Abstract
Background
The present study sought to clarify the development of comorbid emotional distress by comparing different explanations for how youth develop anxiety and depressive symptoms. Specifically, we introduced the diathesis-anxiety approach (whether cognitive vulnerabilities interact with anxiety symptoms), and compared it to a causal model (anxiety symptoms predicting depressive symptoms), and a correlated liabilities model (whether cognitive vulnerabilities interacted with stressors to predict both anxiety and depressive symptoms) to examine which model best explained the relation between depressive and anxiety symptoms in youth.
Methods
678 3rd (n=208), 6th (n=245), and 9th (n=225) grade girls (n=380) and boys (n=298) completed self-report measures at baseline assessing cognitive vulnerabilities (rumination and self-criticism), stressors, depressive and anxiety symptoms. Every 3 months over the next 18 months, youth completed follow-up measures of symptoms and stressors.
Results
While limited support was found for a causal (p > .10) or correlated-liability model (p > .05) for comorbidity, findings did support a diathesis-anxiety approach for both self-criticism (t(2494) = 3.36, p < .001) and rumination (t(2505) = 2.40, p < .05).
Limitations
The present study’s findings are based on self-report measure and makes inferences concerning comorbidity with a community sample.
Conclusions
These results may help clarify past research concerning comorbidity by introducing a diathesis-anxiety approach as a viable model to understand which youth are most at-risk for developing comorbid emotional distress.
Keywords: Youth, Anxiety, Depression, Comorbidity, Developmental Psychopathology
Introduction
Comorbidity, defined as the manifestation of multiple disorders within the same individual (Seligman & Ollendick, 1998), has become the rule rather than the exception with regard to psychopathology (Angold, Costello, & Erkanli, 1999; Essau & Chang, 2009). The most common combination of disorders in youth is depression and anxiety (Angold et al., 1999; Merikangas et al., 2010), with up to 75% of depressed youth experiencing symptoms of anxiety (Essau & Chang, 2009). Experiencing comorbid emotional distress predicts a more severe course of mental illness (Mineka, Watson, & Clark, 1998; Rohde, Lewinsohn, & Seeley, 1991; Starr & Davila, 2008) and poorer treatment response (Ollendick, Jarrett, Grillis-Taquechel, Hovey, & Wolff, 2008; Westen, Novotny, & Thompson-Brenner, 2004; Young, Mufson, & Davies, 2006) compared to experiencing just depression or anxiety alone. Thus, researchers have aimed to understand the developmental underpinnings of these comorbid internalizing disorders to develop more targeted interventions for these distressed youth.
Despite increased attention over the past 25 years on the comorbidity between depression and anxiety (Angold & Costello, 1993; Merikangas et al., 2010; Seligman & Ollendick, 1998), there is still a great deal of uncertainty over why these two disorders are so highly comorbid. Systematic investigations into the relation between the two disorders have largely been guided by two influential theories: the tripartite model of anxiety and depression (see Clark & Watson, 1991 for explanation) and the cognitive content-specificity hypothesis (see Beck, 1976 for explanation). Although originally developed and tested within the context of adulthood, these two theories have been extended downward to youth. However, studies on both the tripartite model (Anderson & Hope, 2008; Laurent & Ettleson, 2001) and the cognitive content-specificity hypothesis (Epkins, 1996; Garber, Weiss, & Shanley, 1993; Jolly, 1993; Schniering & Rapee, 2004) have produced mixed findings concerning comorbid symptoms in children and adolescents. Given the inconsistent support for these two traditional explanations for comorbidity, alternative theories need to be explored.
In reviewing how two disorders may relate, Neale and Kendler (1995) propose twelve different models which may explain high rates of comorbidity between disorders. Overall, Neale and Kendler’s (1995) approach to modeling comorbid psychopathology has become a recommended methodology to understand how two disorders coexist (Krueger & Markon, 2006) and serves as a useful tool for testing competing hypotheses for how depression and anxiety relate. However, despite these advantages, few studies have explicitly and adequately tested these different models with regard to depression and anxiety. In order to adequately test the different models posited by Neale and Kendler (1995), data must be collected over time and include multiple follow-ups to understand the causal principles outlined in several of the models (Middeldorp, Cath, Van Dyck, & Boomsma, 2005).
To date, only three of the 215 empirical articles that have cited Neale and Kendler’s (1995) article have explicitly tested competing models within a multi-wave, longitudinal framework with regard to depression and anxiety. While initial investigations indicated support for a correlated liabilities model, in which anxiety and depression are predicted by shared risk factors (Klein, Lewinsohn, Rohde, Seeley, & Shankman, 2003; Rice, van den Bree, & Thapar, 2004), a more recent investigation found support for both a correlated liabilities model, and a causal model, in which anxiety leads to depression. Specifically, Matthew, Pettit, Lewinsohn, Seeley, and Roberts (2011) found that when anxiety precedes depression, a causal model best explains the relation between depression and anxiety in late adolescents and young adults; however, when a depressive episode precedes anxiety a correlated liabilities approach is the best explanation. This finding by Matthew and colleagues (2011) is consistent with other past research which has also found multiple pathways for developing comorbid emotional distress (Avenvoli, Stolar, Li, Dierker, & Merikangas, 2001).
The present study sought to build upon this research by utilizing a multi-wave (6 assessments every 3 months), longitudinal (over the course of 18 months) study, which is a recommended approach for testing theories related to developmental psychopathology (Willett, Singer, & Martin, 1998). The above studies which simultaneously tested Neale and Kendler’s (1995) models were either family or epidemiological studies which are important for showing the course of clinical disorders across the lifespan, but the length of time between follow-ups may make it more difficult to detect subtle changes in symptom fluctuations, important life events, and potential moderators (Abela & Hankin, 2008). Relatedly, the present study utilized a dimensional approach to conceptualizing psychopathology, as opposed to the categorical (diagnostic) approach used in epidemiological/family studies. While a categorical approach can include important clinical information, utilizing a dimensional approach for depression and anxiety may allow a better understanding of the full spectrum of internalizing symptoms, including the development of sub-threshold symptoms of emotional distress which may be missed using a classification systems (Krueger & Finger, 2001). In addition, the present study focused on late childhood and adolescence, which allowed our hypotheses to be tested during a critical period with regard to the emergence of internalizing symptoms (Abela & Hankin, 2008; Morris & March, 2004).
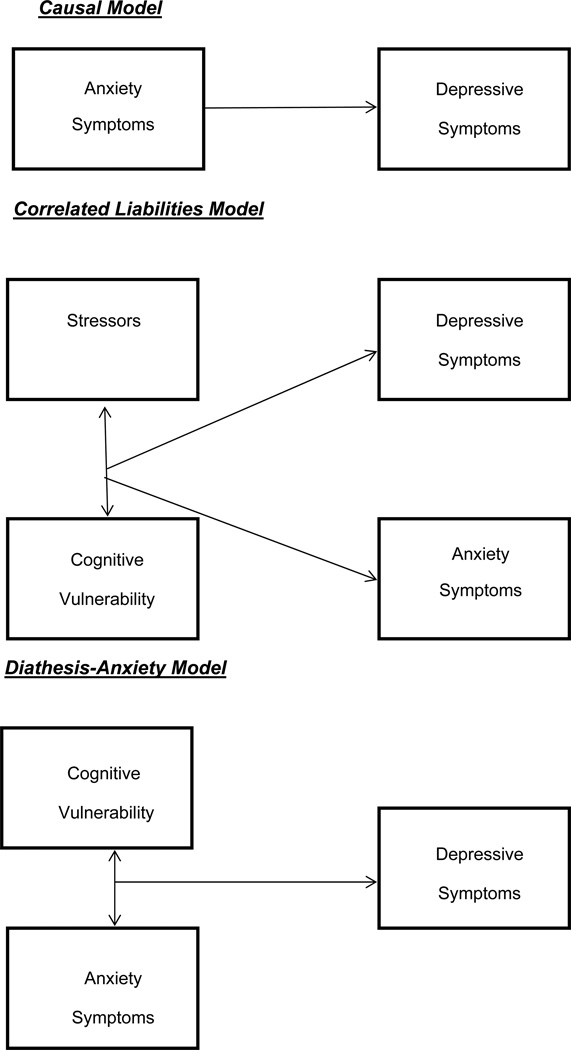
Finally, the present study sought to clarify conflicting findings by introducing and testing a diathesis-anxiety model, which combines the correlated liabilities model and the causal model (see Figure 1 for representations of all three models). This approach is meant to explicitly test whether anxiety symptoms interact with specific vulnerabilities to predict depression in youth. To date, only two studies have utilized this approach to understand the co-occurrence of depression and anxiety symptoms in youth. In a short-term, multi-wave study, Hankin (2008) found that rumination interacted with anxious arousal symptoms to predict prospective depression symptoms in a sample of early and middle adolescents. Meanwhile, in a multi-wave longitudinal study, Feng, Shaw, and Silk (2008) found that maternal negative control interacted with anxiety symptoms to predict depression during childhood and through adolescence. These findings are congruent with Starr and Davila’s recent studies with adults (2012a, 2012b), where the two researchers found that both rumination and a negative attributional style moderated the relation between daily anxious and depressed moods. These preliminary findings suggest that a combination of the causal and correlated liabilities models may resolve conflicting findings concerning the development of comorbid internalizing symptoms during youth. However, it is still unclear whether a diathesis-anxiety approach better explains the co-occurrence of depression and anxiety symptoms compared to the correlated liabilities or causal models.
