Abstract
Pseudomonas putida is a rod-shaped, non fermenting Gram-negative organism frequently found in the environment that utilizes aerobic metabolism, previously thought to be of low pathogenicity. It had been reported as cause of skin and soft tissue infection, especially in immunocompromised patients. A female green grocer, 51 year-old came to internal medicine out-patient clinic with gangrene and osteomyelitis on her 1st, 2nd and 3rd digit and wound on the sole of the right foot since 1 month prior. The patient had history of uncontrolled diabetes since a year ago. She was given ceftriaxone 2 grams b.i.d, metronidazole 500 mg t.i.d empirically and then amikacin 250 mg b.i.d, followed by amputation of the digits and wound debridement. The microorganism's culture from pus revealed multi drug resistant Pseudomonas putida. She recovered well after antibiotics and surgery.
Keywords: Diabetes, Pseudomonas putida, Skin and soft tissue infection
INTRODUCTION
Peudomonas putida, a rod-shaped non fermenting Gram-negative organism frequently found in the environment were previously thought to be of low pathogenicity. A study in Taiwan in 1996 found that P. putida-related infections were only 5% (3/55) of microbiological isolates from SSTI in a 5-year period.[1] A study in Japan in 2011[2] and Korea in 2012[3] found 5 and 18 cases of P. putida bacteremia respectively. In the last three decades, P. putida have been increasingly encountered as significant human pathogens.[3] It had been reported as cause of nosocomial infection in immunocompromised patients[4,5] and in patients possessing medical devices or catheters.[6,7] Outbreaks of blood stream infection associated with contaminated fluids have also been reported.[8] Clinical data on P. putida infections are lacking due to the rarity, relatively low virulence, and high antimicrobial susceptibility. However, the emergence of multi-drug-resistant (MDR) and carbapenem-resistant P. putida has become a concern.[9,10] Here, we report a multi drug resistant P. putida case in diabetic foot gangrene.
CASE REPORT
A female green grocer, 51 year-old came to internal medicine out-patient clinic with wound in right toe since 1 month prior. She did not realize how the wound originated. At the beginning it was only a small blister (diameter of 3 centimeters). After a week the blister became a wound that was painful when she walked. The wound was getting wider, with pus in it. She does not feel paresthesia or numbness in her feet. She also had continuous fever and decreased appetite 3 weeks prior. The patient suffered diabetes and hypertension since a year ago, but she seldom took medicines. She also had a history of same kind of wound in her left sole (diameter of 2 centimeters) 5 month prior, which resolved after a week of antibiotic ointment.
On physical examination, she was moderately ill, compos mentis, within tachycardia and fever. General examinations are within normal limit. On right foot examination, she got gangrene on her 1st, 2nd and 3rd digit and wound sized 15 by 4 centimeter on the palm of the sole. The gangrene was dirty and odorous. Laboratory examination showed leucocyte count 33,120/μl with 85% neutrophil, random blood glucose 252 mg/dl, and (++) proteinuria. Other laboratory examination, procalcitonin level, chest radiology and electrocardiography were within normal range. Her foot radiology showed porous structure, litic lesion on distal proximal phalangs of 1st digit and sub cuticular emphysema.
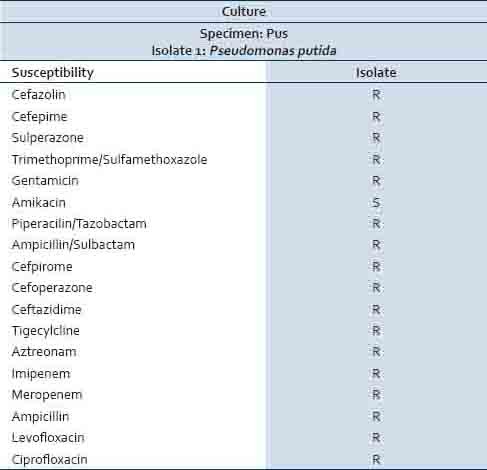
The patient was treated with sub cutaneous ultra fast insulin and empiric antibiotics of ceftriaxone 2 grams b.i.d and metronidazole 500 mg t.i.d. She undergone amputation of the 1st digit and wound debridement on 5th day of admission, then amputation of the 2nd and 3rd digit on the 10th day of admission. The leucocyte count was 13,700/μl with 83% neutrophil on the 10th day and the leucocyte was 9,500/μl on the 14th day. The microorganism's culture obtained from pus of the wound of 1st amputation revealed multi drug resistant Pseudomonas putida came out on the 10th day [Table 1]. Ceftriaxone were substituted with amikacin 250 mg b.i.d on the 10th day, according to the culture result. The patient was discharged on the 15th day of admission with good condition.
