Abstract
Background:
India is currently suffering from an epidemic of noncommunicable diseases; it is thus imperative to screen for cardiovascular risk factors in people visiting Primary Health Centers (PHCs). The objective of the study was to measure the amount of undiagnosed hypertension and selected cardiovascular risk factors present among the adult population through opportunistic screening at the PHC.
Methods:
A facility-based opportunistic screening program was carried out in a PHC in rural Puducherry. Patients and accompanying persons aged 30 years and above, who attended the daily outpatient department (OPD) were included. The OPD provides outpatient services and medical procedures or tests without requirement of an overnight stay, and functions for 4 h a day. Known hypertensive patients and pregnant women were excluded. Information on age, gender, diabetes status, and personal history of tobacco and alcohol use were collected using an interview schedule. Height, weight and waist circumference were measured, along with blood pressure and blood sugar using standard protocols. Systolic blood pressure (SBP) ≥140 and/or diastolic blood pressure (DBP) ≥90 mm Hg was taken as hypertension. SBP of 120-139 mm Hg and/or DBP of 80-89 mm Hg were taken as prehypertension.
Results:
A total of 324 participants were screened; 56.8% were females. The mean standard deviation (SD) age of the participants was 47.7 (SD 12.6) years. Hypertension and prehypertension were present in 17.9% and 37.7% of the participants respectively. 17.3% participants had diabetes. 22.2% and 21.3% of all participants were current users of tobacco and alcohol respectively. Generalized obesity was present in 31.8% of the participants; 19.1% were overweight. 45.1% participants had central obesity.
Conclusions:
A relatively large proportion of adults were found to have prehypertension and obesity, thus showing the need for early intervention.
Keywords: Cardiovascular, hypertension, opportunistic, risk, screening
INTRODUCTION
The major risk factors for rising trends of non-communicable diseases (NCDs) (heart disease, stroke, diabetes mellitus, cancer, and chronic respiratory diseases) in the Asian regions, include tobacco and alcohol consumption, unhealthy diet, physical inactivity, and high blood pressure (BP).[1] Hypertension is an established major risk factor underlying the epidemic of cardiovascular diseases.[2] In India, over the past three decades, the prevalence of adult hypertension has risen dramatically from 5% to between 20-40% in urban areas and 12-17% in rural areas.[3] Hypertension is also estimated to be attributable for nearly 10% of all deaths, which constitute 57% deaths due to stroke, and 24% deaths due to coronary heart disease.[3,4]
There is a paucity of literature regarding opportunistic screening of hypertension and associated cardiovascular risk factors from rural India. As per the guidelines issued by the National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular disease and Stroke, opportunistic screening for hypertension and diabetes in ≥30 years of age is to be done by the health workers at the subcenter level (the most peripheral health center) and referred to the Community Health Centre (CHC), if required. These guidelines exclude PHCs, which lie in between subcenters and CHCs in the usual chain of care. Also, there are no available guidelines for screening of NCD risk factors at the primary care level. We wanted to explore the feasibility and usefulness of screening for NCD risk factors at the level of PHC, which is the most peripheral health institution with a qualified doctor. The present study was thus undertaken to measure the amount of undiagnosed hypertension and selected cardiovascular risk factors present among the adult population through opportunistic screening at the PHC.
METHODS
The present study was a hospital-based cross-sectional study carried out in a PHC located at Ramanathapuram in rural Puducherry. It caters to a population of 9,101 distributed among four villages. Average OPD attendance is around 50 patients/day.
Nonpregnant adult persons (adult patients and accompanying persons) aged 30 years and above, who attended the daily out-patient clinic during September 2013 were included. Known hypertensives (having documented evidence or taking regular treatment) were excluded. Using the formula 4pq/d2, taking P = 22.2% (proportion of people diagnosed to have hypertension in a previous screening program[5]), 5% absolute precision, and a nonresponse rate of 10%, the final sample size calculated was 305.
A pretested semi-structured interview schedule was used to collect data regarding age, gender and personal history of tobacco and alcohol use. Height, weight, waist circumference, BP and random blood sugar (RBS) was measured. Participants having RBS ≥ 140 mg/dl were instructed to come back the next day for fasting blood sugar (FBS) and 2 h postprandial blood sugar (PPBS). Informed written consent was taken from all participants. For newly diagnosed cases of hypertension and diabetes, necessary follow-up care and advice was provided.