Figure 1.
The Three Competing Comorbidity Models for Depression and Anxiety Symptoms in Youth
The present study sought to test these competing models of comorbidity within a cognitive-vulnerability framework. Studies have demonstrated that starting in late childhood individual differences begin to emerge for rumination (Lopez, Driscoll, & Kistner, 2009) and self-criticism (Fichman, Koestner, & Zuroff, 1994), and that these cognitive factors play an important role in predicting depressive and anxiety symptoms across child and adolescent samples (see Hankin, 2008, 2009; Rood, Roelofs, Bogels, & Alloy, 2010 for rumination; see Cohen et al., 2013; Shahar, Blatt, Zuroff, Kuperminc, & Leadbeater, 2004 for self-criticism). However, despite a well-documented relation between both forms of emotional distress, cognitive vulnerabilities are often understudied within a comorbidity context (Dozois & Dobson, 2001). Thus, assessments of rumination and self-criticism were incorporated in the present study, and we tested whether a correlated liabilities (e.g., a vulnerability-stress approach; see Gibb & Coles, 2005 for further explanation), causal, or diathesis-anxiety model best explained the relation between anxiety and depressive symptoms. Furthermore, we examined whether the developmental pathways concerning comorbidity differed across boys and girls and youth of different ages. It was hypothesized that across gender, age, and cognitive vulnerability, the diathesis-anxiety approach would provide a parsimonious explanation for how comorbid depressive and anxiety symptoms emerge in youth.
Method
Participants
Children and adolescents were recruited by brief information letters sent home directly by participating school districts to families with a child in third, sixth, and ninth grades of public schools. The short letter stated that we were conducting a study on social and emotional development in children and adolescents and requested that interested participants call the laboratory to receive detailed information on the study. At baseline, the multi-site sample consisted of 678 youth (362 from Denver, Colorado and 316 from New Brunswick, New Jersey) who had parental consent and gave verbal assent before baseline assessments. The sample was fairly balanced with regard to sex (380 females; 298 males) and consisted of 3rd graders (n=208), 6th graders (n=245), and 9th graders (n=225) at the baseline assessment. Youth completed evaluations every 3 months for 18-months.
Procedure
Only youth who had signed parental consent and gave verbal assent participated in the study. Phase 1 of the study involved a laboratory assessment. A research assistant (RA) met with the youth to complete all self-report measures. Meanwhile, Phase 2 of the study involved a series of 6 telephone follow-up assessments. Assessments occurred every 3 months during the 18 months following the initial assessment. At each assessment, an RA administered a measure for depressive symptoms, anxiety symptoms, and stressors. Participants were compensated $60 at Phase 1, and $15 for every completed follow-up in Phase 2. All aspects of the study were approved by an Institutional Review Board (IRB).
Measures
Children’s Response Style Questionnaire-Rumination Subscale (CRSQ-R; Abela, Rochon, & Vanderbilt, 2004)
The CRSQ-R is modeled after Nolen-Hoeksema’s Response Style Questionnaire (Nolen-Hoeksema & Morrow, 1991). The CRSQ-R consists of 13 items that assess one’s tendency to ruminate, or focus on negative aspects of oneself. For each item, youth are asked to indicate how often they respond in a ruminative way when they are feeling sad, with higher scores indicating higher agreement with the statement. Past research has shown the CRSQ-R to be a reliable and valid measure in youth samples (Abela, Aydin, & Auerbach, 2007; Abela & Hankin, 2011). The CRSQ-R had a Cronbach’s alpha level of 0.87.
Children’s Depressive Experiences Questionnaire Revised, Self-Criticism Subscale (CDEQR-SC; Abela, 2008)
The CDEQR-SC is a 12-item self-report questionnaire used to assess levels of self-criticism in youth. Similar to the 10-item CDEQ-SC (Abela & Taylor, 2003) and 5-item CDEQ-SF-SC (Abela, Fishman, Cohen, & Young, 2012), the CDEQR-SC is an adaptation of the Depressive Experiences Questionnaire (Blatt, D’Afflitti, & Quinlan, 1976), which is a widely used tool to assess self-criticism in adults. For each item, the child must choose which of the following options best represents him or her: not true for me, sort of true for me, or really true for me. Item scores range from 0 to 2 and are summed to obtain total scores ranging between 0 to 24; higher scores represent higher levels of self-criticism. Past research has supported the internal consistency, test-retest reliability, and validity of various versions of the CDEQ (Abela, Fishman, et al., 2012; Abela & Taylor, 2003). The CDEQR-SC had adequate internal consistency in the present study (α = 0.79).
Adolescent Life Events Questionnaire-Revised (ALEQ-R; Hankin & Abramson, 2002)
The ALEQ-R, in its abbreviated form, consists of 57 potentially negative events that are considered fairly typical of adolescence. The measure assesses the occurrence of stressors, which are drawn from various life areas including: academics, familial relationships, friendships, and romantic relationships. The participant indicates the frequency of each event during the previous month by selecting a response on a Likert scale from 1 (“never”) to 5 (“always”). The scores range from 57 to 285, with higher scores indicating more frequent stressful life events. Past research has found the ALEQ-R to be a reliable and valid assessment for assessing negative events in youth (Abela & Hankin, 2011; Hankin, 2008)
Children’s Depressive Inventory (CDI; Kovacs. 1981)
The CDI is a 27-item self-report questionnaire that measures the cognitive, affective, and behavioral symptoms of depression. For each item, children are asked which one of three statements (I am sad once in a while, I am sad many times, I am sad all the time) best describes how they have been thinking and feeling in the past week. Items are scored from 0 to 2, with a higher score indicating greater symptom severity. Total CDI scores ranged from 0 to 51. The CDI is the most commonly used measure for assessing youth depression (Myers & Winters, 2002). In the present study the coefficient alphas ranged between 0.84 and 0.89 across administrations.
Multidimensional Anxiety Scale for Children (MASC; March, 1997)
The MASC is a 39-item measure that assesses the occurrence and intensity of anxiety symptoms. The participant must determine the degree to which each item is true of him or herself on a Likert scale from 0 (“never”) to 3 (“often”), with higher scores indicating greater levels of anxiety symptoms. The measure may be divided into 4 subscales: physical symptoms, social anxiety, separation anxiety/panic, and harm avoidance; however, in the present study only the total score was utilized (range = 0 – 117). Past research has found the MASC to be a reliable and valid tool for measuring symptoms of youth anxiety (Alloy et al., 2012; Brozina & Abela, 2006). Cronbach’s alphas ranging between 0.88 and 0.90 across administrations were found in the present study.
Results
Preliminary Analyses
Preliminary analyses suggested that rumination, self-criticism, depressive symptoms and stressors all exhibited significant positive skew requiring these data to be transformed for purposes of normality. For rumination and self-criticism a square root transformation was used, while for stressors and depressive symptoms a log transformation was necessary. Means, standard deviations, and correlations of all baseline measures, prior to transformations, can be found in Table 1. Of note, the small to medium significant associations between internalizing symptoms and stressors (Grant & Compas, 1995; Muris, Merckelbach, Ollendick, King, & Bogie, 2002), and internalizing symptoms and cognitive vulnerabilities (Garnefski, Legerstee, Kraaij, Kommer, & Teerds, 2002; Lakdawalla, Hankin, & Mermelstein, 2007) are similar to past community research which investigated these constructs in youth. Means and standard deviations for the follow-up measures can be found in Table 2.
