Abstract
Background
Economic recession affects quality of life by increasing rates of mental disorders in particular. Social support can be an important protective factor.
Aim
To estimate the impact of being personally affected by an economic crisis on health-related quality of life (HRQoL), taking into account the possible buffering effect of perceived social support.
Design and setting
Data from the first wave (March 2012 to November 2012) of the ‘Social Support and Quality of Life Study’, a longitudinal study carried out in a primary health care centre in a deprived neighbourhood of Barcelona, Spain.
Method
A total of 143 participants were assessed using the 12-item Short-Form Health Survey, the List of Threatening Experiences and the Duke Social Support scales. The effect of economic crisis on mental and physical HRQoL was assessed using ordinary least squares regression models to test the interaction between social support and having experienced an economic crisis.
Results
There was no statistical association between having suffered an economic crisis and physical HRQoL. The interaction between social support and economic crisis was also tested without finding any statistical association. An interaction was detected between social support and economic crisis in relation to mental HRQoL; those who had low levels of social support and had also experienced an economic crisis had the lowest levels of mental HRQoL.
Conclusion
Social support constitutes a safety net that offers protection against the adverse effect of economic recessions on mental health. Primary care professionals are in a key position to promote social activities and to strengthen social networks in the community.
Keywords: economic recession, health-related quality of life, primary care, social support
INTRODUCTION
Social support is an independent protective factor for health and there is increasing evidence for an increase in mortality associated with a lack of social relationships.1 Recession affects health by worsening health-related quality of life;2–4 increasing the incidence of some communicable diseases;5 and exacerbating mental ill health2,5–9 and increasing suicide rates.5,6 This impact is not direct, and can be buffered by the degree of social protection that the state offers.5,6,10 Some studies have reported an improvement in health status during periods of financial crisis, explained, for instance, by a reduction in smoking, drinking, and sedentary behaviours.6,11,12 However, if governments reduce public expenditure on social welfare and health services during a recession period, the impact can be worse.5,8,10 In this scenario, social support can be an important protective factor.6 Front-line healthcare workers, such as primary healthcare professionals, are in a key position to implement new strategies, based on identified protective factors, to ameliorate the impact of the economic crisis on the population.
The aim of this study was to estimate the impact of being personally affected by an economic crisis on the health-related quality of life of primary healthcare attendees, taking into account the possible buffering effect of perceived social support.
METHOD
Study design
The ‘Social Support and Quality of Life in primary care attendees from a deprived area of Barcelona’ study is a longitudinal study aiming to ascertain which factors (life events) are associated with changes in health-related quality of life (HRQoL), focusing on the buffering effect that perceived level of social support may have. The study began in March 2012. Written informed consent was obtained from participants. This article presents data from the first wave of this study (March 2012 to November 2012).
Setting
The area of the study is a neighbourhood in Sant Adrià de Besòs (Barcelona, Spain). This neighbourhood was established in the early 1970s with the aim of providing adequate housing facilities to internal migrants with low economic resources. They were provided with small apartments in an area that quickly became overcrowded. Data on social deprivation and the high prevalence of mental health problems in this environment have been published elsewhere.13 The population in 2012 was 9412 inhabitants (49% female). Twenty-one per cent were aged <15 years and 13% were >65 years. More than 5% of the population born between 1947 and 1993 are illiterate.14 Average income per capita in 2012 was €3626 (approximately £2845); in Catalonia, it was more than €9000 (approximately £7062).15 There is no available updated information on unemployment rates in the neighbourhood. However, the unemployment rate in this area has been estimated at more than 25%.16
How this fits in
Various studies have pointed out the negative impact of the economic recession on health and health-related quality of life. Social support and networks can be protective factors in times of economic recession. However, there is little evidence about the buffering effect of social support on the impact of the financial crisis on health-related quality of life. This study attempts to fill this gap. Data on individual protective factors in times of recession can help professionals to develop interventions to ameliorate its negative impact.