Height, weight and waist circumference were measured as per the standard criteria.[6] SECA machine was used to measure the height and weight. Height was recorded to the nearest 0.1 cm and weight to the nearest 0.1 kg. Waist circumference was measured as the smallest horizontal girth between the costal margins and the iliac crests at minimal respiration. Two BP readings were taken for each individual by auscultatory method using a mercury sphygmomanometer at an interval of 5 min, and the average was calculated. Glucometer (Freestyle, Optimum H) was used for measuring RBS. FBS and 2 h PPBS were tested using auto analyzer.
The Joint National Committee 7 criterion was used to classify hypertension. Those who had systolic blood pressure (SBP) ≥140 and or diastolic blood pressure (DBP) ≥90 mmHg were diagnosed to have hypertension. SBP of 120-139 mm Hg and or DBP of 80-89 mm Hg were labeled as prehypertensive. Normal BP was taken as SBP < 120 and DBP < 80 mm Hg. Indian Council of Medical Research (ICMR) criteria were used to diagnose diabetes; FBS ≥ 126 mg/dl and/or 2 h PPBS ≥ 200 mg/dl.
Any history of tobacco (in any form) or alcohol use within the last 1-month was taken as current use. Generalized obesity was defined using the new Asia Pacific guidelines for obesity using body mass index values that is, underweight (<18.5 kg/m2), normal (18.5-22.99 kg/m2), overweight (23-24.99 kg/m2) and obese (≥25 kg/m2). Central obesity was defined as having a waist circumference ≥90 cm for men and ≥80 cm for women.
Data were entered in EpiData version 3.1 [The EpiData Association, Odense, Denmark] and was analyzed using SPSS version 17.0 [SPSS Inc., Chicago].
RESULTS
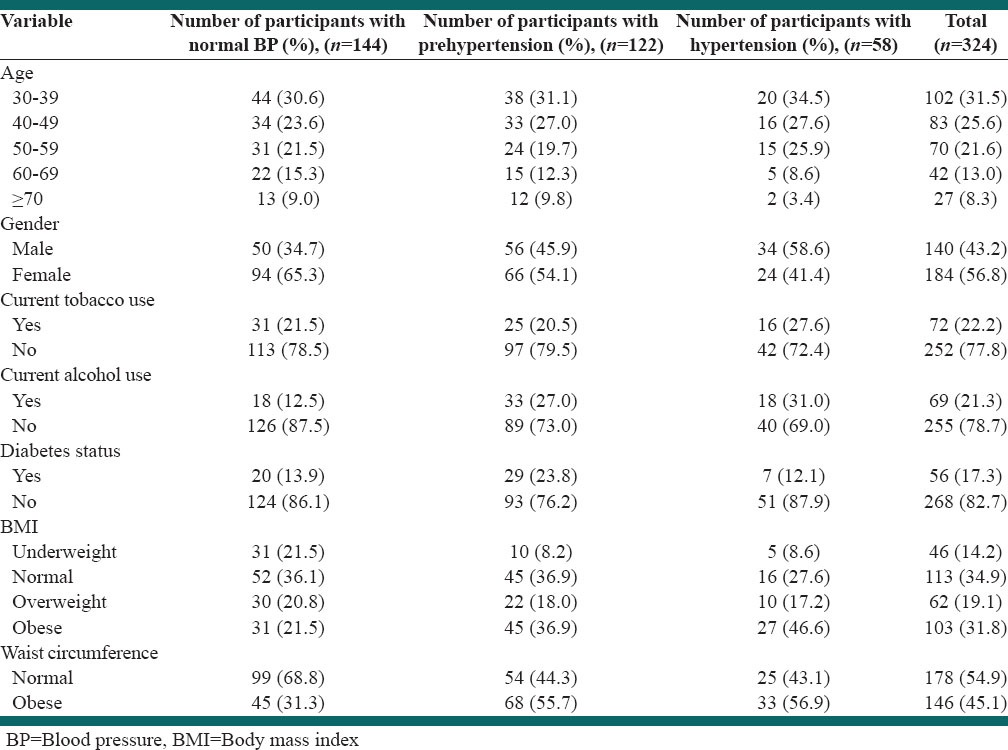
A total of 324 participants were screened. Six patients had established cardiovascular disease, and all of them had previously diagnosed hypertension, hence were excluded from the study. The majority (56.8%) were female [Table 1] and the majority of individuals (31.5%) were in 30-39 years age group. Newly diagnosed hypertension, prehypertension and those having normal BP were 17.9% (58/324), 37.7% (122/324) and 44.4% (144/324) respectively [Table 2]. Over one fifth of all participants were currently using tobacco and alcohol. There were a total 56 cases of diabetes. Central obesity was present in 56.9% and 55.7% of hypertensive and prehypertensive participants respectively. A much lesser number of normotensive participants (31.3%) had central obesity.
