Abstract
BACKGROUND:
Although mirror pain occurs after cordotomy in patients experiencing unilateral pain via a referred pain mechanism, no studies have examined whether this pain mechanism operates in patients who have bilateral pain.
OBJECTIVE:
To assess the usefulness of cordotomy for bilateral pain from the viewpoint of increased pain or new pain caused by a referred pain mechanism.
METHODS:
Twenty-six patients who underwent percutaneous cordotomy through C1-C2 for severe bilateral cancer pain in the lumbosacral nerve region were enrolled. Pain was dominant on 1 side in 23 patients, and pain was equally severe on both sides in 3 patients. Unilateral cordotomy was performed for the dominant side of pain, and bilateral cordotomy was performed for 13 patients in whom pain on the nondominant side developed or remained severe after cordotomy.
RESULTS:
After unilateral cordotomy, 19 patients (73.1%) exhibited increased pain, which for 14 patients was as severe as the original dominant pain. After bilateral cordotomy, 7 patients (53.4%) exhibited new pain, which was located cephalad to the region rendered analgesic by cordotomy and was better controlled than the original pain. No pathological organic causes of new pain were found in any patient, and evidence of a referred pain mechanism was found in 3 patients after bilateral cordotomy.
CONCLUSION:
These results show that a referred pain mechanism causes increased or new pain after cordotomy in patients with bilateral pain. Nevertheless, cordotomy can still be indicated for patients with bilateral pain because postoperative pain is better controlled than the original pain.
KEY WORDS: Bilateral cordotomy, Bilateral pain, Increased pain, New pain, Referred pain, Unilateral cordotomy
Cordotomy, the interruption of nociceptive pathways in the anterolateral column, is effective in relieving cancer pain that cannot be controlled by drug therapy or nerve blocks.1-8 Cordotomy is best indicated in cases of unilateral pain, because unilateral cordotomy is associated with a low risk of serious complications.2-4,7,8 One potential complication, however, is the occurrence of spontaneous new pain in 6.5% to 73.3% of patients who experienced unilateral pain, with the new pain most commonly located in a mirror-image location contralateral to the site of the original pain.2,7,9-11 This new pain may be previously unrecognized pain resulting from organic causes, especially in patients with cancer that has infiltrated and metastasized to the other side.4 However, many researchers believe that a referred pain mechanism brought on by cordotomy plays an important role in the occurrence of new pain,2,10-16 because noxious stimulation applied to a region rendered analgesic by cordotomy can produce distinct pain in a spatially separate location where nociception is not disturbed.10,12,13 In a few cases, new pain has been shown to be referred pain from the originally painful region.14,16
New pain is an unpreventable complication resulting from the interruption of nociceptive pathways and is a major postoperative problem after unilateral cordotomy, although the speculative mechanisms causing new pain in patients who have unilateral pain after cordotomy are likely similar in patients experiencing bilateral pain. However, no studies have yet addressed this issue. We hypothesized that cordotomy causes increased pain or new pain through a referred pain mechanism. Therefore, we examined reports of pain in patients experiencing bilateral cancer pain after unilateral or bilateral cordotomy, paying special attention to a potential referred pain mechanism, to assess the usefulness of cordotomy for pain relief.
METHODS
Study protocols were reviewed and approved by the Ethical Committee of Ehime University School of Medicine (No. 1205018).
Patient Population
Twenty-six patients experiencing bilateral cancer pain who underwent percutaneous cordotomy through C1-C2 vertebral space at Ehime University Hospital and related hospitals from 1986 to 2009 were enrolled in this study. Cordotomy was indicated for patients with refractory severe cancer pain, but not for patients in poor general condition with a life expectancy less than 1 month or with symptoms of respiratory dysfunction.
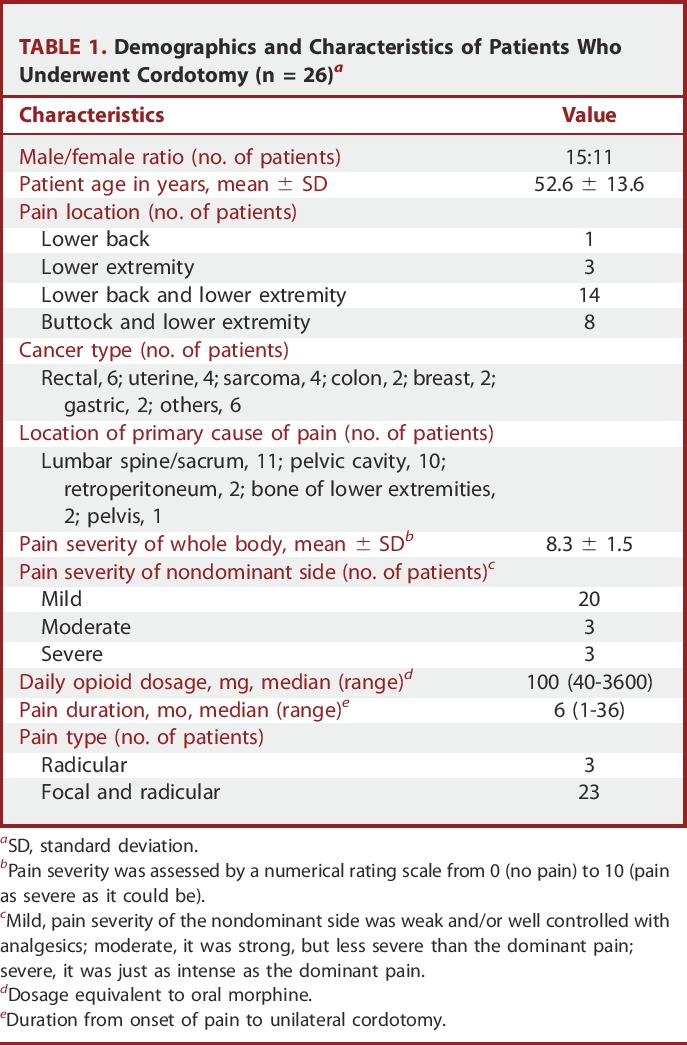
Demographics and characteristics of the patients are shown in Table 1. All patients had pain in the lower back, buttock, and/or lower extremity on both sides, with the pain located almost symmetrically. The primary cause of pain was metastasis or infiltration of cancer to the lumbar spine, sacrum, pelvis, pelvic cavity, and/or retroperitoneum, which was shown by plain x-ray and computed tomography (CT) scanning and was consistent with the occurrence of bilateral pain. Pain severity for the whole body, which was measured by a numerical rating scale ranging from 0 (no pain) to 10 (pain as severe as it could be), was above 7 for all patients. Pain severity was dominant on 1 side in 23 patients and about the same on both sides in 3 patients. Before cordotomy, the main pain treatment was administration of opioid medications via various routes. Activities of daily living were severely disturbed by pain and/or motor and sensory disturbance owing to nerve damage; performance status judged by World Health Organization classification was grade 3 (capable of only limited self-care) for 5 patients and grade 4 (completely disabled) for 21 patients.17
