Abstract
Background
Clinical commissioning groups (CCGs) are required to demonstrate meaningful patient and public engagement and involvement (PPEI). Recent health service reforms have included financial incentives for general practices to develop patient reference groups (PRGs).
Aim
To explore the impact of the patient participation direct enhanced service (DES) on development of PRGs, the influence of PRGs on decision making within general practice, and their interface with CCGs.
Design and setting
A mixed-methods approach within three case study sites in England.
Method
Three case study sites were tracked for 18 months as part of an evaluation of PPEI in commissioning. A sub-study focused on PRGs utilising documentary and web-based analysis; results were mapped against findings of the main study.
Results
Evidence highlighted variations in the establishment of PRGs, with the number of active PRGs via practice websites ranging from 27% to 93%. Such groups were given a number of descriptions such as patient reference groups, patient participation groups, and patient forums. Data analysis highlighted that the mode of operation varied between virtual and tangible groups and whether they were GP- or patient-led, such analysis enabled the construction of a typology of PRGs. Evidence reviewed suggested that groups functioned within parameters of the DES with activities limited to practice level. Data analysis highlighted a lack of strategic vision in relation to such groups, particularly their role within an overall patient and PPEI framework).
Conclusion
Findings identified diversity in the operationalisation of PRGs. Their development does not appear linked to a strategic vision or overall PPEI framework. Although local pragmatic issues are important to patients, GPs must ensure that PRGs develop strategic direction if health reforms are to be addressed.
Keywords: general practice, incentives, patient groups, typology
INTRODUCTION
GPs, like all healthcare providers, have a duty to involve patients, not only in aspects of choice of treatment and self-management, but also in how healthcare services are planned, monitored, delivered, and developed.1 Demonstrating meaningful patient and public engagement and involvement (PPEI) was also one of the key domains for authorising clinical commissioning groups (CCGs).2 This is fundamental to achieving a healthcare system that is responsive to patients’ needs and values.3 How they involve patients is important, particularly as commissioning is now firmly in the hands of primary care clinicians through CCGs and there is very little evidence of this working effectively in the health service per se, let alone in primary care.4 Recent health service reforms created new organisational structures to strengthen the public voice, including incentivising GPs to proactively engage with their patients via patient reference groups (PRGs).5 Since the introduction of the patient participation directed enhanced service (DES), most general practices now have a PRG in some form or other. The DES provides payments to GP practices with key objectives for patients to become involved directly in the decision making that may lead to changes in services within their GP practice promoting ‘the proactive engagement of patients.’ 5 There is a clear emphasis on reaching a broad cross section of the community, yet in a format that is set by the practice itself.
Historically, such groups were known as patient participation groups (PPGs) and have been recognised as part of general practice since the early 1970s, with functions focusing on voluntary work, practice organisation, and health education.6,7 Although PPGs were slow to develop, through support from a national member association8 and campaign,9 around 40% of all English GP practices had an established group by 2009. However, previous research findings identified a number of concerns regarding these groups, including equity of access, uneven distribution, unrepresentative membership, diversity of purpose, variation, and difficulties around assessing cost and benefit.10 Furthermore, PPGs have suffered from problems of longevity, with only a small minority operational for >5 years.6 Nevertheless, recent estimates suggest that such groups continue to increase in numbers, with around 75% operational in 2012.8
A review in 201011 found that most of these groups demonstrated little influence on practice management or service development, functioning primarily as a provider of feedback on services with a relatively passive role within the practice. The review did highlight a few examples of innovative practice, however, where PPGs were more meaningfully involved in the governance of primary care services at practice-based commissioning (PbC) consortium level; for example, a built-in majority of lay members at board level, developing involvement vehicles that moved beyond practice level to increase decision-making capacity. These groups thrived in a culture where there was a history and commitment to PPEI within the organisation, a network approach to development, and an enabling and supportive primary care trust (PCT).11
How this fits in
This study builds on previous research relating to the development and implementation of patient participation initiatives in general practice, exploring the impact of new involvement vehicles, patient reference groups (PRGs). Findings identify inconsistent progression in terms of PRG development between case study sites. Clinical commissioning groups need to move beyond merely establishing PRGs at practice level, with greater commitment to incorporating them into an overall involvement strategic framework.
