Abstract
The concept that excess superoxide production from mitochondria is the driving, initial cellular response underlying diabetes complications has been held for the past decade. However, results of antioxidant-based trials have been largely negative. In the present review, the data supporting mitochondrial superoxide as a driving force for diabetic kidney, nerve, heart, and retinal complications are reexamined, and a new concept for diabetes complications—mitochondrial hormesis—is presented. In this view, production of mitochondrial superoxide can be an indicator of healthy mitochondria and physiologic oxidative phosphorylation. Recent data suggest that in response to excess glucose exposure or nutrient stress, there is a reduction of mitochondrial superoxide, oxidative phosphorylation, and mitochondrial ATP generation in several target tissues of diabetes complications. Persistent reduction of mitochondrial oxidative phosphorylation complex activity is associated with the release of oxidants from nonmitochondrial sources and release of proinflammatory and profibrotic cytokines, and a manifestation of organ dysfunction. Restoration of mitochondrial function and superoxide production via activation of AMPK has now been associated with improvement in markers of renal, cardiovascular, and neuronal dysfunction with diabetes. With this Perspective, approaches that stimulate AMPK and PGC1α via exercise, caloric restriction, and medications result in stimulation of mitochondrial oxidative phosphorylation activity, restore physiologic mitochondrial superoxide production, and promote organ healing.
Introduction
Diabetes is expected to grow two- to fivefold in many countries, including the U.S., China, and India, in the next 20 years (1). The diagnosis of diabetes itself modestly increases the risk of mortality; however, the renal complications of diabetes may be major drivers of the increased cardiovascular morbidity and mortality associated with diabetes (2). Diabetes is a leading cause of renal failure, blindness, heart disease, and limb amputations in adults (http://diabetes.niddk.nih.gov/statistics/index.aspx) (3–5). With the increasing prevalence of diabetes, the overall burden attributed to end-stage renal disease with diabetes has dramatically increased, and reports of increasing incidence of type 2 diabetes in adolescents will result in a further overall increase in diabetes complications and kidney disease (6).
To combat the complications of diabetes, several large trials in the past 5 years have targeted the commonly accepted risk factors, including hyperglycemia, hypertension, and hyperlipidemia. Unfortunately, none of these trials have successfully reduced the primary end point of cardiovascular morbidity and mortality (7,8). It is therefore clear that novel approaches are urgently needed.
The developments of new treatments have largely been guided by the concept that oxidative stress, primarily driven by mitochondrial superoxide, underlies diabetes complications (9,10). An enhanced mitochondrial source of superoxide as a driving force for diabetes complications has been considered as a unifying theory and widely accepted, despite inconclusive support from clinical trials. Recent meta-analyses of randomized clinical trials failed to show benefit of several antioxidants in cardiovascular disease outcomes (11). Of note, a recent phase III study targeting diabetic nephropathy with a potent oral antioxidant, bardoxolone methyl, led to an increase in hypertension, albuminuria, and heart failure in patients with advanced diabetic nephropathy (12).
In the present review, supportive evidence and opposing ideas to the theory of excess mitochondrial superoxide will be discussed. A concept termed “mitochondrial hormesis” will be presented as a new way to understand diabetes complications, primarily diabetic kidney disease, and possibly nerve and cardiac complications of diabetes. Mitochondrial hormesis is consistent with the concept that improved mitochondrial function is associated with “normal” or a slightly increased production of superoxide and suggests a new path forward to reduce organ dysfunction with diabetes.
Are Reactive Oxygen Species Major Contributors to Organ Dysfunction in Aging?
The idea that reactive oxygen species (ROS) contribute to chronic organ damage was attributed to Harman (13) in 1956 and was termed the free radical theory of aging (FRTA). The FRTA was initially based on the recognition that external radiation can be attributed to free radical production and that cell survival can be improved with antioxidants (13). With the discovery of superoxide dismutases (SODs) and the recognition that mitochondria produces hydrogen peroxide (H2O2), the initial FRTA was modified in 1972 to include the role of mitochondrial oxidant production as a source of free radical production that led to a decline in life span (14). In 1980, Miquel et al. (15) formally proposed the mitochondrial theory of aging by arguing that oxygen radicals produced by mitochondria during respiration can exceed the cellular antioxidant defenses. A central tenet of the theory was that the mitochondrial respiratory chain generates superoxide production, which is converted to H2O2 spontaneously or via SOD2. As determined from the amount of mitochondrial H2O2, mitochondrial ROS generation has been estimated to account for between 0.1 and 0.4% of the oxygen consumed by normally functioning mitochondria (16). The respiratory complexes, including flavoproteins, iron-sulfur clusters, and ubisemiquinone, are the major sources of ROS production in mitochondria (17). The subsequent oxidation-derived modifications of DNA, lipids, and proteins were considered to contribute to the aging process (16).
However, the FRTA was met with skepticism during Harman’s time, and irrefutable evidence to support the theory is still lacking. An important approach to test the FRTA is the manipulation of SOD2. Complete deletion of SOD2 reduced the life span of Drosophila and increased neonatal mortality in mice (18,19). However, deletion of SOD2 has also been reported to increase autophagy in mouse embryonic fibroblasts (20), which is in contrast to the finding that aging is associated with a reduction in autophagy and an increase in mammalian target of rapamycin (mTOR) (21).
A more useful model may be the SOD2+/− mice because SOD2 activity is reduced by 50% in all tissues and the mice live to adulthood with clear evidence of increased oxidative damage to nuclear and mitochondrial DNA (mtDNA) (22). Surprisingly, the SOD2+/− mice had no reduction in life span, even with telomere deficiency (23). Furthermore, overexpression of SOD2 did not increase life span (24). The deleterious role of mitochondrial ROS production as a cause of reduced life span has been challenged by findings in Heterocephalus glaber, the naked mole rat. This rat lives to a maximal life span of 28 years, yet has a low level of glutathione peroxidase and a high level of mtROS production (25). The naked mole rat also has high rates of DNA, lipid, and protein oxidative damage (26).