TABLE 1.
Demographics and Characteristics of Patients Who Underwent Cordotomy (n = 26)a
Unilateral (first) cordotomy was performed for the dominant side of pain. Bilateral (second) cordotomy was scheduled to perform in 14 of 26 patients in whom persistent severe pain on the nondominant side developed or continued after unilateral cordotomy, and it was performed in 13 patients, and was canceled to prevent respiratory failure in 1 patient in whom dyspnea occurred during electrical stimulation of the spinal cord. Bilateral cordotomy was performed between 7 and 57 days (median, 14 days) after unilateral cordotomy. The median period of follow-up and death after unilateral cordotomy in 26 patients was 56.5 days (range, 6-295 days) and 106 days (range, 15-319 days), respectively. The median period of follow-up and death after bilateral cordotomy in 13 patients was 42 days (range, 7-281 days) and 158.5 days (range, 16-308 days), respectively.
Cordotomy Procedures
Cordotomy was performed with fluoroscopic guidance for 21 patients and with CT guidance for the 5 most recent patients.3,18 Particular consideration was given to achieving pain relief with a small, selectively placed lesion. A Mullan-Portney electrode or thermocoupled Levin electrode (Radionics, Burlington, Massachusetts) was used. The electrode tip was located in the nociceptive pathway somatotopically corresponding to the lumber and sacral nerves (ie, just ventral of the dentate ligament) by fluoroscopic guidance or at the base of anterolateral column by CT guidance.19 The location of the electrode tip was also ascertained by electrical stimulation. Lesions were started with low currency (or temperature), which was gradually raised until the targeted painful region became analgesic to a strong pinprick by a 22-gauge disposable needle.
Characterization of Pain
New pain was defined as pain occurring in a region that was not painful preoperatively. Clinical features (onset time, location, nature, and severity) and the possible causes (existence of organic change or evidence of referred pain) of increased pain and new pain were examined. To clarify factors contributing to these pains, differences in patient characteristics, pain states before unilateral cordotomy (pain severity, opioid dosage, pain duration, and pain type), and results of cordotomy (pain relief and motor weakness) were analyzed between patients with and without increased or new pain. Organic changes that might have caused pain were examined retrospectively using available roentgenographic imaging data (plain x-ray or CT scanning) and interpreted by hospital radiologists. Referred pain was considered as when pinpricking and pinching the skin or other modes of stimulation or movements in the region rendered hypalgesic or analgesic by cordotomy evoked pain in a spatially separated location where nociception was not disturbed. Pain relief after unilateral or bilateral cordotomy was judged by the relief of pain on the opposite side of the cordotomy or on both sides, respectively, which was determined 1 week after each cordotomy. Motor weakness was evaluated by assessing grip strength in the hand ipsilateral to the cordotomy; a positive reduction was considered as more than a 25% reduction in grip strength immediately after cordotomy compared with that before the operation.
Postoperative pain treatments were mostly the same as those used preoperatively, with the dosages of analgesics adjusted in response to reports of pain. The severity of preoperative pain on the nondominant side and postoperative pain (partially relieved pain, recurrent pain, nondominant pain, increased pain, and new pain) was denoted as mild if it was weak and/or well controlled with or without analgesic agents, moderate if it was strong but less severe and better controlled than the original dominant pain, and severe if it was just as intense as the original dominant pain and could not be controlled.
Data Collection and Statistical Analysis
Data were collected retrospectively from medical records, which were obtained by interview or examination of patients daily during the first week after cordotomy and irregularly at least twice a week during the follow-up period. The unpaired Student t test was used for parametric data, the Mann-Whitney U test was used for nonparametric data, and the Fisher exact test was used for categorical data with the use of SPSS Version 20. A P value of less than .05 was considered statistically significant.