Professional guidance around PPEI for GPs exists in the form of toolkits and briefings, which outline the benefits of effective PPEI along with some suggestions on how to engage and involve.12,13 The Department of Health (DH) also provides some step-based guidance for setting up PRGs,5 and there is also guidance offered through conditions for the DES contract for patient participation, with proposals to extend for the financial year 2015.14 The benefits of developing PRGs are linked to potential improvements in services and performance as well as increasing accountability.5 However, unlike the World Class Commissioning Framework’s competencies for PPEI,15 there is no mechanism for evaluating the effectiveness of PPEI within general practice.
Aim
As part of a larger National Institute for Health Research (NIHR) funded study evaluating patient and public involvement in commissioning,16 this sub-study explored the impact of the DES on the establishment of PRGs, their influence on decision making within general practices, and the relationship PRGs had with emerging CCG structures.
METHOD
A case study design was used with three in-depth qualitative case studies. The research was conducted between May 2010 and April 2013. Case study sites were purposively selected PCTs that would ensure a maximum variety sample across a number of domains. These included urban/rural settings, the number and type of main providers for each PCT (for example, teaching hospital versus district general hospital), and sociodemographic profile (including deprivation and ethnic minority). As the research spanned the NHS reorganisation, the original PCT in each site was replaced by a CCG as the unit of analysis. Site characteristics are shown in Box 1.
Box 1. Case study site characteristics.
| Case study | Setting | Population/ethnicity | Secondary care provider | CCGs |
|---|---|---|---|---|
| CS1 | Mixed urban (town)/rural | Some ethnic minority groups, but mainly white | District general hospital | Single CCG 39 practices (15 single handed) |
| CS2 | Urban (city) | Average size BME population | Teaching hospital | Single CCG 89 practices (5 single handed) |
| CS3 | Urban (town) | High BME population | Foundation trust district general hospital | Single CCG 31 practices (6 single handed) |
BME = Black and minority ethnic. CCG = clinical commissioning group.
Data were collected using a variety of methods. Over 100 interviews were completed with commissioners, providers, and service users, and focus groups were conducted with service users (Table 1 and Table 2).
Table 1.
Focus groups
| Case study | Composition | Characteristics of focus group |
|---|---|---|
| CS1 | 6 participants in 1 focus group | Service users (adult) with neurological long-term conditions |
| CS2 | 4 participants in 1 focus group | Service users (adult) with rheumatoid arthritis |
| CS3 | 20 participants in 2 focus groups | Service users (adult BME) with diabetes |
BME = Black and minority ethnic.
Table 2.
Interviews
| Case study | Service users and representatives | Commissioners (PCT, GP, CCG/LA and PPEI leads) | Providers | Total number of interviews |
|---|---|---|---|---|
| CS1 | 33 | 11 | 4 | 48 |
| CS2 | 11 | 9 | 5 | 25 |
| CS3 | 11 | 13 | 5 | 29 |
|
| ||||
| Total interviewed | 55 | 33 | 14 | 102 |
CCG = clinical commissioning groups. CS = case study. LA = local authority. PCT = primary care trust. PPEI = public engagement and involvement.
All interviews and focus groups were recorded and transcribed. Ten meetings were observed including shadow CCG boards, clinical networks, and locality GP meetings. Six workshops were held to enable an iterative process with participants (Table 3).
Table 3.
Workshops, two per case study site, overall attendance
| Case study | Service users and representatives | Commissioners (PCT, GP, CCG/LA and PPEI leads) | Providers (services/education) | Total attendees at workshops |
|---|---|---|---|---|
| CS1 | 12 | 20 | 21 | 53 |
| CS2 | 18 | 9 | 4 | 31 |
| CS3 | 20 | 25 | 19 | 64 |
CCG = clinical commissioning groups. CS = case study. LA = local authority. PCT = primary care trust. PPEI = public engagement and involvement.