Recent studies have now provided compelling evidence against the view that mtROS production contributes to aging. Exposure of Caenorhabditis elegans to 2-deoxyglucose (DOG), an inhibitor of glycolysis, increased mtROS and increased life span (27). Further, coadministration of N-acetylcysteine with 2-DOG reduced ROS production and blocked the benefit in life span extension (27). Network analysis of the transcriptomic changes with 2-DOG indicated that the mTOR pathway may play a key role (28). Furthermore, stimulation of mitochondrial superoxide with menadione also enhanced life span, whereas overexpression of SOD2 reduced life span in yeast (29). These studies indicate, at least in worms and yeast, that increased mtROS is associated with an increased life span. Thus, debate continues whether mtROS production is indeed a driving force contributing to aging.
Excess Mitochondrial Superoxide As a Unifying Theory Underlying Diabetes Complications
Mitochondria, NADPH oxidases, nitric oxide synthase (NOS), lipoxygenases, and xanthine oxidase are major sources of endogenous ROS (30). During normal respiration, electrons are transferred through a series of oxidative-reductive reactions using proteins as carriers for the electrons. According to the theory of excess mtROS production in diabetes, excess glucose uptake by susceptible cells would lead to an increase in pyruvate entry into the mitochondria and an increased flux of substrates (NADH and reduced flavin adenine dinucleotide [FADH2]) to the electron transport chain (ETC) (9,31), resulting in hyperpolarization of the mitochondrial membrane and accumulation of electrons at complex III and coenzyme Q, which donate electrons to molecular oxygen and generate superoxide anions (31). The implication that diabetes complications would directly result from ETC activity was straightforward and was consistent with the mitochondrial FRTA. Thus, the landmark publications indicating that mitochondrial production of superoxide was a unifying mechanism to regulate the major pathways of diabetes complications (polyol flux, protein kinase C, advanced glycosylation end product, hexosamine flux) were widely accepted (9,10,31).
On the basis of the theory of excess mitochondria superoxide production and from initial studies in cultured aortic endothelial cells exposed to high glucose (9), it would be expected that there would be 1) an increase in ETC activity, 2) hyperpolarization of the mitochondrial membrane gradient, 3) an increase in mitochondrial superoxide anion production, and 4) an increase in downstream markers of ROS activity with exposure to high glucose. Conclusion 4 is supported by convincing data indicating an increase in oxidative damage to DNA and proteins in cells and tissues exposed to high glucose. Markers such as 8-hydroxy-2-deoxyguanosine, 2-isoprostane, nitrotyrosine, and thiobarbituric acid reactive substances have been increased in numerous studies with experimental models of diabetes and in patients (32,33). Therefore, the footprints of oxidative stress support the concept that oxidant stress is indeed present in organs subject to inflammation and fibrosis, including kidneys, heart, and neuronal tissues. However, data regarding stimulation of ETC activity, hyperpolarization of the mitochondrial membrane gradient, and increased mitochondrial production of superoxide anion are less conclusive.
In rats with type 1 diabetes, mitochondrial ETC activity and mitochondrial superoxide are reduced in the dorsal root ganglion (DRG) (34). Mitochondrial superoxide, measured by fluorescent indicators and electron paramagnetic resonance, was not increased in the diabetic heart (35). A similar pattern was found in the OVE26 diabetic mouse (36). In support of the mitochondrial theory of excess superoxide production, hyperpolarization of the mitochondrial membrane potential and an increased ROS signal was reported from in vitro studies of peripheral mononuclear cells and arterioles from patients with diabetes (37). However, other studies have reported impaired hyperpolarization of the mitochondrial membrane potential in human islet tissue (38) or a depolarization of the mitochondrial membrane potential in sensory neurons from diabetic rats (34). A recent report found both reduced mitochondrial membrane potential and a reduction of the respiratory control ratio in diabetic sensory neurons (39).
On the basis of the ETC-induced superoxide theory, it would be expected that uncoupling proteins (UCPs) would be beneficial to reduce the membrane gradient and reduce generation of superoxide. UCP1 is the prototypical UCP but is primarily present in brown adipose tissue and has low basal expression in kidney, neurons, and heart. UCP2 and UCP3 are homologous proteins and may have similar functions to reduce superoxide production. Some have argued that an increase of UCPs may be a compensatory response to hyperpolarization of the mitochondrial membrane. However, a recent study with small interfering RNA to reduce UCP2 in the diabetic kidney did not lead to worsening of kidney function, and reducing UCP2 improved podocyte function (40,41). A benefit of inhibiting UCP2 may be via activation of the adenine nucleotide transporter in the mitochondria to reduce the mitochondrial membrane potential (41); however, this hypothesis remains to be proven. Reduction of UCP2 has also been shown to improve insulin sensitivity and preserve islet cell insulin production (42).
The measurement of superoxide directly would clarify whether there is increased mitochondrial superoxide production in response to high glucose levels. However, this is difficult to accomplish because superoxide has an extremely short half-life. Indeed, the initial studies reporting an increase in mitochondrial superoxide production measured H2O2 in endothelial cells cultured in high glucose (9). Although inhibitors of ETC reduced H2O2 production and prevented stimulation of several pathways (protein kinase C, advanced glycosylation end product, hexosamine), whether the beneficial effects are due to the reduction in mitochondrial superoxide production and whether the data are relevant to the in vivo condition remains unclear. Using an in vivo measurement of superoxide (see below), we found a reduction of superoxide in the streptozotocin (STZ)-induced and Akita-induced diabetic mouse kidney, heart, and liver (43). Additionally, stimulation of mitochondrial function was recently found to be renoprotective (44).
Studies to support the concept of excess mitochondrial superoxide production have used genetic approaches to over express or inhibit SOD2. Indeed, upregulation of SOD2 or UCP1 reduced glucose-induced nuclear factor-κB and epigenetic effects in bovine aortic endothelial cells (45), and a separate study reported that excess expression of SOD2 reduced diabetic kidney and heart diseases (46). However, the SOD2 transgene led to an increase not only in mitochondrial SOD2 but also in cytosolic expression of SOD2 (46). Thus, the benefit seen with transgenic SOD2 may not primarily be at the mitochondrial level but may be due to the reduction of cytosolic superoxide. Another approach would be to reduce SOD2. Surprisingly, the heterozygous SOD2-deficient mouse had no evidence of worsening diabetic kidney disease (43).