Table 1.
Baseline Means, Standard Deviations, and Correlations
| Measures | Mean | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| 1. CRSQ-R | 26.23 | 7.66 | ||||
| 2. CDEQR-SC | 19.27 | 4.29 | .51** | |||
| 3. ALEQ | 64.53 | 17.09 | .38** | .38** | ||
| 4. CDI | 7.02 | 5.84 | .48** | .42** | .52** | |
| 5. MASC | 41.92 | 15.66 | .36** | .34** | .28** | .28** |
Note: CRSQ-R = Baseline scores on the Children’s Response Style Questionnaire, Rumination Subscale; CDEQR-SC = Baselines scores on the Children’s Depressive Experiences Questionnaire, Self-Criticism Subscale; ALEQ = Baseline scores on the Adolescent Life Events Questionnaires; CDI = Baseline scores on the Children’s Depressive Inventory; MASC = Baseline scores on the Multidimensional Anxiety Scale for Children.
= p < .05;
= p < .01
Table 2.
Means and Standard Deviations for all Follow-up Measures
| Measures | Mean | SD | N | |
|---|---|---|---|---|
| CDI | ||||
| FU1 | 5.36 | 5.34 | 605 | |
| FU2 | 4.33 | 4.52 | 585 | |
| FU3 | 4.76 | 4.94 | 588 | |
| FU4 | 3.86 | 4.46 | 592 | |
| FU5 | 4.17 | 4.75 | 571 | |
| FU6 | 5.32 | 5.94 | 552 | |
| MASC | ||||
| FU1 | 42.69 | 15.27 | 603 | |
| FU2 | 42.17 | 14.50 | 583 | |
| FU3 | 41.59 | 15.53 | 593 | |
| FU4 | 40.94 | 14.56 | 590 | |
| FU5 | 41.26 | 15.18 | 568 | |
| FU6 | 34.75 | 15.58 | 556 | |
| ALEQ | ||||
| FU1 | 58.18 | 14.32 | 609 | |
| FU2 | 57.33 | 14.73 | 587 | |
| FU3 | 57.22 | 14.84 | 592 | |
| FU4 | 56.53 | 14.00 | 590 | |
| FU5 | 55.98 | 14.01 | 577 | |
| FU6 | 58.95 | 15.86 | 560 | |
Note: CDI = Scores on the Children’s Depressive Inventory; MASC = Scores on the Multidimensional Anxiety Scale for Children; ALEQ = Scores on the Adolescent Life Events Questionnaire; FU = Follow-up Assessment
Prior to testing the study’s hypotheses, confirmatory factor analyses (CFAs) were conducted to investigate whether self-report measures used in the present study were able to adequately distinguish between a) depressive and anxiety symptoms and b) forms of anxiety (e.g., separation anxiety, social anxiety, physical symptoms of anxiety, and harm avoidance). All CFAs were tested using AMOS 20 software. With regard to depressive and anxiety symptoms, an excellent fit (Hu & Bentler, 1999) was demonstrated for a two-factor model ((X2= 0.779, p = .377), CFI = 1.00, RMSEA = .00 (90% CI: .00 to .14); AIC = 53.10), and there was little support for a one-factor solution ((X2= 303.96, p < .001), CFI = 0.51, RMSEA = .68 (90% CI: .62 to .75); AIC = 424.48). Of note, a chi-square difference test further demonstrated the superiority of a two-factor, opposed to one-factor, solution (AX2= 373.38, p < .001). On the other hand, little support was found for a four factor model which distinguished between the MASC subscales ((X2= 249.514, p < .001, CFI = 0.754, RMSEA = .163 (90% CI: .145 to .182); AIC = 325.38). Taken together, results of the CFAs indicated that we were able to adequately distinguish between depressive and anxiety symptoms, but not differentiate between forms of anxiety symptoms. Thus, consistent with past research (O’Neil & Kendall, 2012; Storch et al., 2011), the hypotheses were tested using the MASC total anxiety score.
Next, as missing data is common in multi-wave longitudinal data, it was examined if participants who missed follow-ups differed systematically from those who had better or perfect completion rates during the course of the study. For the present study, 63.8% of participants completed the Time 1 and all six follow-up assessments, with 19.4% of the sample missing 1 follow-up, 5.7% of the sample missing 2 follow-ups, and 11% of the sample missing 3 or more follow-ups. Consistent with other multi-wave, longitudinal studies, there was a negative relation between the amount of follow-ups completed by participants and prospective depressive symptoms and follow-up stressors (see Twenge & Nolen-Hoeksema, 2002 for a discussion of this issue). In response, the Hedeker and Gibbons (1997) approach was used to see if the number of follow-ups completed by participants influenced any of the hypothesized relations in our study. Overall, no significance was found for follow-ups interacting with any hypothesized vulnerabilities to predict prospective internalizing symptoms (p > .05). Thus, it was concluded that data were missing at random (MAR).1
Data Analytic Approach
Analyses were carried out using the SAS (version 9.2) MIXED procedure. All cognitive vulnerabilities were entered into all models as time-invariant, between-subject, Level 2 variables. Meanwhile, stressors, anxiety symptoms, and depressive symptoms were entered as time-varying, within-subject, Level 1 variables. All Level 2 variables were group mean centered to increase the interpretability of various parameters in our models (Muller, Judd, & Yzerbyt, 2005), and all Level 1 predictors were centered at each participant’s mean so that scores reflect upwards or downwards fluctuations in an individual’s reported occurrence of stressors or symptoms as compared to his or her mean level. Finally, a time-lagged data-analysis approach was utilized when investigating all multi-level models as symptom outcomes at Time T-1 were entered as a time-varying covariate when predicting symptom outcomes at Time T. In addition, anxiety symptoms were entered at time T-1 and depressive symptoms were entered at time T for all causal and diathesis-anxiety models. Reverse models with depressive symptoms predicting anxiety symptoms were also tested within this time-lagged framework.
For all analyses, three additional fixed effects and three additional random effects were included in all statistical models. With regard to fixed effects, preliminary analyses revealed that girls experienced higher depressive symptoms over time compared to boys (t(4097) = 3.35, p = .001, reffect size = 05), and that older youth experienced elevated symptoms of depression compared to younger youth (t(4097) = 10.09, p < .001, reffect size = .16). Therefore, both sex and grade were entered as covariates in all analyses. In addition, because of the high rates of comorbidity between internalizing symptoms (Angold et al., 1999), it is important to account for anxiety symptoms when utilizing depressive symptoms as an outcome, and depressive symptoms when using anxiety symptoms as an outcome. At the same time, automatically controlling for comorbid symptoms may lead to misleading findings because the constructs are correlated (Miller & Chapman, 2001; Schwartz, Susser, Morabia, & Bromet, 2006). Therefore, findings were only considered significant in the present manuscript if the pattern of findings were similar under both conditions. As including concurrent symptoms is considered a more stringent model, all findings reported below reflect estimates while accounting for concurrent symptoms unless otherwise noted. With regard to random effects, a random slope for stressors (p < .001) and random intercept (p < .001) were significant in all analyses for depressive and anxiety symptoms, so these random effects were retained in subsequent analyses. In addition, a heterogeneous autoregressive structure was added to all of the models, as it was significant and provided the best fit (see Littell, Pendergast, & Natarajan, 2000 for explanation of different covariance structures and selection rules). Finally, effect sizes using the r statistic (see Rosnow, Rosenthal, & Rubin, 2000 for explanation of statistic; see Rice & Harris, 2005 for comparisons to other effect size statistics) were calculated for all results.
