Abstract
OBJECTIVE
Obesity and type 2 diabetes continue to increase in prevalence in the U.S. Whether diabetes incidence continues to increase in recent times is less well documented. We examined trends in diabetes incidence over the previous four decades.
RESEARCH DESIGN AND METHODS
Framingham Heart Study participants ages 40–55 years and free of diabetes at baseline (n = 4,795; mean age 45.3 years; 51.6% women) were followed for the development of diabetes in the 1970s, 1980s, 1990s, and 2000s. Diabetes was defined as either fasting glucose ≥126 mg/dL or use of antidiabetes medication. Poisson regression was used to calculate sex-specific diabetes incidence rates for a 47-year-old individual in each decade. Rates were also calculated among obese, overweight, and normal weight individuals.
RESULTS
The annualized rates of diabetes per 1,000 individuals were 2.6, 3.8, 4.7, and 3.0 (women) and 3.4, 4.5, 7.4, and 7.3 (men) in the 1970s, 1980s, 1990s, and 2000s, respectively. Compared with the 1970s, the age- and sex-adjusted relative risks of diabetes were 1.37 (95% CI 0.87–2.16; P = 0.17), 1.99 (95% CI 1.30–3.03; P = 0.001), and 1.81 (95% CI 1.16–2.82; P = 0.01) in the 1980s, 1990s, and 2000s, respectively. Compared with the 1990s, the relative risk of diabetes in the 2000s was 0.85 (95% CI 0.61–1.20; P = 0.36).
CONCLUSIONS
In our community-based sample, the risk of new-onset diabetes continued to be higher in the 2000s compared with the 1970s. In the past decade, diabetes incidence remained steady despite the ongoing trend of rising adiposity.
Introduction
Recent studies indicate that prevalence of both prediabetes and overt diabetes continues to rise in the U.S. (1–3). This increasing prevalence may be due to an increase in diabetes incidence, improved survival among individuals with diabetes, or a combination of these factors.
The trends in prediabetes and diabetes prevalence have paralleled high rates of overweight and obesity, which are leading risk factors for the development of diabetes (4,5). Recent data, however, suggest the prevalence of obesity among adults, which was increasing from the 1970s through the early 2000s, may have leveled off in the past few years (4,6,7). Specifically, data from the National Health and Nutrition Examination Survey (a large nationally representative sample) suggested that the prevalence of obesity, while high, did not change significantly between 2003 and 2004 and 2011 and 2012 (6).
There are few estimates of trends in diabetes incidence in recent times (8). Some existing estimates focus on a single ethnic group or age group and thus may not apply to the general adult population (9,10). Other estimates are based on self-reported diabetes, which may underestimate the true incidence (11,12). We previously reported diabetes incidence in our cohort in the 1970s, 1980s, and 1990s (8), and in the current study, we seek to update these incidence estimates in the context of the obesity epidemic. In the Framingham Heart Study, screening for diabetes is conducted at each examination, along with measures of adiposity such as BMI. Thus, our study is able to provide reliable estimates of diabetes incidence and furthermore to assess the associations of overweight and obesity to the observed trends.
Research Design and Methods
Study Sample
The Framingham Heart Study is a community-based cohort study of cardiovascular disease and risk factors that has been in continuous operation since 1948 beginning with the Original Cohort. Recruitment of the Offspring Cohort began in 1971; participants were invited back for a second examination 8 years after the initial exam and subsequently every 4 years thereafter. Recruitment of the Third Generation Cohort began in 2001. The first examination cycle lasted from 2002 through 2005. The second examination cycle lasted from 2008 through 2011.
To ensure an overlapping age distribution across all decades, we limited the current analysis to participants ages 40 to 55 years who were free of diabetes at the baseline examination. Prevalent diabetes was defined as fasting glucose ≥126 mg/dL or on treatment with insulin or other antidiabetes agent. Offspring participants ages 40–55 years and free of diabetes at exam 1, which ran from 1971 to 1975, formed the sample for the 1970s. Using the same selection criteria, offspring participants from the second examination (1979–1983) formed the sample for the 1980s, and participants from the fourth examination (1987–1991) formed the sample for the 1990s. For the 1970s, 1980s, and 1990s, assessment of incident diabetes was performed at an exam ∼8 years later. Generation 3 participants from the first examination (2002–2005) formed the sample for the 2000s. Incident diabetes was assessed ∼6 years later at the second examination (2008–2011).