The roles of other SODs have also been examined. A model of progressive diabetic kidney disease found a reduction of renal SOD1 and SOD3, but not SOD2 (47). Deficiency of the intracellular SOD1 was found to exacerbate diabetic kidney disease in models of STZ (48) and Akita type 1 diabetes (49). Interestingly, deficiency of the extracellular SOD3 was not associated with enhanced diabetes complications. It remains possible that deficiency of SOD1 may have cross talk with SOD2 or that SOD1 may directly regulate mitochondrial superoxide because low levels of SOD1 are present in the inner mitochondrial membrane (50). Thus, it appears from these publications that increased cytosolic superoxide and other ROS moieties may play a more prominent role than mitochondrial superoxide in contributing to diabetic kidney disease.
Compounds such as mitoQ10, mitoTEMPOL, and mitoE use the cation triphenylphosphonium (TPP+) linked to Q10, TEMPOL, or vitamin E to enhance mitochondrial uptake and have been used to determine if mitochondrial superoxide production contributes to pathological outcomes (51). Several studies indicate that these compounds provide benefit with respect to reduced inflammation and fibrosis markers in kidney, heart, and vascular cells (51). However, a recent report identified that the linker compound TPP+ by itself has mitochondrial toxicity independent of an antioxidant effect (52). In addition, the concentrations used to enhance mitochondrial uptake are 10- to 100×-fold excess of what is commonly used with in vivo administration. Thus, the effects of mitoQ10, mitoTEMPOL, and mitoE in vivo may be due to an antioxidant effect outside the mitochondria rather than to mitochondrial-specific antioxidant effects (52).
Nonmitochondrial sources of high glucose–induced cytosolic ROS include the isoforms of NADPH oxidase (Nox) and uncoupled endothelial NOS (eNOS) (53,54). Several studies using nonspecific inhibitors of Nox (55) or more specific inhibitors of Nox1 and Nox4 have found beneficial effects in protecting against diabetic kidney and vascular disease (56). The Nox2-deficient mouse does not appear to contribute to diabetic kidney disease (57); however, there are convincing data to support a role for Nox4 in diabetic kidney disease (58). Nox isoforms may also play a critical role in regulating insulin resistance and inflammation (59). Interestingly, Nox4 may also be localized to mitochondria and may primarily produce H2O2 (60). The role of H2O2 as a source of oxidant stress in diabetes and its complications is supported by studies demonstrating a protective benefit of overproduction of cytosolic or mitochondrial catalase (61,62). In future studies, the timing of mitochondrial ROS generation with intracellular spatial differentiation of specific ROS species in different tissues and models of diabetes will be necessary to clarify the time course and role of mitochondrial dysfunction as a producer or target of ROS.
Therapeutic Implications of Reducing Mitochondrial Superoxide Anion Production
The causal role of mitochondrial superoxide production for human diabetes complications will ultimately require well-designed randomized phase III clinical trials with interventions that specifically target mitochondrial superoxide anion production. To date, studies with antioxidants, such as vitamin E, β-carotene, and vitamin A, have not demonstrated a clear benefit to reduce diabetic cardiovascular complications (11,63). MitoQ10 has been shown to provide beneficial effects in hypertension (51); however, mitoQ10 may work either as a pro- or antioxidant in intact cells (64) and may regulate mitochondrial calcium levels independently of its antioxidant activity (65).
Recently, there was much excitement regarding the nuclear regulatory factor 2 (Nrf2) activator, bardoxolone (66). Because Nrf2 is a potent stimulator of oxidant scavenging systems (SOD, glutathione peroxidase, catalase), the phase II data indicating bardoxolone may improve renal function lent credence to the oxidant stress hypothesis for diabetes complications (66). However, the phase III study was prematurely stopped due to congestive heart failure and excess mortality (12). Renal parameters were inconclusive because the patients receiving the active drug showed a decrease in serum creatinine but an increase in albuminuria and blood pressure. Therefore, a reasonable conclusion from the available clinical data is that a beneficial role of nonspecific antioxidants for diabetes complications has not been established and that the role of mitochondrial superoxide as the driving force of diabetes complications should be reevaluated.
New Evidence to Provide Novel Perspectives on ROS and Diabetes Complications
Is there an alternative view regarding mitochondrial superoxide production that is consistent with recent data regarding mitochondrial function in animal models of diabetes complications? New insights could be achieved with measures of superoxide production in real time and in vivo. Such an approach has recently been reported (67). Dihydroethidium (DHE), or hydroethidine, is able to react with superoxide anion specifically and show discrete differences in its excitation wavelength when exposed to superoxide anion but not when exposed to H2O2 or peroxynitrite (68). DHE enters cells rapidly and can irreversibly bind superoxide anion and remain stable as the oxidized moiety. An important caveat is that ex vivo interpretation of DHE is fraught with difficulty, primarily due to rapid autooxidation in ambient oxygen. However, when DHE is prepared under low oxygen conditions and quickly given in vivo, the lower internal oxygen milieu allows DHE to enter cells in the nonoxidized state (67). The major oxidation products of DHE are likely ethidium or 2-hydroxyethidium. In vitro studies have shown 2-hydroxyethidium is the major oxidation product (69); however, the predominant oxidation product in vivo appears to be ethidium, as demonstrated by fluorescence lifetime measurements (67). The specificity of DHE to measure superoxide production in vivo was demonstrated as the DHE oxidation product was increased in the tissues of the SOD2-deficient mice and reduced with SOD mimetics (67).