Causal Model
It was first examined whether anxiety symptoms (at Time T-1) predicted depressive symptoms (at Time T). Higher-ordered interactions were examined to see if this relation varied as a function of age and/or sex, but no significance was found for any of these interactions (p > .05). Similarly, there was also no significance found for anxiety symptoms directly predicting prospective depressive symptoms (b = 0.009; SE = 0.005; t(2551) = 1.82, p = 0.07, reffect size = .04). The reverse relation was next tested, to see if depressive symptoms (at Time T-1) predicted anxiety symptoms (at Time T). With regard to any interactions between age and/or sex, no significance was found (p > .05). With regard to depressive symptoms directly predicting anxiety symptoms, inconsistent support emerged with depressive symptoms predicting anxiety symptoms when controlling for concurrent depressive symptoms (b = 0.790; SE = 0.191; t(2551) = 4.14, p < .001, reffect size = 08), but insignificant when omitting this covariate (b = 0.336; SE = 0.190; t(2580) = 1.77, p =0.09, reffect size = 03). Thus, conclusive statements concerning a causal relation between depressive symptoms predicting anxiety symptoms could not be made.
Correlated Liabilities Models
Next, it was tested whether specific cognitive vulnerabilities interacted with stressors to predict prospective depressive and anxiety symptoms. It was first tested whether gender and/or grade moderated any of the potential correlated liabilities models. However, no significant interactions emerged (p > .10), suggesting that the vulnerability-stress models did not vary as a function of grade and/or sex. With regard to depressive symptoms, no support for rumination (b = 0.009; SE = 0.005; t(2495) = 1.61, p = 0.10, reffect size = 03) or self-criticism (b = 0.010; SE = 0.005; t(2484) = 1.84, p =0.07, reffect size = 04) interacting with stressors to predict depressive symptoms was found. Similarly, we found that neither rumination (b = 0.396; SE = 0.214; t(2517) = 1.85, p = 0.06; reffect size =0.04) nor self-criticism (b = −0.046; SE = 0.213; t(2506) = −0.22, p = .83, reffect size = 0.00) interacted with stressors to predict elevated anxiety symptoms.
Diathesis-Anxiety Models
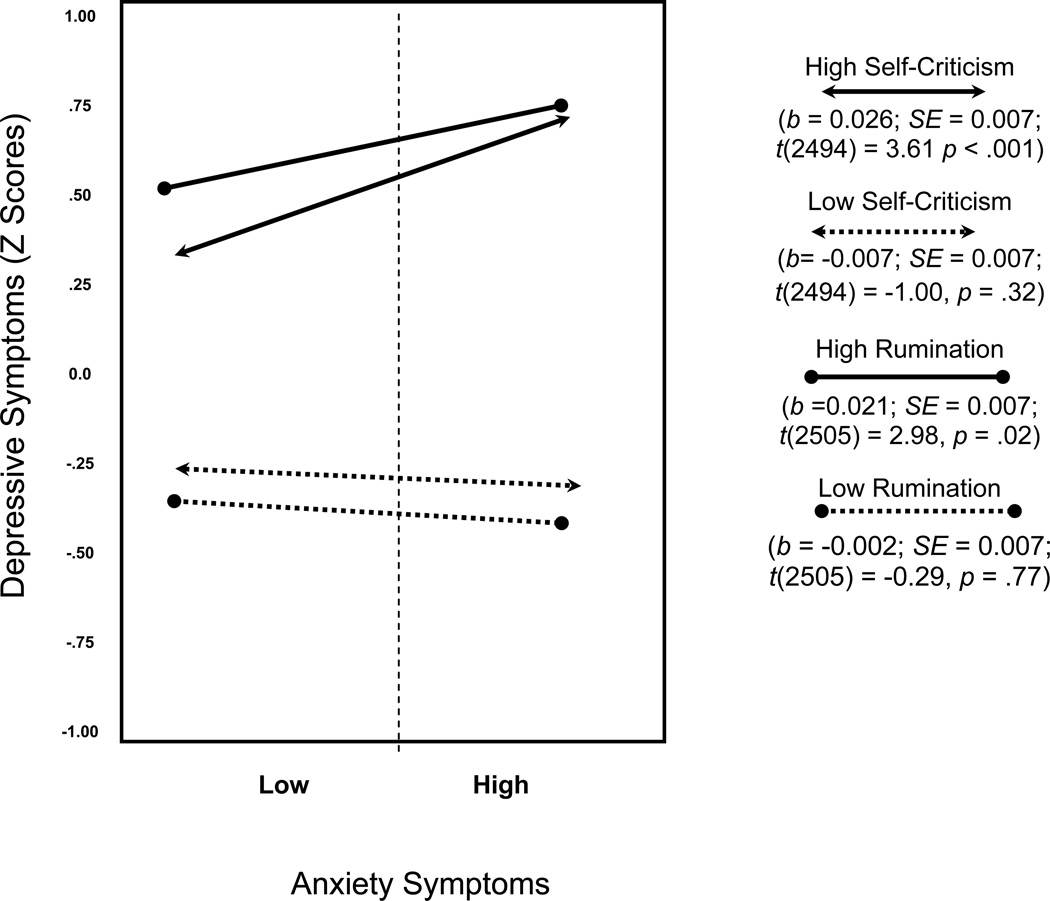
It was first tested whether gender and/or grade moderated any of the proposed diathesis-anxiety models. However, no significant four-way or three-way relations emerged (p > .10). Next, it was tested whether self-criticism and rumination significantly interacted with anxiety symptoms to predict prospective depressive symptoms. Complete results for these analyses can be found in Table 3. Results suggested that both self-criticism (t(2494) = 3.36, p < .001, reffect size = 07) and rumination (t(2505) = 2.40, p = .02, reffect size = 05) interacted with anxiety symptoms to predict prospective depressive symptoms. To examine the form of these interactions, the predicted CDI scores for children possessing either a high or low ruminative or self-critical style (plus or minus 1.5 SD above/below the group mean) and who reported low or high MASC scores in comparison to their own average MASC score (plus or minus 1.5 SD) were calculated. As both CDI and MASC are within-subject variables centered at each participant’s mean, slopes are interpreted as the increase in a child’s CDI score that would be expected given he or she scored one standard deviation higher on the MASC. The results of such calculations are presented in Figure 2 and, as can be seen, individuals with a high ruminative or self-critical style who experience high levels of anxiety were most at risk for experiencing elevated depressive symptoms over time.
Table 3.
Diathesis-Anxiety Models for Self-Criticism and Rumination
| Model for Rumination | ||||
|---|---|---|---|---|
| B | SE | T | Df | |
| Grade | 0.025 | 0.005 | 5.43*** | 621 |
| Gender | −0.013 | 0.022 | −0.61 | 621 |
| Anxiety | 0.049 | 0.005 | 9.79*** | 2505 |
| Depress_Lag | −0.071 | 0.005 | −14.29*** | 2505 |
| Anxiety_Lag | 0.010 | 0.005 | 1.90 | 2505 |
| Rumination | 0.137 | 0.011 | 12.45*** | 621 |
| Rumination x Anxiety_Lag | 0.012 | 0.005 | 2.40* | 2505 |
| Model for Self-Criticism | ||||
| Grade | 0.020 | 0.005 | 4.04*** | 618 |
| Gender | 0.010 | 0.023 | 0.44 | 618 |
| Anxiety | 0.484 | 0.005 | 9.67*** | 2494 |
| Depress_Lag | −0.071 | 0.005 | −14.42*** | 2494 |
| Anxiety_Lag | 0.010 | 0.005 | 1.85 | 2494 |
| Self-Criticism | 0.102 | 0.012 | 8.86*** | 618 |
| Self-Criticism x Anxiety_Lag | 0.016 | 0.004 | 3.36*** | 2494 |
Note: Grade = Child’s grade in school; Gender = Child’s gender (0 = Boy; 1 = Girl); Anxiety = Scores on the Multidimensional Anxiety Scale for Children over time; Depress_Lag = Scores on the Children’s Depressive Inventory at Time (T-1); Scores on the Multidimensional Anxiety Scale for Children over time at Time (T-1); Rumination = Baseline scores on the Children’s Response Style Questionnaire; Self-Criticism = Children’s Depressive Experience Questionnaire, Self-Criticism subscale.
= p < .05;
= p < .01;
= p < .001.
Figure 2.
Predicted slope of the relation between anxiety symptoms (T-1) and depressive symptoms (T) possessing high or low cognitive vulnerabilities (Diathesis-Anxiety Models).
