Abstract
Adult subjects with systemic capillary leak syndrome (SCLS) present with acute and recurrent episodes of vascular leak manifesting as severe hypotension, hypoalbuminemia, hemoconcentration, and generalized edema. We studied clinical disease characteristics, serum cytokine profiles, and treatment modalities in a cohort of children with documented SCLS. Six children with SCLS were recruited from the United States, Australia, Canada, and Italy. Serum cytokines from SCLS subjects and a group of 10 healthy children were analyzed. Children with SCLS (aged 5–11 years old) presented with at least 1 acute, severe episode of hypotension, hypoalbuminemia, and hemoconcentration in the absence of underlying causes for these abnormalities. In contrast to what is observed in adult SCLS, identifiable infectious triggers precipitated most episodes in these children, and none of them had a monoclonal gammopathy. We found elevated levels of chemokine (C-C motif) ligand 2 (CCL2), interleukin-8, and tumor necrosis factor α in baseline SCLS sera compared with the control group. All patients are alive and well on prophylactic therapy, with 4 patients receiving intravenous or subcutaneous immunoglobulins at regular intervals. The clinical manifestations of pediatric and adult SCLS are similar, with the notable exceptions of frequent association with infections and the lack of monoclonal gammopathy. Prophylactic medication, including high dose immunoglobulins or theophylline plus verapamil, appears to be safe and efficacious therapy for SCLS in children.
Keywords: systemic capillary leak syndrome, vascular hyperpermeability, intravenous immunoglobulin, inflammatory cytokines
In 1960, Clarkson et al1 first described a young woman presenting with recurrent episodes of shock due to “sudden phenomenal loss of plasma from her vascular bed.” Since then, only 200 to 300 similar cases of what was later termed the “systemic capillary leak syndrome” (SCLS) have been reported.2,3 Most of the documented subjects are adults, who experience recurrent episodes of severe hypotensive shock due to extravasation of plasma fluid and proteins into the interstitium, resulting in hemoconcentration, hypoalbuminemia, hyponatremia, and severe generalized edema. SCLS is associated with substantial morbidity and mortality, with a 5-year overall survival of 73% to 76%.3,4
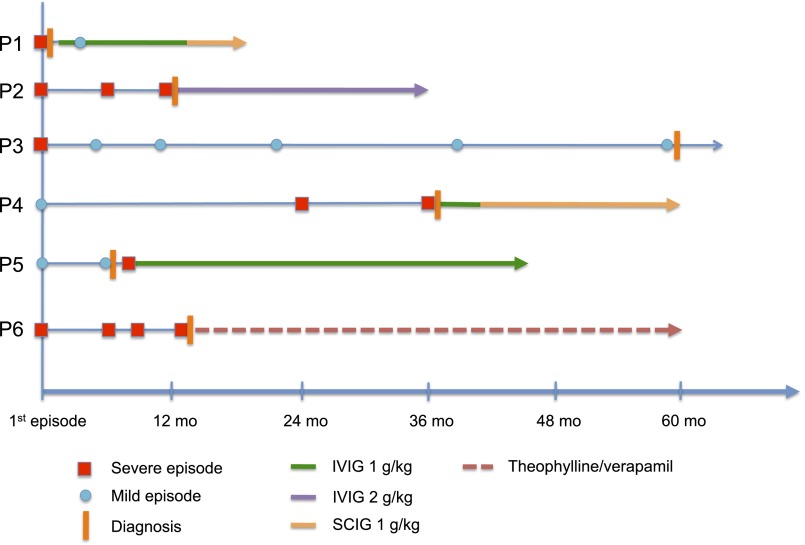
A European registry of predominantly adult patients with SCLS suggested statistically significant increases in survival in those receiving prophylactic therapy (including theophylline and terbutaline and/or intravenous immunoglobulin [IVIG]) compared with patients who received no prophylaxis.3 Only 9 cases of clear-cut, idiopathic SCLS have been reported previously in children.3,5–12 Here we describe 6 children, aged between 5 months and 11 years, who presented with recurrent episodes of systemic capillary leak. Children were given prophylactic therapy successfully, which included theophylline plus verapamil or intravenous or subcutaneous IgG. We summarize clinical investigations (Fig 1 and Table 1) and serum cytokine analysis (Fig 2). Methods and statistical analysis are described in the Supplemental Information.