All case study participants were invited to a summative workshop, with a total number of 47 attendees (27 lay representatives, 15 commissioners, and five NHS providers).
In total, 113 documents relevant to PPEI in each site were analysed. All data were managed on NVivo using a framework approach (version 10). A framework method for analysing qualitative data was selected as it is suited to assessing the effects of policies from the perspective of people they affect.17 Analysis of data was undertaken within and between each case study, with at least two researchers independently cross-checking coded transcripts to enable inter-rater reliability.
This study reports on findings relevant to PRGs. In addition to data collected from the above methods, researchers undertook a web-based search within each case study site to determine the numbers of active PRGs. Results were then mapped against findings from the main study to assess the positioning of PRGs within the PPEI structure as a whole within each site. A management fellow was funded to work with the study team to develop local research capacity in case study 1 (CS1). This enabled a more detailed examination in this case study site including an extended documentary analysis in relation to published PRG terms of reference and minutes of PRG meetings, to identify the aims and objectives of individual groups. The numbers of PRGs before and after the introduction of the DES incentive were taken into consideration to identify the impact of the contract.
RESULTS
In all three case studies, there was evidence of a high percentage of active practice websites (averaging 82%): CS1 had 39 practices, with 32 having accessible practice websites; case study 2 (CS2) had 89 practices, with 71 having accessible practice websites; and case study 3 (CS3) had 30 practices, with 24 accessible practice websites. However, the actual number of the websites demonstrating that their patient group was active showed a wide variation (Figure 1).
Figure 1.
GP practice patient groups in case study sites, March 2013.
In CS1, for example, nine (27%) PRGs were visible within 32 practice websites. In CS3, this rose to 15 (58%) out of 26 practice websites, while in CS2, 66 PRGs (93%) were visible within 71 practice websites. Website analysis also highlighted differences in terminology such as PRG, PPG, patient forum, or patient group.
Data analysis also highlighted a wide variance in how these groups were operationalised. The predominant mode of operation for CS1 was through the use of virtual groups (seven out of nine). In contrast, both CS2 and CS3 had larger percentages of actual face-to-face PRGs, 47 out of 66 (71%) and 10 out of 15 (64%), respectively. Some practices did use a combination of both methods.
Documentary analysis in relation to CS1, revealed an increase in the number of PRGs pre and post DES incentive. In 2011–2012 this numbered 13, by 2012–2013 this number had risen to 28 (115% increase), with a further rise to 31 practices by 2013–2014 (11% increase). This is an increase of 115% by year 2 and a further 11% increase for year 3.
The extended web-based analysis of CS1 found that PRG terms of reference and minutes identified that such groups functioned within the basic parameters of the DES, for example, activities relating to the administration of patient surveys. This rather narrow approach resulted in limited engagement by patients:
‘We’ve had the occasional circular round … and there have been question and answer mainly, tick or put a cross, you know. But that’s all, yeah.’
(CS1 patient focus group)
‘During total purchasing we did involve them in some of the service design and development that we were doing, so we had active membership of patients within that. Since the demise of the PPG and since the demise of fundholding, probably from about 1987 [sic] to, you know, sort of, 2000, we kept on our PPG and our PPG has acted more as an advisory service to the practice doing feedback as to, you know, how they were experiencing the services.’
(CS3 practice manager)
Changes that were highlighted tended to focus at practice level, on pragmatic issues such as waiting times or telephone queries rather than clinical or managerial factors. However, it was often these basic issues that impacted most on patient experience with the establishment of a PRG being seen as a tool to address these concerns:
‘There was a few complaints come through about the appointment system and different things. And it was a general feeling on the part of the clinicians that the patients needed to know more about the practice and if they worked together, that might help their understanding.’
(CS1 practice manager)
The data also revealed no single approach to establishing PRGs, a number of styles to the operationalisation of PRGs becoming clear. Some PRGs reflected a GP-led agenda, lacking clear terms of reference and predominantly consultative in nature.