To provide a more stringent test, it was examined whether the diathesis-anxiety models remained significant even when including the traditional vulnerability-stress interactions. The pattern of findings remained similar for both rumination (b = 0.124; SE = 0.005; t(2505) = 2.58, p = .009, reffect size = 05) and self-criticism (b = 0.016; SE = 0.005; t(2494) = 3.40, p < .001, reffect size = .07) interacting with anxiety symptoms to predict depressive symptoms. Finally, it was tested whether the reverse relation was also significant by specifically examining if these vulnerabilities interacted with depressive symptoms to predict prospective anxiety symptoms. Findings for both rumination (b = 0.241; SE = 0.182; t(2495) = 1.32, p = 0.19, reffect size = 03) and self-criticism (b = 0.106; SE = 0.179; t(2484) = 0.59, p = 0.55, reffect size = 01) in these models were insignificant, suggesting that a diathesis-anxiety, but not diathesis-depression model, may be a valid explanation for comorbid depressive and anxiety symptoms.
Discussion
The goal of the present study was to add new knowledge to the ongoing debate concerning the etiological origins of comorbid depressive and anxiety symptoms in youth. Findings from this research support other findings (Avenvoli et al., 2001; Matthew et al., 2011), which have suggested that a combination of a correlated liabilities model and causal model may best explain the emergence of comorbid emotional states. However, where past research suggested that both models independently predict comorbid depression and anxiety, the present study introduced the diathesis-anxiety approach, and found that synthesizing both of Neale and Kendler’s (1995) comorbidity models may provide the best explanation for comorbid symptoms in youth. Specifically, we found that youth who experience elevated anxiety symptoms only go on to develop depressive symptoms, if they also tend to ruminate or be self-critical. Not only novel, these findings provide impactful insight into the development of emotional distress in youth, which may be translated into future clinical and research endeavors.
A traditional explanation for comorbid symptoms states that anxiety directly predicts the onset of depressive symptoms (Flannery-Schroeder, 2006). However, the present study is more consistent with recent research which suggested that this causal model may not be the best explanation for why comorbid depressive and anxiety symptoms exist (Moffitt et al., 2008; Rice et al., 2004). Instead, researchers have suggested that past findings supporting anxiety directly predict depression may be due to an overreliance on retrospective studies in which earlier episodes of depressive episodes are underreported (Moffitt et al., 2008) or that the occurrence of anxiety before depression represents an earlier expression of psychopathology from a shared vulnerability (Rice et al., 2004). Our research also suggests that the causal model may not provide the best explanation as to why depressive and anxiety symptoms co-occur; however, findings from the present study suggest that anxiety symptoms do play a role in the development of depressive symptoms.
The emergence of diathesis-anxiety models is consistent with other past research in youth (Feng et al., 2008; Hankin, 2008) and adults (Starr & Davila, 2012a, 2012b) and helps introduce a new explanation for comorbid emotional distress in youth. The present study found that anxiety symptoms interacted with rumination and self-criticism to predict prospective depressive symptoms in children and adolescents. Importantly, support for the reverse model of depressive symptoms interacting with cognitive vulnerabilities to predict prospective anxiety symptoms was not found. This finding is similar to recent research which suggested that anxiety is a variable risk factor for depression, but depression does not confer risk for anxiety (Aune & Stiles, 2009; Grant et al., 2013). There are several possible explanations which may explain why anxiety uniquely predicts symptoms of depression. A common hypothesis is that anxiety develops earlier than depression, and therefore, naturally predates (and predicts) depressive symptoms (Aune & Stiles, 2009). However, even when examining symptom fluctuations in young adults, anxiety symptoms act as a vulnerability for depressive symptoms, but the reverse is not true (Grant et al., 2013). Thus, it seems that a strict developmental explanation may be limited in explaining why anxiety specifically predicts depression.
An alternative explanation may be that there is something unique about the interaction between anxiety symptoms and cognitive vulnerabilities. Recent research has shown that rumination and self-blame (a byproduct of self-criticism; Dunkley, Zuroff, & Blankenstein, 2003) are closely related to symptoms of anxiety in children (Legerstee, Garnefski, Jellesma, Verhulst, & Utens, 2010) and adolescents (Legerstee, Garnefski, Verhulst, & Utens, 2011). While these cognitive coping mechanisms are typically conceptualized as vulnerabilities for anxiety symptoms (Lewis, Byrd, & Ollendick, 2012), other research suggests that the relation is more reciprocal in nature (Starr & Davila, 2012a). In other words, as one’s symptoms of anxiety increase, maladaptive coping mechanisms such as rumination and self-criticism also increase. Therefore, it may be that higher amounts of rumination and self-criticism, or experiencing these thoughts over a prolonged period of time, may lead to a distinct form of emotional distress in the form of depressive symptoms.
There is also a possible behavioral explanation as to why support for a diathesis-anxiety, but not for a diathesis-depressive model, was found. As anxiety symptoms increase individuals are likely to disengage in different activities (e.g., sports, going to a friend’s house; Morris & March, 2004). While avoidance provides temporary relief from distress, it ultimately may lead to an isolating context with little reward, and eventually depressive symptoms (Aune & Stiles, 2009). Findings from the present study suggest that this may be especially true if the anxious individual is perseverating on their situation (rumination) or blaming oneself for the lack of perceived success (self-criticism). As depression is also related to avoidance (Trew, 2011), one may expect this isolating environment to continue for youth as they experience depressive symptoms. However, while this environment may lead to an increase in depressive symptoms, there may be little reason to believe this context would provoke anxiety symptoms. Thus, it may be that avoidance serves as a mediator for increased depressive symptoms both within a diathesis-anxiety and diathesis-depressive framework. This hypothesis would support why both anxiety and depressive symptoms beget depression, but only anxiety symptoms predict prospective anxiety (Keenan, Feng, Hipwell, & Klostermann, 2009).
An added strength of the present study was that it directly tested diathesis-anxiety interactions alongside traditional, vulnerability-stress interactions. While a majority of research has shown that the interactions between rumination and stressors (Abela & Hankin, 2011; Abela, Hankin, Sheshko, Fishman, & Stolow, 2012) and self-criticism and stressors (Abela, Sakellaropoulo, & Taxel, 2007; Abela & Taylor, 2003) predict depressive symptoms, a smaller body of research has been unable to replicate these effects (e.g., Cohen et al., 2013; Priel & Shahar, 2000 for self-criticism; Sarin, Abela, & Auerbach, 2005 for rumination). While methodological differences may be an important reason for the difficulty in replicating these vulnerability-stress findings, another possibility is that the interaction between anxiety symptoms and cognitive vulnerabilities is more proximal to depressive symptoms as opposed to a vulnerability-stress interaction. Within this framework, it may be that anxiety symptoms are highly correlated with stressors (Lewis et al., 2012), because it is part of the reaction to negative events (Grant & Compas, 1995). This may make anxiety symptoms temporally closer to the onset of depressive symptoms and therefore, easier to detect as a predictor of depressive symptoms when in the presence of elevated rumination and/or self-criticism. Given the small effect sizes and preli minary nature of these findings, future research is needed to further test the explanatory power of a diathesis-anxiety approach.
Limitations and Future Directions
While the large sample, multi-wave, longitudinal design, rigorous statistical analyses, and dimensional approach to psychopathology were all strengths of the study, there are some notable limitations. First, findings from the study are based on self-report measures. While reliable and valid measures were used, a multi-method approach is a logical next step when investigating these questions. For instance, computer-based tasks have been shown to provide objective information concerning cognitive vulnerability (Beevers, 2005; Gibb, Beevers, & McGeary, 2013), and semi-structured interviews may provide better insight into the nature of stressors (Rudolph, Hammen, Burge, Lindberg, Herzberg, & Daley, 2000), depressive symptoms (Ingram & Siegle, 2002), and anxiety symptoms (Velting, Setzer, & Albano, 2004). Second, the present study utilized a community sample to make inferences on comorbid clinical conditions. Therefore, it needs to be tested whether these models are able to predict symptom patterns within a clinical sample. Third, the present study was unable to distinguish between forms of anxiety symptoms, and instead treated it as a unitary construct. Given the important differences between distinct forms of anxiety and depressive symptoms (Kaufman & Charney, 2000), and anxiety symptoms and cognitive vulnerabilities (Ferreri, Lapp, & Peretti, 2011), future studies should use methods which can differentiate between distinct forms of anxiety. Finally, although we found statistical significance for our findings, the effect sizes were in the small range. While past research has noted that small effect sizes are expected when conducting non-experimental field research (McClelland & Judd, 1993), cautious interpretations should be made until other studies have replicated these findings.