FIGURE 1.
Longitudinal follow-up of 6 children with SCLS. Clinical course, date of formal diagnosis of SCLS, and treatments were recorded after the initial presenting episode over the time periods indicated as denoted by each symbol.
TABLE 1.
Summary of Clinical Investigations
| P1 | P2 | P3 | P4 | P5 | P6 | Foeldvari et al 19955 | Karatzios et al 20066 | Onal et al 20077 | Dowden et al 20098 | Sion-Sarid et al 20109 | Gousseff et al 20113 | Piastra et al 201210 | Perme et al 201311 | Iwasa et al 201412 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Current age, ya | 9 | 5 | 11 | 8 | 8 | 9 | 9 | 6 | 7 | 6 | 8 | 5 | 9 | 11 | 11 |
| Age at first episode | 8 y | 2y | 5 y | 3 y | 4.5 y | 3 y | 3 y | 5 y | 5 m | 6 y | 5 m | 5 y | 6 y | 8 y | 10 y |
| Gender | M | F | F | F | M | F | F | F | M | M | M | F | F | M | F |
| Number of severe acute episodesb | 1 | 3 | 1 | 2 | 1 | 4 | 5 | 2 | 3 | 1 | 5 | 2 | 2 | 2 | 2 |
| Mild episodesc | 1 | No | Multiple with viral illness | 1 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 |
| Infectious trigger (NPA or throat swab) | Rhinovirus parainfluenza 3 | Respiratory syncytial virus influenza B | Influenza A | Rhinovirus, parainfluenza, paronychia | Influenza A | Group A Streptococcus | Unknown | Influenza A (H3N2) | Unknown | Unknown | Unknown | Unknown | Unknown | Influenza A (H3N2 and H1N1) | Unknown |
| Prodrome | Lethargy, coryzal symptoms, abdominal and leg pain, thirst, vomiting | Coryzal Sx, vomiting, fever | Fever, lethargy, abdominal and leg pain, thirst, vomiting | Fever, coryzal symptoms, headache, periorbital swelling, cough, abdominal pain, vomiting | Fever, lethargy, sore throat, periorbital swelling, abdominal pain, vomiting, diarrhea | Cough, periorbital swelling | Cough, fever anorexia | Fever, abdominal pain, vomiting | Vomiting, diarrhea | Fever, vomiting | Abdominal pain, vomiting | Unknown | Fever, cough | Fever, coryzal symptoms, periorbital swelling | Fever, abdominal pain, diarrhea |
| Leak phase | 3 Hsd | 3 Hsd | 3 Hsd | 3 Hsd | 3 Hsd | 3 Hsd | 3 Hsd | 3 Hsd | 3 Hsd | 3 Hsd | 3 Hsd | 3 Hsd | 3 Hsd | 3 Hsd | 3 Hsd |
| Postleak diuresis | Yes, pulmonary edema | Yes, pulmonary edema | Yes | Yes, pulmonary edema | Yes, pulmonary edema requiring extracorporeal membrane oxygenation | Unknown | Unknown | Unknown | Yes | Unknown | Yes, pulmonary edema | Unknown | Yes, pulmonary edema | Unknown | Yes, pulmonary edema |