One individual who was included in the previous report from our cohort in the 1970s was excluded from the present analysis due to missing BMI (8). A total of 3,103 unique individuals from the Offspring Cohort (n = 1,587 women) contributed to 1,308, 1,551, and 1,663 person-examinations in the 1970s, 1980s, and 1990s, respectively. A total of 1,692 unique individuals from the Generation 3 Cohort (n = 889 women) were observed in the 2000s. Thus, the overall sample consisted of a total of 4,795 unique individuals (n = 2,476 women).
Assessment of Outcome
Incident diabetes was defined as a fasting plasma glucose ≥126 mg/dL or use of glucose-lowering medication at the follow-up examination. In a secondary analysis, we defined individuals with “diagnosed diabetes” cases if they were treated with a glucose-lowering agent at the time of the follow-up examination.
Metabolic Risk Factor Assessment
Key metabolic risk factors were measured at the clinic exam. BMI, defined as weight in kilograms (assessed using a Detecto scale; Detecto, Webb City, MO) divided by the square of the height in meters, was calculated. Waist circumference was measured at the level of the umbilicus and reported to the nearest quarter inch. Smoking status and alcohol consumption were assessed via physician interview. Seated systolic and diastolic blood pressures were measured on site manually using a mercury column sphygmomanometer. Total cholesterol was measured on fasting morning samples.
Hypertension was defined as systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or on treatment.
Statistical Analyses
Sex-specific mean age and BMI were calculated for each decade. To adjust for difference in follow-up time between cohorts, we used Poisson regression with duration of follow-up as an offset to calculate overall and sex-specific annualized diabetes incidence rates for a 47-year-old individual in each decade.
Next, we stratified individuals by BMI category—normal (BMI <25 kg/m2), overweight (BMI 25 to <30 kg/m2), class 1 obesity (BMI 30 to <35 kg/m2), or class 2 obesity (BMI ≥35 kg/m2)—and calculated diabetes incidence rates for a 47-year-old individual within each BMI category for each decade.
Using the 1970s as the reference period, we calculated overall and sex-specific age-adjusted relative risks of incident diabetes in the 1980s, 1990s, and 2000s. We also calculated overall and sex-specific age- and BMI-adjusted relative risks of incident diabetes in the 1980s, 1990s, and 2000s. Additionally, we calculated the relative risk of incident diabetes in the 2000s compared with the 1990s.
Finally, we characterized individuals who developed diabetes and individuals who remained free of diabetes based on demographics and standard cardiovascular risk factors including smoking status, blood pressure, and hypercholesterolemia.
All analyses were performed using SAS version 9.3.
Secondary Analyses
To evaluate the possibility that differences in incidence in the 2000s were attributable to the shorter accrual time (6-year follow-up vs. 8-year follow-up in other decades), we performed a sensitivity analysis by expanding the age range in the 2000s to include individuals from ages 40 to 57 years at baseline.
To assess whether diabetes detection is improving, we calculated rates of diagnosed diabetes for each decade.
Assessment of Bariatric Surgery
Because of the reported increases in bariatric surgery in the 2000s (13), we conducted a chart review to determine the number of participants who had undergone bariatric surgery. We selected all participants who had lost >20% of their body weight between baseline and follow-up examination. Fifteen participants were identified in this manner; we then performed a detailed chart review on these individuals to determine whether they had undergone a bariatric procedure. Of these, five had had a bariatric procedure, and two of the five had developed diabetes in the interval, which then resolved after weight loss.
Results
The mean age ranged from 46.0 years in the 1970s to 45.9 years in the 2000s. The mean BMI per decade were 25.0, 24.8, 25.6, and 26.4 kg/m2 among women and 26.9, 27.0, 27.8, and 28.0 kg/m2 among men in the 1970s, 1980s, 1990s, and 2000s respectively (Table 1).
Table 1.