RESULTS
After unilateral cordotomy, 19 of 26 (73.1%) patients experienced increased pain, 7 patients experienced no change in pain severity, and no patients experienced new pain. By contrast, after bilateral cordotomy, new pain occurred in 7 of 13 (53.4%) patients.
Unilateral Cordotomy
Pain Relief
Unilateral cordotomy relieved the targeted pain in all 26 patients. Pain relief continued during the follow-up period in all patients except for 3, in whom mild pain reoccurred immediately after bilateral cordotomy that was undertaken 7, 19, and 57 days after unilateral cordotomy, respectively.
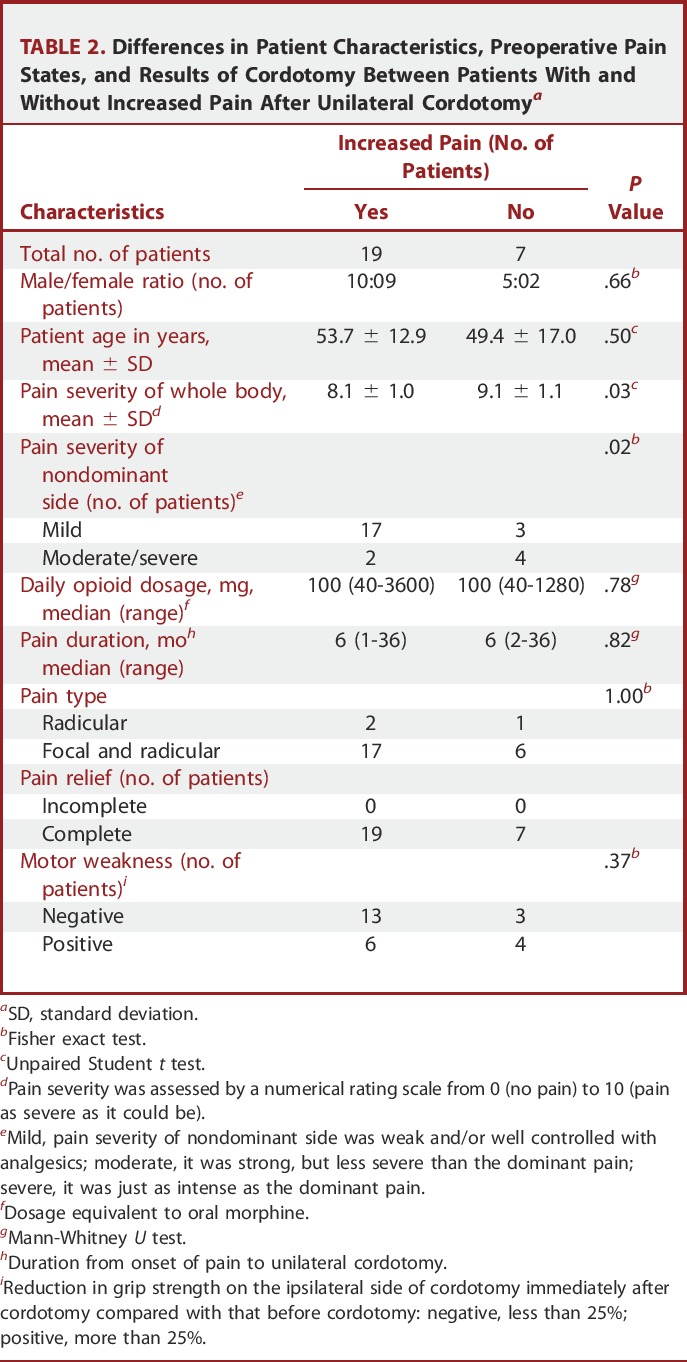
Increased Pain
Increased pain occurred immediately after cordotomy in 8 patients, within 1 day in 7 patients, and within 3 days in 4 patients. Pain severity increased gradually and became stable within 1 or 2 weeks in 16 patients, and it became severe immediately after cordotomy and subsided to mild within 1 day in 3 patients. As a result, mild pain on the nondominant side became severe in 9 patients, became moderate in 5 patients, and did not change in 3 patients; moderate pain on the nondominant side became severe in 2 patients and did not change in 1 patient; and severe pain on the nondominant side did not change in 3 patients.
The increased pain was qualitatively similar to that of the original pain in all patients. Referred pain was detected in 1 patient, in whom pinching of the whole area of skin that was rendered analgesic but not hypalgesic caused pain in a mirror position or more cephalad position on the contralateral side (case 39 in the study by Nagaro et al10).
Increased pain occurred more often in patients with mild pain on the nondominant side than in patients with moderate or severe pain on the nondominant side (17 of 20 vs 2 of 6, P = .02; Table 2).
TABLE 2.
Differences in Patient Characteristics, Preoperative Pain States, and Results of Cordotomy Between Patients With and Without Increased Pain After Unilateral Cordotomya
Bilateral Cordotomy
Pain Relief
Bilateral cordotomy relieved the targeted pain in 10 patients and partially relieved the targeted pain in 3 patients. The severity of partially relieved pain was mild in 2 patients and moderate in 1 patient. Its effect on pain relief did not change during the follow-up period.