| Nonfatal complications | NA | Pericardial effusion | Compartment syndrome Rhabdomyolysis | Pleural effusion | Cardiac arrest, pericardial and pleural effusion, ascites | Compartment syndrome, Rhabdomyolysis, peroneal neuropathy | No | Compartment syndrome, Rhabdomyolysis | No | Compartment syndrome | Cerebral edema, acute renal failure | Unknown | Rhabdomyolysis | Rhabdomyolysis, renal failure | Compartment syndrome, fasciotomies, rhabdomyolysis, ascites, pleural and pericardial effusion, ARF requiring CHDF |
| Acute CRP (mg/L) | 10 | 12 | 14.7 | 22 | ND | Unknown | Unknown | 8 | Unknown | Unknown | Normal | Unknown | Normal | <3 | 32.4 |
| Acute complements (C3, C4) | Low C3, C4 | Normal | Low C3, C4 | Low C3, C4 | Low C3 | Unknown | Low C3 | Unknown | Normal | Unknown | Unknown | Unknown | Unknown | Unknown (baseline normal) | Unknown |
| Acute CH50 | Normal | Normal | Low | ND | ND | Unknown | Unknown | Unknown | Unknown | Unknown | Unknown | Unknown | Unknown | Unknown | |
| C1 esterase inhibitor | Normal | Normal | Normal | Normal | ND | Normal | Normal | Normal | Normal | Unknown | Unknown | Unknown | Normal | Normal | Unknown |
| Serum Tryptase | Normal | Normal | ND | Increased (17.6) | ND | Unknown | Unknown | Unknown | Unknown | Unknown | Unknown | Unknown | Normal | Unknown | Unknown |
| Monoclonal gammopathy | No | No | No | No | No | No | No | Unknown | No | Unknown | No | Unknown | Unknown | No | Unknown |
| Acute Igs (g/L) | Low IgG (4.96) and IgM (0.28) | Normal | Low IgG (4.61) | Low IgG (3.2) and IgM (0.36) | Low IgG (4.3) | Unknown | Low IgG | Unknown | Unknown | Unknown | Unknown | Unknown | Normal | Unknown (baseline normal) | Unknown |
| ANA titer | Negative | 160 speckled | 2560 speckled | Negative | Negative | Unknown | Negative | Unknown | Unknown | Unknown | Unknown | Unknown | Negative | Unknown | Unknown |
| Prophylactic therapy | SCIG | IVIG | No | SCIG | IVIG | Theophylline, verapamil | Unknown | Unknown | Theophylline, ginkgo biloba | No | Unknown | Unknown | No | No | Theophylline, terbutaline |
| Outcomea | Alive | Alive | Alive | Alive | Alive | Alive | Alive | Alive | Alive | Dead | Alive | Alive | Alive | Alive | Alive |
ND, not done.
At the time of publication.
Acute episodes presenting as shock requiring fluid resuscitation and/or PICU admission.
Acute episodes of swelling without shock.
Hypotension, hemoconcentration, hypoalbuminemia.
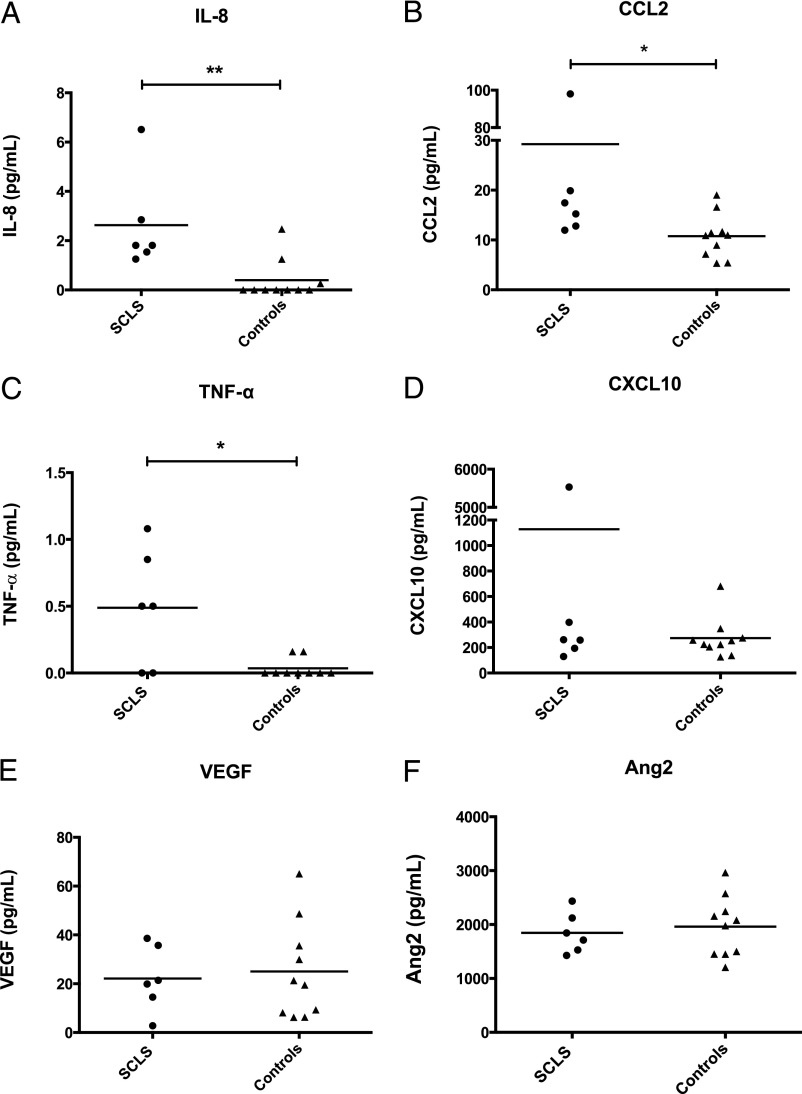
FIGURE 2.