Table 1.
Age and gender distribution of the study participants screened for hypertension (n=324)
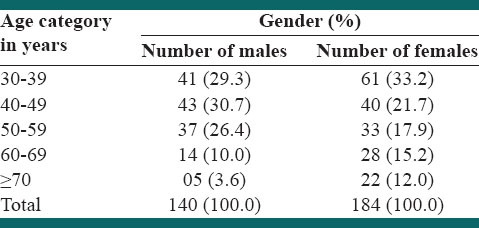
Table 2.
Distribution of age, gender and cardiovascular risk factors among normotensive, prehypertensive and hypertensive participants (n=324)
DISCUSSION
The yield of newly diagnosed hypertension and prehypertension in the present study were only slightly lesser than the Screening India's Twin Epidemic Study conducted among participants ≥18 years of age, with 22.2% patients being newly diagnosed hypertensives and 60.1% having prehypertension.[5] These higher values may be because of the fact that the information was collected from general practitioners, who are generally based in urban areas. Another reason could be a lower age cut-off used for including participants as compared to the present study. As per our knowledge, this is the only large scale muticentric study available in India to date giving an estimate of undiagnosed hypertension through opportunistic screening.
A relatively large community-based survey done by Rao et al. among 1239 respondents aged ≥30 years in rural Karnataka found the prevalence of prehypertension to be 38.7%, with 20.2% being newly detected cases of hypertension.[7] These findings are very similar to our study. This shows that facility-based screening could be a more cost-effective option than community based screening. Cost-effectiveness studies are needed though to prove this.
In some previous studies, increasing age that is, age >40 years was found to be associated with hypertension, but in our study a higher prevalence was seen in 30-39 years age group.[8,9] This could be because of the difference in the population studied and the study design; one study was conducted among laborers and the other was a community based study, whereas the present study was a hospital-based study. Our study results thus demonstrate the importance of opportunistic screening so that the disease is picked up at an earlier age. Two studies showed that the prevalence of hypertension is more among males as compared to females similar to our study.[7,10] Another study showed no gender difference though.[11]
In rural Ballabgarh, prevalence of self-reported daily current tobacco use among males and females aged 15-64 years was 52.6% and 17.7% respectively.[12] In rural Maharashtra, prevalence of tobacco use was found to be 16%, which is similar to our study.[13] In our study, the proportion of tobacco users was higher among hypertensive participants as compared to those with normal BP. In earlier studies, alcohol intake was seen in 9.4% and 11% of the participants respectively, compared to a higher prevalence of 21.3% in the present study.[5,13] This can be explained based on the fact that alcohol is more freely available for sale at a lower price in Puducherry, as compared to Maharashtra as a result of government policies. In a study by Agarwal et al., 18% and 3.2% of participants were overweight and obese respectively.[13] These lower proportions observed can be attributed to the different criteria for BMI used in that study (World Health Organization criteria). In our study, 46.1% hypertensive participants had generalized obesity. Among prehypertensive and normotensive participants, 36.9% and 21.5% had obesity.
The present study is one of the very few studies in India to have tested the feasibility of a facility-based opportunistic screening program for cardiovascular risk factors at the Primary Health Centre level. Most of the studies published earlier had given community-based data from rural areas. One of the limitations was that we did not include all the sociodemographic variables like socioeconomic status, marital status, etc., One reason for doing so was that our main focus was to capture the yield obtained from opportunistic screening.
