disease, education level and marital status were extracted from patients medical files. After neurological examination, Kurtzke Expanded Disability Status Scale (EDSS) was assessed.
Results:
Ninety-one (79.8%) patients were female and 23 (20.2%) were male. Mean age and EDSS was 34.7 ± 9.6 years and 2.3 (median: 1.5). Mean PSQI score and overall QOL score were 4.5 and 57. Sixty-seven cases were good sleepers (PSQI ≤ 5) and 47 were poor sleepers (PSQI > 5). Except five subscales, all others were significantly different between good and poor sleepers. There was significant positive correlation between PSQI score and EDSS (r = 0.24, P < 0.001) and negative correlation between EDSS and physical and mental health (r = −0.48, P < 0.001, r = −0.43, P < 0.001). EDSS and total PSQI score were independent predictors of physical and mental health composites.
Conclusions:
Sleep quality as a factor which affecting QOL should be considered and evaluated properly in MS patients.
Keywords: Multiple sclerosis, quality of life, sleep quality
INTRODUCTION
Multiple sclerosis (MS) is a disabling, auto immune disease which affects central nervous system.[1] MS will cause physical and emotional difficulties for affected cases.[2,3] Most patients with MS complain from psychological problems such as poor sleep. The exact cause of poor sleep is not determined in MS, but pain, fatigue, depression and immunotherapy have been considered as potential factors, which could have role in sleep disturbances among MS patients.[4,5]
Health related quality of life (QOL) is assessment of individual's perception of function and health beyond the current situation. Until now, different studies evaluated QOL in MS patients and reported lower QOL scores than healthy ones.[6,7,8]
Depression, level of disability, need for support had been considered as the factors related with poor QOL while higher level of education and higher income were related with better QOL.[6,9,10,11,12]
By means of self-reported questionnaires, poor sleep was associated with lower health related QOL in MS.[13,14]
In a previous study Ghaem and Haghighi reported poor sleep in 87% of Iranian MS patients and found that Pittsburgh Sleep Quality Index (PSQI) was significantly negatively correlated with items of QOL questionnaire.[12]
As there are limited studies evaluating quality of sleep and QOL in MS cases simultaneously, we designed this study to evaluate QOL and poor sleep in Iranian patients with MS and the relationship between PSQI score and QOL subscales.
METHODS
In this cross sectional study, which conducted in MS clinic of Sina and Imam Hospitals (affiliated hospitals of Tehran University of Medical Sciences), 114 cases with definite MS due to MC Donald criteria (consecutive cases) enrolled.
Patients who were under treatment with antidepressant agents and who had attack during the previous month were excluded.
All cases were asked to fill informed consent form before study entrance.
Demographic data (sex, age), duration of the disease, education level, and marital status were extracted from patients medical files.
After neurological examination, Kurtzke Expanded Disability Status Scale (EDSS) was assessed.
Patients asked to fill valid and reliable Persian versions of PSQI and MSQOL-54 questionnaires.
Pittsburg Sleep Questionnaire, a self-administrative instrument, consists of nine questions generating seven-component scores (sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction). Each component score ranged from 0 to 3 (0, not in the past month; 1, less than once per week; 2, once or twice per week; and 3, 3 or more times/week). A valid and reliable Persian version of this test was applied for assessing the quality of sleep in current survey. The total score ranges from 0 to 21 while higher scores indicates poorer sleep quality; a total score ≥ 5 indicates a “poor” sleeper. Valid and reliable Persian version administered.[15]
Multiple sclerosis QOL-54 is a structured, self-report questionnaire containing 14 sub scales (physical function, role limitations-physical, role limitations-emotional, pain, emotional well-being, energy, health perceptions, social function, cognitive function, health distress, overall QOL, and sexual function, satisfaction with sexual function and change in health.[16]
Sum of subtotals; physical function, health perceptions, energy/fatigue, role limitation-physical, pain, sexual function, social function, health distress makes the physical health composite and sum of subtotals; health distress, overall QOL, emotional well-being, role limitation-emotional, cognitive function makes the mental health composite. The higher the scores, the better QOL.[16]
All data were analyzed using SPSS software version 18.0 (SPSS Inc., Chicago, IL, USA).