Cytokine profiles of pediatric SCLS sera. A–F, Cytokine levels in sera from 6 asymptomatic children with SCLS and 10 healthy children without SCLS were measured by multiplexed enzyme-linked immunosorbent assay or standard enzyme-linked immunosorbent assay (Ang2). *P < .05, **P = .0003, Mann-Whitney U test.
Case Summaries
Case 1
An 8-year-old white boy presented with acute shock and generalized edema, which was preceded by 2 days of coryzal symptoms, lethargy, excessive thirst, and vomiting. He exhibited tachycardia (170 beats per minute), hypotension (74/36 mm Hg), metabolic acidosis, marked hemoconcentration (hemoglobin [Hgb] 225 g/L), and hypoalbuminemia (20 g/L). He was stabilized with multiple fluid boluses and a 4% albumin infusion. The edema resolved slowly over 4 days, followed by diuresis and development of pulmonary edema requiring oxygen supplementation. Although workup for presumed sepsis (blood, urine, and cerebrospinal fluid cultures) was negative, a nasopharyngeal aspirate (NPA) tested positive for Rhinovirus and Parainfluenza 3 by polymerase chain reaction. Two weeks later, he presented with mild facial and limb swelling, hemoconcentration, and hypoalbuminemia without hypotension, which responded to a short course of oral steroids. The diagnosis of SCLS was made, and IVIG infusions (1 g/kg monthly) were commenced without recurrence of further acute episodes. However, due to significant IVIG-related headaches and abdominal pain, subcutaneous immunoglobulin (SCIG) injections (80 mg/kg 3 times weekly) were substituted for IVIG, which he has tolerated well.
Case 2
A 22-month-old white girl presented with severe shock (blood pressure 46/21 mm Hg) and generalized edema after a 4-day history of fever, vomiting, and coryzal symptoms. Initial blood tests revealed significant hemoconcentration (Hgb 180 g/L), hypoalbuminemia (15 g/L), and metabolic acidosis. She was resuscitated with multiple fluid and albumin boluses. Twenty-four hours later, she developed significant polyuria and pulmonary edema requiring intubation and ventilation. Her clinical course was complicated by rhabdomyolysis (CK 14 590 IU/L), which resolved spontaneously. NPA tested positive for respiratory syncytial virus although all cultures were negative. An initial diagnosis of culture negative sepsis was made. At 28 and 33 months of age, she presented with shock associated with hemoconcentration and hypoalbuminemia, precipitated by nonspecific prodromal symptoms. The third episode (at 33 months) was complicated by pericardial effusion, which required drainage. On both occasions, all cultures were negative, but the NPA was positive for influenza B virus at the time of the last episode. Upon the third presentation, SCLS was diagnosed, and she was commenced on IVIG (2 g/kg per month). She remains well without further acute episodes.