CONCLUSIONS
Our study showed that the yield of undiagnosed hypertension and prehypertension through facility-based opportunistic screening in rural Puducherry was 17.9% and 37.7% respectively. Majority of the undiagnosed hypertension was detected in the most productive years of life, that is, 30-49 year age group, and in males, who are usually the breadwinners. Proportions of generalized and central obesity were high, that is, 31.8% and 45.1% respectively. As a relatively large number of adults were found to have prehypertension, and because obesity is a modifiable risk factor, there is a scope for early intervention.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ahmed SM, Hadi A, Razzaque A, Ashraf A, Juvekar S, Ng N, et al. Clustering of chronic non-communicable disease risk factors among selected Asian populations: Levels and determinants. Glob Health Action. 2009:2. doi: 10.3402/gha.v2i0.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fuentes R, Ilmaniemi N, Laurikainen E, Tuomilehto J, Nissinen A. Hypertension in developing economies: A review of population-based studies carried out from 1980 to 1998. J Hypertens. 2000;18:521–9. doi: 10.1097/00004872-200018050-00003. [DOI] [PubMed] [Google Scholar]
- 3.Mohan S, Campbell N, Chockalingam A. Time to effectively address hypertension in India. Indian J Med Res. 2013;137:627–31. [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens. 2004;18:73–8. doi: 10.1038/sj.jhh.1001633. [DOI] [PubMed] [Google Scholar]
- 5.Joshi SR, Saboo B, Vadivale M, Dani SI, Mithal A, Kaul U, et al. Prevalence of diagnosed and undiagnosed diabetes and hypertension in India – Results from the Screening India's Twin Epidemic (SITE) study. Diabetes Technol Ther. 2012;14:8–15. doi: 10.1089/dia.2011.0243. [DOI] [PubMed] [Google Scholar]
- 6.Somannavar S, Ganesan A, Deepa M, Datta M, Mohan V. Random capillary blood glucose cut points for diabetes and pre-diabetes derived from community-based opportunistic screening in India. Diabetes Care. 2009;32:641–3. doi: 10.2337/dc08-0403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rao CR, Kamath VG, Shetty A, Kamath A. High Blood pressure prevalence and significant correlates: A quantitative analysis from coastal Karnataka, India. ISRN Preventive Medicine. 2012. Dec 3, [Last cited on 2014 Apr 02]. Available from: http://www.hindawi.com/journals/isrn.preventive.medicine/2013/574973/abs . [DOI] [PMC free article] [PubMed]
- 8.Mahmood SE, Srivastava A, Shrotriya VP, Shaifali I, Mishra P. Prevalence and epidemiological correlates of hypertension among labour population. Natl J Community Med. 2011;2:43–8. [Google Scholar]
- 9.Bansal SK, Saxena V, Kandpal SD, Gray WK, Walker RW, Goel D. The prevalence of hypertension and hypertension risk factors in a rural Indian community: A prospective door-to-door study. J Cardiovasc Dis Res. 2012;3:117–23. doi: 10.4103/0975-3583.95365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.By Y, Mr NG, Ag U. Prevalence, awareness, treatment, and control of hypertension in rural areas of davanagere. Indian J Community Med. 2010;35:138–41. doi: 10.4103/0970-0218.62578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vimala A, Ranji SA, Jyosna MT, Chandran V, Mathews SR, Pappachan JM. The prevalence, risk factors and awareness of hypertension in an urban population of Kerala (South India) Saudi J Kidney Dis Transpl. 2009;20:685–9. [PubMed] [Google Scholar]
- 12.Gupta V, Yadav K, Anand K. Patterns of tobacco use across rural, urban, and urban-slum populations in a north Indian community. Indian J Community Med. 2010;35:245–51. doi: 10.4103/0970-0218.66877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agarwal VK, Bhalwar R, Basannar DR. Prevalence and determinants of hypertension in a rural community. Med J Armed Forces India. 2008;64:21–5. doi: 10.1016/S0377-1237(08)80139-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