Other groups were patient-led, formulating their own terms of reference and setting their own agenda:
‘… they’re coming up with their own [terms of reference] really, and that’s what we want them to do, defining, you know, what they want and how they want to function really.’
(CS2 GP)
Data from documentary analysis, interviews, and observed meetings from the project’s main study16 also highlighted a number of pertinent issues. Participants recognised that the DES was an incentive for practices to establish PRGs, which enabled CCGs to demonstrate that they had active PPEI, required for authorisation:
‘I would say that the PPG DES has probably had more of an influence and raised … the profile of patient participation more than any of the commissioning documents … in my opinion.’
(CS3 practice manager)
‘I think things have changed … the fact there was the DES there to be taken up, you know, has stimulated us to do it.’
(CS2 GP)
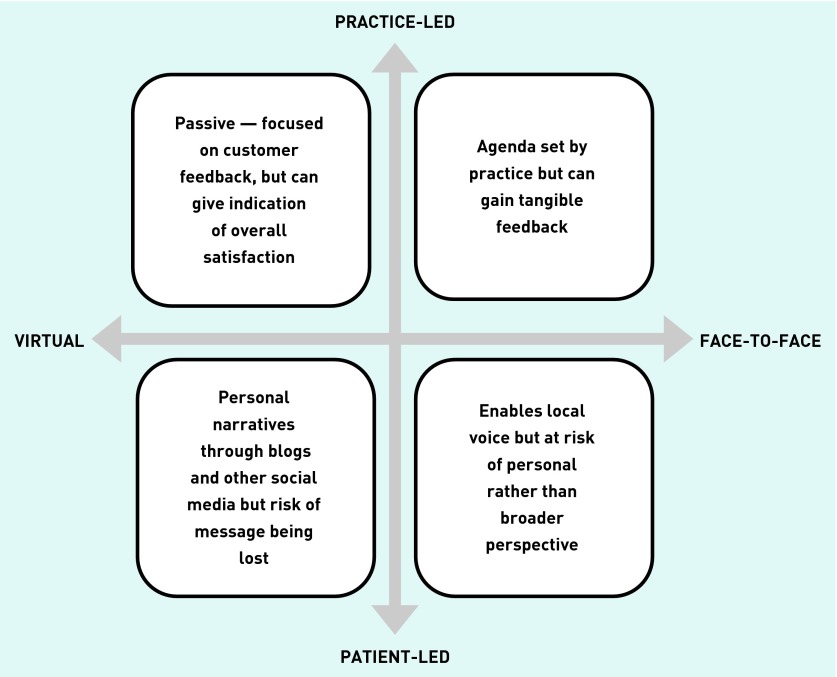
Analysis of PRG terms of reference and other documents led to the development of a typology of PRGs. Figure 2 incorporates two continuums, one focusing on the mode of PRG delivery (virtual or face-to-face). The second continuum focuses on whether the PRG is patient- or practice-led, leading to four distinct typologies, each approach has its strengths but with elements of risk.
Figure 2.
Typology of patient reference groups.
While this analysis identified key aspects of how PRGs were developed and operationalised, the study found little evidence of a strategic vision in relation to these groups, particularly their role within an overall PPEI framework. At the time of the main research study, none of the case studies could demonstrate clearly how PRGs would feed into organisational decision making and care provision. A number of PPEI vehicles were identified, including PRGs, membership schemes, and patient panels; however, how each element would function, communicate, and relate to each other could not be clearly demonstrated:
‘My worry is that information doesn’t find its way up and concerns don’t find their way up from the shop floor, as it were.’
