Abstract
Epithelioid hemangioendothelioma is a rare neoplasm of vascular origin whose involvement of organs such as lung, spleen, bone, breast and liver has already been reported. The clinical signs and the prognosis of this tumor are quite variable. From the present case report, the authors have sought to contribute with literature data, by reviewing clinical and radiological features which may be useful to include such a condition in the differential diagnosis of liver lesions.
Keywords: Liver, Neoplasms, Epithelioid hemangioendothelioma, Imaging diagnosis, Magnetic resonance imaging
Abstract
O hemangioendotelioma epitelioide é uma neoplasia rara de origem vascular, cujo acometimento de órgãos como o pulmão, o baço, o osso, a mama e o fígado já foi relatado. O quadro clínico e o prognóstico deste tumor são bastante variáveis. A partir de um relato de caso, procuramos contribuir com os dados existentes na literatura, revisando características clínicas e radiológicas que podem ser úteis para inseri-lo no diagnóstico diferencial das lesões hepáticas.
INTRODUCTION
Epithelioid hemangioendothelioma is a rare vascular tumor composed of epithelioid cells and hyalinized fibrotic stroma(1). It is considered as a malignant tumor with low/ intermediate aggressiveness and variable clinical presentation and prognosis(2,3). The authors report a case of involvement of multiple organs incidentally found in an asymptomatic female patient.
CASE REPORT
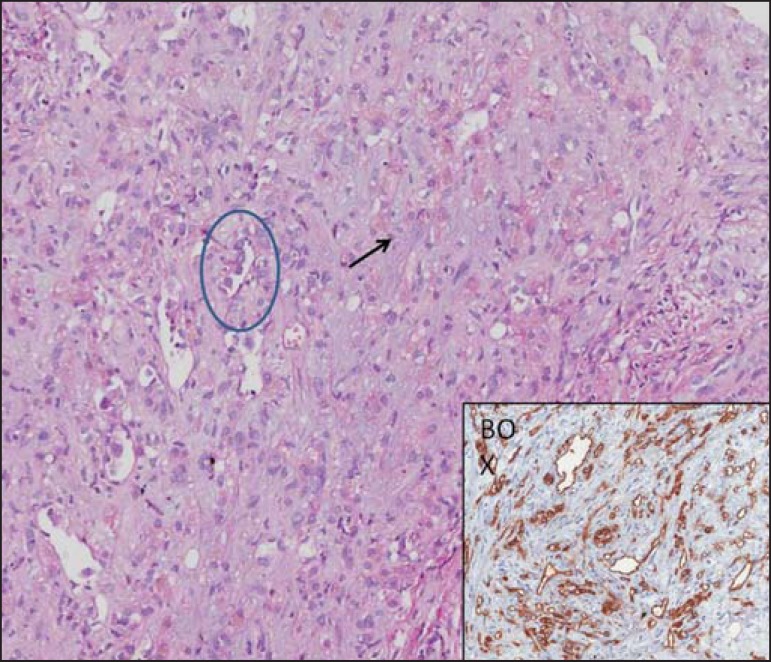
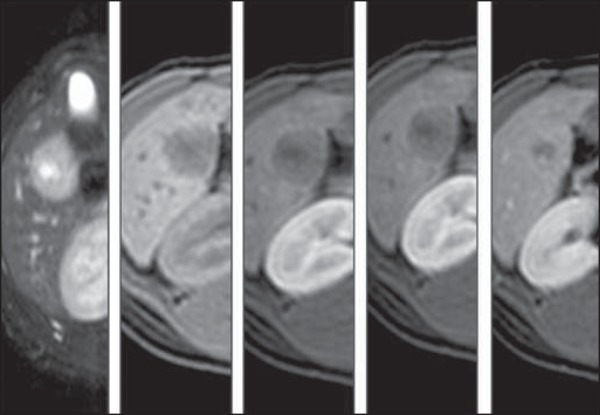
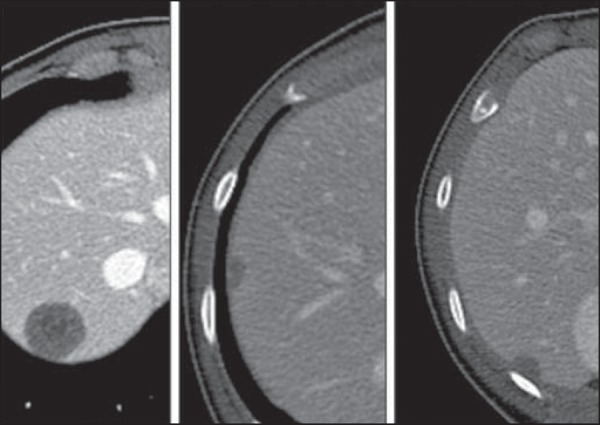
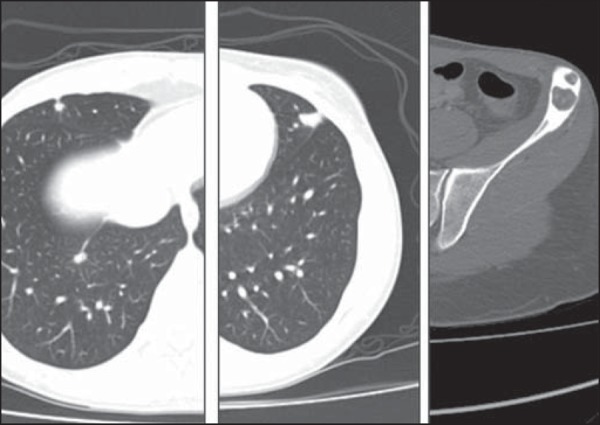
A 28-year-old female patient presented with a hypoechogenic hepatic nodule incidentally found at routine ultrasonography (US). Further investigation with magnetic resonance imaging (MRI) identified other predominantly peripheral hepatic nodules varying in size, with low signal intensity on T1-weighted sequences and intermediate signal intensity on T2-weighted sequences, and a hypovascular, "bull-eye" enhancement pattern (Figure 1). Additionally, other hepatic nodules (Figure 2) as well as pulmonary nodules and lytic lesions in the left iliac bone marrow were characterized at computed tomography (CT) (Figure 3). Tumor markers, colonoscopy and endoscopy were negative for neoplastic lesions. The diagnosis of epithelioid hemangioendothelioma was confirmed by US-guided biopsy whose biopsy slide is illustrated on Figure 4.
Figure 1.
Magnetic resonance imaging (T2 STIR, TIGRE, pre-contrast, arterial, portal and equilibrium phases). Circumscribed nodule located in the periphery of the visceral aspect of the segment IV, with target sign on T2-weighted sequence, low signal intensity on T1-weighet sequence and hypovascular and progressive contrast enhancement. The lesion margins are indistinguishable at the delayed phase.