New Pain
New pain was located cephalad to the region rendered analgesic or hypalgesic by bilateral cordotomy, where nociception was normal or slightly disturbed (right flank, 1 patient; right chest, 2 patients; left chest, 1 patient; precordium, 2 patients; nape, 1 patient; Figure 1). The new pain was qualitatively different from that of the original pain in all patients. New pain occurred immediately after bilateral cordotomy in 2 patients and 1 to 19 days after bilateral cordotomy in 5 patients (median, 3 days; range, 0-19 days). In 2 patients, the new pain was mild and disappeared within 3 weeks and 2 months after bilateral cordotomy, respectively. In 5 patients, the new pain (mild, 2 patients; moderate, 3 patients) continued until death or loss of spinal cord function due to tumor infiltration (median, 116 days; range, 36-169 days). No abnormal findings with regard to the new pain were revealed by roentgenographic examination for any patients (plain x-ray, 4 patients; CT scanning, 3 patients). Evidence of referred pain was found for 3 patients (cases 39, 67, and 82; Figure 1) and not found for 4 patients. One of the patients who showed evidence of referred pain was the previously mentioned patient in whom referred pain was observed after unilateral cordotomy; pinching of the skin rendered analgesic on both sides caused new pain in the left chest area (case 39; Figure 1). For the other 2 patients, referred pain was observed after bilateral cordotomy but not after unilateral cordotomy; movements of the lower extremities, but not pinching of the skin rendered analgesic, provoked or increased new pain in the precordium. In 2 of the 3 patients with referred pain (cases 39 and 67; Figure 1), relief or reduction of the new pain was obtained by lumbar epidural block, which produced hypoesthesia or anesthesia below the lower abdominal wall.
FIGURE 1.
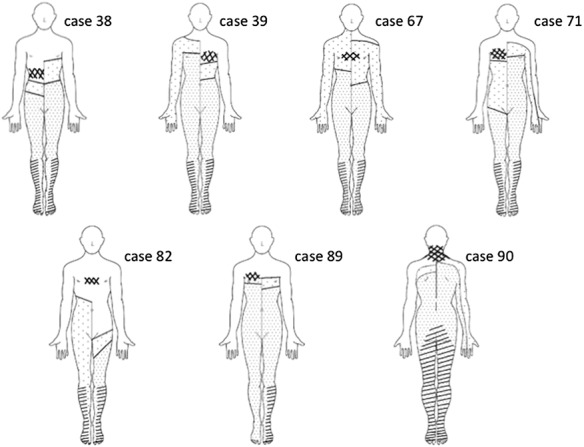
Schematic diagram showing pain locations in 7 patients who exhibited new pain after bilateral cordotomy. The cross-hatched area denotes the region of new pain. The hatched area denotes the region of original pain before cordotomy. The heavily and lightly spotted areas denote the regions rendered analgesic and hypalgesic, respectively, by unilateral and bilateral cordotomy. The case numbers are the same as those used throughout the study by Nagaro et al.10
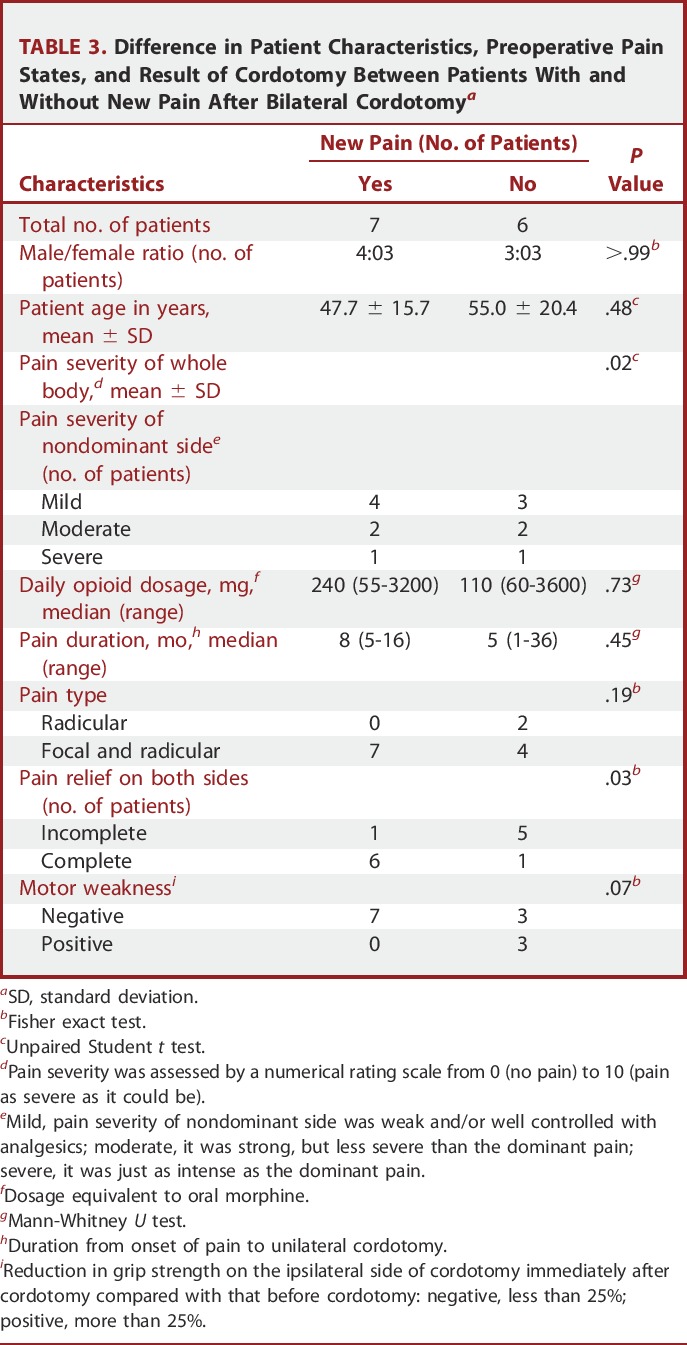
New pain occurred more often in patients with complete relief of the original pain on both sides (6 of 7 patients) than in patients with lingering concerns of original pain (ie, incompletely relieved pain or reoccurrence of pain; 1 of 6 patients; P = .03; Table 3).