In Spain, access to health care is universal and free at the point of use. The primary care centre is the first point of access to the health system. It consists of a multidisciplinary team of GPs, nurses, paediatricians, and social workers. They are responsible for a broad range of services, including illness prevention and health promotion activities. All salaries include a capitation component.17 The GP:patient ratio is 1:1100. Appointment duration is approximately 8 minutes.
Sampling
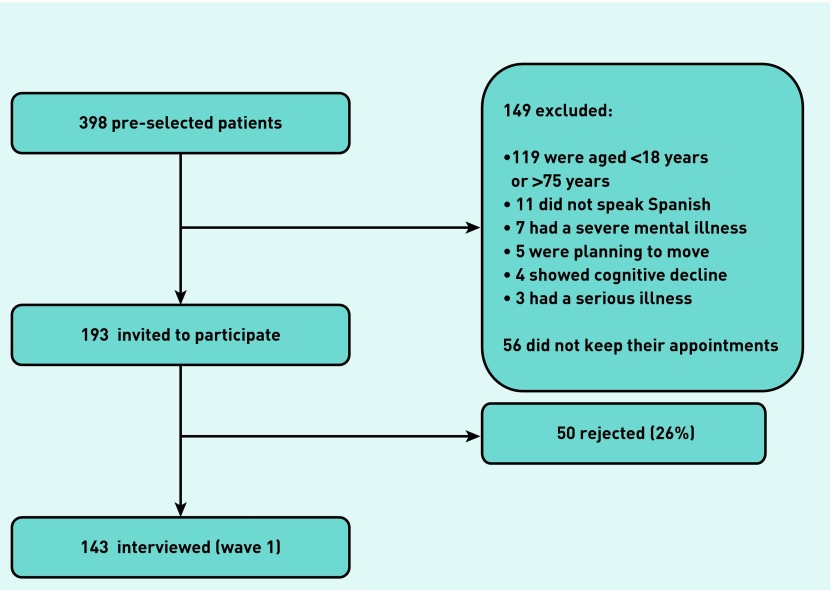
Six professionals from the primary care centre (two GPs, three nursing practitioners, and one social worker) invited patients to participate in the study from March 2012 to November 2012. Patients were selected through a systematic sampling strategy, inviting one of each four to six patients from their appointment lists at random starting points each day. Exclusion criteria are shown in Figure 1. A total of 398 patients were randomly selected. Of those, 149 were excluded and 56 did not keep their appointments. A total of 193 were invited to participate and 50 declined, leaving a study sample of 143 participants. This formed the initial cohort to be followed-up. Those who declined to participate were asked for permission to record their sex and age. There were no statistical differences between those who accepted by sex (52.2% of those who declined were female versus 67.8% of those who accepted; P = 0.06), or age (mean age of those who declined was 53.7 years versus 53.9 years for those who accepted; P = 0.97).
Figure 1.
Participants included in the Social Support and Quality of Life Study.
To maximise efficiency, a sequential analysis or sequential hypothesis testing strategy was followed. This means that sample size was not fixed in advance. Rather, data were analysed as they were collected and further participants were invited if needed.18 It is expected that when results are obtained from the second wave, it will be possible to calculate the power of the associations found and to determine whether an increase in sample size is required or not.
Measures
The outcome variable was HRQoL. HRQoL was assessed with the Spanish version 1.0 of the 12-item Short-Form Health Survey (SF-12). The SF-12 is a valid, reliable, and widely-used instrument for the assessment of HRQoL. Two measures were derived: a physical component summary scale (PCS-12) indicating physical quality of life, and a mental component summary scale (MCS-12) for mental quality of life. Each scale uses all 12 items but with different weights. PCS-12 and MCS-12 scales were scored using norm-based methods.19
Exposure variables were having experience a personal economic crisis and self-perceived social support.
Having experienced a personal economic crisis was measured as a positive response to one of the following questions: In the past 6 months:
Have you suffered an economic crisis? And/or
Have you been fired from your job? Or have you been looking for a job for more than a month without any success?
