Abstract
Background
Minority ethnic groups in the UK have worse outcomes for some cancer types compared with the white majority. Black males have worse staging at diagnosis of prostate cancer and often present as emergencies, suggesting possible delays in the diagnostic pathway. Delay may arise from lower awareness of cancer symptoms, reluctance to report symptoms, reduced desire for investigation, or a combination of these. Reduced desire for investigation was examined in this study
Aim
To investigate whether black males in the UK would choose to be tested for prostate cancer compared with the white majority.
Design and setting
A vignette (hypothetical scenario)-based, electronic survey of male patients aged ≥40 years from four general practices in Bristol, UK.
Method
The vignettes described possible prostate cancer symptoms (equating to risk levels of 2%, 5%, and 10%), investigative procedures, and possible outcomes. Participants indicated whether they would choose investigation in these scenarios. Analysis used logistic regression, with preference for investigation as the outcome variable and ethnicity as the main explanatory variable.
Results
In total, 449 (81%) of 555 participants opted for investigation, regardless of risk levels; of these, the acceptance rate was 94% (251 out of 267) among white males and 70% (198 out of 285) among black males. In multivariable analyses, preference for investigation was lower in black males, even after controlling for relevant confounding factors including specific risk level (odds ratio 0.13; 95% confidence interval = 0.07 to 0.25; P<0.001).
Conclusion
Black males are less likely to opt for investigation at any risk level of prostate cancer compared with white males. This may explain some of their late-stage presentation at diagnosis and subsequent poorer outcomes.
Keywords: ethnic groups, primary health care, prostate cancer
INTRODUCTION
When compared with white males, black males have higher incidence and worse outcomes of prostate cancer. In the US where routine screening with prostate specific antigen (PSA) is widespread, African–Americans are around 1.6 times more likely to be diagnosed with prostate cancer and are more than twice as likely to die from the disease than their white counterparts.1 In the UK, where PSA screening is not recommended, prostate cancer incidence is approximately three times higher,2 and case-specific mortality rates are 35% greater in black males compared with white males.3 These ethnic differences in mortality, in addition to possible biological differences, may arise at several points in the diagnostic and treatment pathways.4
The present study focuses on diagnosis. Some of the differences in black versus white mortality rates may be linked to diagnostic delay, although existing, albeit weak, UK studies found no evidence of such a relationship.5 Black males also have worse staging at diagnosis6 and are 1.7 times more likely to present as an emergency.4
Prostate cancer diagnosis is generally preceded by symptoms (although the possibility of cancer may not be recognised), followed by presentation to primary care, where initial assessment may lead to investigation or referral.7,8 The first interval is pre-presentational; patients may delay presenting to primary care due to fear of cancer. Non-recognition or misattribution of cancer symptoms, comorbidity, socioeconomic deprivation, and self-medication may also affect this process. In minority ethnic groups, stigma, cultural and religious preferences, language and communication barriers, as well as racial discrimination, are additional possible contributory factors to delay.9
Once patients present to primary care, however, the decision regarding whether or not to investigate for cancer is determined, in the main, by GPs. National guidance recommends shared decision making between doctor and patient,10 but it is unknown to what extent this is achieved in reality. Lower urinary tract symptoms, such as urgency and hesitancy, are common, and none is particularly suggestive of malignant, as opposed to benign, disease.11 Both digital rectal examination and PSA testing have false positives and false negatives. Furthermore, prostate cancer treatments may lead to complications, such as incontinence or impotence; men knowing this may decline testing.
Patient views on testing for cancer have rarely been investigated. In a vignette (hypothetical scenario)-based study in 2014, Banks et al reported that patients in the UK preferred to be investigated for lung, pancreatic, and colorectal cancer, even at low risk levels.12 That study was not powered to identify any ethnic differences in the preference for cancer investigation. To address this, the current study adopted a similar approach to investigate whether the preference for prostate cancer investigation in black patients is comparable with that of white patients.
How this fits in
Black males have worse outcomes in several cancer types, including prostate cancer, and they present more frequently to primary care before diagnosis when compared with white males. It is not certain whether black males have different attitudes to testing for cancer, which could explain this. This vignette-based study showed a considerably lower preference for testing in black males. Furthermore, their preference for testing was lower at the lowest risk level.
METHOD
Design and participants
This was a vignette-based survey of primary care patients, performed between January 2014 and April 2014. Participants were males aged ≥40 years, attending four general practices in Bristol, UK. Selected practices (selected from 10 potentially eligible general practices) were those located in areas with a high concentration of minority ethnic groups; these were recruited through the local Primary Care Research Network.
The survey was administered via a tablet computer (iPad) and gathered basic information on participants’ sociodemographic characteristics, including:
age;
ethnicity (defined using the 2001 UK Census groupings);
income;
level of education;
employment status;
previous history of cancer (personal, family, or close friends);
travel time to hospital; and
convenience of the nearest main hospital.