TABLE 3.
Difference in Patient Characteristics, Preoperative Pain States, and Result of Cordotomy Between Patients With and Without New Pain After Bilateral Cordotomya
Other Complications
Motor weakness occurred after unilateral cordotomy in 10 of 26 patients; grip strength was reduced by 25% to 50% in 6 patients, by 50% to 75% in 3 patients, and by 75% to 100% in 1 patient. Motor weakness occurred after bilateral cordotomy in 3 of 13 patients; grip strength was reduced by 25% to 50% in all 3 of these patients. Motor function was restored to a degree without disability within 2 weeks for all patients except 2, in whom apparent hemiparesis after unilateral cordotomy continued during the follow-up period (15 and 73 days after cordotomy, respectively). General fatigue occurred within a few days after unilateral cordotomy in 5 patients and after bilateral cordotomy in 5 patients; this fatigue subsided within 1 week. Dysesthesia in the region that had been painful before unilateral cordotomy and was rendered analgesic by unilateral cordotomy occurred in 3 patients, 1, 6, and 15 days after cordotomy, respectively. Dysesthesia in the region that had been painful before bilateral cordotomy and was rendered analgesic by bilateral cordotomy occurred immediately or within 1 day after bilateral cordotomy in all 3 patients in whom dysesthesia occurred after unilateral cordotomy. Mild dysesthesia after unilateral cordotomy increased its severity after bilateral cordotomy in all 3 patients in whom there was no difference in the severity and nature of the dysesthesia on the 2 sides, and it became severe and intolerable in 1 patient. Dysesthesia spread to the entire region (below Th12) rendered analgesic by bilateral cordotomy in 1 patient within 2 months after bilateral cordotomy. This dysesthesia remained throughout the follow-up period or until death (48, 167, and 240 days after bilateral cordotomy, respectively). Spontaneous urination was not disturbed after unilateral cordotomy in 4 patients or after bilateral cordotomy in 1 patient who urinated without a catheter. Physical status deteriorated from grade 3 to 4 in 2 patients after unilateral cordotomy because of hemiparesis and did not change from grade 4 after bilateral cordotomy in any patient. No respiratory failure occurred in any patient.
Differences Between Fluoroscopic and CT Guidance Methods
Thirty cordotomies (21 unilateral, 9 bilateral) for 21 patients were performed under fluoroscopic guidance, and 9 cordotomies (5 unilateral, 4 bilateral) for 5 patients were performed under CT guidance. No complications were encountered by using the CT guidance method. Motor weakness occurred more frequently after fluoroscopic-guided cordotomy than after CT-guided cordotomy (13 of 30 vs 0 of 9, P = .02). There was no difference in the occurrence of new pain or increased pain (8 of 9 vs 18 of 30, P = .23) or in the occurrence of relief from the targeted pain (8 of 9 vs 28 of 30, P = .56, respectively) between fluoroscopic and CT guidance.
DISCUSSION
This is the first comprehensive report on increased pain and new pain after cordotomy in patients with bilateral cancer pain.
Increase in Pain After Unilateral Cordotomy
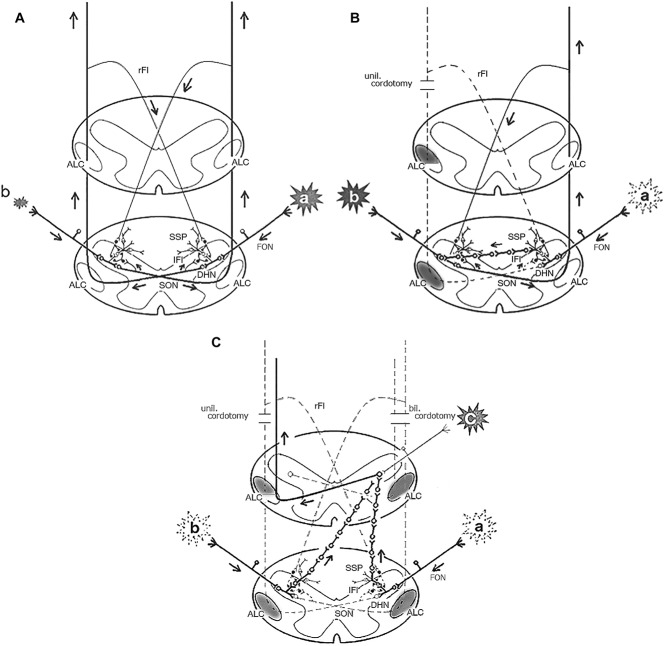
We found that most patients with bilateral pain before cordotomy (73.1%) experienced an increase in pain that existed before cordotomy on the nondominant side but no new pain after unilateral cordotomy. This finding is in contrast to the previous finding that up to 73.3% of patients with unilateral pain before cordotomy experienced new pain after unilateral cordotomy.2,7,9-11 This suggests that increased pain shares a common underlying neural mechanism with new pain (ie, a referred pain mechanism; Figure 2A and B). The similarity between the clinical features (rate, frequency, onset time, and location) of increased pain and new pain supports this idea.11 A distinct difference between increased pain and new pain after unilateral cordotomy is its severity; increased pain is as severe as the original pain in half of patients, but new pain is temporary or weaker than the original pain in most patients.9,11 This difference might result from organic changes in the nondominant side, such as the transmission of noxious input into ipsilateral spinal dorsal horn neurons and their resulting sensitization.10,20,21 An increase in pain severity in most of the patients who underwent unilateral cordotomy, especially among those with pain that was originally mild, shows that this treatment is not of much benefit to many patients experiencing bilateral pain.