These two questions are part of the List of Threatening Experiences questionnaire.20–22 This questionnaire has been validated in Spanish primary care patients.22
Self-perceived social support was assessed using the Duke questionnaire,23–25 which included 11 items grouped into two subscales: confidant support and affective support; as well as a total score. The item response options are on a 5-point scale ranging from 1 (much less than I would like) to 5 (as much as I would like). Participants were coded into low social support if their total score was <30 points (1 standard deviation [SD] under the mean) and high social support (all the others). This questionnaire has been validated in Spanish primary care patients,25 showing good test–retest reliability and cohesiveness.
Statistical analysis
The effect of economic crisis on HRQoL was assessed using ordinary least squares (OLS) regression models. First, estimated parameters (β) were reported for the contribution of economic crisis alone to HRQoL. A second model adjusted for self-perceived social support. In the third model, a proxy of health status (that is, self-reporting a severe illness) was included. The fourth model was also adjusted for age and sex. Finally, the interaction between social support and having experienced an economic crisis was tested. Regression diagnostic tests were conducted to check the normality and homoscedasticity of residuals.
All analyses were carried out using Stata (version 12). All significance tests were carried out using two-sided tests evaluated at the 0.05 level of significance.
RESULTS
Of the 143 patients evaluated, 67.8% were female with a mean age of 54 years (SD = 16.60). Regarding HRQoL, mean values were 44.85 (SD = 13.07) for the physical component and 38.98 (SD = 14.36) for the mental component. In addition, nearly 22% (n = 31) of the sample self-reported a severe illness or injury in the previous 6 months. A total of 37.8% (n = 54) of the participants stated that in the previous 6 months they had experienced an economic crisis. The percentage of people reporting high self-perceived social support was 77.6% (n = 111).
Impact on physical health-related quality of life
Table 1 summarises the impact that an economic crisis was found to have on physical HRQoL. There was no statistical association between having experienced an economic crisis and physical HRQoL. The only factors that seemed to be associated with physical HRQoL were: self-reporting a severe illness in the previous 6 months (decrease more than 7 points), being male (increase 7 points), and age (as age increases, physical HRQoL decreases). In model 5, the interaction between social support and economic crisis was also tested without finding any statistical association. This last model explained 14.8% of the variance.
Table 1.
Factors associated with physical health-related quality of life
| Factor | Model 1: β (95% CI) | Model 2: β (95% CI) | Model 3: β (95% CI) | Model 4: β (95% CI) | Model 5: β (95% CI) |
|---|---|---|---|---|---|
| Having experienced an economic crisis | 3.48 (−0.95 to 7.92) | 3.57 (−0.90 to 8.04) | 3.95 (−0.48 to 8.38) | 2.03 (−2.77 to 6.83) | 3.66 (−1.74 to 9.05) |
| Having a low level of social support | −1.02 (−6.22 to 4.18) | −1.18 (−6.40 to 4.05) | −0.39 (−5.47 to 4.68) | 2.50 (−4.21 to 9.20) | |
| Being ill or injured during the previous 6 months | −5.44 (−10.65 to −0.24)a | −6.75 (−11.69 to −1.81)b | −6.37 (−11.34 to −1.41)a | ||
| Sex (reference female) | 7.14 (2.83 to 11.45)c | 7.19 (2.89 to 11.43)c | |||
| Age (median 57 years) | −0.15 (−0.29 to −0.02)a | −0.15 (−0.28 to −0.02)a | |||
| Interaction economic crisis AND low level of social support | −6.57 (−16.54 to 3.39) | ||||
| Constant term | 43.54 | 43.73 | 44.93 | 42.74 | 42.09 |
| Adjusted R2 | 0.98% | 0.38% | 2.89% | 14.38% | 14.82% |
P<0.05.
P<0.01.
P<0.001.
The Breusch–Pagan/Cook–Weisberg test for heteroscedasticity was not significant (P = 0.3142), suggesting that the variance of the error term was constant (one of the OLS’s assumptions). On the other hand, according to the Shapiro–Francia test of normality, the residuals did not fit a normal distribution (P = 0.02). This could affect the validity of the hypothesis tested.