(CS2 GP PPEI lead CCG)
DISCUSSION
Summary
The National Association for Patient Participation (NAPP) believe that over 75% of general practices in England now have a PRG,7 with groups still developing. Findings from CS1 data would suggest that financial incentive and the ‘must-do’ nature of PPIE in general practice has had a direct impact on the increased proliferation of PRGs. Case study sites highlighted that such groups took a number of forms including virtual, actual, and Patient Opinion (an online survey). Such variation between case study sites parallels historical difficulties with development and distribution of PRGs.9
Different terminology in relation to the description of such groups has the potential to cause confusion and to lead to a lack of clarity of purpose and function. This research study specifically utilised the term PRG; however, the research findings highlighted that a number of other group descriptions are also in use, such as PPG, patient forum, and patient group. The NAPP highlight differences between PRGs (post DES) and PPGs (set up before the DES), suggesting that PPGs reflect grassroots groups with their own terms of references, with flexibility in determining how they will function within a practice. PRGs are bound by the Patient Participation DES contract rules, with concerns of a more limited remit focusing exclusively on the six steps identified within the DES contract.7
There are a number of issues related to the typologies identified (Figure 2). For example, a practice-led, virtual group may focus on customer feedback; however, this can dilute patient experience to overall satisfaction, which may distort particular areas meriting improvement.18 Virtual group initiatives that are patient-led, including blogs, can focus on issues and complaints aired by local patients but it is unclear whether such issues are acted on or even received by health professionals. A strong emphasis on virtual PRGs suggests some narrow definitions of involvement limited to information exchange only. Advice available through the DES can be widened, however, to represent the population of any practice with active patients being the potential leaders for change and virtual PRGs can greatly boost patient surveys.19 Although the predominance of virtual PRGs could indicate a tokenistic response to policy demands, this may also allow participation of a more diverse population including those in employment or younger people. Further work is required to determine the outcomes of the different models of PRGs.
Patient-led, face-to-face groups can facilitate a strong local voice within the involvement process; however, if representation issues are not addressed adequately, there is a risk of a personalised agenda becoming predominant. Conversely, representativeness is a contested concept in citizen participation and involvement, with arguments made that there is a tendency for staff to question legitimacy if feeling threatened by personal narratives.19 PRGs bring new challenges to any healthcare interest already established; particularly in the current financial context.19
If agendas are set by practices, then there is also the potential to address issues that are not relevant to local patients or population. The typology identifies the continuing impact of organisational values on how PRGs are developed within individual practices. The rapid pace of change and need to secure authorisation, suggests that the establishment of such groups was of primary focus, with less thought given to how such groups would fit into the overall vision of the CCG and its strategic development.
Strengths and limitations
The present research found limited evidence of the influence of PRGs within CCGs; however, such groups were in the early stages of development at the time of the research study. The sub-study only focused on an in-depth analysis within one case study site (CS1), limiting the comparison between other sites (CS2 and CS3). CS1 was different in that it included rural populations that may live further away from the practice than in the other two case studies. It also had comparatively less deprivation and hence raises implications on the generalisability of the results. This research was able to capture the position of PRGs at a time of significant reform, however, with PPEI supposedly at the centre. Furthermore, there has been limited evidence in relation to the operationalisation of PRGs. These findings, therefore, expand knowledge within this area.
Comparison with existing literature
A clear challenge for CCGs will be effective facilitation of PRGs within an overall PPEI strategy. A continuing lack of influence has potential repercussions if not adequately addressed by CCGs, as lack of decision-making capabilities has been one of the main causes of PRG failure in the past,10 hastening the tendency towards the limited lifespan of such groups.20 Previously, there has been little engagement between general practices and their patients or local communities.21 Primary care teams need a clear strategic framework, models of best practice, and adequate resources to manage and develop PPEI initiatives.21 Early reviews of the new DES incentivising general practices to develop and support PRGs suggested that it would have a significant impact; however, the evidence from this study suggests that this has not been completely realised.22,23 Although aspirations for PRGs have been high, other studies also found limited developments in practice.24–26 If there are limited opportunities for active involvement in vital organisational issues and care, this leaves PPEI vehicles open to criticism of tokenism.20,27
Finally, PRGs are widely variable and therefore capturing a true measure of how effective they are poses challenges for CCGs and NHS England.