Table 1.
The microorganism culture obtained from pus of the wound of the patient
DISCUSSION
Pseudomonas putida is a rod-shaped, non fermenting Gram-negative organism frequently found in the environment that utilizes aerobic metabolism. It usually lived on the root of plants. It is able to tolerate environmental stresses due to its diverse control of proteins including protein and peptide secretion and trafficking, protein modification and repair, protein folding and stabilization, and degradation of proteins, peptides, and glycopeptides. Some important proteins include the global regulatory proteins which link the pathway genes to the cell status. An important protein of P. putida is the Crc protein which is part of the signal transduction pathway moderating the carbon metabolism. It also functions in bio film production.[11]
P. putida is generally considered to have a low level of virulence. A study revealed that the prognosis of P. putida bacteremia has been shown to be good, with 93% of cases being cured.[2] In contrast to previous reports, another study found that the mortality rate in P. putida bacteremia was high, where mortality rate in patients with P. putida pneumonia was 40% compared to 13% in previous studies.[3] In this case illustration, we report a case of P. putida skin and soft tissue infections in a 51 year-old female with diabetic foot gangrene. The patient had symptoms and signs of sepsis, such as tachycardia, fever, and leucocytosis; but the procalcitonin level was not elevated.
The underlying diseases of P. putida infection were solid tumor followed by traumatic intracranial hemorrhage, history of operation within the previous 3 months, and neutropenia. Eighty nine percent had been administered antibiotics within 1 month prior to bacteremia. Polymicrobial infection was found in one third cases.[3] The most common primary site of P. putida infection was the central venous catheter followed by ventilator-associated pneumonia and the biliary tract. Seventy seven percent were device-related infections (central venous catheter, endotracheal tube, biliary stent, and indwelling urinary catheter).[2] Pseudomonas putida is not commonly isolated from skin and soft tissue infections (SSTIs).[12,13] A study about P. putida infections over a 5-year period showed that SSTIs represented only 5% of cases. Of the 5 cases of SSTIs, 80% were associated with trauma, and the other case may have had an inoculating event given that they contracted the illness from wading through flood water. Bacteremia was present in only 1 of the 5 cases and appropriate antimicrobial therapy resulted in a good clinical outcome in all patients. Infection control also plays an important role in the treatment of P. putida SSTIs.[1] A case report on P. putida bacteremia due to skin and soft tissue infections that was lethal, which had malnutrition, immobility, and peripheral vascular disease as risk factors.[14] It can be concluded that P. putida infection and bacteremia is associated with an indwelling device or immunocompromised state.[1] In this case, the patient had uncontrolled diabetes mellitus with its micro and macro vascular complications, such as nephropathy and peripheral arterial disease as risk factors for P. putida infection. The patient works as green grocer at traditional market, owing to the possibility of her contact with P. putida in the plant roots.
Pseudomonas putida shows high susceptibility to various antibiotics. A study found 100% susceptibility of to ciprofloxacin and tobramycin and 87% to imipenem and piperacillin/tazobactam.[12] Studies recently have reported the emergence of multi drug resistant (MDR) and carbapenem-resistant P. putida isolates from the urinary tract, tracheal aspiration, and areas other than blood. This carbapenem-resistance mechanism was known to be related with metallo-β-lactamase (MBL) production. The carbapenem-resistance rates did not differ significantly from those of P. aeruginosa blood isolates (P = 0.771).[13]
The microorganism culture specimen obtained from this patient recovered multi drug resistant P. putida, only sensitive to amikacin. The patient had been treated with ceftriaxone and metronidazole for 10 days, and ceftriaxone was substituted with amikacin after culture result came out. Even that the result was good, as the patient's foot gangrene resolved and she was discharged with good condition. The first explanation was the difference of microorganism's susceptibility to antibiotics at in vitro and in vivo settings. The second explanation was the P. putida infection was not become a bacteremia, as the procalcitonin level was normal, so the wound debridement and amputation able to remove the source of infection before P. putida spread.