We recently adapted the in vivo DHE method to study basal superoxide production in various organs under control conditions and with type 1 diabetes (43). Surprisingly, the results showed the opposite of the predicted theory. There was a high basal level of superoxide production in the normal mouse kidney, heart, and liver and a reduction in all three organs with diabetes (43). This was found with STZ-induced diabetes as well as in the Akita diabetic mouse (43). Because the in vivo oxidation product of DHE remains controversial, a similar reduction was also observed in isolated mitochondria from diabetic kidney in measurements using two different approaches: superoxide measurements using electron paramagnetic resonance and H2O2 measurements using Amplex Red (43). Thus, multiple in vivo and ex vivo approaches did not show evidence of enhanced mitochondrial superoxide production in the diabetic kidney.
Studies in the SOD2+/− mouse demonstrated a high level of renal DHE fluorescence with SOD2 deficiency, indicating increased superoxide production. However, the increased superoxide production was not associated with increased renal disease under basal conditions or with diabetes (44). A study evaluating diabetic neuropathy did not find evidence of enhanced neuropathy in the SOD2+/− mouse with type 1 diabetes, although there was an increase in a type 2 model (70).
The surprising result of reduced superoxide production in the diabetic kidney led us to evaluate the function of pyruvate dehydrogenase (PDH) complex and mitochondrial ETC activity with diabetes. PDH phosphorylation is known to inhibit pyruvate uptake into mitochondria, and increased PDH phosphorylation was found in the diabetic kidney (43). Similar results have been reported in diabetic heart tissue (71). Activity of complexes I, III, and IV was reduced in the diabetic kidney (43). Reduced ETC activity was also found in skeletal muscle of patients with type 2 diabetes (72) and in an animal model of diabetic cardiomyopathy (73). As noted above, diabetic DRG was recently found to have reduced mtROS generation and reduced ETC activity (34), and studies in Schwann cells have demonstrated alterations in mitochondrial respiration with high glucose but no change in superoxide production (74).
In addition to reduced superoxide production, we found an overall reduction of renal mitochondrial content and PGC1α (43). PGC1α is a transcriptional coactivator that drives the nuclear transcription of several genes involved in mitochondrial biogenesis, including Nrfs 1 and 2, peroxisome proliferator–activated receptors, estrogen-related receptors, mitochondrial protein ATP synthetase (β-subunit), and COX (cytochrome c oxidase) subunits (COX II and COX IV) (75). PGC1α-induced stimulation of Nrf1 and Nrf2 promotes the expression of mitochondrial transcription factor A, which drives transcription and replication of mtDNA (75). Thus, there is evidence not only of reduced mitochondrial function with diabetes but also that overall mitochondrial content and biogenesis are reduced in the diabetic kidney. We also recently found evidence of reduced mitochondrial content, function, and PGC1α mRNA levels in human diabetic kidney disease (76). Importantly, several studies have found a reduction in PGC1α and reduced mitochondrial biogenesis in islets and human skeletal muscle in patients with diabetes (77,78). Mitochondrial content and PGC1α were also reduced in DRG of STZ-induced type 1 diabetes, and features of neuropathy were exacerbated in PGC1α-deficient diabetic mice (79). A similar reduction in mitochondrial function, content, and PGC1α was also found in the DRG of db/db mice (80).
Whether the reduction in mitochondrial function and content was contributing to diabetes-induced organ dysfunction was addressed by stimulating mitochondrial biogenesis by activating the master energy sensor AMPK. This heterotrimeric enzyme is phosphorylated on its catalytic subunit, α1 (81), and activated in response to reduced energy supply. Activation of AMPK reduces protein synthesis, enhances glucose uptake, and stimulates mitochondrial biogenesis via stimulation of PGC1α. Reduction of AMPK activation would be expected in caloric excess states, such as diabetes and high-fat feeding, and such a reduction has been found in the kidney with type 1 diabetes (43) and with a high-fat diet (82,83). Stimulation of AMPK activation led to an increase in PDH and ETC activity, PGC1α, mitochondrial content, and stimulation of superoxide production in the diabetic kidney. Importantly, with increased mitochondrial function and superoxide production, there was an associated improvement in albuminuria, urine H2O2, mesangial matrix expansion, and a reduction of profibrotic factors (i.e., transforming growth factor-β). Similar benefits with AMPK activators, including resveratrol, have been demonstrated in different animal models of diabetic kidney disease (43,84,85). Studies in the STZ-diabetic rat model and the db/db mouse have also demonstrated a similar pattern of reduced AMPK activity in diabetic DRG neurons and improvement of mitochondrial function with AMPK agonists (86). Thus stimulation of mitochondrial function and superoxide production is associated with an improvement in diabetic kidney and nerve disease.
Several relevant studies have been reported with the diabetic retina and heart. A prior study found no increase in the tricarboxylic acid cycle (TCA) cycle or NADH production in the diabetic retina, and exposure to high glucose led to an increase in glycolytic flux but not TCA cycle activity (87). In the normal heart, there is a balance between fatty acid and glucose oxidation; however, in the diabetic heart, there is reduced glucose oxidation and a relative increase in fatty acid oxidation (88). AMPK activation (with metformin) has been found to benefit heart function in a model of diabetic cardiomyopathy in the OVE26 mouse model (89), and berberine, another AMPK activator, reduced myocardial ischemic-reperfusion injury in diabetic rats (90). Furthermore, mitochondrial biogenesis and AMPK activity were reduced in the diabetic ob/ob heart, and adiponectin treatment stimulated AMPK, PGC1α, and mitochondrial biogenesis with associated reduced susceptibility to myocardial injury after infarction (91). Excess mitochondrial biogenesis may not always be beneficial, however, because overexpression of PGC1α in muscle did not uniformly protect against the development of insulin resistance (92), and overexpression of PGC1α in endothelial cells resulted in aberrant reendothelialization and blunted wound healing (93).