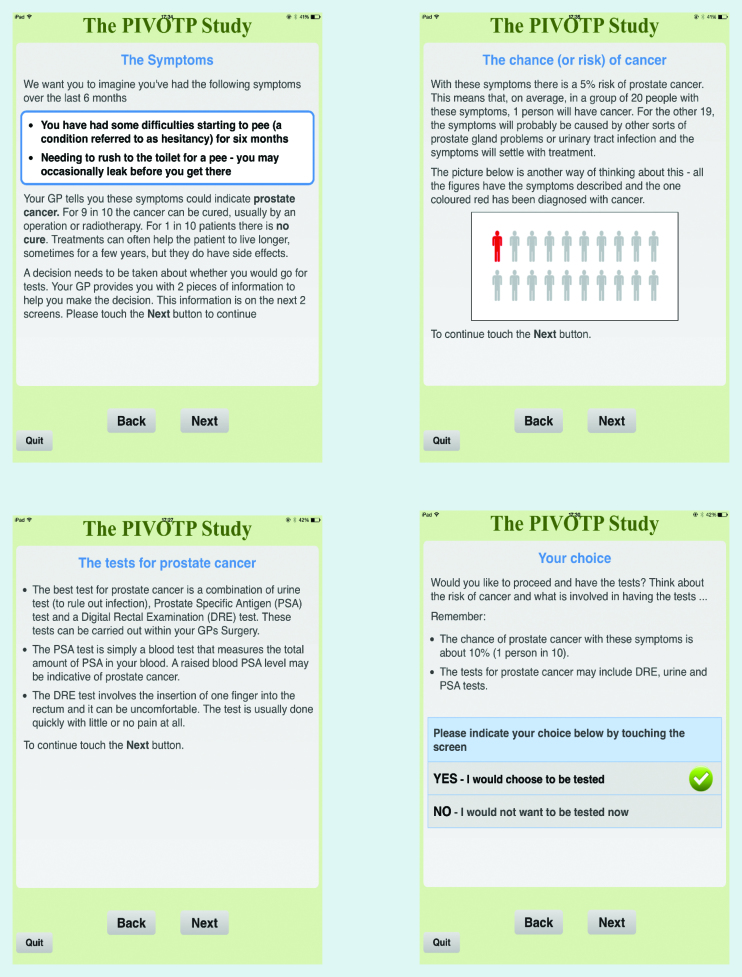
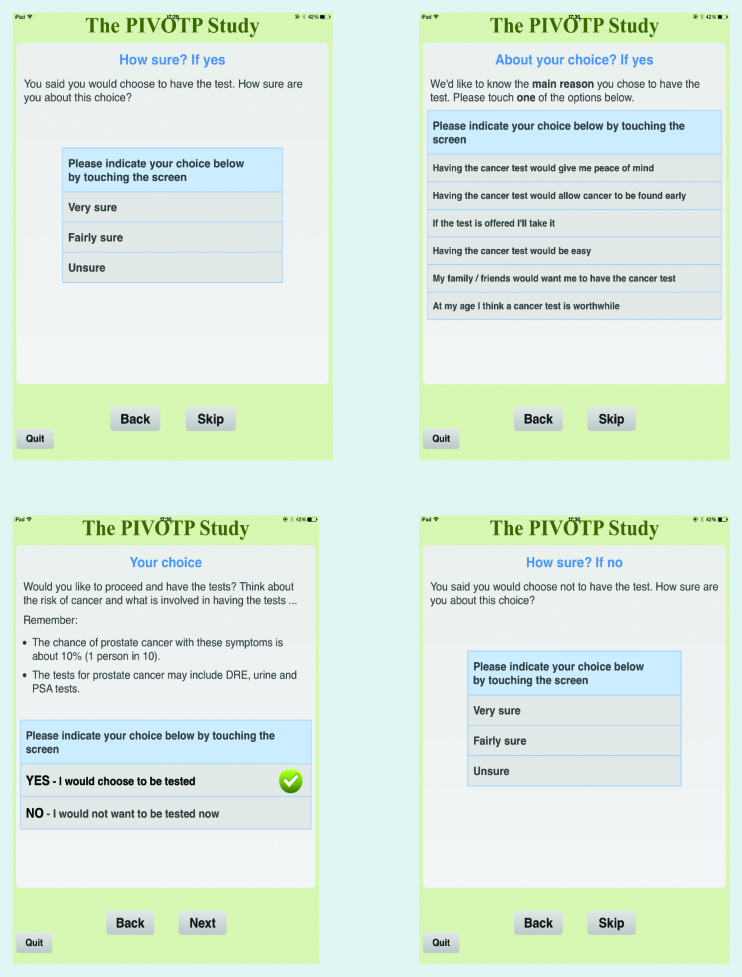
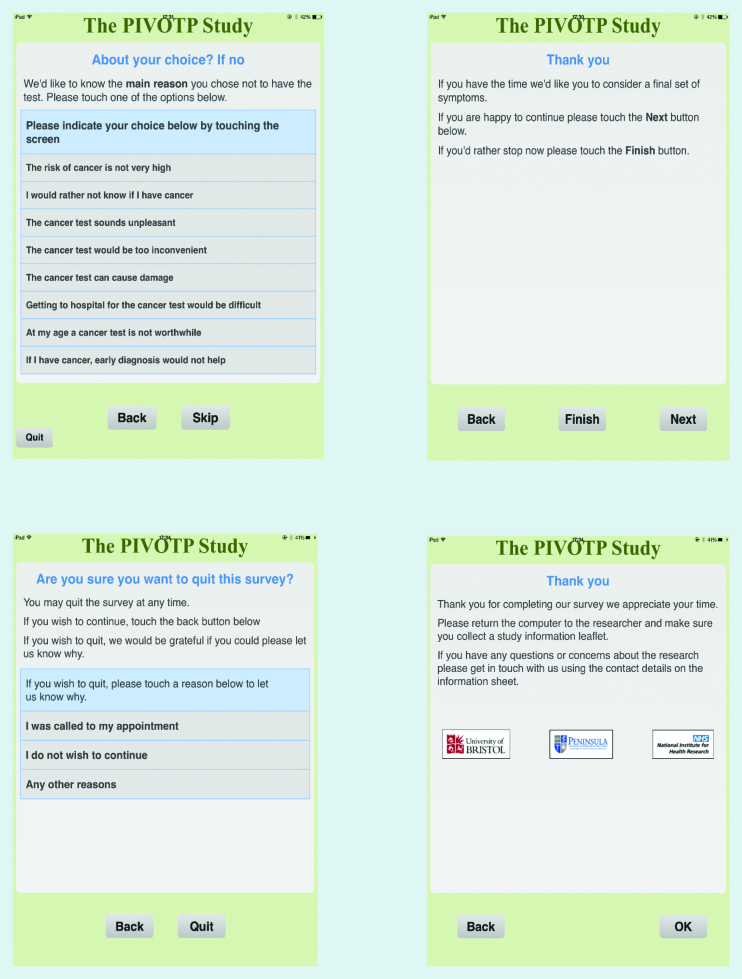
Three different vignettes each included a description of prostate cancer symptoms, or symptom combinations, and the estimated risk of prostate cancer (2%, 5%, and 10%); symptoms were portrayed numerically and pictorially. The selection of symptom profiles was based on clinical experience, primary care evidence, and guidelines from the National Institute for Health and Care Excellence (NICE).10,11 Table 1 outlines each vignette; Appendix 1 shows the screens and exact wording seen by the participants The vignettes also gave information about physical examination, relevant tests, and differential diagnoses with an approximate prognosis should prostate cancer be detected.
Table 1.
Prostate cancer symptoms and associated risk levels, as described in the vignette
| Prostate cancer symptom(s)a | Risk level, % |
|---|---|
| Hesitancy (difficulties starting to urinate) | 2 |
|
| |
| Frequency/urgency (needing to rush to the toilet to urinate) | 5 |
| Hesitancy | |
|
| |
| Weight loss | 10 |
| Frequency/urgency | |
| Hesitancy | |
All symptoms last 6 weeks.
Finally, the vignettes summarised all the information and requested participants to indicate whether or not they would choose diagnostic investigation if they had the symptoms in question. Participants were subsequently asked to choose from a predefined list of reasons for choosing or declining investigation. Extensive piloting of vignettes and the technology had been performed for a previous study, including two cycles with patient representatives;12 the piloting in this extension involved informal testing of terminology relating to urinary symptoms and risk with black community groups.
Procedure
Participants awaiting their primary care appointment were approached opportunistically by one researcher, who had the study information on the iPad screen and on paper. Patients who appeared to be <40 years of age were avoided because prostate cancer is rare in younger males. Before completing the survey, selected participants gave or declined oral informed consent, supplemented by a consent screen on the iPad. Occasionally, the practice’s bilingual link worker or professional interpreters helped clarify/translate the vignette. Participants could complete up to two vignettes, selected at random and at different risk levels. In addition, they were able to exit the survey at any stage if they desired or were called into their consultation.
Statistical analysis
The aim was to survey at least 572 males (286 of each ethnicity), providing 90% power at the 5% significance level to detect a difference between the groups in preference for investigation, 80% versus 90%, with the latter figure being the outcome in the earlier study.12
Black males in this study were those who self-identified as black–black British African or black–black British Caribbean, while white males were self-identified white British. Males who identified with ethnic groups other than the above categories were classified as ‘other groups’ and were omitted from the analyses due to small numbers.