FIGURE 2.
Schematic diagram of the proposed mechanism of increased pain and new pain after cordotomy in patients experiencing bilateral pain. A, the stream (←) of noxious impulses and feedback inhibition in the subsidiary pathway (SSP) under normal conditions. Noxious impulses travel up the nociceptive pathway along the anterolateral column (ALC) on the opposite side. The SSP is inhibited by reflected (rFI) and/or local feedback inhibition (lFI). Pain is felt at the lesion on both sides (“a” and “b”), and its severity correlates with the magnitude of noxious input from each lesion. The size of the sparkle corresponds to the severity of pain. FON, first-order neuron; DHN, dorsal horn neuron; SON, second-order neuron. B, release of feedback inhibition by unilateral (unil.) cordotomy and the stream (←) of noxious impulses underlying increased pain. Unilateral cordotomy stops the input from the dominant side of pain “a” from traveling up the usual pathway and releases feedback inhibition on SSP synapses via FONs innervating “a.” The input from “a” is thus transmitted through the SSP and converges on the DHNs corresponding to “b,” thereby increasing pain at “b.” C, release of feedback inhibition by bilateral (bil.) cordotomy and the stream (←) of noxious impulses underlying new pain. Bilateral cordotomy for the increased pain at “b” stops the input from “b” from traveling up the usual pathway and releases feedback inhibition on SSP synapses via FONs innervating “b.” The input from “a” and “b” thus ascends the SSP and converges on the most caudally located DHNs corresponding to “c,” thereby causing new pain at “c.”
New Pain After Bilateral Cordotomy
New pain occurred cephalad to the region rendered analgesic or hypalgesic by bilateral cordotomy. A few previous reports have described new pain in similar locations after bilateral cordotomy. Peet22 observed new pain in 6 of 18 patients after open thoracic cordotomy, Nathan2 described new pain after open cordotomy but did not mention its incidence, and Ischia et al5 reported new pain in 1 of 34 patients after percutaneous cordotomy. However, these reports did not provide detailed descriptions of clinical features or causes of new pain. Other studies describing the outcomes of bilateral cordotomy did not mention new pain, presumably because it might have been attributed to the surgical wound, nerve root damage during the operation, organic pathological changes, or unknown causes.4,23-27
The mechanism by which previously unrecognized pain becomes apparent after relief from severe pain is likely not the same as the mechanism of new pain, as the new pain was located far from the original pain, and no pathological changes were observed through roentgenography, although subtle organic changes or functional disorders might have caused the new pain. Evidence of referred pain suggests that the new pain was referred from the originally painful region. Furthermore, the absence of evidence of referred pain does not exclude a role of a referred pain mechanism, because the noxious stimulus produced by cancer causes referred pain more easily than other stimulations such as pinching or pinpricking the skin.16 The emergence of evidence of referred pain after bilateral cordotomy in patients with no such evidence after unilateral cordotomy suggests that bilateral cordotomy facilitates the occurrence of referred pain.
The results of the present study indicate that an important contributing factor to the occurrence of new pain is the relief of original pain on both sides after bilateral cordotomy. This is consistent with the occurrence of new pain after unilateral cordotomy, which is associated with pain relief and analgesia at the target area.11 The neural mechanism underlying referred pain following unilateral cordotomy may be extended to that underlying new pain following bilateral cordotomy (Figure 2C); noxious input from the originally painful regions on both sides ascends (via the subsidiary pathway released by cordotomy) and converges on the most caudally located dorsal horn neurons innervated by intact second-order neurons, causing referred pain that is felt just above the region rendered analgesic by cordotomy.10
Other Complications After Cordotomy
Cordotomy can cause complications related to spinal pathways located close to or intertwined with the nociceptive pathway.1-8 Thus, it is noteworthy that complications caused by the interruption of nonnociceptive pathways were not observed in the 5 patients who underwent CT-guided cordotomy (4 of whom underwent bilateral cordotomy). Therefore, the present study shows that proper procedures and patient selection can prevent the occurrence of serious complications (eg, respiratory failure, hemiparesis, urinary dysfunction) even after bilateral cordotomy, at least for patients experiencing pain in the lower half of their body.