Support for a diathesis-anxiety approach to comorbidity helps lay a foundation for future research on comorbid emotional disorders in youth. Whether a diathesis-anxiety approach may provide the best explanation for comorbid depression and anxiety symptoms across various intrapersonal and interpersonal risk factors, or whether multiple pathways to comorbidity will emerge (Matthew et al., 2011), remains an important area of research. With regard to clinical implications, findings from the present study support others who have advocated for targeting anxiety symptoms within the context of depression prevention and treatment programs (Flannery-Schroeder, 2006; Young et al., 2006). Additionally, our findings reinforce the need to use specific techniques to target problematic cognitive styles (e.g., see Garber, 2006) and decrease symptoms of anxiety which are activating these specific cognitive styles (e.g., Conrad & Roth, 2007) when treating comorbid emotional distress in youth. Because findings from this paper are preliminary, these translated implications are speculative at this point. However, continued research on the etiology of comorbid conditions may lead to more successful treatment of an impaired youth population (Mineka et al., 1998), which has proven difficult to treat (Ollendick et al., 2008).
Acknowledgments
This research was supported by NIMH grants F31MH096430 awarded to Joseph Cohen and R01-MH 077195 awarded to Benjamin Hankin and Jami Young.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Of note, the Little’s Missing Completely at Random (MCAR) test was statistically significant, and we therefore did not impute any missing data for any of the analyses reported in the manuscript. However, we did retest our findings with imputed data using estimation maximization procedures (EM). Of note, the pattern of findings remained similar with and without imputed data.
The manuscript is dedicated to Dr. John R. Z. Abela, whose brilliance helped lay the foundation for the presented research, and whose creativity continues to inspire us.
The authors have no conflicts of interest to disclose.
Drs. John Abela and Benjamin Hankin designed the original study which the present study built upon. Drs. Jami Young and Brandon Gibb co-mentored Joseph Cohen, and helped write the protocol for the present study. Dr. Jami Young also proofread several drafts of the manuscript, and Dr. Brandon Gibb provided statistical consultation. Joseph Cohen wrote the manuscript and conducted the statistical analyses.
References
- Abela JRZ. Children’s Depressive Experiences Questionnaire-Revised. New Brunswick, NJ: Unpublished Measure, Rutgers University; 2008. [Google Scholar]
- Abela JRZ, Aydin CM, Auerbach RP. Responses to depression in children: Reconceptualizing the relation among response styles. Journal of Abnormal Child Psychology. 2007;35:913–927. doi: 10.1007/s10802-007-9143-2. [DOI] [PubMed] [Google Scholar]
- Abela JRZ, Fishman MB, Cohen JR, Young JF. Personality predispositions to depression in children of affectively-ill parents: The buffering role of self-esteem. Journal of Clinical Child & Adolescent Psychology. 2012;41:391–401. doi: 10.1080/15374416.2012.654463. [DOI] [PubMed] [Google Scholar]
- Abela JRZ, Hankin BL. Cognitive vulnerability to depression in children and adolescents. In: Abela JRZ, Hankin BL, editors. Handbook of depression in children and adolescents. New York, NY: The Guilford Press; 2008. pp. 35–78. [Google Scholar]
- Abela JRZ, Hankin BL. Rumination as a vulnerability factor to depression during the transition from early to middle adolescence: A multiwave longitudinal study. Journal of Abnormal Psychology. 2011;120:259–271. doi: 10.1037/a0022796. [DOI] [PubMed] [Google Scholar]
- Abela JR, Hankin BL, Sheshko DM, Fishman MB, Stolow D. Multi-wave prospective examination of the stress-reactivity extension of response styles theory of depression in high-risk children and early adolescents. Journal of abnormal child psychology. 2012;40:277–287. doi: 10.1007/s10802-011-9563-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abela JRZ, Rochon A, Vanderbilt E. A test of the integration of the response styles and social support theories of depression in third and seventh grade children. Journal of Social and Clinical Psychology. 2004;23:653–674. [Google Scholar]
- Abela JRZ, Sakellaropoulo M, Taxel E. Integrating two subtypes of depression: Psychodynamic theory and its relation to hopelessness depression in schoolchildren. Journal of Early Adolescence. 2007;27:363–385. [Google Scholar]
- Abela JRZ, Taylor G. Specific vulnerability to depressive mood reactions in schoolchildren: The moderating role of self-esteem. Journal of Clinical Child and Adolescent Psychology. 2003;32:408–418. doi: 10.1207/S15374424JCCP3203_09. [DOI] [PubMed] [Google Scholar]
- Alloy LB, Black SK, Young ME, Goldstein KE, Shapero BG, Moore LC. Cognitive vulnerabilities and depression versus other psychopathology symptoms and diagnoses in early adolescence. Journal of Clinical Child & Adolescent Psychology. 2012;41:539–560. doi: 10.1080/15374416.2012.703123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson ER, Hope DA. A review of the tripartite model for understanding the link between anxiety and depression in youth. Clinical Psychology Review. 2008;28:275–287. doi: 10.1016/j.cpr.2007.05.004. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ. Depressive comorbidity in children and adolescents: Empirical, theoretical, and methodological issues. Annual Progress in Child Psychiatry and Child Development. 1993;150:1779–1791. doi: 10.1176/ajp.150.12.1779. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychology and Allied Disciplines. 1999;40:57–88. [PubMed] [Google Scholar]
- Aune T, Stiles TC. The effects of depression and stressful life events on the development and maintenance of syndromal social anxiety: Sex and age differences. Journal of Clinical Child & Adolescent Psychology. 2009;38:501–512. doi: 10.1080/15374410902976304. [DOI] [PubMed] [Google Scholar]
- Avenvoli S, Stolar M, Li J, Dierker L, Merikangas KR. Comorbidity of depression in children and adolescents: Models and evidence from a prospective high-risk family study. Society of Biological Psychiatry. 2001:1071–1081. doi: 10.1016/s0006-3223(01)01142-8. [DOI] [PubMed] [Google Scholar]
- Beck AT. Cognitive therapy and the emotional disorders. Oxford: International Universities Press; 1976. [Google Scholar]
- Beevers CG. Cognitive vulnerability to depression: A dual process model. Clinical Psychology Review. 2005;25:975–1002. doi: 10.1016/j.cpr.2005.03.003. [DOI] [PubMed] [Google Scholar]
- Blatt SJ, D’Afflitti JP, Quinlan DM. Experiences of depression in normal young adults. Journal of Abnormal Psychology. 1976;95:383–389. doi: 10.1037//0021-843x.85.4.383. [DOI] [PubMed] [Google Scholar]
- Brozina K, Abela JRZ. Symptoms of depression and anxiety in children: Specificity of the hopelessness theory. Journal of Clinical Child & Adolescent Psychology. 2006;35:515–527. doi: 10.1207/s15374424jccp3504_3. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Conrad A, Roth WT. Muscle relaxation therapy for anxiety disorders: It works but how? Journal of Anxiety Disorders. 2007;21:243–264. doi: 10.1016/j.janxdis.2006.08.001. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Dozois DJ, Dobson KS. Information processing and cognitive organization in unipolar depression: Specificity and comorbidity issues. Journal of Abnormal Psychology. 2001;110:236. doi: 10.1037//0021-843x.110.2.236. [DOI] [PubMed] [Google Scholar]
- Dunkley DM, Zuroff DC, Blankstein KR. Self-critical perfectionism and daily affect: Dispositional and situational influences on stress and coping. Journal of Personality and Social psychology. 2003;84:234–252. [PubMed] [Google Scholar]
- Epkins CC. Cognitive specificity and affective confounding in social anxiety and dysphoria in children. Journal of Psychopathology and Behavioral Assessment. 1996;18:83–101. [Google Scholar]