Participant characteristics were summarised using simple descriptive statistics. Few participants completed a second vignette, so analyses of preferences for investigation were restricted to the first. Logistic regression was used to compare the binary outcome preference for investigation (opting for investigation versus not doing so) between white and black groups, firstly without adjustment and, secondly, adjusted for potential confounders, including age, employment status, convenience of hospital, previous history of cancer, and prostate cancer risk. As a second test of the possible effect of age on the main outcome, a stratified analysis was performed using three age groups. However, as expected from the main analysis, this was insignificant; as such, the results have been omitted. All analyses were conducted using Stata (version 13).
RESULTS
General practices
Ten potentially eligible general practices expressed interest in participation, of these, four were selected, one had data on patients’ ethnicity, with 2.5% of the practice patients reported as being black.13 This practice was selected despite having a relatively low percentage of black males, to increase generalisability. The remaining three were located in areas with a high concentration of black African or black Caribbean people (40%, 40%, and 17%, respectively) when compared with an overall figure of 3.3% for England and Wales.14
The mean number of patients registered in the practices was 12 567 (range 5176–18 035); the average practice size in England is 7041.13 All four practices were in areas of considerable socioeconomic deprivation, when compared with the average Index of Multiple Deprivation (IMD) score for England in 2012. The mean IMD score for the four practices was 36.9 (range 29.6–43.5), compared with an average of 21.8 for England in 2012.13
Patients’ characteristics
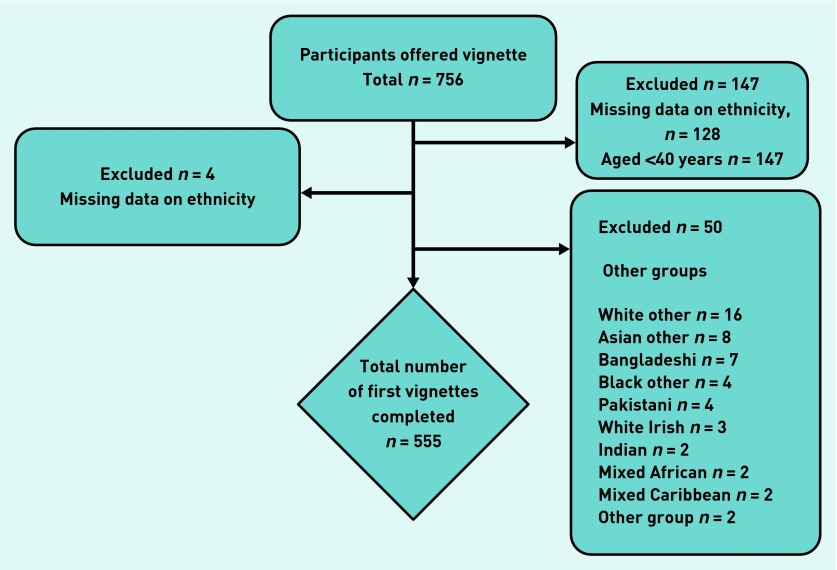
In total, 756 males were asked to participate; 147 either declined (n = 128) or were <40 years of age (n = 19). Four omitted the questions on ethnicity, and 50 self-identified with other ethnic groups therefore were excluded; this left 555 participants for analysis. Figure 1 shows the participant selection process and the number of vignettes completed. Table 2 shows participants’ characteristics by ethnic group.
Figure 1.
Participant selection process.
Table 2.
Participants’ (n = 555)a characteristics by black (n = 286) and white (n = 269) males
| Characteristics | Black males, % | White males, % |
|---|---|---|
| Age, years | ||
| 40–59 | 74 | 39 |
| 60–69 | 11 | 28 |
| ≥70 | 15 | 33 |
|
| ||
| Income, £ | ||
| <10 000 | 41 | 44 |
| 10 000–25 000 | 54 | 52 |
| 25 000–40 000 | 5 | 5 |
|
| ||
| Highest educational qualification | ||
| None | 29 | 30 |
| GCSE/equivalent | 36 | 33 |
| Vocational or A-level | 17 | 27 |
| Degree or more advanced | 18 | 10 |
|
| ||
| Employment status | ||
| Retired | 21 | 51 |
| Not in paid employment | 22 | 14 |
| Working part time | 15 | 16 |
| Working full time | 42 | 19 |
|
| ||
| Convenience of hospital | ||
| Very convenient | 69 | 82 |
| Quite convenient | 26 | 16 |
| Quite inconvenient | 4 | 2 |
| Very inconvenient | 2 | 0 |
|
| ||
| Travel time to hospital, hours | ||
| <0.5 | 93 | 95 |
| 0.5–1 | 7 | 5 |
|
| ||
| Previously diagnosed with cancer | 3 | 4 |
|
| ||
| Family or close friend previously diagnosed with cancer | 39 | 59 |
The lowest sample size was 552 of a maximum of 555. GCSE = General Certificate of Secondary Education.