Implications for research and practice
GP practices have responded to the DES incentive scheme, with the number of PRGs increasing since its initiation. The requirement for PPEI as part of the authorisation process was also an additional incentive in their establishment. However, a number of key issues have been highlighted in the research. The increase in proliferation of such groups has not been partnered with a clear picture or vision as to their place within an organisational structure or their role with CCG PPEI strategy.
The lack of clear lines of communication and feedback within the CCGs studied potentially undermines the purpose of such groups. Addressing this issue will be paramount if PRGs are to be successful. Furthermore, the DES represents a top-down initiative; research findings suggest that the incentive has led to a predominantly GP-led agenda. Based on clear evidence that working in partnership with local communities, such as a practice population, can improve health outcomes even with socially disadvantaged groups,28 there needs to be recognition of the importance of patient-led involvement. Using PRGs as a forum to reflect on services can be a catalyst for local change,29 and, without adapting established groups accordingly, GP practices will be unable to capture the local voice of patients and limit the chances for local people to engage in debates regarding provision and commissioning of services. Lack of clear purpose and genuine involvement with key organisational issues has the potential to leave this DES incentive in danger of foundering.
Acknowledgments
We acknowledge the participants who took part in this study and thank them for their contribution. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Health Services and Delivery Research Programme, NIHR, NHS or the Department of Health.
Funding
The research was supported the National Institute for Health Research Health Services and Development Research Programme (HS&DR 08/1806/261).
Ethical approval
Research ethics and research governance approval was obtained from Research Ethics Committee (REC) reference 10/H0713/24) and had NHS approval.
Provenance
Freely submitted; externally peer reviewed
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Department of Health . Equity and excellence: Liberating the NHS. London: DH; 2010. [Google Scholar]
- 2.NHS England CCG authorisation: key facts http://www.england.nhs.uk/resources/resources-for-ccgs/auth/ccg-auth-facts/ (accessed 26 Jan 2015)
- 3.Coulter A, Ellins J. Patient focused interventions: A review of the evidence. London: The Health Foundation; 2006. Picker Institute Europe August 2006. [Google Scholar]
- 4.Commission for Healthcare Audit and Inspection. Healthcare Commission. Listening, learning, working together. A national study of how well healthcare organisations engage local people in planning and improving their services. 2009. http://emergingsustainability.org/files/Engaging%20patients%20%20public%20national%20report%20-%20final.pdf (accessed 14 Jan 2015)
- 5.British Medical Association, NHS Employers. Patient participation directed enhanced service (DES) for GMS contract. Guidance and audit requirements for 2011/12 2012/13. 2011 Apr; BMA, NHS Employers, [Google Scholar]
- 6.Richardson A, Bray C. Promoting health through participation: experience of groups for patient participation in general practice. London: Policy Studies Institute; 1987. [Google Scholar]
- 7.Nagraj S, Gillam S. Patient participation groups: BMJ. 2011;342:d2333. doi: 10.1136/bmj.d2333. [DOI] [PubMed] [Google Scholar]
- 8.National Association for Patient Participation (NAPP) 2012. What are PPGs? http://www.napp.org.uk/ppgintro.html (accessed 15 Dec 2014)
- 9.Growing Patient Participation: 21 ways to help your practice thrive. NAPP; 2009. National Association for Patient Participation, Royal College of General Practitioners, British Medical Association, NHS Alliance. http://www.napp.org.uk/GPP_21Ways_acc.pdf (accessed 26 Jan 2015) [Google Scholar]