Impact on mental health-related quality of life
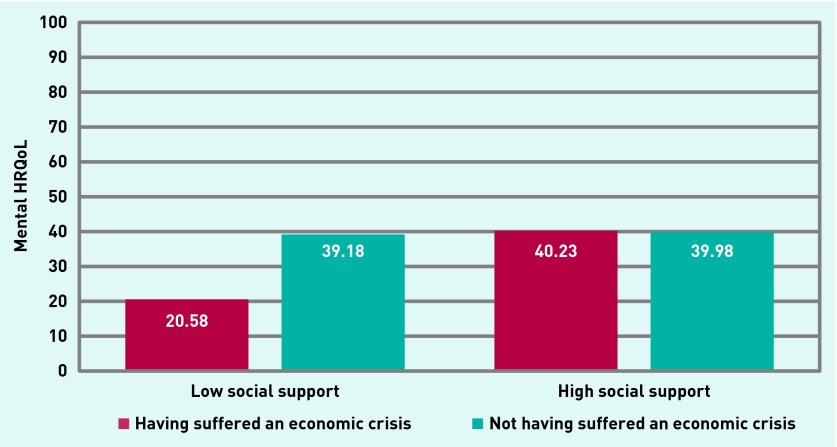
Economic crisis seemed to have an impact on the mental HRQoL of participants (Table 2). When tested alone, having experienced an economic crisis reduced HRQoL by more than 5 points. This association remained when adjusted for self-reporting of a severe illness (model 2). However, it disappeared when adjusted for age and sex (model 3). After testing the interaction between social support and economic crisis, only those who had low social support and had also experienced an economic crisis were found to have lower levels of mental HRQoL (model 5). This last model explained 20.2% of the variance. A graphic representation is provided in Figure 2.
Table 2.
Factors associated with mental health-related quality of life
| Factor | Model 1: β (95% CI) | Model 2: β (95% CI) | Model 3: β (95% CI) | Model 4: β (95% CI) | Model 5: β (95% CI) |
|---|---|---|---|---|---|
| Having experienced an economic crisis | −6.41 (−11.22 to −1.62)b | −5.73 (−10.44 to −1.03)a | −5.66 (−10.38 to −0.95)a | −4.43 (−9.77 to 0.91) | 0.25 (−5.53 to 6.02) |
| Having a low level of social support | −7.89 (−13.36 −2.42)b | −8.44 (−14.00 to −2.88)c | −9.09 (−14.74 −3.45)c | −0.80 (−7.98 to 6.37) | |
| Being ill or injured during the previous 6 months | −4.36 (−9.90 to 1.17) | −5.68 (−11.17 to −0.18)a | −4.60 (−9.91 to 0.71) | ||
| Sex (reference female) | 6.01 (1.22 to 10.81)a | 6.15 (1.55 to 10.76)b | |||
| Age (median 57 years) | 0.02 (−0.12 to 0.17) | 0.05 (−0.09 to 1.19) | |||
| Interaction economic crisis AND low level of social support | −18.85 (−29.53 to −8.17)d | ||||
| Constant term | 41.41 | 42.92 | 43.95 | 35.82 | 39.98 |
| Adjusted R2 | 4.06% | 8.67% | 9.39% | 13.62% | 20.23% |
P<0.05.
P<0.01.
P<0.005.
P<0.001.
Figure 2.
Effect of an economic crisis on mental health-related quality of life, according to level of social support (n = 143).
The Breusch–Pagan/Cook–Weisberg test for heteroscedasticity was not significant (P = 0.21), suggesting that the variance of the error term is constant. According to the Shapiro–Francia test of normality, the residuals fit a normal distribution (P = 0.06).
DISCUSSION
Summary
The results suggest that high levels of social support provided a buffer against the adverse effects of an economic recession on mental HRQoL in a deprived area of Barcelona (Spain). Nevertheless, neither social support nor economic crisis was related to physical HRQoL.