Of the 555 participants entering analysis, 286 (52%) self-identified as black males and 269 (48%) as white males. Black males were younger (74% aged 40–59 years) and a greater percentage were in full-time employment compared with their white counterparts (42% versus 19%). Just over half of the group of white males had retired. More white males (59%) than black males (39%) had a family member or friend with a history of cancer.
Preference for investigation
Overall, 81% of the participants opted for investigation. Participants’ preferences for investigation differed by ethnicity with 94% of white males opting for investigation regardless of risk levels and 70% of black males doing so. The difference between the groups was most marked at the lowest risk level: just 44% of black males opted for investigation compared with 91% of white males (Table 3).
Table 3.
Preference for testing in black males and white males
| Level of risk, % | Black males,% (n) | White males,% (n) | COR | AORa | 95% CI | P-value |
|---|---|---|---|---|---|---|
| 2 | 44 (40/90) | 91 (98/108) | ||||
| 5 | 82 (79/96) | 97 (83/86) | ||||
| 10 | 80 (79/99) | 96 (70/73) | ||||
| All | 70 (198/285) | 94 (251/267) | 0.15 | 0.13 | 0.07 to 0.25 | <0.001 |
AOR = adjusted odds ratio. COR = crude odds ratio.
Adjusted for participants’ age, employment status, convenience of hospital, previous history of cancer (none of which was independently associated with opting for investigation), and prostate cancer risk level.
After controlling for participants’ age, employment status, convenience of hospital, and previous history of cancer (none of which was independently associated with opting for investigation), plus prostate cancer risk level, the odds of opting for investigation remained significantly lower in black males (odds ratio [OR] 0.13; 95% confidence interval [CI] = 0.07 to 0.25; P<0.001) (Table 3). A test of interaction showed little evidence that the OR differed by level of risk (P = 0.41).
Reason for choice
Although the main reason cited by males of both groups was early diagnosis, a much higher proportion of white males selected this option. In black males, peace of mind was almost as important (Table 4).
Table 4.
Main reasons cited for investigation preferences in black males and white males
| Main reason for choosing investigation | Black males, % n = 197 | White males, % n = 251 | P-valuea |
|---|---|---|---|
| Having the cancer test would give me peace of mind | 41 | 15 | |
| Having the cancer test would allow cancer to be found early | 45 | 72 | |
| If the test is offered I’ll take it | 11 | 9 | 0.001 |
| Having the test would be easy | 1 | 0 | |
| My family/friends would want me to have the cancer test | 1 | 0 | |
| At my age, I think a cancer test is worthwhile | 1 | 3 | |
|
| |||
| Main reason for declining investigation | Black males, % n = 85 | White males, % n = 14 | |
|
| |||
| The risk of cancer is not very high | 45 | 43 | |
| I would rather not know I have cancer | 37 | 14 | |
| The cancer test sounds unpleasant | 12 | 7 | |
| The cancer test can cause damage | 1 | 7 | <0.001 |
| The cancer test would be too inconvenient | 0 | 0 | |
| Getting to hospital for the cancer test would be difficult | 0 | 0 | |
| At my age, a cancer test is not worthwhile | 2 | 29 | |
| If I have cancer, early diagnosis would not help | 4 | 0 | |
χ2 test P-value.
Fewer white males than black males gave their reasons for declining investigation although, again, differences were significant (Table 4).
For males in both groups, the main reason cited for declining investigation was low risk of cancer; however, a considerably higher proportion of black males stated that they did not want to know if they had cancer (Table 4).
DISCUSSION
Summary
In this study, it was found that black males opt for investigation for possible prostate cancer less frequently than white males; this did not appear to be related to any specific, recorded, patient characteristic. This lower preference for investigation in black males was particularly marked when the risk of cancer in the vignette was low: less than half of black males opted for investigation when the risk of prostate cancer was the lowest value offered (namely 2%). In contrast, white males had a very high preference for investigation, including at the 2% risk level.
Several factors were not significantly associated with black males’ preferences for investigation, including age, income, employment status, convenience of the nearest main hospital, or a family history of cancer.
Strengths and limitations
To the authors’ knowledge, this is the first study to examine ethnic differences in the desire to be tested for prostate cancer. This study built on a previous, successful project that was not powered to explore ethnic differences; as a result, much of the design and piloting for this study had already been performed, and procedural problems overcome.