Student's t-test and Fisher's exact tests were used to compare continuous and categorical variables. Correlation coefficient calculated to assess association between variables. Multiple linear regression analysis was conducted by considering mental, and physical health and PSQI score as dependent variable and age, sex EDSS and PSQI score as independent variables.
P < 0.05 was considered to be significant.
RESULTS
One-hundred and fourteen MS cases were participated in this study. Of which ninety-one (79.8%) were female, and 23 (20.2%) were male. Mean age and EDSS was 34.7 ± 9.6 years and 2.3 (median: 1.5). Seventy-six were married and remaining were single. Four patients were uneducated, 25 had primary school education, and 85 had educated in university [Table 1].
Table 1.
Mean scores of PSQI and subscales of quality of life questionnaire in all cases

Sixty-seven cases were good sleepers (PSQI ≤ 5) and 47 were poor sleepers (PSQI > 5). Except five subscales, all others were significantly different between good and poor sleepers [Table 2].
Table 2.
comparison of subscales of QOL questionnaire in cases with good and poor sleep

There was a significant correlation between total PSQI score and most subscales of QOL score [Table 3].
Table 3.
Correlation coefficient between total PSQI score and subscales of QOL questionnaire

There was significant positive correlation between PSQI score and EDSS (r = 0.24, P < 0.001) and negative correlation between EDSS and physical and mental health (r = 0.48, P < 0.001, r = 0.43, P < 0.001).
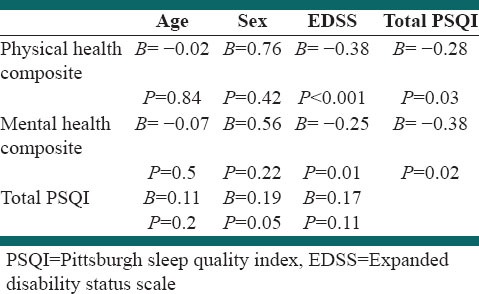
Expanded Disability Status Scale and total PSQI score were independent predictors of physical and mental health composites [Table 4].
Table 4.
Predictors of mental and physical composites and total PSQI score
DISCUSSION
The result of the the current study showed that most subscales of QOL questionnaire were significantly different between MS patients who were good and poor sleepers. We also found that EDSS and total PSQI score were independent predictors of physical and mental health composites.
The results demonstrated significant positive correlation between PSQI score and EDSS and negative correlation between EDSS and physical and mental health composites. The results are compatible with Ghaem and Haghighi findings.[12]
In their study, significant negative correlation reported between EDSS and physical and mental scores and significant negative correlation between physical and mental scores and PSQI score. Against their results, we investigated significant correlation between EDSS and PSQI score while they reported no significant correlation between EDSS and PSQI score (r = 0.1, P = 0.1).[12] In another study, Merkelbach et al. reported significant correlation between physical aspects of QOL questionnaire and EDSS while no correlation between EDSS and mental part of QOL questionnaire was detected.[17]
These findings could show that higher disability due to disease is correlated with poorer sleep in patients with MS, whereas better mental and physical health are related with better sleep quality.
On the other hand regression analysis showed that EDSS and total PSQI score were independent predictors of both physical and mental health composites. In Ghaem and Haghighi study, PSQI, EDSS, and fatigue scores were predictors of physical score of QOL not mental part of QOL score.[12] Lobentanz et al. assessed QOL in 504 patients with MS. They reported that depressive mood score was predictor of all domains of QOL score while EDSS, PSQI and FSS scores were only predictive for physical domain[13] while in this study both EDSS and PSQI score were predictors of both mental and physical aspects of QOL score.
In recent years, assessment of health related QOL in cases with MS has been considered which provides information regarding the individual's perception of function and health.[6] Literature showed that higher levels of disability, depression and need for support services were related with reduced QOL in MS patients.[6,9,11] The result of our study demonstrated that sleep quality could be another factor affecting QOL in MS cases.