- 10.Brown I. Patient participation groups in general practice in the National Health Service. Health Expect. 1999;2:169–178. doi: 10.1046/j.1369-6513.1999.00057.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parsons S, Winterbottom A, Cross P, Redding D. The quality of patient engagement and involvement in primary care: an Inquiry into the Quality of General Practice in England. 2010. The Kings Fund, http://www.pickereurope.org/wp-content/uploads/2014/10/The-quality-of-patient-engagement...-primary-care.pdf (accessed 14 Jan 2015)
- 12.British Medical Association Patient and public involvement — a toolkit for doctors. 2011. Jun, http://bma.org.uk/search?query=toolkit%20public%20involvement (accessed 15 Dec 2014)
- 13.Royal College of General Practitioners. Briefing guide: effective patient and public involvement. 2011. http://www.rcgp.org.uk/revalidation-and-cpd/~/media/1DEEDB9447064393BA5F44D8255EB988.ashx (accessed 28 Jan 2015)
- 14.NHS Employers Enhanced services 2014/15. http://www.nhsemployers.org/PayAndContracts/GeneralMedicalServicesContract/DirectedEnhancedServices/Pages/Enhancedservices201415.aspx (accessed 14 Jan 2015)
- 15.Department of Health World Class Commissioning: competencies. http://www.yhscg.nhs.uk/Governance/World%20class%20commissioning.pdf (accessed 14 Jan 2014)
- 16.Peckham S, Wilson PM, Williams L, et al. Commissioning for long-term conditions: hearing the voice of and engaging users — a qualitative multiple case study. Health Services and Delivery Research. 2014 doi: 10.3310/hsdr02440. [DOI] [PubMed] [Google Scholar]
- 17.Srivastava A, Thomson SB. Framework Analysis: A qualitative methodology for applied policy research. J Admin Governance. 2009;4(2):72–77. [Google Scholar]
- 18.National Association for Patient Participation Commissioning Patient engagement. http://www.napp.org.uk/commissioning2.html (accessed 15 Dec 2014)
- 19.Bleich SN, Özaltin E, Murray CJL. How does satisfaction with the health-care system relate to patient experience? Bull World Health Org. 2009;87(4):271–278. doi: 10.2471/BLT.07.050401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wood B. Patient power? The politics of Patients’ Associations in Britain and America. Buckingham. Philadelphia: Open University Press; 2000. [Google Scholar]
- 21.Nathan S, Stephenson N, Braithwaite J. Sidestepping questions of legitimacy: How community representatives manoeuvre to effect change in a health service. Health (London) 2014;18(1):23–40. doi: 10.1177/1363459312473617. [DOI] [PubMed] [Google Scholar]
- 22.Anonymous GP practices ‘despondent’ as they struggle to meet terms of patient participation DES’. Pulse. 2011. Aug 18, http://www.pulsetoday.co.uk/gp-practices-despondent-as-they-struggle-to-meet-terms-of-patient-participation-des/12569137.article#.VLaCzP24n8s (accessed 14 Jan 2015)
- 23.Anonymous GPC warns practices over outsourcing patient participation to private companies. Pulse. 2011. Oct 20, http://www.pulsetoday.co.uk/gpc-warns-practices-over-outsourcing-patient-participation-to-private-companies/12931633.article#.VLaBA_24n8s (accessed 14 Jan 2015)
- 24.Checkland K, Coleman A, McDermott I, et al. Primary care-led commissioning: applying lessons from the past to the early development of clinical commissioning groups in England. Br J Gen Pract. 2013 doi: 10.3399/bjgp13X671597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hudson B. Public and patient engagement in commissioning in the English NHS: an idea whose time has come? Public Manag Rev. 2015;17(1):1–16. [Google Scholar]
- 26.Brown I. Involving the public in general practice in an urban district: levels and type of activity and perceptions of obstacles. Health Soc Care Comm. 2000;8(4):251–259. doi: 10.1046/j.1365-2524.2000.00247.x. [DOI] [PubMed] [Google Scholar]
- 27.Greenhalgh T. The BMJ and the Big Society. BMJ. 2011;342:d3691. doi: 10.1136/bmj.d3691. [DOI] [PubMed] [Google Scholar]
- 28.O’Mara-Eves A, Brunton G, McDaid D, et al. Community engagement to reduce inequalities in health: a systematic review, meta-analysis and economic analysis. Public Health Res. 2013;1(4) doi: 10.3310/phr01040. [DOI] [PubMed] [Google Scholar]
- 29.Farr M. Collaboration in public services: can service users and staff participate together? In: Barnes M, Cotterell P, editors. Critical perspectives on user involvement. Bristol: Policy Press; 2012. pp. 79–88. [Google Scholar]