New Theory of Mitochondrial Hormesis As a Central Player in Diabetes Complications
The concept that increased production of mitochondrial superoxide can be beneficial has been termed mitochondrial hormesis. Mitochondrial hormesis was initially used to describe the beneficial acute increase in mitochondrial respiration when cells are exposed to toxins such as heavy metals (94). A beneficial role of mitochondrial superoxide may be linked to improved endothelial function because 2-DOG was found to stimulate AMPK and phosphorylate eNOS via stimulation of ROS (95). Exercise has been shown to stimulate muscle ROS production, and a study in humans found that exercise increased adiponectin levels and insulin sensitivity; however, pretreatment with antioxidants (vitamin C and vitamin E) led to a loss of the protective benefits of exercise (96).
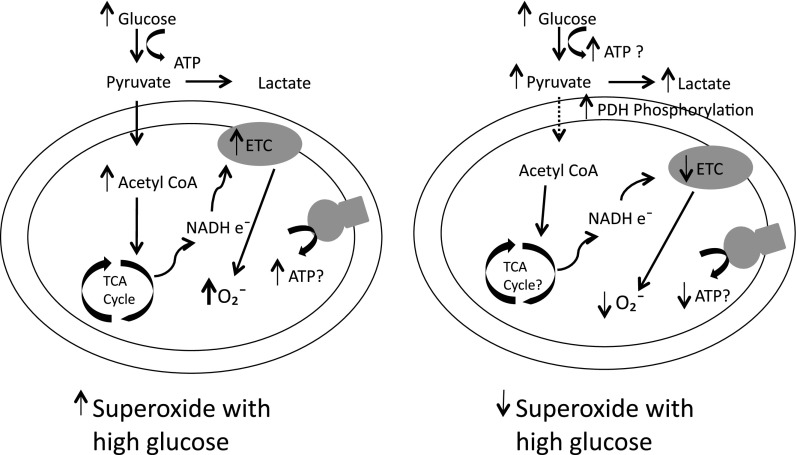
In the context of a chronic insult, such as hyperglycemia, mitochondrial hormesis places the finding of reduced mitochondrial superoxide in target organs of diabetes in a new context (Fig. 1). A well-functioning mitochondria would have robust ETC activity while generating physiologic levels of superoxide. Under normal conditions, the mammalian organism is intermittently exposed to low or normal levels of blood glucose necessitating efficient use of glucose to generate sufficient ATP production to meet the demands of differentiated cells. However, when presented with an excess of glucose, there would not be any evolutionary benefit to produce excess ATP and the excess production of ATP may even be harmful. Therefore, inhibition of mitochondrial ETC activity and ATP production in response to excess glucose would be physiologically inappropriate. The reduced ETC activity would consequently have less mitochondrial superoxide generation. Although, reduced mitochondrial ETC activity would be adaptive in the short-term, the state of diabetes is unusual in evolutionary terms, and a persistent reduction of mitochondrial function and suppression of biogenesis could ultimately be detrimental to differentiated organ function and be linked with inflammation. Viewed in this light, the concept of mitochondrial hormesis is highly intuitive. Approaches to restore mitochondrial balance and stimulate ETC activity will be associated with increased mitochondrial superoxide production to “normal levels” and allow the cell to restore its normal differentiated function and promote organ healing.
Figure 1.
New evidence-based hypothesis implicating reduced superoxides in diabetes complications. The conventional wisdom views that with excess intracellular glucose exposure there is a consequent increase in pyruvate-mediated stimulation of the TCA cycle leading to increased production of electron donors to drive the ETC and generate superoxide. However, based on new in vivo data from the diabetic kidney and nerve, a counterview suggests that excess intracellular glucose enhances PDH phosphorylation to block pyruvate uptake into mitochondria, which results in reduced activity of the ETC and limits mitochondrial ATP production. The reduced ETC activity will result in less superoxide production—rather than more—in diabetic organs in vivo. Increased glycolytic flux may also be a feature in target organs of diabetes complications.
Therapeutic Strategies
Diabetes complications, including kidney disease, are the most important concerns once a patient is diagnosed with diabetes. Along with existing approaches to improve glycemic levels and reduce blood pressure and cholesterol levels, additional benefits may arise from approaches to restore mitochondrial function, oxidative phosphorylation activity, and possibly, increase mitochondrial superoxide production. Restoring mitochondrial function could be attained by caloric reduction (episodic fasting) and exercise, which have been shown to increase life span and reduce organ inflammation and fibrosis (97). Exercise regimens can improve kidney histology and lower albuminuria in the absence of weight loss and improvement in blood glucose in mice (98), and a lifestyle change with exercise has been consistently shown to be of benefit across a variety of human chronic diseases (99). One plausible mechanism, among others, is the stimulation of mitochondrial biogenesis and mitochondrial activity with exercise. As noted, muscle has a beneficial increase in oxidant production with exercise (96). However, in the Look AHEAD (Action for Health in Diabetes) trial, patients with diabetes who underwent weight reduction and increased exercise had improvements in glycemic control and less dependence on medications to lower cholesterol but did not have a significant reduction in cardiovascular events (100).
Caloric restriction and exercise confer their protective effects, at least in part, via stimulation of AMPK. AMPK reduction has now been found in several models of diabetic kidney disease in mice (43,84), rats (101), and recently, in human diabetic nephropathy (43). AMPK reduction has also been found in the heart, nerve, and retina of animal models with diabetes (86,91,102–104). A potential endogenous ligand to stimulate AMPK is adiponectin. Adiponectin has consistently been found to be reduced in patients with obesity, insulin resistance, and low-grade albuminuria (105). In mice, a high-fat diet leads to an initial reduction of adiponectin (within 1 week), but chronic high-fat feeding is associated with restored adiponectin levels despite a persistent reduction in AMPK activity in the kidney (82). Interestingly, drugs that have proven clinical benefit for diabetes and its complications have been found to stimulate AMPK. These include metformin (106), angiotensin II receptor blockers (107), and aspirin (108). Other newer drugs have potent AMPK activity and may also be beneficial for diabetes complications (109).