We have reported a case of multi drug resistant P. putida infection in diabetic foot gangrene. The infection was able to be taken care of and result was good, but we must be aware of the multi drug resistant P. putida in skin and soft tissue infection.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Yang CH, Young T, Peng MY. Clinical spectrum of Pseudomonas putida infection. J Formos Med Assoc. 1996;95:754–61. [PubMed] [Google Scholar]
- 2.Yoshino Y, Kitazawa T, Kamimura M, Tatsuno K, Ota Y, Yotsuyanagi H. Pseudomonas putida bacteremia in adult patients: Five case reports and a review of the literature. J Infect Chemother. 2011;17:278–82. doi: 10.1007/s10156-010-0114-0. [DOI] [PubMed] [Google Scholar]
- 3.Kim SE, Park SH, Park HB, Park KH, Kim SH, Jung SI, et al. Nosocomial Pseudomonas putida Bacteremia: High Rates of Carbapenem Resistance and Mortality. Chonnam Med J. 2012;48:91–5. doi: 10.4068/cmj.2012.48.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anaissie E, Fainstein V, Miller P, Kassamali H, Pitlik S, Bodey GP, et al. Pseudomonas putida. Newly recognized pathogen in patients with cancer. Am J Med. 1987;82:1191–4. doi: 10.1016/0002-9343(87)90223-3. [DOI] [PubMed] [Google Scholar]
- 5.Martino R, Martínez C, Pericas R, Salazar R, Solá C, Brunet S, et al. Bacteremia due to glucose non-fermenting gram-negative bacilli in patients with hematological neoplasias and solid tumors. Eur J Clin Microbiol Infect Dis. 1996;15:610–5. doi: 10.1007/BF01709374. [DOI] [PubMed] [Google Scholar]
- 6.Souza Dias MB, Habert AB, Borrasca V, Stempliuk V, Ciolli A, Araújo MR, et al. Salvage of long-term central venous catheters during an outbreak of Pseudomonas putida and Stenotrophomonas maltophilia infections associated with contaminated heparin catheter-lock solution. Infect Control Hosp Epidemiol. 2008;29:125–30. doi: 10.1086/526440. [DOI] [PubMed] [Google Scholar]
- 7.Oğuz SS, Unlü S, Saygan S, Dilli D, Erdoðan B, Dilmen U. Rapid control of an outbreak of Pseudomonas putida in a tertiary neonatal intensive care unit. J Hosp Infect. 2010;76:361–2. doi: 10.1016/j.jhin.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 8.Torii K, Noda Y, Miyazaki Y, Ohta M. An unusual outbreak of infusion-related bacteremia in a gastrointestinal disease ward. Jpn J Infect Dis. 2003;56:177–8. [PubMed] [Google Scholar]
- 9.Treviño M, Moldes L, Hernández M, Martínez-Lamas L, García-Riestra C, Regueiro BJ. Nosocomial infection by VIM-2 metallo-beta-lactamase-producing Pseudomonas putida. J Med Microbiol. 2010;59:853–5. doi: 10.1099/jmm.0.018036-0. [DOI] [PubMed] [Google Scholar]
- 10.Kumita W, Saito R, Sato K, Ode T, Moriya K, Koike K, et al. Molecular characterizations of carbapenem and ciprofloxacin resistance in clinical isolates of Pseudomonas putida. J Infect Chemother. 2009;15:6–12. doi: 10.1007/s10156-008-0661-9. [DOI] [PubMed] [Google Scholar]
- 11.Espinosa-Urgel M, Salido A, Ramos JL. Genetic Analysis of Functions Involved in Adhesion of Pseudomonas putida to Seeds. J Bacteriol. 2000;182:2363–9. doi: 10.1128/jb.182.9.2363-2369.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fass RJ, Barnishan J, Solomon MC, Ayers LW. In vitro activities of quinolones, beta-lactams, tobramycin, and trimethoprim-sulfamethoxazole against nonfermentative gram-negative bacilli. Antimicrob Agents Chemother. 1996;40:1412–8. doi: 10.1128/aac.40.6.1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bogaerts P, Huang TD, Rodriguez-Villalobos H, Bauraing C, Deplano A, Struelens MJ, et al. Nosocomial infections caused by multidrug-resistant Pseudomonas putida isolates producing VIM-2 and VIM-4 metallo-beta-lactamases. J Antimicrob Chemother. 2008;61:749–51. doi: 10.1093/jac/dkm529. [DOI] [PubMed] [Google Scholar]
- 14.Thomas BS, Okamoto K, Bankowski MJ, Seto TB. A Lethal Case of Pseudomonas putida Bacteremia Due to Soft Tissue Infection. Infect Dis Clin Pract (Baltim Md) 2013;21:147–213. doi: 10.1097/IPC.0b013e318276956b. [DOI] [PMC free article] [PubMed] [Google Scholar]