The vignettes were realistic and used primary care data to provide estimates of the actual risk of prostate cancer.11 In addition, the electronic nature of the questionnaire minimised missing data and was accepted by 80% of patients who often have a long waiting time, with few or no distractions. The response rate of >80% was excellent, and there was no obvious difference by ethnic groups in those declining to participate.
However, some limitations are present. Black male patients (who have a higher incidence rate for prostate cancer) were compared with white male patients; as a result, the findings cannot be generalised beyond these two groupings. In addition, two black ethnicities (black–black British African and black–black British Caribbean) were grouped together; there are many different black ethnic groups, which may have different views on the advantages of testing for prostate cancer.
A further limitation is that only prostate cancer was studied so it is not possible to determine whether the lower preference for investigation in black males would also be found for other cancers, or in black females. Furthermore, the sample population comprised GP attenders. Although conducting the study in the GP practice offered the major advantage of providing translation where needed, and being the setting where initial investigation for prostate cancer takes place, it is not possible to determine whether a true community sample, or a sample in other cities, would have yielded different results. That said, there is no reason to think this would be the case.
The final consideration is whether vignettes give valid answers. This was discussed relatively widely in Banks et al ’s recent study: most, but not all, studies considered vignettes to provide meaningful responses.12
Comparison with existing literature
Overall, 81% of the sample participants opted for investigation in the first vignette. This proportion is lower than the 88% reported in Banks et al ’s study (although 89% of participants in that study were white British); the differences by risk groups in that study were also slightly larger. In the study reported here, 94% of white males opted for investigation; this may reflect the different cancer site: prostate, as opposed to colon, pancreas, or lung. Prostate cancer is generally found in older males, has lower mortality rates, and is relatively more common in black males; all of these factors make it somewhat atypical.
There was a general increase in the preference for investigation with higher risk of cancer in black males; a finding reported by Banks et al,12 although in that case it was largely driven by their colorectal findings. The rationale appears logical; it was not seen in white males but this could be a result of their high overall preference for investigation.
This study’s findings of a lower preference for investigation in black males, compared with white males, could perhaps indicate why it has been found that emergency presentations are increased, and mortality and staging at diagnosis are worse, in black males.3,4,15 The current findings are based on a vignette that presupposed entry into health care, and strictly does not extrapolate on the decision to seek health care when a man has symptoms; however, it is plausible that a lower desire for investigation may also engender a lower desire to seek help.
Black males have been reported to have a worse fear of prostate cancer when compared with white males.4,16 They fear that the disease could be terminal and that its treatment could lead to severe sexual disorders (such as erectile dysfunction, sterility, and decreased sex drive), which, in turn, may change their close relationships with their spouses.16,17 Several (mainly US) studies have highlighted fear as a major deterrent to black males’ medical help-seeking, even when experiencing lower urinary tract symptoms.16 This factor may explain some of the views expressed by black males in this study rather than assuming that they were making accurate judgement of their cancer risk. It is also well recognised that black males do not like visiting doctors and may be influenced in their healthcare seeking by family members;18,19 interestingly, however, a specific family history of cancer did not appear to be important in the current study.
Conversely, patients’ knowledge of prostate cancer signs and symptoms, investigative procedures, and possible outcomes of treatments may influence their willingness for investigation.17,20 Males of both ethnicities have similar knowledge of prostate risks and symptoms,4 although black males tend to underestimate their personal risk of the disease,21 and are often less conversant with the PSA and rectal examination procedures, and may abstain from investigation altogether due to this.17,20 Some black males perceive rectal examination as a threat to their masculinity and consider it an undignified test.17,20 They are also more likely to be too embarrassed about lower urinary tract symptoms and generally less comfortable seeing their GPs compared with their white counterparts.4,22 These factors, in addition to language or communication barriers, stigma, and socioeconomic deprivation may provide an alternative explanation to black males’ reluctance for prostate cancer investigation when symptomatic.
Models of behavioural change (for example, the health belief model and self-regulatory models) have been used to explain patients’ attitudes towards cancer screening and early diagnosis.23,24 The questionnaire in this study did not collect specific information to assess this, although the main reasons cited by participants for choosing or declining investigation provide useful insights in this regard. In total, 86% of those declining prostate cancer investigation were black males, around half of whom cited low risks as the main reason for their choice. This is consistent with the findings of a US study, which reported moderate perceived susceptibility and perceived severity of prostate cancer in black males.24 Worryingly, 37% of those who declined indicated that they would rather not know they have cancer; this, again, echoes their fears of the disease and perceived negative consequences of it being diagnosed.
In both groups who opted for investigation, early detection of prostate cancer was the main reason cited for their decision, and black males cited peace of mind almost as frequently. White male reasoning in this situation may be interpreted in line with their perceived benefits of treatment and curability of the disease, while black males’ views may, again, reflect their greater fear of prostate cancer diagnosis and possible treatment outcomes.