Pathways that may be downstream of AMPK and also regulate mitochondrial biogenesis are the sirtuins and mTOR inhibitors. Sirt1 and Sirt3 are NAD(+)-dependent deacetylases that have been shown to contribute to the benefit of caloric restriction with aging and angiotensin II inhibition (110). Sirt1 activation can reduce inflammation and fibrosis, and its benefits have been attributed to reducing H2O2-induced p53 acetylation (111). Sirt1 has potent deacetylase activity on PGC1α (112) and may contribute to mitochondrial biogenesis and restoration of mitochondrial function (113). Of possible interest in this regard are certain small peptides that prevent a fall in renal PGC1α and improve mitochondrial and renal function and structure under conditions of renal injury (114). Stimulation of mitochondrial biogenesis via upregulation of tubular PGC1α has a protective effect and reduces renal fibrosis in response to nephrotoxins (44). An increase in mTOR is a consistent finding in diabetic glomerular complications, and inhibition of mTOR leads to beneficial responses, possibly by stimulating mitochondrial biogenesis (115). Interestingly, a recent study found that Nox4 stimulates mTOR and inhibition of Nox4-mTOR activity may underlie its beneficial effect (116). Resveratrol has been found to reduce diabetes complications in db/db mice (85,117), likely via stimulation of AMPK, Sirt, and PGC1α. Improving mitochondrial biogenesis and function may not necessarily imply that mitochondrial ETC activity and mitochondrial superoxide production will be increased; however, it is reassuring that in states where mitochondrial biogenesis has been associated with a physiologic increase in mitochondrial ROS production (25,26,28,29,34,43,96,98), there do not appear to be any negative consequences.
Concluding Remarks
With the continued rise in diabetes and diabetes complications, a critical review of our accepted theoretical dogmas are required to develop new breakthroughs. Excess production of mitochondrial superoxide as a unifying theory to underlie diabetic renal complications has been widely accepted but should be questioned as new data that are in conflict with many of the fundamental tenets for this concept continue to emerge. A contrasting view that incorporates mitochondrial hormesis is supported by recent data linking reduction of AMPK, sirtuins, and PGC1α pathways and increased mTOR with reduced mitochondrial ROS, biogenesis, and progression of disease. Stimulation of mitochondrial biogenesis and physiological mitochondrial superoxide production via pharmacologic and lifestyle changes suggests numerous therapeutic choices that may be pursued in future studies. The reduction of mitochondrial superoxide may contribute to deleterious pathways, such as chronically reduced AMPK and eNOS activity, or may be solely an indicator of reduced mitochondrial ETC activity. Thus far, a beneficial role of mitochondrial superoxide production has not yet been established in diabetes complications. However, this new concept should also be questioned and critically assessed with existing and new tools. Novel methods of measuring specific ROS moieties and mitochondrial function in intact cells and tissues will give new insights relevant to understanding mitochondrial function in their intact cytoarchitectural configuration. New methods to image real-time longitudinal measurements of key aspects of mitochondrial and cellular function in relevant animal models and in the human condition, coupled with omics analysis, are expected to provide some fundamental truths regarding diabetes and its complications.
Article Information
Acknowledgments. Critical review of the manuscript was provided by Peter Oates (Oates Biomedical Consulting). Manjula Darshi (Center for Renal Translational Medicine, University of California, San Diego) provided editorial assistance in preparation of the manuscript.
Funding. Support for the studies reported here was provided by funding from JDRF and the National Institutes of Health (DP3-DK-094352).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Prior Presentation. Parts of this work were presented as an oral presentation at the 74th Scientific Sessions of the American Diabetes Association, San Francisco, CA, 13–17 June 2014, and at the American Society of Nephrology Kidney Week 2014, Philadelphia, PA, 11–16 November 2014.
References
- 1.Alberti KG, Zimmet P. Global burden of disease—where does diabetes mellitus fit in? Nat Rev Endocrinol 2013;9:258–260 [DOI] [PubMed] [Google Scholar]
- 2.Afkarian M, Sachs MC, Kestenbaum B, et al. Kidney disease and increased mortality risk in type 2 diabetes. J Am Soc Nephrol 2013;24:302–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Antonetti DA, Klein R, Gardner TW. Diabetic retinopathy. N Engl J Med 2012;366:1227–1239 [DOI] [PubMed] [Google Scholar]
- 4.Ahola AJ, Saraheimo M, Forsblom C, Hietala K, Sintonen H, Groop PH; FinnDiane Study Group . Health-related quality of life in patients with type 1 diabetes—association with diabetic complications (the FinnDiane Study). Nephrol Dial Transplant 2010;25:1903–1908 [DOI] [PubMed] [Google Scholar]
- 5.Martin CL, Albers J, Herman WH, et al.; DCCT/EDIC Research Group . Neuropathy among the diabetes control and complications trial cohort 8 years after trial completion. Diabetes Care 2006;29:340–344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gregg EW, Li Y, Wang J, et al. Changes in diabetes-related complications in the United States, 1990-2010. N Engl J Med 2014;370:1514–1523 [DOI] [PubMed] [Google Scholar]
- 7.Patel A, MacMahon S, Chalmers J, et al.; ADVANCE Collaborative Group . Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–2572 [DOI] [PubMed] [Google Scholar]
- 8.Fried LF, Emanuele N, Zhang JH, et al.; VA NEPHRON-D Investigators . Combined angiotensin inhibition for the treatment of diabetic nephropathy. N Engl J Med 2013;369:1892–1903 [DOI] [PubMed] [Google Scholar]
- 9.Nishikawa T, Edelstein D, Du XL, et al. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature 2000;404:787–790 [DOI] [PubMed] [Google Scholar]