Case 3
A 6-year-old white girl presented with pallor and shock after a 48-hour history of fever, coryzal symptoms, abdominal pain, and vomiting. She had significant hypotension (75/56 mm Hg) and metabolic acidosis on presentation, which was associated with hemoconcentration (Hgb 209 g/L) and hypoalbuminemia (18 g/L). Fluid boluses stabilized her hemodynamic status; however, her edema worsened, resulting in compartment syndrome of the left arm and both legs and rhabdomyolysis (creatine kinase [CK] 200 000 IU/L), necessitating fasciotomies. Although cultures were negative, NPA was positive for influenza A. She was discharged with a persistent right foot drop and a presumed diagnosis of severe viremia. The diagnosis of SCLS was made retrospectively 1 year ago at 11 years of age. Because her current symptoms are limited to moderate facial edema accompanying viral infections and she has not experienced a severe episode in 6 years, no prophylactic therapy was commenced.
Case 4
A 3-year-old girl presented with mild hypotension, lethargy, and periorbital edema after several days of coryzal symptoms and diarrhea. Mild hypoalbuminemia and hyponatremia were noted. She was discharged after treatment with antibiotics and intravenous fluids. At age 5, she presented with severe hypotensive shock (blood pressure 60/30 mm Hg) after a 2-day history of nonproductive cough, diarrhea, and a paronychia that was incised and drained (group A Streptococcus). She had significant hemoconcentration (Hgb 175 g/L), hypoalbuminemia (11 g/L), and hyponatremia (129 mmol/L). She was resuscitated with intravenous antibiotics, crystalloid, vasopressors, albumin, and stress dose steroids. Three days later, she was intubated for flash pulmonary edema. Infectious workup failed to reveal a source for presumed sepsis. At age 6, she again presented with hypotension, lower limb swelling, and oliguria associated with hemoconcentration and hypoalbuminemia after a 2-day prodrome of fever, abdominal pain, and vomiting. She was treated with intravenous albumin and IVIG (2 g/kg), which led to eventual recovery. At this stage, the diagnosis of SCLS was made. She was commenced on IVIG (2 g/kg monthly). However, due to severe postinfusion headaches, this therapy was replaced with biweekly SCIG (125 mg/kg). She remains well on this regimen and has had no further episodes.
Case 5
A 4-year-old boy, who presented with a 3-day history of coryzal symptoms and periorbital edema, was noted to have hemoconcentration (Hgb 182 g/L), hyponatremia (120 mmol/L), and hypoalbuminemia (17 g/L) at the time of admission, but he did not develop hypotension and recovered after receiving fluid resuscitation and antibiotics for presumed sepsis. Six months later, he presented with similar signs and symptoms after a several-day bout of vomiting and diarrhea, which again resolved with administration of intravenous saline and albumin. At that time, treatment with montelukast was begun for presumed SCLS. One month later, he presented with hypotension and hypoalbuminemia after flulike symptoms. Shortly after admission, he developed severe shock with cardiac arrest, requiring 43 minutes of cardiopulmonary resuscitation and 4 days of extracorporeal membrane oxygenation. Further studies revealed ascites, pericardial and pleural effusions, and influenza A infection. He recovered after treatment with oseltamivir, steroids, broad-spectrum antibiotics, and IVIG. Subsequently, therapy with monthly IVIG (1 g/kg) was initiated, and he has remained symptom-free for more than 3 years.
Case 6
This patient’s clinical presentation was reported previously13 and is summarized in Table 1 and Fig 1.
Discussion
Here we report the largest case series thus far of idiopathic SCLS in children. We noted several differences between pediatric and adult SCLS. Nearly all pediatric subjects (14 of 15) experienced a flulike prodrome, in contrast to adults, in whom 25% to 50% of the episodes were preceded by a flulike illness.4,14 All of the patients in our cohort and 8 of 15 reported cases overall (53%) had a documented infectious trigger. Secondly, none of the pediatric patients tested to date had a monoclonal gammopathy (n = 10). By contrast, 75% to 95% of adults with classic acute SCLS have monoclonal gammopathy of undetermined significance.2,3
Our current and limited understanding of SCLS pathogenesis is that endothelial contraction and adhesive junction remodelling lead to capillary hyperpermeability and subsequent plasma extravasation.14,15 Although the high prevalence of monoclonal gammopathy of undetermined significance in adult cases raises the possibility of a paraprotein/autoantibody-mediated mechanism, we and others14–16 have been unable to demonstrate a direct pathogenic function of the monoclonal IgG in SCLS. Other soluble factors such as cytokines could also have a role. A previous report8 and our recent study17 revealed elevated levels of inflammatory cytokines (interleukin [IL]-1β, IL-6, IL-8, IL-12, CXCL10 (chemokine [C-X-C motif]) ligand 10, chemokine (C-C motif) ligand 2, and tumor necrosis factor α [TNF-α]) and canonical permeability mediators (vascular endothelial growth factor [VEGF] and angiopoietin 2) in acute adult SCLS sera. Episodic SCLS sera, but not control sera, induced endothelial barrier dysfunction in vitro.14,15 In contrast, we found elevated levels of IL-8, TNF-α, and CCL2 in pediatric SCLS sera compared with sera from healthy control children, whereas concentrations of VEGF, Ang2, or CXCL10 were not different from controls (Fig 2). However, the absolute levels of all cytokines were much lower in the children tested than those seen in adults.