Implications for practice
The pathway to diagnosis of symptomatic prostate cancer is complex, the success of which depends largely on prompt presentation of symptoms to primary care and prompt referral to secondary or specialist care. Both stages may be influenced by patients’ preference for diagnostic investigation. GPs should be aware of the reduced appetite for testing in black males (which is possibly linked to fear and perceived negative outcomes of a prostate cancer diagnosis) and may consider being proactive in discussing the subject. This is particularly important as a study has suggested lower self-initiated discussion with the doctor about prostate cancer in black Caribbean males (as measured in native-born and foreign-born black males in the US).25
Prostate cancer awareness campaigns currently targeting black males may prove less effective where patients are unwilling to take up diagnostic investigation. Campaigners may consider including information about testing procedures and promote the benefits of early diagnosis. This is especially relevant as black community groups are increasingly keen to see PSA screening become available. If such campaigns could also incorporate encouragement for symptomatic testing, the differences reported in this study may narrow.
Black males, who have a higher incidence of prostate cancer and a higher mortality from it, are less inclined than white males to be tested for the disease. Education targeted at the black community and the health professionals who treat them may help to address this.
Acknowledgments
We thank Bristol Clinical Commissioning Group (Bristol CCG) for coordinating the recruitment of the general practices, all four practices who took part in this study, Vasilis Nikolaou for helping with statistics, and Sarah Price for proofreading the manuscript. The views expressed in this report are those of the authors and not necessarily those of the UK’s NHS, Department of Health, or Policy Research Unit, who provided funding for this research.
Appendix 1. The vignette as viewed by participants.
Funding
The Policy Research Unit in Cancer Awareness, Screening and Early Diagnosis receives funding for a research programme from the Department of Health Policy Research Programme. It is a collaboration between researchers from seven institutions (Queen Mary University of London, UCL, King’s College London, London School of Hygiene and Tropical Medicine, Hull York Medical School, Durham University, and Peninsula Medical School). The views expressed are those of the authors and not necessarily those of the NHS, or the Department of Health. Obioha C Ukoumunne is funded by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for the South West Peninsula at Royal Devon and Exeter NHS Foundation Trust. The views expressed in this publication are those of the authors and not necessarily those of the NIHR.
Ethical approval
Ethical approval was obtained from Camden and Islington National Research Ethics Service Committee (ref 13/LO/1823).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
William Hamilton is the clinical lead for the continuing revision of the 2005 guidance published by the National Institute for Health and Care Excellence (NICE). His contribution to this article is in a personal capacity and should be interpreted as neither representing the view of the Guideline Development Group nor that of NICE. The other authors declare no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.US Cancer Statistics Working Group . US Department of Health and Human Services Centers for Disease Control and Prevention and National Cancer Institute. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2005. United Statistics Cancer Statistics: 2002 Incidence and Mortality. [Google Scholar]
- 2.Ben-Shlomo Y, Evans S, Ibrahim F, et al. The risk of prostate cancer amongst black men in the United Kingdom: the PROCESS cohort study. Eur Urol. 2008;53(1):99–105. doi: 10.1016/j.eururo.2007.02.047. [DOI] [PubMed] [Google Scholar]
- 3.Evans S, Metcalfe C, Ibrahim F, et al. Investigating black–white differences in prostate cancer prognosis: a systematic review and meta-analysis. Int J Cancer. 2008;123(2):430–435. doi: 10.1002/ijc.23500. [DOI] [PubMed] [Google Scholar]
- 4.Metcalfe C, Evans S, Ibrahim F, et al. Pathways to diagnosis for black men and white men found to have prostate cancer: the PROCESS cohort study. Br J Cancer. 2008;99(7):1040–1045. doi: 10.1038/sj.bjc.6604670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martins T, Hamilton W, Ukoumunne OC. Ethnic inequalities in time to diagnosis of cancer: a systematic review. BMC Fam Pract. 2013;14(1):197. doi: 10.1186/1471-2296-14-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones BA, Liu WL, Araujo AB, et al. Explaining the race difference in prostate cancer stage at diagnosis. Cancer Epidemiol Biomarkers Prev. 2008;17(10):2825–2834. doi: 10.1158/1055-9965.EPI-08-0203. [DOI] [PubMed] [Google Scholar]