Baseline characteristics and annualized rates of incident diabetes for a 47-year-old individual
| 1970s | 1980s | 1990s | 2000s | |
|---|---|---|---|---|
| Women, n | 656 | 786 | 862 | 889 |
| Age, years | 46 (4) | 47 (5) | 47 (4) | 46 (4) |
| BMI, kg/m2 | 25.0 (4.3) | 24.8 (4.5) | 25.6 (5.3) | 26.4 (6.0) |
| Incident diabetes, n | 13 | 24 | 32 | 19 |
| Annualized rate per 1,000 (95% CI) | 2.6 (1.5–4.5) | 3.8 (2.5–5.7) | 4.7 (3.3–6.7) | 3.6 (2.3–5.6) |
| Men, n* | 652 | 765 | 801 | 803 |
| Age, years | 46 (4) | 47 (5) | 47 (4) | 46 (4) |
| BMI, kg/m2 | 26.9 (3.2) | 27.0 (3.4) | 27.8 (3.9) | 28.0 (4.3) |
| Incident diabetes, n | 17 | 28 | 48 | 36 |
| Annualized rate per 1,000 (95% CI) | 3.4 (2.1–5.5) | 4.5 (3.1–6.6) | 7.4 (5.5–9.9) | 7.5 (5.4–10.5) |
| Overall, n | 1,308 | 1,551 | 1,663 | 1,692 |
| Incident diabetes, n | 30 | 52 | 80 | 55 |
| Annualized rate per 1,000 (95% CI) | 3.0 (2.1–4.3) | 4.1 (3.2–5.5) | 6.0 (4.8–7.5) | 5.5 (4.2–7.1) |
Data are mean (SD) or n unless otherwise indicated.
Overall sample included 2,476 unique women and 2,319 unique men; some individuals were included in more than one decade.
Overall Diabetes Incidence
The overall annualized rates of diabetes per 1,000 individuals were 3.0, 4.1, 6.0, and 5.5 in the 1970s, 1980s, 1990s, and 2000s, respectively (Table 1). The age-adjusted relative risks of diabetes were 1.37 (95% CI 0.87–2.16; P = 0.17) in the 1980s, 1.99 (95% CI 1.30–3.03; P < 0.01) in the 1990s, and 1.81 (95% CI 1.16–2.82; P = 0.01) in the 2000s, using the 1970s are the reference period (Table 2).
Table 2.
Relative risks of incident diabetes for individuals ages 40–55 years free of diabetes in the 1980s, 1990s, and 2000s compared with the 1970s
| Age-adjusted RR (95% CI) | P value | RR with age and BMI adjustment (95% CI) | P value | |
|---|---|---|---|---|
| Overall | ||||
| 1970s | Ref | 1 | ||
| 1980s | 1.37 (0.87–2.16) | 0.17 | 1.34 (0.85–2.11) | 0.20 |
| 1990s | 1.99 (1.30–3.03) | <0.01 | 1.58 (1.03–2.42) | 0.04 |
| 2000s | 1.81 (1.16–2.82) | 0.01 | 1.32 (0.84–2.08) | 0.22 |
| Women | ||||
| 1970s | Ref | Ref | ||
| 1980s | 1.45 (0.74–2.86) | 0.28 | 1.42 (0.72–2.80) | 0.31 |
| 1990s | 1.80 (0.94–3.44) | 0.08 | 1.40 (0.72–2.70) | 0.32 |
| 2000s | 1.37 (0.67–2.78) | 0.38 | 0.96 (0.47–1.97) | 0.92 |
| Men | ||||
| 1970s | Ref | Ref | ||
| 1980s | 1.32 (0.72–2.42) | 0.36 | 1.29 (0.71–2.37) | 0.40 |
| 1990s | 2.16 (1.24–3.76) | <0.01 | 1.68 (0.95–2.95) | 0.07 |
| 2000s | 2.20 (1.24–3.92) | <0.01 | 1.52 (0.84–2.75) | 0.16 |
Ref, referent; RR, relative risk.
Compared with the 1990s, the age-adjusted relative risk of diabetes incidence in the 2000s was 0.85 (95% CI 0.61–1.20; P = 0.36).
Sex-Specific Diabetes Incidence
The annualized diabetes rates for a 47-year-old woman per 1,000 individuals were 2.6, 3.8, 4.7, and 3.6 in the 1970s, 1980s, 1990s, and 2000s (Table 1). The corresponding rates in men were 3.4, 4.5, 7.4, and 7.5.
Among women the decade-specific, age-adjusted relative risks of diabetes with 1970s as a reference were 1.45, 1.80, and 1.37 in the 1980s, 1990s, and 2000s (Table 2). Among men the corresponding relative risks were 1.32 (P = 0.36), 2.16 (P < 0.01), and 2.20 (P < 0.01).