Strengths and limitations
This is the first project to examine the protective factor of social support in HRQoL during an economic recession using individual data. That is, taking into account whether the person has experienced the effects of recession or not, independently of the overall context. However, the results have to be interpreted with the following limitations in mind. First, the study used, as exposure variables, self-perceived measures of both having experienced an economic crisis and social support without any objective data. This could affect reliability. Second, the cross-sectional nature of the study means that is it not possible to assume that the reduction in mental HRQoL is a direct consequence of the interaction between having experienced an economic crisis and self-perceived social support. Third, this is a preliminary analysis of the first wave of a cohort study. As explained in the method section, the study is following a sequential analysis or sequential hypothesis testing strategy. As such, the data may not be powerful enough to detect differences at this point. Fourth, the data were analysed using OLS. The OLS assumptions had goodness-of-fit with the mental HRQoL model, but not at all with the physical model. Hence, results regarding physical HRQoL should be interpreted with caution. Last, the external validity of the data is very limited because of the particular characteristics of this neighbourhood.
Comparisons with existing literature
HRQoL scores based on the SF-12 are norm-based. This means that the expected value will be around 50. However, this study is being carried out in primary health care so lower values are expected as people visiting their GP or nurse practitioner are usually unwell. Studies conducted in different primary care settings using the SF-12 found mean values around 42–45, similar to the results of this study.26–28
The impact of recession on mental HRQoL has been reported by others, both in Spain8,9,29 and internationally.2,6,7,30,31 The consequences of recession (loss of employment and financial burden) generate stress that affects people’s mental health. The buffering effect of social support, ameliorating the impact of economic recession, has been suggested by others,6 although this is the first time that evidence of this has been found. That being said, various studies have shown that social support helps to moderate the impact of other acute and/or chronic health stressors.32,33
Regarding the impact of recession on physical HRQoL, the results of the current study are in line with those reported by Regidor et al in Spain,34 which also did not find a relationship. One possible explanation could be that an economic crisis takes longer to have an impact on physical health than on mental health.
Implications for practice
Identifying protective factors for HRQoL in a recession period is important to alleviate its impact. However, actions have to be conducted at multiple levels,1,35 from the individual to the state (welfare policies), while taking the role of primary care professionals into account. These professionals are in an ideal position to identify those with low levels of social support, referring them to appropriate social services and/or monitoring them. This could be especially important during times of recession because they constitute the most vulnerable population. Strategies that can increase the social resources of a community, such as social prescribing,36,37 can be included as health promotion activities in primary care.
In conclusion, the preliminary data suggest that the impact of an economic crisis on mental HRQoL is not direct but could be explained by the absence of social support. Taking this into account, more social and community-oriented primary care should be established.
Acknowledgments
We are grateful to Barcelona Primary Care Headquarters (Ambit d’Atenció Primària de Barcelona Ciutat) of the public Catalan Institute of Health (Institut Català de La Salut) for its support in recognition of this project though the XB 2012 call for research projects. We are also thankful to all the people who agreed to participate in this study without receiving any material compensation. We also thank Stephen Kelly for his help in English language editing. In loving memory of Alberto Ramos.
Funding
This project was partially funded by the Spanish Network of Primary Care Research ‘redIAPP,’ (RD06/0018/0017); funded by the Institute of Health Carlos III, Spanish Ministry of Health.