- Essau CA, Chang WC. Epidemiology, comorbidity, and course of adolescent depression. In: Essau CA, editor. Treatment of adolescent depression: Theory and practice. Oxford: Oxford University Press; 2009. [Google Scholar]
- Feng X, Shaw DS, Silk JS. Developmental trajectories of anxiety symptoms among boys across early and middle childhood. Journal of Abnormal Psychology. 2008;117:32–47. doi: 10.1037/0021-843X.117.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreri F, Lapp LK, Peretti CS. Current research on cognitive aspects of anxiety disorders. Current Opinion in Psychiatry. 2011;24:49–54. doi: 10.1097/YCO.0b013e32833f5585. [DOI] [PubMed] [Google Scholar]
- Fichman L, Koestner R, Zuroff DC. Dependency, self-criticism, and perceptions of inferiority at summer camp: I’m even worse than you think. Journal of Youth and Adolescence. 1994;25:113–126. [Google Scholar]
- Flannery-Schroeder EC. Reducing anxiety to prevent depression. American Journal of Preventative Medicine. 2006;31:136–142. doi: 10.1016/j.amepre.2006.07.006. [DOI] [PubMed] [Google Scholar]
- Garber J. Depression in children and adolescents: linking risk research and prevention. American Journal of Preventive Medicine. 2006;31:104–125. doi: 10.1016/j.amepre.2006.07.007. [DOI] [PubMed] [Google Scholar]
- Garber J, Weiss B, Shanley N. Cognitions, depressive symptoms, and development in adolescents. Journal of Abnormal Psychology. 1993;102:47–57. doi: 10.1037//0021-843x.102.1.47. [DOI] [PubMed] [Google Scholar]
- Garnefski N, Legerstee J, Kraaij V, van den Kommer T, Teerds JAN. Cognitive coping strategies and symptoms of depression and anxiety: A comparison between adolescents and adults. Journal of Adolescence. 2002;25:603–611. doi: 10.1006/jado.2002.0507. [DOI] [PubMed] [Google Scholar]
- Gibb BE, Beevers CG, McGeary JE. Toward an integration of cognitive and genetic models of risk for depression. Cognition & Emotion. 2013;27:193–216. doi: 10.1080/02699931.2012.712950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibb BE, Coles M. Cognitive vulnerability–stress models of psychopathology: A developmental perspective. In: Hankin BL, Abela JRZ, editors. Development of psychopathology: A vulnerability-stress perspective. Thousand Oaks, CA: Sage; 2005. pp. 104–135. [Google Scholar]
- Grant KE, Compas BE. Stress and anxious-depressed symptoms among adolescents: Searching for mechanisms of risk. Journal of Consulting and Clinical Psychology. 1995;63:1015–1021. doi: 10.1037//0022-006x.63.6.1015. [DOI] [PubMed] [Google Scholar]
- Grant DM, Judah MR, Mills AC, Lechner WV, Davidson CL, Wingate LR. Rumination and excessive reassurance seeking: Mediators of the relationship between social anxiety and depression? Journal of Psychopathology and Behavioral Assessment. 2013:1–10. [Google Scholar]
- Hankin BL. Cognitive vulnerability-stress model of depression during adolescence: Investigating depressive symptom specificity in a multi-wave prospective study. Journal of Abnormal Child Psychology. 2008;36:999–1014. doi: 10.1007/s10802-008-9228-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL. Development of sex differences in depressive and co-occurring anxious symptoms during adolescence: Descriptive trajectories and potential explanations in a multiwave prospective study. Journal of Clinical Child & Adolescent Psychology. 2009;38:460–472. doi: 10.1080/15374410902976288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY. Measuring cognitive vulnerability to depression in adolescence: Reliability, validity, and gender differences. Journal of Clinical Child and Adolescent Psychology. 2002;31:491–504. doi: 10.1207/S15374424JCCP3104_8. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD. Longitudinal Data Analysis. Hoboken, NJ: John Wiley & Sons, Inc; 1997. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. [Google Scholar]
- Ingram RE, Siegle GJ. Contemporary methodological issues in the study of depression: Not your father's Oldsmobile. In: Gotlib IH, Hammen CL, editors. Handbook of depression. New York, NY: Guilford Press; 2002. pp. 86–114. [Google Scholar]
- Jacobs RH, Reinecke MA, Gollan JK, Kane P. Empirical evidence of cognitive vulnerability for depression among children and adolescents: A cognitive science and developmental perspective. Clinical Psychology Review. 2008;28:759–782. doi: 10.1016/j.cpr.2007.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jolly JB. A multi-method test of the cognitive-specificity hypothesis in young adolescents. Journal of Anxiety Disorders. 1993;7:223–233. [Google Scholar]
- Kaufman J, Charney D. Comorbidity of mood and anxiety disorders. Depression and Anxiety. 2000;12:79–86. doi: 10.1002/1520-6394(2000)12:1+<69::AID-DA9>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Keenan K, Feng X, Hipwell A, Klostermann S. Depression begets depression: Comparing the predictive utility of depression and anxiety symptoms to later depression. Journal of Child Psychology and Psychiatry. 2009;50:1167–1175. doi: 10.1111/j.1469-7610.2009.02080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Lewinsohn PM, Rohde P, Seeley JR, Shankman SA. Family study of comorbidity between major depressive disorder and anxiety disorders. Psychological Medicine. 2003;33:703–714. doi: 10.1017/s0033291703007487. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Rating scales to assess depression in school-aged children. Acta Paedopsychiatrica: International Journal of Child & Adolescent Psychiatry. 1981;46:305–315. [PubMed] [Google Scholar]
- Krueger RF, Finger MS. Using item response theory to understand comorbidity among anxiety and unipolar mood disorders. Psychological Assessment. 2001;13:140–151. [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakdawalla Z, Hankin BL, Mermelstein R. Cognitive theories of depression in children and adolescents: A conceptual and quantitative review. Clinical Child and Family Psychology Review. 2007;10:1–24. doi: 10.1007/s10567-006-0013-1. [DOI] [PubMed] [Google Scholar]
- Laurent J, Ettelson R. An examination of the tripartite model of anxiety and depression and its application to youth. Clinical Child and Family Psychology Review. 2001;4:209–229. doi: 10.1023/a:1017547014504. [DOI] [PubMed] [Google Scholar]
- Legerstee JS, Garnefski N, Jellesma FC, Verhulst FC, Utens EMWJ. Cognitive coping and childhood anxiety disorders. European Child and Adolescent Psychiatry. 2010;19:143–150. doi: 10.1007/s00787-009-0051-6. [DOI] [PubMed] [Google Scholar]
- Legerstee JS, Garnefski N, Verhulst FC, Utens EMWJ. Cognitive coping in anxiety-disordered adolescents. Journal of Adolescence. 2011;34:319–326. doi: 10.1016/j.adolescence.2010.04.008. [DOI] [PubMed] [Google Scholar]
- Lewis KM, Byrd DA, Ollendick TH. Anxiety symptoms in African-American and Caucasian youth: Relations to negative life events, social support, and coping. Journal of Anxiety Disorders. 2012;26:32–39. doi: 10.1016/j.janxdis.2011.08.007. [DOI] [PubMed] [Google Scholar]
- Littell RC, Pendergast J, Natarajan R. Tutorial in biostatistics: Modeling covariance structure in the analysis of repeated measures data. Statistics in Medicine. 2000;19:1793–1819. doi: 10.1002/1097-0258(20000715)19:13<1793::aid-sim482>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Lopez CM, Driscoll KA, Kistner JA. Sex differences and response styles: Subtypes of rumination and associations with depressive symptoms. Journal of Clinical Child & Adolescent Psychology. 2009;38:27–35. doi: 10.1080/15374410802575412. [DOI] [PubMed] [Google Scholar]
- March JS. Manual for the Multidimensional Anxiety Scale for Children (MASC) Toronto: Multi-Health Systems; 1997. [Google Scholar]
- Matthew AR, Petit JW, Lewinsohn PM, Seeley JR, Roberts RE. Co-morbidity between major depressive disorder and anxiety disorders: Shared etiology or direct causation? Psychological Medicine. 2011;41:2023–2034. doi: 10.1017/S0033291711000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClelland GH, Judd CM. Statistical difficulties of detecting interactions and moderator effects. Psychological Bulletin. 1993;114:376–390. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J, Burstein M, Swanson SA, Avenvoli S, Cui L, Swendson J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Middeldorp CM, Cath DC, Van Dyck R, Boomsma DI. The co-morbidity of anxiety and depression in the perspective of genetic epidemiology: A review of twin and family studies. Psychological Medicine. 2005;35:611–624. doi: 10.1017/s003329170400412x. [DOI] [PubMed] [Google Scholar]