- 7.Hamilton W. Five misconceptions in cancer diagnosis. Br J Gen Pract. 2009 doi: 10.3399/bjgp09X420860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hamilton W, Sharp D. Symptomatic diagnosis of prostate cancer in primary care: a structured review. Br J Gen Pract. 2004;54(505):617–621. [PMC free article] [PubMed] [Google Scholar]
- 9.Walter F, Webster A, Scott S, Emery J. The Andersen Model of Total Patient Delay: a systematic review of its application in cancer diagnosis. J Health Serv Res Policy. 2012;17(2):110–118. doi: 10.1258/jhsrp.2011.010113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Institute for Health and Care Excellence . Referral guidelines for suspected cancer. London: NICE; 2005. http://www.nice.org.uk/guidance/cg027 (accessed 2 Jan 2015) [Google Scholar]
- 11.Hamilton W, Sharp DJ, Peters TJ, Round AP. Clinical features of prostate cancer before diagnosis: a population-based, case-control study. Br J Gen Pract. 2006;56(531):756–762. [PMC free article] [PubMed] [Google Scholar]
- 12.Banks J, Hollinghurst S, Bigwood L, et al. Preferences for cancer investigation: a vignette-based study of primary-care attendees. Lancet Oncol. 2014;15(2):232–240. doi: 10.1016/S1470-2045(13)70588-6. [DOI] [PubMed] [Google Scholar]
- 13.Public Health England . National general practice profiles. London: Public Health England; 2013. http://fingertips.phe.org.uk/profile/general-practice/data#mod,2,pyr,2013,pat,19,par,E38000022,are,L81015,sid1,2000005,ind1,-,sid2,-,ind2,- (accessed 2 Jan 2015) [Google Scholar]
- 14.Office for National Statistics . Ethnicity and National Identity in England and Wales 2011. London: ONS; 2012. http://www.ons.gov.uk/ons/rel/census/2011-census/key-statistics-for-local-authorities-in-england-and-wales/rpt-ethnicity.html#tab-Differences-in-ethnicity-across-local-authorities- (accessed 26 Jan 2015) [Google Scholar]
- 15.National Cancer Intelligence Network Mortality from Prostate Cancer. 2012. Urological Cancers SSCRG. http://www.ncin.org.uk/view?rid=1701 (accessed 27 Jan 2015)
- 16.Pedersen VH, Armes J, Ream E. Perceptions of prostate cancer in Black African and Caribbean men: a systematic review. BMJ Support Palliat Care. 2011;1(Suppl 1):A13. doi: 10.1002/pon.2043. [DOI] [PubMed] [Google Scholar]
- 17.Price JH, Colvin TL, Smith D. Prostate cancer: perceptions of African–American males. J Natl Med Assoc. 1993;85(12):941–947. [PMC free article] [PubMed] [Google Scholar]
- 18.Griffith DM, Ober Allen J, Gunter K. Social and cultural factors influence African American men’s medical help seeking. Res Soc Work Pract. 2011;21(3):337–347. [Google Scholar]
- 19.Gascoigne P, Mason MD, Roberts E. Factors affecting presentation and delay in patients with testicular cancer: results of a qualitative study. Psychooncology. 1999;8(2):144–154. doi: 10.1002/(SICI)1099-1611(199903/04)8:2<144::AID-PON349>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 20.Richardson JT, Webster JD, Fields NJ. Uncovering myths and transforming realities among low-SES African–American men: implications for reducing prostate cancer disparities. J Natl Med Assoc. 2004;96(10):1295–1302. [PMC free article] [PubMed] [Google Scholar]
- 21.Jones AR, Shipp M, Thompson CJ, Davis MK. Prostate cancer knowledge and beliefs among black and white older men in rural and urban counties. J Cancer Educ. 2005;20(2):96–102. doi: 10.1207/s15430154jce2002_10. [DOI] [PubMed] [Google Scholar]
- 22.Maliski SL, Connor S, Fink A, Litwin MS. Information desired and acquired by men with prostate cancer: data from ethnic focus groups. Health Educ Behav. 2006;33(3):393–409. doi: 10.1177/1090198105276223. [DOI] [PubMed] [Google Scholar]
- 23.Tavafian SS. Predictors of cervical cancer screening: an application of health belief model. In: Rajamanickam R, editor. Topics on cervical cancer with an advocacy for prevention. Rijeka, Croatia: InTech; 2012. http://cdn.intechopen.com/pdfs/30744/InTech-Predictors_of_cervical_cancer_screening_an_application_of_health_belief_model.pdf (accessed 27 Jan 2015) [Google Scholar]
- 24.Odedina FT, Dagne G, Pressey S, et al. Prostate cancer health and cultural beliefs of black men: the Florida Prostate Cancer Disparity Project. Infect Agent Cancer. 2011;6(2):S10. doi: 10.1186/1750-9378-6-S2-S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Odedina FT, Dagne G, LaRose-Pierre M, et al. Within-group differences between native-born and foreign-born Black men on prostate cancer risk reduction and early detection practices. J Immigr Minor Health. 2011;13(6):996–1004. doi: 10.1007/s10903-011-9471-8. [DOI] [PubMed] [Google Scholar]