Diabetes Incidence by BMI Category
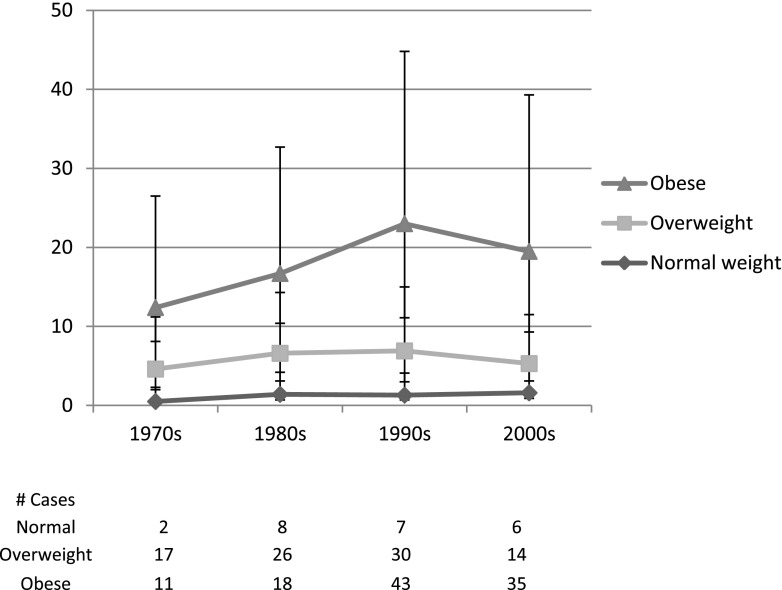
To evaluate the association between the risk of diabetes and increasing adiposity, we calculated diabetes incidence stratified by normal, overweight, or obese BMI (Fig. 1). Among class 1 obese individuals (BMI 30 to <35 kg/m2), the annualized rates of diabetes for a 47-year-old individual per 1,000 people were 7.0, 8.0, 14.1, and 7.5 in the 1970s, 1980s, 1990s, and 2000s, respectively (Table 3). Among class 2 obese individuals (BMI ≥35 kg/m2), the annualized rates were 11.7, 18.8, 21.7, and 26.7 per 1,000 in each successive decade. Thus, among class 1 obese, incidence rates were higher in the 1990s than in the 2000s, but among class 2 obese that trend was reversed. The number of individuals with class 2 obesity in each decade was relatively small, yielding wider CIs.
Figure 1.
Annualized rates of diabetes per 1,000 individuals. Age-adjusted annualized rates of diabetes for a 47-year-old per 1,000 individuals, stratified by normal, overweight, or obese BMI. Error bars represent 95% CIs. Number of participants at risk in the normal, overweight, and obese categories, respectively, in the 1970s were 585, 542, and 181; in the 1980s: 721, 604, and 226; in the 1990s: 671, 654, and 338; in the 2000s: 651, 637, and 404.
Table 3.
Annualized rates of diabetes by BMI category for a 47-year-old individual
| 1970s | 1980s | 1990s | 2000s | |
|---|---|---|---|---|
| Normal weight (BMI <25 kg/m2), n | 585 | 721 | 671 | 651 |
| BMI, mean (SD) | 22.7 (1.6) | 22.5 (1.7) | 22.5 (1.7) | 22.4 (1.7) |
| Incident diabetes, n | 2 | 8 | 7 | 6 |
| Annualized rate, per 1,000 individuals (95% CI) | 0.5 (0.1–1.8) | 1.4 (0.7–2.8) | 1.3 (0.6–2.8) | 1.6 (0.7–3.5) |
| Overweight (BMI 25 to <30 kg/m2), n | 542 | 604 | 654 | 637 |
| BMI, mean (SD) | 27.1 (1.4) | 27.2 (1.4) | 27.3 (1.4) | 27.3 (1.4) |
| Incident diabetes, n | 17 | 26 | 30 | 14 |
| Annualized rate, per 1,000 individuals (95% CI) | 4.1 (2.6–6.6) | 5.2 (3.5–7.7) | 5.6 (3.9–8.1) | 3.7 (2.2–6.2) |
| Class 1 obesity (BMI 30 to <35 kg/m2), n | 149 | 185 | 256 | 265 |
| BMI, mean (SD) | 31.9 (1.4) | 31.9 (1.3) | 32.0 (1.3) | 32.0 (1.4) |
| Incident diabetes, n | 8 | 12 | 29 | 12 |
| Annualized rate, per 1,000 individuals (95% CI) | 7.0 (3.5–13.9) | 8.0 (4.5–14.2) | 14.1 (9.7–20.5) | 7.5 (4.3–13.2) |
| Class 2 obesity (BMI ≥35 kg/m2), n | 32 | 41 | 82 | 139 |
| BMI, mean (SD) | 37.7 (3.4) | 38.8 (3.1) | 39.5 (4.4) | 39.3 (4.1) |
| Incident diabetes, n | 3 | 6 | 14 | 23 |
| Annualized rate, per 1,000 individuals (95% CI) | 11.7 (3.8–36.5) | 18.8 (8.4–41.9) | 21.7 (12.8–36.6) | 26.7 (17.7–40.5) |
Characterization of Individuals With Incident Diabetes
Cardiovascular risk factor profiles describing individuals who developed incident diabetes in each decade are presented as a descriptive analysis (Table 4).