Figure 2.
Computed tomography. Other peripheral nodules with variable sizes and of smaller dimensions are characterized in the right liver lobe. In the present case, hepatic capsular retraction was not identified.
Figure 3.
Computed tomography. Pulmonary nodules located at the periphery of the costal surface of the middle lobe and in the lingular segment. Lytic bone lesions with marginal sclerosis in the left iliac bone.
Figure 4.
Neoplastic spindle and epithelioid cells infiltrating the sinusoidal structures, residual hepatocytes intermingled with neoplastic cells (arrow). Clusters of neoplastic epithelioid cells (circle). Positive immunohistochemical CD34 in neoplastic cells demonstrated in the right inferior box of the figure.
DISCUSSION
Epithelioid hemangioendothelioma is a tumor of endothelial origin composed eosinophilic, dendritic and inflammatory cells dispersed over a myxomatous or fibrotic stroma(4). Such tumor is immunohistochemically identifiable by the positivity for the factor VIII (FVIII-RAg)(3,4). Macroscopically, the tumor presents as multifocal nodules measuring from 0.5 to 14 cm(2,4). In up to 18% of cases, there is a single nodule measuring on average 5.6 cm(4).
This tumor is most frequently found in women, at a ratio of 1.6:1(4,5). There is an association with estrogens and exposure to vinyl chloride, but the nature of such an association is still to be elucidated(4).
The hepatic involvement may be either nodular or diffuse(2,6,7). The nodular pattern is characterized by the presence of multiple, peripheral and subcapsular lesions varying in size, while the diffuse pattern results from coalescence of nodules, producing a peripheral, infiltrating lobular lesion(1,2,6). Retraction and lobulation of the liver represent typical findings(1,2). The lesions are hypoechogenic at US and hypodense at non-contrast-enhanced CT. At MRI, they demonstrate low signal intensity on T1-weighted, and high/ intermediate signal intensity on T2-weighted sequences, where a target sign with central high signal intensity can be identified. The central portion with low signal intensity may be a result from the presence of hemorrhage, calcification and coagulative necrosis. Both at CT and MRI, the nodules present a hypovascular and peripheral enhancement pattern. A perilesional halo with poor contrast uptake may be identified, corresponding to the avascular region between the nodule and the liver parenchyma(1,2). Calcifications occur in 23% of the lesions(4). In the present case, the nodules presented a target-shaped enhancement, with homogeinization at the delayed contrast phase.