Nocturia, pain, spasm and restless leg syndrome are among common causes of sleep problems in MS cases.[2] These could affect sleep quality. In this study mean PSQI score was 4.5 ± 3.5 in all cases while in our previous study mean PSQI score of 100 cases with MS was 8.4. In the current survey, 58% were good sleepers. In Bøe Lunde et al. study, mean PSQI score of MS patients was 8.6 and 43% were good sleepers.[5]
Previous studies confirmed poor sleep in near 50% of MS patients.[18,19]
Psychological problems especially depression, are common in MS patients and have bidirectional effect on sleep in affected cases. Depression worsens insomnia and insomnia could worsen depression.[20,21] Poor sleep is also related with excessive daytime sleepiness and fatigue,[22] all could affect QOL in MS patients.
Multiple sclerosis is an autoimmune disease affecting both physical and mental aspect of patients's lives. Fatigue, depression, physical disability, cognitive, emotional, and psychological problems are factors contribute to their QOL.[23] QOL assessment has been considered important to assess disease progression, treatment and the management of care in MS patients.[24,25] Along with other factors, as this study suggests, sleep quality should be evaluated in MS cases.
This study had some limitations. First, we excluded cases who were under treatment with antidepressant agent. Second, we did not refer cases with sleep impairment for polysomnography. More studies with larger sample size, multi centric design are recommended.
CONCLUSIONS
Sleep quality as a factor, which affecting QOL should be considered and evaluated properly in MS patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ghajarzadeh M, Jalilian R, Eskandari G, Ali Sahraian M, Reza Azimi A. Validity and reliability of Persian version of Modified Fatigue Impact Scale (MFIS) questionnaire in Iranian patients with multiple sclerosis. Disabil Rehabil. 2012;35:1–4. doi: 10.3109/09638288.2012.742575. [DOI] [PubMed] [Google Scholar]
- 2.Ghajarzadeh M, Sahraian MA, Fateh R, Daneshmand A. Fatigue, depression and sleep disturbances in Iranian patients with multiple sclerosis. Acta Med Iran. 2012;50:244–9. [PubMed] [Google Scholar]
- 3.Ghajarzadeh M, Jalilian R, Eskandari G, Sahraian MA, Azimi A, Mohammadifar M. Fatigue in multiple sclerosis: Relationship with disease duration, physical disability, disease pattern, age and sex. Acta Neurol Belg. 2013;113:411–4. doi: 10.1007/s13760-013-0198-2. [DOI] [PubMed] [Google Scholar]
- 4.Brass SD, Duquette P, Proulx-Therrien J, Auerbach S. Sleep disorders in patients with multiple sclerosis. Sleep Med Rev. 2010;14:121–9. doi: 10.1016/j.smrv.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 5.Bøe Lunde HM, Aae TF, Indrevåg W, Aarseth J, Bjorvatn B, Myhr KM, et al. Poor sleep in patients with multiple sclerosis. PLoS One. 2012;7:e49996. doi: 10.1371/journal.pone.0049996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hopman WM, Coo H, Edgar CM, McBride EV, Day AG, Brunet DG. Factors associated with health-related quality of life in multiple sclerosis. Can J Neurol Sci. 2007;34:160–6. doi: 10.1017/s0317167100005989. [DOI] [PubMed] [Google Scholar]
- 7.Grima DT, Torrance GW, Francis G, Rice G, Rosner AJ, Lafortune L. Cost and health related quality of life consequences of multiple sclerosis. Mult Scler. 2000;6:91–8. doi: 10.1177/135245850000600207. [DOI] [PubMed] [Google Scholar]
- 8.Aronson KJ. Quality of life among persons with multiple sclerosis and their caregivers. Neurology. 1997;48:74–80. doi: 10.1212/wnl.48.1.74. [DOI] [PubMed] [Google Scholar]
- 9.Pittock SJ, Mayr WT, McClelland RL, Jorgensen NW, Weigand SD, Noseworthy JH, et al. Quality of life is favorable for most patients with multiple sclerosis: A population-based cohort study. Arch Neurol. 2004;61:679–86. doi: 10.1001/archneur.61.5.679. [DOI] [PubMed] [Google Scholar]