Usefulness of Cordotomy for Bilateral Pain
Increased pain, new pain, and dysesthesia arising from the interruption of nociceptive pathways are unpreventable and intrinsic complications of cordotomy. Increased pain occurs in most patients experiencing bilateral pain after unilateral cordotomy, and new pain occurs in most patients in whom original pain on both sides was relieved by bilateral cordotomy. However, severe increased pain after unilateral cordotomy can be relieved by bilateral cordotomy, and new pain after bilateral cordotomy is weaker and better controlled than the original pain in most patients. Thus, cordotomy may be useful for treating bilateral pain if bilateral cordotomy is performed to address severe pain occurring on the opposite side of the pain that was relieved by unilateral cordotomy.
Dysesthesia is a well recognized complication of cordotomy, with a reported incidence of around 15%.28 In the present study, dysesthesia that occurred shortly after cordotomy in the region where pain was located before cordotomy might have been caused by a damaged peripheral nerve that was present preoperatively but was not conspicuous because of the overriding pain. Dysesthesia that spread over the entire region rendered analgesic by cordotomy might have been caused by the destruction of second-order neurons in the nociceptive pathway.28 It is remarkable that dysesthesia occurred in the side rendered analgesic by bilateral cordotomy in the patients in whom dysesthesia occurred following unilateral cordotomy, and that the dysesthesia increased in severity following bilateral cordotomy. The occurrence of dysesthesia in each region rendered analgesic after unilateral and bilateral cordotomy suggests that the dysesthesia may have occurred in patients prone to dysesthesia. Dysesthesia following unilateral cordotomy is clinically important, because it may forecast that dysesthesia occurs in the region rendered analgesic by bilateral cordotomy, and dysesthesia increases in severity after bilateral cordotomy. This observation suggests that we must be prudent in our decision to perform bilateral cordotomy in patients in whom dysesthesia occurs after unilateral cordotomy.
The degree of patient satisfaction and the influence of cordotomy on patients' quality of life were not investigated in this study. However, we believe that most patients, except for 1 patient who had severe dysesthesia and moderate new pain after bilateral pain relief, were satisfied with cordotomy, because they experienced a decrease in pain and stated that undergoing the procedure was beneficial.
Limitations
This study has some limitations. In particular, this study was performed retrospectively with a small number of patients; therefore, a prospective study including a larger number of patients is necessary for confirming our findings. Also, cordotomy procedures and follow-up periods took place between 1986 and 2009. Cordotomy is indicated for any case in which refractory severe pain is not relieved with less invasive methods. However, because of recent advances in cancer treatment and the management of cancer pain, the number of patients requiring cordotomy has decreased, and the characteristics of patients indicated for cordotomy has changed across this time period. Therefore, the results of our study may not be entirely applicable to the current clinical situation.
CONCLUSION
Our results indicate that most patients with bilateral cancer pain exhibit increased pain after unilateral cordotomy and new pain after bilateral cordotomy through the mechanism of referred pain from the originally painful region. Nevertheless, it is our opinion that bilateral cordotomy can be indicated for patients with uncontrollable bilateral pain, because severe increased pain after unilateral cordotomy can be relieved by bilateral cordotomy, and new pain after bilateral cordotomy is weaker and better controlled than the original pain.
Disclosure
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Acknowledgment
The authors thank Naomi Kazatani for editorial assistance.
COMMENT
This study provides a good documentation of 23 cancer patients presenting with bilateral severe pain treated with cordotomy between 1986 and 2009. This is the first comprehensive report on the status of pain and new pain after a cordotomy for bilateral pain. The potential mechanism of action is schematically reviewed. The difference between the results under fluoroscopy and CT guidance is also documented.
Despite better pharmacological options for patients who have cancer, the cordotomy remains a viable option when needed.
Line Jacques
San Francisco, California
CME QUESTIONS:
-
When performing a percutaneous cordotomy for chronic refractory lower body pain, through which intervertebral space is this procedure performed?
A. C1-2
B. C2-3
C. C3-4
D. C4-5
E. C5-6
-
What is a contraindication for bilateral percutaneous cordotomy in the treatment of chronic refractory pain?
A. Pain associated with tumor compression of a peripheral nerve
B. Life expectancy of < 6 months
C. Severe pulmonary dysfunction
D. Unilateral upper extremity pain
-
What type of pain is best treated by percutaneous cordotomy?