- Miller GA, Chapman JP. Misunderstanding analysis of covariance. Journal of Abnormal Psychology. 2001;110:40–48. doi: 10.1037//0021-843x.110.1.40. [DOI] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Harrington H, Caspi A, Kim-Cohen J, Goldberg D, Gregory AM, Poutlon R. Depression and generalized anxiety disorder: Cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Archives of General Psychiatry. 2008;64:651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- Morris TL, March JS. Anxiety disorders in children and adolescents. 2nd Edition. New York: Guildford Press; 2004. [Google Scholar]
- Muller D, Judd CM, Yzerbyt VY. When moderation is mediated and mediation is moderated. Journal of Personality and Social Psychology. 2005;89:852–863. doi: 10.1037/0022-3514.89.6.852. [DOI] [PubMed] [Google Scholar]
- Muris P, Merckelbach H, Ollendick T, King N, Bogie N. Three traditional and three new childhood anxiety questionnaires: Their reliability and validity in a normal adolescent sample. Behaviour Research and Therapy. 2002;40:753–772. doi: 10.1016/s0005-7967(01)00056-0. [DOI] [PubMed] [Google Scholar]
- Myers K, Winters NC. Ten-year review of rating scales. II: Scales for internalizing disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:634–659. doi: 10.1097/00004583-200206000-00004. [DOI] [PubMed] [Google Scholar]
- Neale MC, Kendler KS. Models of comorbidity for multifactorial disorders. American Journal of Human Genetics. 1995;57:935–953. [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta Earthquake. Journal of Personality and Social Psychology. 1991;61:115–121. doi: 10.1037//0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Stice E, Wade E, Bohon C. Reciprocal relations between rumination and bulimic, substance abuse, and depressive symptoms in female adolescents. Journal of Abnormal Psychology. 2007;116:198–207. doi: 10.1037/0021-843X.116.1.198. [DOI] [PubMed] [Google Scholar]
- Ollendick TH, Jarrett MA, Grills-Taquechel AE, Hovey LD, Wolff JC. Comorbidity as a predictor and moderator of treatment outcome in youth with anxiety, affective, attention, deficit/hyperactivity disorder, and oppositional/conduct disorders. Clinical Psychology Review. 2008;28:1447–1471. doi: 10.1016/j.cpr.2008.09.003. [DOI] [PubMed] [Google Scholar]
- O'Neil KA, Kendall PC. Role of comorbid depression and co-occurring depressive symptoms in outcomes for anxiety-disordered youth treated with cognitive-behavioral therapy. Child & Family Behavior Therapy. 2012;34:197–209. [Google Scholar]
- Rice F, van den Bree MBM, Thapar A. A population-based study of anxiety as a precursor for depression in childhood and adolescence. BMC Psychiatry. 2004;4 doi: 10.1186/1471-244X-4-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice ME, Harris GT. Comparing effect sizes in follow-up studies: ROC Area, Cohen’s d, and r. Law and Human Behavior. 2005;29:615–620. doi: 10.1007/s10979-005-6832-7. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Comorbidity of unipolar depression II: Comorbidity in adolescents and adults. Journal of Abnormal Psychology. 1991;100:214–222. [PubMed] [Google Scholar]
- Rood L, Roelofs J, Bogels SM, Bogels SM, Alloy LB. Dimensions of negative thinking and the relations with symptoms of depression and anxiety in children and adolescents. Cognitive Therapy and Research. 2010;34:333–342. doi: 10.1007/s10608-009-9261-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosnow RL, Rosenthal R, Rubin DB. Contrasts and correlations in effect size estimation. Psychological Science. 2000;11:446–453. doi: 10.1111/1467-9280.00287. [DOI] [PubMed] [Google Scholar]
- Rudolph KD, Hammen C, Burge D, Lindberg N, Herzberg D, Daley SE. Toward an interpersonal life-stress model of depression: The developmental context of stress generation. Development and Psychopathology. 2000;12:215–234. doi: 10.1017/s0954579400002066. [DOI] [PubMed] [Google Scholar]
- Schniering CA, Rapee RM. The relationship between automatic thoughts and negative emotions in children and adolescents: A test of the cognitive content-specificity hypothesis. Journal of Abnormal Psychology. 2004;113:464–470. doi: 10.1037/0021-843X.113.3.464. [DOI] [PubMed] [Google Scholar]
- Schwartz S, Susser E, Morabia A, Bromet E. What is a cause. In: Susser SSE, Morabia A, Bromet EJ, editors. Psychiatric epidemiology: Searching for the causes of mental disorders. New York, NY: Oxford University Press; 2006. pp. 33–42. [Google Scholar]
- Seligman LD, Ollendick TH. Comorbidity of anxiety and depression in children and adolescents: An integrative review. Clinical Child and Family Psychology Review. 1998;1:125–144. doi: 10.1023/a:1021887712873. [DOI] [PubMed] [Google Scholar]
- Shahar G, Blatt SJ, Zuroff DC, Kuperminc G, Leadbeater BJ. Reciprocal relations between depressive symptoms and self-criticism (but not dependency) among early adolescent girls (but not boys) Cognitive Therapy and Research. 2004;28:85–103. [Google Scholar]
- Starr LR, Davila J. Differentiating interpersonal correlates of depressive symptoms and social anxiety in adolescence: Implications for models of comorbidity. Journal of Clinical Child & Adolescent Psychology. 2008;37:337–349. doi: 10.1080/15374410801955854. [DOI] [PubMed] [Google Scholar]
- Starr LR, Davila J. Responding to anxiety with rumination and hopelessness: Mechanism of anxiety-depression symptoms co-occurrence? Cognitive Therapy and Research. 2012a;36:321–337. doi: 10.1007/s10608-011-9363-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starr LR, Davila J. Cognitive and interpersonal moderators of daily co-occurrence of anxious and depressed moods in generalized anxiety disorder. Cognitive Therapy and Research. 2012b;36:655–669. doi: 10.1007/s10608-011-9434-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storch EA, Caporino NE, Morgan JR, Lewin AB, Rojas A, Brauer L, Murphy TK. Preliminary investigation of web-camera delivered cognitive-behavioral therapy for youth with obsessive-compulsive disorder. Psychiatry Research. 2011;189:407–412. doi: 10.1016/j.psychres.2011.05.047. [DOI] [PubMed] [Google Scholar]
- Trew JL. Exploring the roles of approach and avoidance in depression: An integrative model. Clinical Psychology Review. 2011;31:1156–1168. doi: 10.1016/j.cpr.2011.07.007. [DOI] [PubMed] [Google Scholar]
- Twenge JM, Nolen-Hoeksema S. Age, gender, race, socioeconomic status, and birth cohort difference on the children's depression inventory: A meta-analysis. Journal of abnormal psychology. 2002;111:578. doi: 10.1037//0021-843x.111.4.578. [DOI] [PubMed] [Google Scholar]
- Velting ON, Setzer NJ, Albano AM. Update on and advances in assessment and cognitive-behavioral treatment of anxiety disorders in children and adolescents. Professional Psychology: Research and Practice. 2004;35:42–54. [Google Scholar]
- Westen D, Novotny CM, Thompson-Brenner H. The empirical status of empirically supported psychotherapies: Assumptions, findings, and reporting in controlled clinical trials. Psychological Bulletin. 2004;130:631–663. doi: 10.1037/0033-2909.130.4.631. [DOI] [PubMed] [Google Scholar]
- Willett JB, Singer JD, Martin NC. The design and analysis of longitudinal studies of development and psychopathology in context: Statistical models and methodological recommendations. Development and Psychopathology. 1998;10:395–426. doi: 10.1017/s0954579498001667. [DOI] [PubMed] [Google Scholar]
- Young JF, Mufson L, Davies M. Impact of comorbid anxiety in an effectiveness study of interpersonal psychotherapy for depressed adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:904–912. doi: 10.1097/01.chi.0000222791.23927.5f. [DOI] [PubMed] [Google Scholar]