- 10.Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes 2005;54:1615–1625 [DOI] [PubMed] [Google Scholar]
- 11.Myung SK, Ju W, Cho B, et al.; Korean Meta-Analysis Study Group . Efficacy of vitamin and antioxidant supplements in prevention of cardiovascular disease: systematic review and meta-analysis of randomised controlled trials. BMJ 2013;346:f10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Zeeuw D, Akizawa T, Audhya P, et al.; BEACON Trial Investigators . Bardoxolone methyl in type 2 diabetes and stage 4 chronic kidney disease. N Engl J Med 2013;369:2492–2503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harman D. Aging: a theory based on free radical and radiation chemistry. J Gerontol 1956;11:298–300 [DOI] [PubMed] [Google Scholar]
- 14.Harman D. The biologic clock: the mitochondria? J Am Geriatr Soc 1972;20:145–147 [DOI] [PubMed] [Google Scholar]
- 15.Miquel J, Economos AC, Fleming J, Johnson JE Jr. Mitochondrial role in cell aging. Exp Gerontol 1980;15:575–591 [DOI] [PubMed] [Google Scholar]
- 16.Sanz A, Stefanatos RK. The mitochondrial free radical theory of aging: a critical view. Curr Aging Sci 2008;1:10–21 [DOI] [PubMed] [Google Scholar]
- 17.Turrens JF. Mitochondrial formation of reactive oxygen species. J Physiol 2003;552:335–344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kirby K, Hu J, Hilliker AJ, Phillips JP. RNA interference-mediated silencing of Sod2 in Drosophila leads to early adult-onset mortality and elevated endogenous oxidative stress. Proc Natl Acad Sci U S A 2002;99:16162–16167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mukherjee S, Forde R, Belton A, Duttaroy A. SOD2, the principal scavenger of mitochondrial superoxide, is dispensable for embryogenesis and imaginal tissue development but essential for adult survival. Fly (Austin) 2011;5:39–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang Y, Zhang HM, Shi Y, et al. Loss of manganese superoxide dismutase leads to abnormal growth and signal transduction in mouse embryonic fibroblasts. Free Radic Biol Med 2010;49:1255–1262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lamming DW, Ye L, Sabatini DM, Baur JA. Rapalogs and mTOR inhibitors as anti-aging therapeutics. J Clin Invest 2013;123:980–989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van Remmen H, Ikeno Y, Hamilton M, et al. Life-long reduction in MnSOD activity results in increased DNA damage and higher incidence of cancer but does not accelerate aging. Physiol Genomics 2003;16:29–37 [DOI] [PubMed] [Google Scholar]
- 23.Guachalla LM, Ju Z, Koziel R, et al. Sod2 haploinsufficiency does not accelerate aging of telomere dysfunctional mice. Aging (Albany, NY Online) 2009;1:303–315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jang YC, Pérez VI, Song W, et al. Overexpression of Mn superoxide dismutase does not increase life span in mice. J Gerontol A Biol Sci Med Sci 2009;64:1114–1125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andziak B, O’Connor TP, Buffenstein R. Antioxidants do not explain the disparate longevity between mice and the longest-living rodent, the naked mole-rat. Mech Ageing Dev 2005;126:1206–1212 [DOI] [PubMed] [Google Scholar]
- 26.Andziak B, O’Connor TP, Qi W, et al. High oxidative damage levels in the longest-living rodent, the naked mole-rat. Aging Cell 2006;5:463–471 [DOI] [PubMed] [Google Scholar]
- 27.Schulz TJ, Zarse K, Voigt A, Urban N, Birringer M, Ristow M. Glucose restriction extends Caenorhabditis elegans life span by inducing mitochondrial respiration and increasing oxidative stress. Cell Metab 2007;6:280–293 [DOI] [PubMed] [Google Scholar]
- 28.Priebe S, Menzel U, Zarse K, et al. Extension of life span by impaired glucose metabolism in Caenorhabditis elegans is accompanied by structural rearrangements of the transcriptomic network. PLoS ONE 2013;8:e77776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pan Y, Schroeder EA, Ocampo A, Barrientos A, Shadel GS. Regulation of yeast chronological life span by TORC1 via adaptive mitochondrial ROS signaling. Cell Metab 2011;13:668–678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Finkel T, Holbrook NJ. Oxidants, oxidative stress and the biology of ageing. Nature 2000;408:239–247 [DOI] [PubMed] [Google Scholar]
- 31.Giacco F, Brownlee M. Oxidative stress and diabetic complications. Circ Res 2010;107:1058–1070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Broedbaek K, Weimann A, Stovgaard ES, Poulsen HE. Urinary 8-oxo-7,8-dihydro-2′-deoxyguanosine as a biomarker in type 2 diabetes. Free Radic Biol Med 2011;51:1473–1479 [DOI] [PubMed] [Google Scholar]
- 33.Williams KJ, Qiu G, Usui HK, et al. Decorin deficiency enhances progressive nephropathy in diabetic mice. Am J Pathol 2007;171:1441–1450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Akude E, Zherebitskaya E, Chowdhury SK, Smith DR, Dobrowsky RT, Fernyhough P. Diminished superoxide generation is associated with respiratory chain dysfunction and changes in the mitochondrial proteome of sensory neurons from diabetic rats. Diabetes 2011;60:288–297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Herlein JA, Fink BD, O’Malley Y, Sivitz WI. Superoxide and respiratory coupling in mitochondria of insulin-deficient diabetic rats. Endocrinology 2009;150:46–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bugger H, Boudina S, Hu XX, et al. Type 1 diabetic Akita mouse hearts are insulin sensitive but manifest structurally abnormal mitochondria that remain coupled despite increased uncoupling protein 3. Diabetes 2008;57:2924–2932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Widlansky ME, Wang J, Shenouda SM, et al. Altered mitochondrial membrane potential, mass, and morphology in the mononuclear cells of humans with type 2 diabetes. Transl Res 2010;156:15–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Anello M, Lupi R, Spampinato D, et al. Functional and morphological alterations of mitochondria in pancreatic beta cells from type 2 diabetic patients. Diabetologia 2005;48:282–289 [DOI] [PubMed] [Google Scholar]