A. Phantom limb
B. Cancer-related
C. Failed back
D. Central post stroke (CPSP)
E. Complex regional (CRPS)
REFERENCES
- 1.Spillar WG. The occasional clinical resemblance between caries of the vertebra and lumbothoracic syringomyeria, and the location within the spinal cord of the fibers for sensations of pain and temperature. Univ Pa Med Bull. 1905;18:147-154. [Google Scholar]
- 2.Nathan PW. Results of antero-lateral cordotomy for pain in cancer. J Neurol Neourosurg Psychiatry. 1963;26:353-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosomoff HL, Brown CJ, Sheptak P. Percutaneous radiofrequency cervical cordotomy: technique. J Neurosurg. 1965;23(6):639-644. [DOI] [PubMed] [Google Scholar]
- 4.White JC, Sweet WH. Pain and the Neurosurgeon. Springfield, MA: Charles C Thomas; 1969. [Google Scholar]
- 5.Ischia S, Luzzani A, Ischia A, Maffezzoli G. Bilateral percutaneous cervical cordotomy: immediate and long-term results in 36 patients with neoplastic disease. J Neurol Neurosurg Psychiatry. 1984;47(2):141-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raslan AM, Cetas JS, McCartney S, Burchiel KJ. Destructive procedures for control of cancer pain: the case for cordotomy. J Neurosurg. 2011;114(1):155-170. [DOI] [PubMed] [Google Scholar]
- 7.Sanders M, Zuurmond W. Safety of unilateral and bilateral percutaneous cervical cordotomy in 80 terminally ill cancer patients, J Clin Oncol. 1995;13(6):1509-1512. [DOI] [PubMed] [Google Scholar]
- 8.Vissers KC, Besse K, Wagemans M, et al. 23. Pain in patients with cancer. Pain Pract. 2011;11(5):453-475. [DOI] [PubMed] [Google Scholar]
- 9.Ischia S, Ischia A, Luzzani A, Toscano D, Steele A. Results up to death in the treatment of persistent cervico-thoracic (pancoast) and thoracic malignant pain by unilateral percutaneous cervical cordotomy. Pain. 1985;21(4):339-355. [DOI] [PubMed] [Google Scholar]
- 10.Nagaro T, Amakawa K, Kimura S, Arai T. Reference of pain following percutaneous cervical cordotomy. Pain. 1993;53(2):205-211. [DOI] [PubMed] [Google Scholar]
- 11.Nagaro T, Adachi N, Tabo E, Kimura S, Arai T, Dote K. New pain following cordotomy: clinical features, mechanisms, and clinical importance. J Neurosurg. 2001;95(3):425-431. [DOI] [PubMed] [Google Scholar]
- 12.Ray BS, Wolff HG. Studies on pain “spread of pain”; evidence on site of spread within the neuraxis of effects of painful stimulation, Arch Neurol Psychiatry. 1945;53:257-261. [Google Scholar]
- 13.Nathan PW. Reference of sensation at the spinal cord level. J Neurol Neurosurg Psychiatry. 1956;19(2):88-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nagaro T, Kimura S, Arai T. A mechanism of new pain following cordotomy; reference of sensation. Pain. 1987;30(1):89-91. [DOI] [PubMed] [Google Scholar]
- 15.Bowsher D. Contralateral mirror-image pain following anterolateral cordotomy. Pain. 1988;33(1):63-65. [DOI] [PubMed] [Google Scholar]
- 16.Nagaro T, Amakawa K, Arai T, Ochi G. Ipsilateral referral of pain following cordotomy. Pain. 1993;55(2):275-276. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. WHO Handbook for Reporting Results of Cancer Treatment. Offset Publ., no.48. Geneva, Switzerland: WHO; 1979. [Google Scholar]
- 18.Kanpolat Y, Ugur HC, Ayten M, Elhan AH. Computed tomography-guided percutaneous cordotomy for intractable pain in malignancy. Neurosurgery. 2009;64(3 suppl):187-193. [DOI] [PubMed] [Google Scholar]
- 19.Lahuerta J, Bowsher D, Lipton S, Buxton PH. Percutaneous cervical cordotomy: a review of 181 operations on 146 patients with a study on the location of “pain fibers” in the C-2 spinal cord segment of 29 cases. J Neurosurg. 1994;80(6):975-985. [DOI] [PubMed] [Google Scholar]
- 20.Shimoyama M, Tatsuoka H, Ohtori S, Tanaka K, Shimoyama N. Change of dorsal horn neurochemistry in a mouse model of neuropathic cancer pain. Pain. 2005;114(1-2):221-230. [DOI] [PubMed] [Google Scholar]
- 21.Khasabov SG, Hamamoto DT, Harding-Rose C, Simone DA. Tumor-evoked hyperalgesia and sensitization of nociceptive dorsal horn neurons in a murine model of cancer. Brain Res. 2007;1180:7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peet MM. The control of intractable pain in lumbar region, pelvis and lower extremities by section of the anterolateral columns of the spinal cord (chordotomy). Arch Surg. 1926;13:153-204. [Google Scholar]
- 23.Rosomoff HL. Bilateral percutaneous cervical radiofrequency cordotomy. J Neurosurg. 1969;31(1):41-46. [DOI] [PubMed] [Google Scholar]
- 24.Amano K, Kawamura H, Tanikawa T, et al. Bilateral versus unilateral percutaneous high cervical cordotomy as a surgical method of pain relief. Acta Neurochir Suppl (Wien). 1991;52:143-145. [DOI] [PubMed] [Google Scholar]
- 25.Yegul I, Erhan E. Bilateral CT-guided percutaneous cordotomy for cancer pain relief. Clin Radiol. 2003;58(11):886-889. [DOI] [PubMed] [Google Scholar]
- 26.Bekar A, Kocaeli H, Abaş F, Bozkurt M. Bilateral high-level percutaneous cervical cordotomy in cancer pain due to lung cancer: a case report. Surg Neurol. 2007;67(5):504-507. [DOI] [PubMed] [Google Scholar]
- 27.Atkin N, Jackson KA, Danks RA. Bilateral open thoracic cordotmy for refractory cancer pain: a neglected technique?. J Pain Symptom Manage. 2010;39(5):924-929. [DOI] [PubMed] [Google Scholar]
- 28.Nagaro T, Oka S, Amakawa K, et al. Classification of postcordotomy dysesthesia [In Japanese]. Masui. 1994;43(9):1356-1361. [PubMed] [Google Scholar]