- 10.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS) Neurology. 1983;33:1444–52. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 11.Wallin MT, Wilken JA, Turner AP, Williams RM, Kane R. Depression and multiple sclerosis: Review of a lethal combination. J Rehabil Res Dev. 2006;43:45–62. doi: 10.1682/jrrd.2004.09.0117. [DOI] [PubMed] [Google Scholar]
- 12.Ghaem H, Haghighi AB. The impact of disability, fatigue and sleep quality on the quality of life in multiple sclerosis. Ann Indian Acad Neurol. 2008;11:236–41. doi: 10.4103/0972-2327.44559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lobentanz IS, Asenbaum S, Vass K, Sauter C, Klösch G, Kollegger H, et al. Factors influencing quality of life in multiple sclerosis patients: Disability, depressive mood, fatigue and sleep quality. Acta Neurol Scand. 2004;110:6–13. doi: 10.1111/j.1600-0404.2004.00257.x. [DOI] [PubMed] [Google Scholar]
- 14.Merlino G, Fratticci L, Lenchig C, Valente M, Cargnelutti D, Picello M, et al. Prevalence of ‘poor sleep’ among patients with multiple sclerosis: An independent predictor of mental and physical status. Sleep Med. 2009;10:26–34. doi: 10.1016/j.sleep.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 15.Farrahi Moghaddam J, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A. Reliability and validity of the Persian version of the Pittsburgh Sleep Quality Index (PSQI-P) Sleep Breath. 2012;16:79–82. doi: 10.1007/s11325-010-0478-5. [DOI] [PubMed] [Google Scholar]
- 16.Ghaem H, Haghighi AB, Jafari P, Nikseresht AR. Validity and reliability of the Persian version of the multiple sclerosis quality of life questionnaire. Neurol India. 2007;55:369–75. doi: 10.4103/0028-3886.33316. [DOI] [PubMed] [Google Scholar]
- 17.Merkelbach S, Sittinger H, Koenig J. Is there a differential impact of fatigue and physical disability on quality of life in multiple sclerosis? J Nerv Ment Dis. 2002;190:388–93. doi: 10.1097/00005053-200206000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Tachibana N, Howard RS, Hirsch NP, Miller DH, Moseley IF, Fish D. Sleep problems in multiple sclerosis. Eur Neurol. 1994;34:320–3. doi: 10.1159/000117070. [DOI] [PubMed] [Google Scholar]
- 19.Bamer AM, Johnson KL, Amtmann D, Kraft GH. Prevalence of sleep problems in individuals with multiple sclerosis. Mult Scler. 2008;14:1127–30. doi: 10.1177/1352458508092807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paparrigopoulos T, Ferentinos P, Kouzoupis A, Koutsis G, Papadimitriou GN. The neuropsychiatry of multiple sclerosis: Focus on disorders of mood, affect and behaviour. Int Rev Psychiatry. 2010;22:14–21. doi: 10.3109/09540261003589323. [DOI] [PubMed] [Google Scholar]
- 21.Riemann D, Berger M, Voderholzer U. Sleep and depression – Results from psychobiological studies: An overview. Biol Psychol. 2001;57:67–103. doi: 10.1016/s0301-0511(01)00090-4. [DOI] [PubMed] [Google Scholar]
- 22.Frauscher B, Egg R, Brandauer E, Ulmer H, Berger T, Poewe W, et al. Daytime sleepiness is not increased in mild to moderate multiple sclerosis: A pupillographic study. Sleep Med. 2005;6:543–7. doi: 10.1016/j.sleep.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 23.Noble JG, Osborne LA, Jones KH, Middleton RM, Ford DV. Commentary on ‘disability outcome measures in multiple sclerosis clinical trials’. Mult Scler. 2012;18:1718–20. doi: 10.1177/1352458512457847. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell AJ, Benito-León J, González JM, Rivera-Navarro J. Quality of life and its assessment in multiple sclerosis: Integrating physical and psychological components of wellbeing. Lancet Neurol. 2005;4:556–66. doi: 10.1016/S1474-4422(05)70166-6. [DOI] [PubMed] [Google Scholar]
- 25.Solari A. Role of health-related quality of life measures in the routine care of people with multiple sclerosis. Health Qual Life Outcomes. 2005;3:16. doi: 10.1186/1477-7525-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]