Ethical approval
This study was approved by the Jordi Gol i Gorina Ethic Committees.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davalos ME, French MT. This recession is wearing me out! Health-related quality of life and economic downturns. J Ment Health Policy Econ. 2011;14(2):61–72. [PubMed] [Google Scholar]
- 3.Vandoros S, Hessel P, Leone T, Avendano M. Have health trends worsened in Greece as a result of the financial crisis? A quasi-experimental approach. Eur J Public Health. 2013;23(5):727–731. doi: 10.1093/eurpub/ckt020. [DOI] [PubMed] [Google Scholar]
- 4.Zavras D, Tsiantou V, Pavi E, et al. Impact of economic crisis and other demographic and socio-economic factors on self-rated health in Greece. Eur J Public Health. 2013;23(2):206–210. doi: 10.1093/eurpub/cks143. [DOI] [PubMed] [Google Scholar]
- 5.Karanikolos M, Mladovsky P, Cylus J, et al. Financial crisis, austerity, and health in Europe. Lancet. 2013;381(9874):1323–1331. doi: 10.1016/S0140-6736(13)60102-6. [DOI] [PubMed] [Google Scholar]
- 6.Wahlbeck K, McDaid D. Actions to alleviate the mental health impact of the economic crisis. World Psychiatry. 2012;11(3):139–145. doi: 10.1002/j.2051-5545.2012.tb00114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costa G, Marra M, Salmaso S, Salute GAC. [Health indicators in the time of crisis in Italy]. [In Italian] Epidemiol Prev. 2012;36(6):337–366. [PubMed] [Google Scholar]
- 8.Roca M, Gili M, Garcia-Campayo J, García-Toro M. Economic crisis and mental health in Spain. Lancet. 2013;382(9909):1977–1978. doi: 10.1016/S0140-6736(13)62650-1. [DOI] [PubMed] [Google Scholar]
- 9.Gili M, Roca M, Basu S, et al. The mental health risks of economic crisis in Spain: evidence from primary care centres, 2006 and 2010. Eur J Public Health. 2013;23(1):103–108. doi: 10.1093/eurpub/cks035. [DOI] [PubMed] [Google Scholar]
- 10.McDaid D, Quaglio G, Correia de Campos A, et al. Health protection in times of economic crisis: challenges and opportunities for Europe. J Public Health Policy. 2013;34(4):489–501. doi: 10.1057/jphp.2013.35. [DOI] [PubMed] [Google Scholar]
- 11.Asgeirsdottir TL, Corman H, Noonan K, et al. Was the economic crisis of 2008 good for Icelanders? Impact on health behaviors. Econ Hum Biol. 2014;13:1–19. doi: 10.1016/j.ehb.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 12.Dávila Quintana CD, González López-Valcárcel B. [The economic crisis and health]. [In Spanish] Gac Sanit. 2009;23(4):261–265. doi: 10.1016/j.gaceta.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 13.Tizón JL, Ferrando J, Artigue J, et al. Neighborhood differences in psychoses: prevalence of psychotic disorders in two socially-differentiated metropolitan areas of Barcelona. Schizophr Res. 2009;112(1–3):143–148. doi: 10.1016/j.schres.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 14.Ajuntament de Sant Adrià de Besòs Anuari de Població. 2012. [Statistics] [In Spanish] http://www.sant-adria.net/serveis/padro_municipal_habitants_dades_estadistiques/anuari-de-poblacio-2012 (accessed 15 Jan 2015)
- 15.Barrimina Sociodemographic data on the residents of La Mina. 2014. [In Spanish]. http://barrimina.cat/castellano/mina11.htm (accessed 15 Jan 2015)
- 16.Statistical Institute of Catalonia (IDESCAT) Unemployment rates. 2014. [In Spanish] http://www.idescat.cat/emex/?id=081944&lang=es#h1fe000000000 (accessed 15 Jan 2015)
- 17.Borkan J, Eaton CB, Novillo-Ortiz D, et al. Renewing primary care: lessons learned from the Spanish health care system. Health Aff (Millwood) 2010;29(8):1432–1441. doi: 10.1377/hlthaff.2010.0023. [DOI] [PubMed] [Google Scholar]
- 18.Rogers MS, Chang AM, Todd S. Using group-sequential analysis to achieve the optimal sample size. BJOG. 2005;112(5):529–533. doi: 10.1111/j.1471-0528.2005.00479.x. [DOI] [PubMed] [Google Scholar]
- 19.Vilagut G, Valderas JM, Ferrer M, et al. [Interpretation of SF-36 and SF-12 questionnaires in Spain: physical and mental components]. [In Spanish] Med Clin (Barc) 2008;130(19):726–735. doi: 10.1157/13121076. [DOI] [PubMed] [Google Scholar]