Table 4.
Risk factor profiles by decade for diabetes and no diabetes (ages 40–55 years)
| 1970s | 1980s | 1990s | 2000s | |
|---|---|---|---|---|
| Diabetes, n | 30 | 52 | 80 | 55 |
| Age, years | 46 (3.1) | 49 (4.8) | 48 (4.3) | 47 (3.9) |
| Percent women | 43.3 | 46.2 | 40.0 | 34.6 |
| BMI, kg/m2 | 29.6 (4.2) | 29.7 (4.8) | 31.3 (6.5) | 32.9 (6.6) |
| Overweight, % | 56.7 | 50.0 | 37.5 | 25.5 |
| Obesity, % | 36.7 | 34.6 | 53.8 | 63.6 |
| Current smoking, % | 40.0 | 44.2 | 32.5 | 14.6 |
| Systolic blood pressure, mmHg | 135 (13.2) | 131 (14.4) | 131 (14.6) | 129 (15.6) |
| Hypertension, % | 63.3 | 50.0 | 46.3 | 45.5 |
| Antihypertension treatment, % | 20.0 | 30.8 | 20.0 | 30.9 |
| Total cholesterol, mg/dL | 217 (43.9) | 220 (37.0) | 200 (34.8) | 200 (35.3) |
| Lipid-lowering treatment, % | 0.0 | 0.0 | 3.8 | 14.6 |
| No diabetes, n | 1,278 | 1,499 | 1,583 | 1,637 |
| Age, years | 46 (4.1) | 47 (4.7) | 47 (4.4) | 46 (4.1) |
| Percent women | 50.3 | 50.8 | 52.4 | 53.2 |
| BMI, kg/m2 | 25.9 (3.8) | 25.7 (4.0) | 26.5 (4.5) | 26.9 (5.2) |
| Overweight, % | 41.1 | 38.6 | 39.4 | 38.1 |
| Obesity, % | 13.3 | 13.9 | 18.6 | 22.5 |
| Current smoking, % | 39.5 | 34.6 | 24.5 | 13.9 |
| Systolic blood pressure, mmHg | 126 (16.6) | 123 (15.2) | 122 (15.4) | 118 (14.4) |
| Hypertension, % | 28.1 | 23.8 | 24.8 | 21.9 |
| Antihypertension treatment, % | 5.5 | 9.9 | 9.2 | 12.0 |
| Total cholesterol, mg/dL | 211 (36.5) | 210 (36.6) | 203 (37.0) | 195 (33.8) |
| Lipid-lowering treatment, % | 1.1 | 0.8 | 2.0 | 10.8 |
Continuous data are shown as mean (SD).
Secondary Analyses
We considered that the shorter follow-up time in the 2000s (6 years) compared with the other decades (8 years) may have led to underestimation of the true diabetes incidence in the 2000s. To assess this possibility, we conducted a sensitivity analysis expanding the baseline age range to 40–57 years in the 2000s (Supplementary Table 1). In this analysis, the diabetes incidence rates were 3.6 per 1,000 women (95% CI 2.3–5.6) and 7.5 per 1,000 men (95% CI 5.4–10.4). These results are nearly identical to the primary analysis. Therefore, this shorter accrual period is unlikely to explain our findings.
The annualized rates of diagnosed diabetes per 1,000 for a 47-year-old individual increased steadily with each decade: 0.6 (95% CI 0.3–1.3) in the 1970s, 1.4 (95% CI 0.8–2.2) in the 1980s, 2.2 (95% CI 1.5–3.2) in the 1990s, and 3.0 (95% CI 2.1–4.3) in the 2000s.
