Sir,
Non-fermenting Gram-negative bacilli (NFGNB) are a group of organisms that either do not utilize glucose as a source of energy or utilize it oxidatively. NFGNB can cause a significant number of infections, ranging from superficial to deep-seated and disseminated infections in immunocompromised hosts, neutropenic patients, patients with cystic fibrosis, patients on mechanical ventilation and indwelling catheters, and patients undergoing invasive diagnostic and therapeutic procedures. Blood stream infections (BSI) caused by NFGNB are a major cause of morbidity and mortality worldwide. High intrinsic resistance of NFGNB to antimicrobial compounds makes the treatment of BSIs caused by them difficult and expensive. NFGNB have a varied isolation rate, ranging from 2.18 to 45.9%, as observed from various clinical samples.[1]
In an attempt to recognize the antibiotic resistance and prevalence pattern among NFGNB associated with BSIs in cancer patients, a prospective study was conducted over a period of one year from July 2013 to June 2014, at a tertiary care cancer institute in North India. Blood culture was performed in BacT/Alert blood culture bottles (bioMerieux, Durham, North Carolina, USA). From the positive bottles, the subcultures were performed on MacConkey agar and blood agar. The VITEK®2 Compact (C) system (bioMerieux, North Carolina, USA) was used to identify NFGNB up to the species level, using the Gram-negative Identification (GN-ID) 21341 card, and antibiotic susceptibility testing (AST) was done using the AST 281 card. The antibiotic susceptibility results were expressed as susceptible, intermediate or resistant, according to the criteria of the Clinical Laboratory Standards Institute (CLSI) M100-S23 (2013).[2]
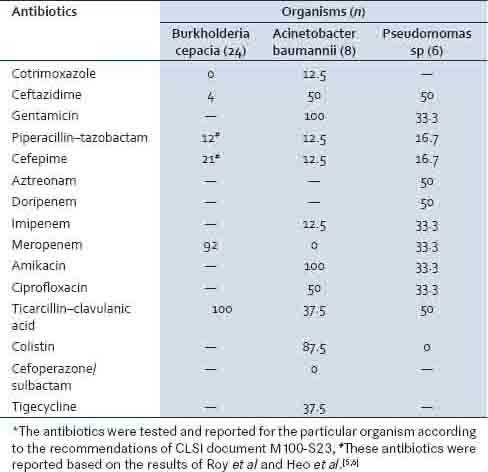
Among 815 total samples received for blood culture, 249 bottles were flagged as positive in the BacT Alert 3D. However, only 172 yielded pathogenic bacteria on subculture. Sixty-three (36.6%) were Gram-negative and 108 (62.7%) were Gram-positive organisms, while one isolate was fungus (Candida sp.). Forty, out of 63 (63.5%) Gram-negative organisms were NFGNB, out of which Burkholderia cepacia (60%) was the predominant isolate. Acinetobacter baumannii (20%), Pseudomonas aeruginosa (12.5%), Pseudomonas stutzeri (2.5%), Alcaligenes faecalis (2.5%), and Sphingomonas paucimobilis (2.5%) were the other NFGNB isolated from the blood stream infections. The antibiotic susceptibility results are given in Table 1, which shows the percentage of resistant isolates. A high level of resistance against the first- and second-line antibiotics was noted.
Table 1.
Antibiotic resistance pattern (percentage) of NFGNB isolated from blood culture
In this study, NFGNB were isolated from 4.9% of the total blood samples received for the culture. Out of the total Gram-negative bacilli, the NFGNB in our study were 63.5% (40/63), and B. cepacia was the predominant NFGNB. Prabash et al., in 2010, analyzed the blood cultures of cancer patients (neutropenic and non-neutropenic) and found that non-fermenters comprised a majority of the Gram-negative bacilli isolated (62.24%), with Pseudomonas (30.37%) and Acinetobacter sp. (11.57%) being the predominant NFGNBs.[3]
The in vitro anti-microbial susceptibility of Burkholderia cepacia isolates revealed 92% resistance to meropenem, while the susceptibility to co-trimoxazole was 100%. The 2010 Sanford Guide recommends co-trimoxazole as the treatment of choice for these infections. The other antibiotics to which B. cepacia isolates are susceptible are meropenem, ceftazidime, ceftibuten, chloramphenicol, and trimethoprim.[4] However, according to literature, the antibiogram of B. cepacia isolates from cancer patients may be slightly different, with increased susceptibility to some antibiotics, especially piperacillin, piperacillin-tazobactam, and cefepime.[5,6] One hundred and 87.5% of A. baumannii isolates were resistant to aminoglycosides and colistin, respectively, while all the isolates were susceptible to meropenem. Among the Pseudomonas species, a high level of resistance was recorded for ceftazidime (50%), aztreonam (50%), and doripenem (50%). Colistin and cefepime showed maximum activity with an overall susceptibility of 100 and 83.3%, respectively.
A single isolate of A. faecalis (2.5%) was resistant to all antibiotics, except amikacin. However, S. paucimobilis (2.5%) was a fairly sensitive strain, with resistance observed only against ceftazidime and aztreonam.
The emerging challenges of multidrug resistance, both intrinsic and acquired, among NFGNB, are of serious concern to the treating physician. Improved antibiotic stewardship and infection control measures will be needed to prevent or slow down the emergence and spread of multidrug-resistant NFGNB in the healthcare setting. Identification of NFGNB and monitoring their susceptibility patterns will help in improving the empirical therapy.
REFERENCES
- 1.Deepak J, Rajat P, Shamanth AS, Munesh S, Vikrant N, Neelam S. Prevalence of Non fermenting gram negative bacilli and their in vitro susceptibility pattern in a tertiary care hospital of Uttarakhand: A study from foot hills of Himalayas. Saudi J Health Sci. 2013;2:8–12. [Google Scholar]
- 2.Performance Standards for Antimicrobial Susceptibility Testing, 23rd Informational Supplement. Wayne: CLSI; 2013. Clinical and Laboratory Standards Institute. [Google Scholar]
- 3.Prabash K, Medhekar A, Ghadyalpatil N, Noronha V, Biswas S, Kurkure P, et al. Blood stream infections in cancer patients: A single center experience of isolates and sensitivity pattern. Indian J Cancer. 2010;47:184–8. doi: 10.4103/0019-509X.63019. [DOI] [PubMed] [Google Scholar]
- 4.Gilbert DN, Moellering RC, Jr, Eliopoulos GM, Chambers HF, Saag MS. The Sanford Guide to Antimicrobial Therapy. 40th ed. Sperryville, VA: Antimicrobial Therapy, INC.; 2010. [Google Scholar]
- 5.Roy P, Ahmed NH, Biswal I, Grover RK. Antimicrobial susceptibility patternof Burkholderia cepacia isolates from patients with malignancy. J Global Infect Dis. 2014;6:90–1. doi: 10.4103/0974-777X.132064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heo ST, Kim SJ, Jeong YG, Bae IG, Jin JS, Lee JC. Hospital outbreak of Burkholderia stabilis bacteraemia related to contaminated chlorhexidine in haematological malignancy patients with indwelling catheters. J Hosp Infect. 2008;70:241–5. doi: 10.1016/j.jhin.2008.07.019. [DOI] [PubMed] [Google Scholar]