Although the role of IVIG for the prevention of SCLS episodes in adults is now well-established,3,18–21 its use in pediatric SCLS has not been reported. Four of our 6 patients were treated with IV or SCIG, and none had a further severe episode while on this treatment, suggesting that immunoglobulin prophylaxis (1–2 g/kg per month) is effective therapy for SCLS in children. Two patients did not tolerate this high dose of IVIG well, experiencing significant postinfusion symptoms despite premedication. SCIG injections, which are associated with lower peak immunoglobulin levels, appear to be a suitable alternative in these instances.
Finally, an important question regarding pediatric SCLS is the natural history of the disease, which then dictates the length of prophylactic therapy. One of our patients (P3) was not commenced on prophylaxis but has remained well with only mild infection-associated edema. Although further longitudinal studies are required, it is possible that SCLS in children resolves spontaneously over time.
Conclusions
Our case series suggests potential differences in the pathophysiology of adult and pediatric SCLS. Although the study is limited by its small sample size, our observations suggest that maintenance therapy for SCLS, including IVIG or theophylline plus verapamil, is effective prophylaxis for this rare but serious condition in children.
Supplementary Material
Acknowledgments
We thank Laura Wisch, MS, Celeste Nelson, MS, Michael Young, BS (National Institute of Allergy and Infectious Diseases, National Institutes of Health); Brynn Wainstein, MD, PhD (Department of Immunology and Infectious Diseases, Sydney Children’s Hospital, Sydney, Australia), Gary Williams, MD (Pediatric ICU, Sydney Children’s Hospital, Sydney, Australia); Stephen Jacobe, MD (Pediatric ICU, The Children’s Hospital at Westmead, Sydney, Australia); Hemant P. Sharma, MD, MHS. (Department of Allergy and Immunology, Children’s National Medical Center, Washington, DC); and Iain C. Jamieson, MD, Peterborough Regional Health Centre, Peterborough, Ontario, Canada, for recruiting, caring for, and referring patients for the study.
