Sir,
Elizabethkingia meningoseptica is a rare and unusual bacterium causing fulminant hospital infections. It is important to identify E. meningoseptica infections as the bacterium exhibits intrinsic resistance for most antimicrobial agents except quinolones, trimethoprim-sulfamethoxazole, rifampicin, and vancomycin.-[1,2] We describe a cluster of four cases, who developed ventilator associated pneumonia (VAP) with E. meningoseptica, in Intensive Care Unit (ICU) of our tertiary care hospital in March, 2013.
All were female patients with a mean age of 65.5 years (range: 49-77 years). The mean time of development of VAP due to E. meningoseptica after mechanical ventilation was 12.1 days (range: 3-17 days). Endotracheal aspirates from these patients were collected and sent to the microbiology laboratory for culture and identification of pathogen. Quantitative culture done on MacConkey agar and sheep blood agar showed significant growth of pathogen (≥105 CFU/ml) [Figures 1 and 2]. The biochemical characterization and VITEK identification revealed that the isolate in all four cases was E. meningoseptica (99% probability). Antimicrobial susceptibility testing performed by Kirby-Bauer disc diffusion method revealed that the bacterium was resistant to penicillins, cephalosporins, aminoglycosides, quinolones and colistin, but was susceptible to trimethoprim-sulfamethoxazole, rifampicin, and vancomycin in all four cases [Figure 3]. As there are still no standard guidelines for susceptibility testing of E. meningoseptica, interpretation of trimethoprim-sulfamethoxazole, rifampicin, and vancomycin susceptibility was done in comparison with Staphylococcus aureus (ATCC 25923). The results of susceptibility testing were later confirmed with VITEK 2 automated system. All four patients were treated with rifampicin, vancomycin, and trimethoprim-sulfamethoxazole. Mean duration of antibiotic therapy was 8.7 days. Improvement with therapy was seen in two patients, one patient expired, and one took discharge against advice.
Figure 1.
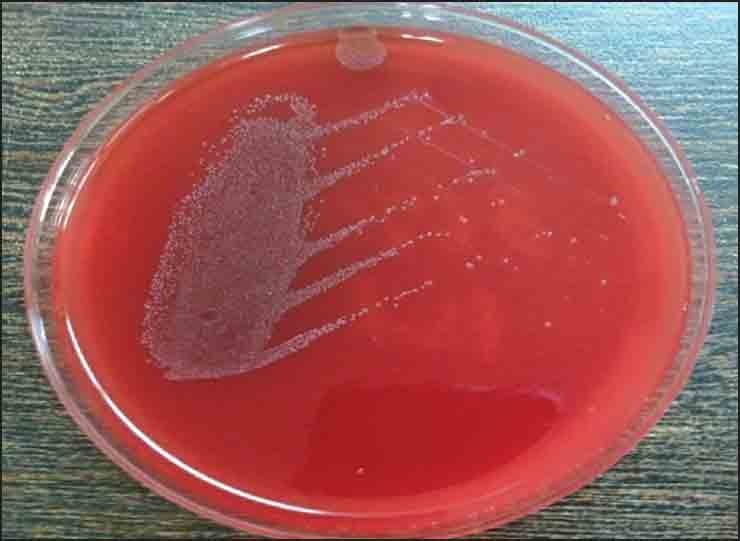
Blood agar showing growth of Elizabethkingia meningoseptica
Figure 2.

MacConkey agar showing growth of Elizabethkingia meningoseptica
Figure 3.