Conclusions
In our community-based cohort, we observed that the risk of incident diabetes was higher in the 1990s compared with the 1970s. Diabetes incidence continued to be higher in the 2000s compared with the 1970s. Mean BMI has increased with each decade, and diabetes incidence remains highest among obese individuals. Notably, even among obese individuals, diabetes incidence rates increased in the 1990s and 2000s compared with the 1970s. Thus, rates of incident diabetes remained higher in the 2000s compared with the 1970s, likely related to ongoing high prevalence of obesity.
While there are some published studies reporting an increase in diabetes incidence in the 1990s (8,10), there are few other estimates of trends in U.S. diabetes incidence in the 2000s in the published literature. Data from the National Health Interview Survey from 1997–2003 showed an increase in diabetes incidence from 4.9 per 1,000 individuals in 1997 to 6.9 per 1,000 individuals in 2004 (14). There are several possible explanations for their reported increase in diabetes incidence, while we observed no increase over a similar time frame. Their data are based on self-report of diabetes and thus are less reliable than data obtained through directly measured fasting plasma glucose values and physician-reviewed medication history. Furthermore, the reported increase in diabetes incidence in that study could be due to improved detection of diabetes rather than a true population change in incidence. In contrast, our study followed the same individuals over time and applied a consistent definition of diabetes that included both diagnosed and undiagnosed cases. We conducted a sensitivity of diabetes incidence limited to diagnosed cases, and we observed an increase in diagnosed diabetes in each successive decade, suggesting that detection is indeed improving. Finally, the National Health Interview Survey includes a broader age range of 18–79 years. The inclusion of older individuals in particular would be expected to yield a different estimate than the age range used in our study. Consistent with our findings, another study reported that self-reported diabetes incidence in New York City was stabilizing, from 9.4 per 1,000 in 2002 to 8.6 per 1,000 in 2008 (11). However as discussed above, self-reported diabetes is likely less reliable; in this case, the incidence could be underestimated depending on patient education and access to health care.
Looking at recent trends in prediabetes can also help to inform trends in diabetes. The National Health and Nutrition Examination Survey data showed that prediabetes prevalence based on fasting glucose remained unchanged from 25.4% in 1999–2002 to 24.6% in 2003–2006 to 27.5% in 2007–2010 (1). Because prediabetes is a precursor of overt diabetes, this report that prediabetes did not change is consistent with our findings of stable diabetes incidence in the 2000s compared with the 1990s.
We also found that diabetes incidence did not change significantly in the 2000s compared with the 1990s, despite an increase in mean BMI and despite more individuals with class 2 obesity in the 2000s. There are several potential factors that may have contributed to the stable diabetes incidence that we observed between the 1990s and the 2000s. One possibility is that we underestimated diabetes in the 2000s because of the shorter accrual time (6 years) compared with the prior decades (8 years). We attempted to correct for this in a secondary analysis that expanded the age range studied in the 2000s, which did not significantly alter the results. Thus, the shorter accrual time is unlikely to have substantially impacted our results from the 2000s.
Second, observed differences in the 2000s may represent a “cohort effect.” Participants for the 2000s were drawn from a different population (Third Generation) than the participants from the prior decades (Offspring Cohort), and thus, observed differences in the 2000s may reflect a characteristic or exposure that is unique to the Third Generation cohort. Potential factors may include differences in diet or physical activity between cohorts, both of which could affect diabetes risk.
Third, increased use of bariatric surgery in the 2000s may have affected diabetes incidence. Bariatric procedures increased 10-fold in the U.S. from ∼16,200 in 1994 to 171,000 in 2005 (15). In our population, we identified only five individuals who had had bariatric surgery, only two of whom had documented diabetes. However, even if all five individuals would have developed diabetes had they not had bariatric surgery, this would not explain the stable incidence rate between the 1990s and 2000s.
Finally, it is possible that the leveling of diabetes incidence in the 2000s despite an increase in mean BMI compared with the 1990s is partly due to a saturation effect, meaning that the most susceptible individuals in the 2000s may have already acquired diabetes at baseline and thus been excluded from the current analysis. This possibility is plausible in the context of high obesity rates. This phenomenon has been described in the Pima Indian population, for example, in which diabetes incidence increased among ages 5–14 years but decreased among ages 25–34 years over the same time period (16).
Our descriptive analysis suggested that individuals diagnosed with diabetes in the 2000s seem to have lower rates of cigarette smoking and higher rates of treatment for other modifiable cardiovascular risk factors.