Footnotes
Drs Hsu, Xie, Stone, and Druey conceptualized and designed the study and drafted the initial manuscript; Dr Xie performed cytokine analysis; Drs Kakakios, Wong, and Frith assisted in writing the case summaries and critically edited the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported in part by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases, National Institutes of Health (project number AI001830, to Dr Druey). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Clarkson B, Thompson D, Horwith M, Luckey EH. Cyclical edema and shock due to increased capillary permeability. Am J Med. 1960;29:193–216 [DOI] [PubMed] [Google Scholar]
- 2.Druey KM, Greipp PR. Narrative review: the systemic capillary leak syndrome. Ann Intern Med. 2010;153(2):90–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gousseff M, Arnaud L, Lambert M, et al. Capillary Leak Syndrome Registry . The systemic capillary leak syndrome: a case series of 28 patients from a European registry. Ann Intern Med. 2011;154(7):464–471 [DOI] [PubMed] [Google Scholar]
- 4.Kapoor P, Greipp PT, Schaefer EW, et al. Idiopathic systemic capillary leak syndrome (Clarkson’s disease): the Mayo clinic experience. Mayo Clin Proc. 2010;85(10):905–912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Foeldvari I, Waida E, Junker AK. Systemic capillary leak syndrome in a child. J Pediatr. 1995;127(5):739–741 [DOI] [PubMed] [Google Scholar]
- 6.Karatzios C, Gauvin F, Egerszegi EP, et al. Systemic capillary leak syndrome presenting as recurrent shock. Pediatr Crit Care Med. 2006;7(4):377–379 [DOI] [PubMed] [Google Scholar]
- 7.Onal H, Aktuglu-Zeybek C, Altun G, Ozyilmaz I, Alhaj S, Aydin A. Capillary leak syndrome in a 5-month-old infant associated with intractable diarrhoea. Ann Trop Paediatr. 2007;27(1):81–86 [DOI] [PubMed] [Google Scholar]
- 8.Dowden AM, Rullo OJ, Aziz N, Fasano MB, Chatila T, Ballas ZK. Idiopathic systemic capillary leak syndrome: novel therapy for acute attacks. J Allergy Clin Immunol. 2009;124(5):1111–1113 [DOI] [PubMed] [Google Scholar]
- 9.Sion-Sarid R, Lerman-Sagie T, Blumkin L, Ben-Ami D, Cohen I, Houri S. Neurologic involvement in a child with systemic capillary leak syndrome. Pediatrics. 2010;125(3). Available at: www.pediatrics.org/cgi/content/full/125/3/e687 [DOI] [PubMed] [Google Scholar]
- 10.Piastra M, Pietrini D, Conti G, De Rosa G, Rigante D. Sudden shock from capillary leak. Lancet. 2012;379(9819):976. [DOI] [PubMed] [Google Scholar]
- 11.Perme T, Pokorn M, Markelj G, et al. Two episodes of systemic capillary leak syndrome in an 8-year-old boy, following influenza A virus infection. Pediatr Infect Dis J. 2014;33(2):222–224 [DOI] [PubMed] [Google Scholar]
- 12.Iwasa T, Ohashi H, Kihira K, et al. 10-year-old girl with life-threatening idiopathic systemic capillary leak syndrome: a case report. BMC Pediatr. 2014;14:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Milani GP, Dellepiane RM, Castellazzi ML, Mazzoni MBM, Bianchetti MG, Fossali EF. Episodic idiopathic systemic capillary leak syndrome in a girl. Pediatr Int. 2013;55(4):e81–e82 [DOI] [PubMed] [Google Scholar]
- 14.Xie Z, Ghosh CC, Patel R, et al. Vascular endothelial hyperpermeability induces the clinical symptoms of Clarkson disease (the systemic capillary leak syndrome). Blood. 2012;119(18):4321–4332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xie Z, Ghosh CC, Parikh SM, Druey KM. Mechanistic classification of the systemic capillary leak syndrome: Clarkson disease. Am J Respir Crit Care Med. 2014;189(9):1145–1147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang W, Ewan PW, Lachmann PJ. The paraproteins in systemic capillary leak syndrome. Clin Exp Immunol. 1993;93(3):424–429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xie Z, Chan E, Yin Y, et al. Inflammatory Markers of the Systemic Capillary Leak Syndrome (Clarkson Disease). J Clin Cell Immunol. 2014;5:1000213 doi:10.4172/2155-9899.1000213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lambert M, Launay D, Hachulla E, et al. High-dose intravenous immunoglobulins dramatically reverse systemic capillary leak syndrome. Crit Care Med. 2008;36(7):2184–2187 [DOI] [PubMed] [Google Scholar]
- 19.Pecker M, Adams M, Graham W. The systemic capillary leak syndrome. Ann Intern Med. 2011;155(5):335–, author reply 335–336. [DOI] [PubMed] [Google Scholar]
- 20.Marra AM, Gigante A, Rosato E. Intravenous immunoglobulin in systemic capillary leak syndrome: a case report and review of literature. Expert Rev Clin Immunol. 2014;10(3):349–352 [DOI] [PubMed] [Google Scholar]
- 21.Xie Z, Chan E, Long LM, Nelson C, Druey KM. High dose intravenous immunoglobulin therapy of the systemic capillary leak syndrome (Clarkson disease). Amer J Med. 2014. In press. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.