- 20.Brugha T, Bebbington P, Tennant C, Hurry J. The List of Threatening Experiences: a subset of 12 life event categories with considerable long-term contextual threat. Psychological Medicine. 1985;15(1):189–194. doi: 10.1017/s003329170002105x. [DOI] [PubMed] [Google Scholar]
- 21.Brugha TS, Cragg D. The List of Threatening Experiences: the reliability and validity of a brief life events questionnaire. Acta Psychiatr Scand. 1990;82(1):77–81. doi: 10.1111/j.1600-0447.1990.tb01360.x. [DOI] [PubMed] [Google Scholar]
- 22.Motrico E, Moreno-Küstner B, de Dios Luna J, et al. Psychometric properties of the List of Threatening Experiences: LTE and its association with psychosocial factors and mental disorders according to different scoring methods. J Affect Disord. 2013;150(3):931–940. doi: 10.1016/j.jad.2013.05.017. [DOI] [PubMed] [Google Scholar]
- 23.Broadhead WE, Gehlbach SH, de Gruy FV, Kaplan BH. The Duke-UNC Functional Social Support Questionnaire. Measurement of social support in family medicine patients. Med Care. 1988;26(7):709–723. doi: 10.1097/00005650-198807000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Parkerson GR, Jr, Broadhead WE, Tse CK. Validation of the Duke Social Support and Stress Scale. Fam Med. 1991;23(5):357–360. [PubMed] [Google Scholar]
- 25.Bellón Saameño JA, Delgado Sánchez A, Luna del Castillo JD, Lardelli Claret P. [Validity and reliability of the Duke-UNC-11 questionnaire of functional social support] [In Spanish] Aten Primaria. 1996;18(4):153–156. 158–163. [PubMed] [Google Scholar]
- 26.Manuti B, Rizza P, Pileggi C, et al. Assessment of perceived health status among primary care patients in Southern Italy: findings from a cross-sectional survey. Health Qual Life Outcomes. 2013;11:93. doi: 10.1186/1477-7525-11-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pinto-Meza A, Fernández A, Fullana MA, et al. Impact of mental disorders and chronic physical conditions in health-related quality of life among primary care patients: results from an epidemiological study. Qual Life Res. 2009;18(8):1011–1018. doi: 10.1007/s11136-009-9522-y. [DOI] [PubMed] [Google Scholar]
- 28.Jayasinghe UW, Proudfoot J, Barton CA, et al. Quality of life of Australian chronically-ill adults: patient and practice characteristics matter. Health Qual Life Outcomes. 2009;7:50. doi: 10.1186/1477-7525-7-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bartoll X, Palència L, Malmusi D, et al. The evolution of mental health in Spain during the economic crisis. Eur J Public Health. 2014;24(3):415–418. doi: 10.1093/eurpub/ckt208. [DOI] [PubMed] [Google Scholar]
- 30.Ng KH, Agius M, Zaman R. The global economic crisis: effects on mental health and what can be done. J R Soc Med. 2013;106(6):211–214. doi: 10.1177/0141076813481770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giotakos O, Karabelas D, Kafkas A. [Financial crisis and mental health in Greece] [In Greek] Psychiatriki. 2011;22(2):109–119. [PubMed] [Google Scholar]
- 32.Moskowitz D, Vittinghoff E, Schmidt L. Reconsidering the effects of poverty and social support on health: a 5-year longitudinal test of the stress-buffering hypothesis. J Urban Health. 2013;90(1):175–184. doi: 10.1007/s11524-012-9757-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. [PubMed] [Google Scholar]
- 34.Regidor E, Barrio G, Bravo MJ, de la Fuente L. Has health in Spain been declining since the economic crisis? J Epidemiol Community Health. 2014;68(3):280–282. doi: 10.1136/jech-2013-202944. [DOI] [PubMed] [Google Scholar]
- 35.Economou M, Madianos M, Peppou LE, et al. Cognitive social capital and mental illness during economic crisis: a nationwide population-based study in Greece. Soc Sci Med. 2014;100:141–147. doi: 10.1016/j.socscimed.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 36.Cawston P. Social prescribing in very deprived areas. Br J Gen Pract. 2011;61(586):350. doi: 10.3399/bjgp11X572517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brandling J, House W. Social prescribing in general practice: adding meaning to medicine. Br J Gen Pract. 2009;59(563):454–456. doi: 10.3399/bjgp09X421085. [DOI] [PMC free article] [PubMed] [Google Scholar]