Strengths of our study include the large community-based cohort with directly measured BMI and fasting blood glucose as well as robust assessment of other cardiovascular risk factors. We did not rely on self-reported diabetes or height and weight, which can be susceptible to bias. Some limitations warrant mention. Our sample is primarily white and thus not generalizable across other ethnicities. Moreover, diabetes trends in the Framingham cohorts may not be nationally representative. Due to the age range used in this study (40–55 years), we would not have captured an increase in diabetes incidence at a younger age.
In our community-based sample, risk of diabetes increased in the 1990s and 2000s compared with the 1970s. Over the past decade, despite the ongoing trend of rising obesity, diabetes incidence remained relatively stable.
Article Information
Funding. The Framingham Heart Study of the National Heart, Lung, and Blood Institute is supported by contract N01-HC-25195. T.M.A. is supported by a National Institutes of Health–sponsored T32 training grant.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. T.M.A. researched data and wrote the manuscript. K.M.P. and M.J.P. performed statistical analysis and reviewed and edited the manuscript. C.S.F. researched data and reviewed and edited the manuscript. C.S.F. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc14-1432/-/DC1.
A slide set summarizing this article is available online.
References
- 1.Bullard KM, Saydah SH, Imperatore G, et al. Secular changes in U.S. Prediabetes prevalence defined by hemoglobin A1c and fasting plasma glucose: National Health and Nutrition Examination Surveys, 1999-2010. Diabetes Care 2013;36:2286–2293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ioannou GN, Bryson CL, Boyko EJ. Prevalence and trends of insulin resistance, impaired fasting glucose, and diabetes. J Diabetes Complications 2007;21:363–370 [DOI] [PubMed] [Google Scholar]
- 3.Selvin E, Parrinello CM, Sacks DB, Coresh J. Trends in prevalence and control of diabetes in the United States, 1988-1994 and 1999-2010. Ann Intern Med 2014;160:517–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960-1994. Int J Obes Relat Metab Disord 1998;22:39–47 [DOI] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA 2006;295:1549–1555 [DOI] [PubMed] [Google Scholar]
- 6.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012;307:491–497 [DOI] [PubMed] [Google Scholar]
- 7.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fox CS, Pencina MJ, Meigs JB, Vasan RS, Levitzky YS, D’Agostino RB Sr. Trends in the incidence of type 2 diabetes mellitus from the 1970s to the 1990s: the Framingham Heart Study. Circulation 2006;113:2914–2918 [DOI] [PubMed] [Google Scholar]
- 9.Dabelea D, Bell RA, D’Agostino RB Jr, et al.; Writing Group for the SEARCH for Diabetes in Youth Study Group . Incidence of diabetes in youth in the United States. JAMA 2007;297:2716–2724 [DOI] [PubMed] [Google Scholar]
- 10.Burke JP, Williams K, Gaskill SP, Hazuda HP, Haffner SM, Stern MP. Rapid rise in the incidence of type 2 diabetes from 1987 to 1996: results from the San Antonio Heart Study. Arch Intern Med 1999;159:1450–1456 [DOI] [PubMed] [Google Scholar]
- 11.Tabaei BP, Chamany S, Driver CR, Kerker B, Silver L. Incidence of self-reported diabetes in New York City, 2002, 2004, and 2008. Prev Chronic Dis 2012;9:E114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Incidence of diagnosed diabetes per 1,000 population aged 17–89 years, by age, 1980–2011 [article online], 2014. Available from http://www.cdc.gov/diabetes/statistics/incidence/fig3.htm. Accessed 24 November 2014
- 13.Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgical procedures. JAMA 2005;294:1909–1917 [DOI] [PubMed] [Google Scholar]
- 14.Geiss LS, Pan L, Cadwell B, Gregg EW, Benjamin SM, Engelgau MM. Changes in incidence of diabetes in U.S. adults, 1997-2003. Am J Prev Med 2006;30:371–377 [DOI] [PubMed] [Google Scholar]
- 15.Robinson MK. Surgical treatment of obesity—weighing the facts. N Engl J Med 2009;361:520–521 [DOI] [PubMed] [Google Scholar]
- 16.Pavkov ME, Hanson RL, Knowler WC, Bennett PH, Krakoff J, Nelson RG. Changing patterns of type 2 diabetes incidence among Pima Indians. Diabetes Care 2007;30:1758–1763 [DOI] [PubMed] [Google Scholar]