The course of the disease is varied(4,5), with cases where even tumor regression may be observed without any type of treatment(4). Lungs (81%), abdominal lymph nodes (39%), mesenterium and omentum (31%) are the most common sites of metastatic involvement(4,8).
There is a consensus about the option for surgical treatment by means of either nodulectomy (nodular pattern) or liver transplantation (diffuse involvement). Liver transplantation is acceptable even in cases of metastatic disease(3,8), except for the pediatric population(6). Five-year disease-free survival is observed in 43% of patients submitted to liver transplantation, and disease recurrence occurs in 33% of cases(5). In the present case, chemotherapy, interferon and arterial chemoembolization were utilized in the treatment of the patient(5). As the natural history of the disease is considered, it is difficult to evaluate the actual effectiveness of each of the employed therapeutic strategies(4).
In the presence of hepatic and extra-hepatic nodules, one should initially consider a systemic involvement by neoplastic disease that is more common than epithelioid hemangioendothelioma, a rare neoplasm. In the present case, the investigation of the main primary sites (breast, stomach, colon) was negative. In such context, the knowledge about radiological findings of epithelioid hemangioendothelioma was useful to include it in the differential diagnosis. Peripheral hepatic lesions in association with capsular retraction, particularly in young women with no cancer history, constitute signs of suspicion for epithelioid hemangioendothelioma.
Footnotes
Torres LR, Timbó LS, Ribeiro CMF, Galvão Filho MM, Verrastro CGY, D’Ippolito G. Multifocal and metastatic hepatic hemangioendothelioma: case report and literature review. Radiol Bras. 2014 Mai/Jun;47(3):194–196.
Study developed at Hospital São Luiz, at Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), and at Laboratório Fleury - Medicina Diagnóstica, São Paulo, SP, Brazil.
REFERENCES
- 1.Matsui O, Kobayashi S, Gabata T, et al. Fígado: massas hepáticas focais. In: Haaga JH, Dogra VS, Forsting M, editors. TC e RM: uma abordagem do corpo humano completo. 5ª ed. Rio de Janeiro: Elsevier; 2009. pp. 1561–1562. [Google Scholar]
- 2.Araújo ALE. Patologias neoplásicas malignas. In: Araújo ALE, editor. Ressonância magnética do fígado. Rio de Janeiro: Guanabara Koogan; 2006. pp. 300–301. [Google Scholar]
- 3.Santos CER, Correia MM, Pereira RS, et al. Hemangioendotelioma epitelióide hepático: relato de caso com tratamento multimodal. Rev Bras Cancerol. 2007;53:217–222. [Google Scholar]
- 4.Makhlouf HR, Ishak KG, Goodman ZD. Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer. 1999;85:562–582. doi: 10.1002/(sici)1097-0142(19990201)85:3<562::aid-cncr7>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 5.García-Botella A, Díez-Valladares L, Martín-Antona E, et al. Epithelioid hemangioendothelioma of the liver. J Hepatobiliary Pancreat Surg. 2006;13:167–171. doi: 10.1007/s00534-005-1021-0. [DOI] [PubMed] [Google Scholar]
- 6.Da Ines DD, Petitcolin V, Joubert-Zakeyh J, et al. Epithelioid hemangioendothelioma of the liver with metastatic coeliac lymph nodes in an 11-year-old boy. Pediatr Radiol. 2010;40:1293–1296. doi: 10.1007/s00247-009-1532-y. [DOI] [PubMed] [Google Scholar]
- 7.Lyburn ID, Torreggiani WC, Harris AC, et al. Hepatic epithelioid hemangioendothelioma: sonographic, CT, and MR imaging appearances. AJR Am J Roentgenol. 2003;180:1359–1364. doi: 10.2214/ajr.180.5.1801359. [DOI] [PubMed] [Google Scholar]
- 8.Kayler LK, Merion RM, Arenas JD, et al. Epithelioid hemangioendothelioma of the liver disseminated to the peritoneum treated with liver transplantation and interferon alpha-2B. Transplantation. 2002;74:128–130. doi: 10.1097/00007890-200207150-00022. [DOI] [PubMed] [Google Scholar]