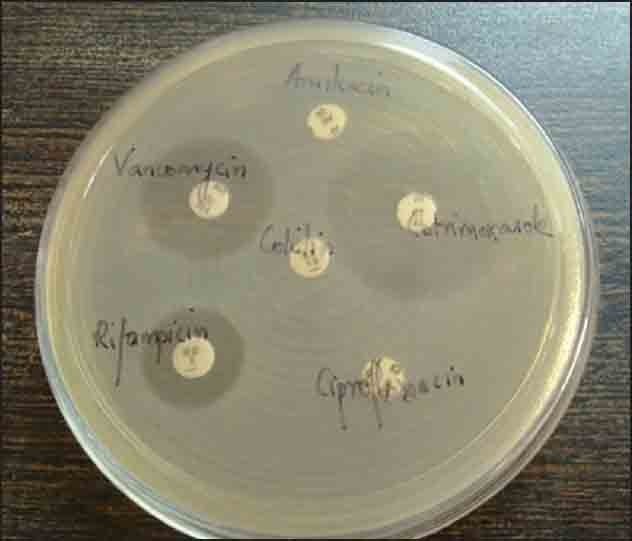
Antimicrobial susceptibility testing of Elizabethkingia meningoseptica by Kirby-Bauer disc diffusion method
To trace the source of infection multiple environmental samples were taken from ventilator machines, humidifier boxes, hospital trolley, AC duct, bed curtains, bed railings, saline bottles, and tap water of the ICU. E. meningoseptica with the same sensitivity pattern was isolated from the humidifier water. Thus, humidifier water was identified as the source of infection. The humidifier boxes in the ventilator circuit of all the four patients were sterilized by autoclave. Repeat samples taken from the humidifier boxes after sterilization did not yield any bacteria on culture.
Our study is the first report of an acute outbreak of VAP with E. meningoseptica in India. Earlier Weaver et al. in 2010 and Gόngφr et al. in 2003 have reported similar outbreaks.[3,4] The predisposing factors for infection with this pathogen are adults with some underlying severe illness, on life support devices and on prolonged antibiotic treatment.[3] Two out of four patients had predisposing comorbid illness like diabetes and carcinoma breast and all four patients were on a mechanical ventilator. Previous studies have shown that E. meningoseptica is found as colonizer in tap water, tubing of ventilators and in sink basins of the hospital wards.[5] Infections caused by E. meningoseptica have a high mortality rate due to the delay in the administration of appropriate therapy.
We stress the importance of awareness of infections caused by E. meningoseptica, and prompt collaborative action by microbiologist and infection control team to control such hospital outbreaks.
REFERENCES
- 1.Hsu MS, Liao CH, Huang YT, Liu CY, Yang CJ, Kao KL, et al. Clinical features, antimicrobial susceptibilities, and outcomes of Elizabethkingia meningoseptica (Chryseobacterium meningosepticum) bacteremia at a medical center in Taiwan, 1999-2006. Eur J Clin Microbiol Infect Dis. 2011;30:1271–8. doi: 10.1007/s10096-011-1223-0. [DOI] [PubMed] [Google Scholar]
- 2.Spangler SK, Visalli MA, Jacobs MR, Appelbaum PC. Susceptibilities of non-Pseudomonas aeruginosa gram-negative nonfermentative rods to ciprofloxacin, ofloxacin, levofloxacin, D-ofloxacin, sparfloxacin, ceftazidime, piperacillin, piperacillin-tazobactam, trimethoprim-sulfamethoxazole, and imipenem. Antimicrob Agents Chemother. 1996;40:772–5. doi: 10.1128/aac.40.3.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weaver KN, Jones RC, Albright R, Thomas Y, Zambrano CH, Costello M, et al. Acute emergence of Elizabethkingia meningoseptica infection among mechanically ventilated patients in a long-term acute care facility. Infect Control Hosp Epidemiol. 2010;31:54–8. doi: 10.1086/649223. [DOI] [PubMed] [Google Scholar]
- 4.Güngör S, Ozen M, Akinci A, Durmaz R. A Chryseobacterium meningosepticum outbreak in a neonatal ward. Infect Control Hosp Epidemiol. 2003;24:613–7. doi: 10.1086/502261. [DOI] [PubMed] [Google Scholar]
- 5.Amer MZ, Bandey M, Bukhari A, Nemenqani D. Neonatal meningitis caused by Elizabethkingia meningoseptica in Saudi Arabia. J Infect Dev Ctries. 2011;5:745–7. doi: 10.3855/jidc.1570. [DOI] [PubMed] [Google Scholar]