- 39.Chowdhury SR, Saleh A, Akude E, et al. Ciliary neurotrophic factor reverses aberrant mitochondrial bioenergetics through the JAK/STAT pathway in cultured sensory neurons derived from streptozotocin-induced diabetic rodents. Cell Mol Neurobiol 2014;34:643–649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Qiu W, Zhou Y, Jiang L, et al. Genipin inhibits mitochondrial uncoupling protein 2 expression and ameliorates podocyte injury in diabetic mice. PLoS ONE 2012;7:e41391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Friederich-Persson M, Aslam S, Nordquist L, Welch WJ, Wilcox CS, Palm F. Acute knockdown of uncoupling protein-2 increases uncoupling via the adenine nucleotide transporter and decreases oxidative stress in diabetic kidneys. PLoS ONE 2012;7:e39635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang CY, Baffy G, Perret P, et al. Uncoupling protein-2 negatively regulates insulin secretion and is a major link between obesity, beta cell dysfunction, and type 2 diabetes. Cell 2001;105:745–755 [DOI] [PubMed] [Google Scholar]
- 43.Dugan LL, You YH, Ali SS, et al. AMPK dysregulation promotes diabetes-related reduction of superoxide and mitochondrial function. J Clin Invest 2013;123:4888–4899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kang H, Ahn S, Choi P, et al. Defective fatty acid oxidation in renal tubular epithelial cells has a key role in kidney fibrosis development. Nat Med 2015;21:37–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.El-Osta A, Brasacchio D, Yao D, et al. Transient high glucose causes persistent epigenetic changes and altered gene expression during subsequent normoglycemia. J Exp Med 2008;205:2409–2417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.DeRubertis FR, Craven PA, Melhem MF, Salah EM. Attenuation of renal injury in db/db mice overexpressing superoxide dismutase: evidence for reduced superoxide-nitric oxide interaction. Diabetes 2004;53:762–768 [DOI] [PubMed] [Google Scholar]
- 47.Fujita H, Fujishima H, Chida S, et al. Reduction of renal superoxide dismutase in progressive diabetic nephropathy. J Am Soc Nephrol 2009;20:1303–1313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.DeRubertis FR, Craven PA, Melhem MF. Acceleration of diabetic renal injury in the superoxide dismutase knockout mouse: effects of tempol. Metabolism 2007;56:1256–1264 [DOI] [PubMed] [Google Scholar]
- 49.Fujita H, Fujishima H, Takahashi K, et al. SOD1, but not SOD3, deficiency accelerates diabetic renal injury in C57BL/6-Ins2(Akita) diabetic mice. Metabolism 2012;61:1714–1724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kawamata H, Manfredi G. Import, maturation, and function of SOD1 and its copper chaperone CCS in the mitochondrial intermembrane space. Antioxid Redox Signal 2010;13:1375–1384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Graham D, Huynh NN, Hamilton CA, et al. Mitochondria-targeted antioxidant MitoQ10 improves endothelial function and attenuates cardiac hypertrophy. Hypertension 2009;54:322–328 [DOI] [PubMed] [Google Scholar]
- 52.Reily C, Mitchell T, Chacko BK, Benavides G, Murphy MP, Darley-Usmar V. Mitochondrially targeted compounds and their impact on cellular bioenergetics. Redox Biol 2013;1:86–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cifarelli V, Geng X, Styche A, Lakomy R, Trucco M, Luppi P. C-peptide reduces high-glucose-induced apoptosis of endothelial cells and decreases NAD(P)H-oxidase reactive oxygen species generation in human aortic endothelial cells. Diabetologia 2011;54:2702–2712 [DOI] [PubMed] [Google Scholar]
- 54.Hoshiyama M, Li B, Yao J, Harada T, Morioka T, Oite T. Effect of high glucose on nitric oxide production and endothelial nitric oxide synthase protein expression in human glomerular endothelial cells. Nephron, Exp Nephrol 2003;95:e62–e68 [DOI] [PubMed] [Google Scholar]
- 55.Asaba K, Tojo A, Onozato ML, et al. Effects of NADPH oxidase inhibitor in diabetic nephropathy. Kidney Int 2005;67:1890–1898 [DOI] [PubMed] [Google Scholar]
- 56.Sedeek M, Gutsol A, Montezano AC, et al. Renoprotective effects of a novel Nox1/4 inhibitor in a mouse model of type 2 diabetes. Clin Sci (Lond) 2013;124:191–202 [DOI] [PubMed] [Google Scholar]
- 57.You YH, Okada S, Ly S, et al. Role of Nox2 in diabetic kidney disease. Am J Physiol Renal Physiol 2013;304:F840–F848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jha JC, Gray SP, Barit D, et al. Genetic targeting or pharmacologic inhibition of NADPH oxidase nox4 provides renoprotection in long-term diabetic nephropathy. J Am Soc Nephrol 2014;25:1237–1254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Youn JY, Siu KL, Lob HE, Itani H, Harrison DG, Cai H. Role of vascular oxidative stress in obesity and metabolic syndrome. Diabetes 2014;63:2344–2355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Block K, Gorin Y, Abboud HE. Subcellular localization of Nox4 and regulation in diabetes. Proc Natl Acad Sci U S A 2009;106:14385–14390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Brezniceanu ML, Liu F, Wei CC, et al. Attenuation of interstitial fibrosis and tubular apoptosis in db/db transgenic mice overexpressing catalase in renal proximal tubular cells. Diabetes 2008;57:451–459 [DOI] [PubMed] [Google Scholar]
- 62.Anderson EJ, Lustig ME, Boyle KE, et al. Mitochondrial H2O2 emission and cellular redox state link excess fat intake to insulin resistance in both rodents and humans. J Clin Invest 2009;119:573–581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lonn E, Bosch J, Yusuf S, et al.; HOPE and HOPE-TOO Trial Investigators . Effects of long-term vitamin E supplementation on cardiovascular events and cancer: a randomized controlled trial. JAMA 2005;293:1338–1347 [DOI] [PubMed] [Google Scholar]
- 64.Plecitá-Hlavatá L, Jezek J, Jezek P. Pro-oxidant mitochondrial matrix-targeted ubiquinone MitoQ10 acts as anti-oxidant at retarded electron transport or proton pumping within Complex I. Int J Biochem Cell Biol 2009;41:1697–1707 [DOI] [PubMed] [Google Scholar]
- 65.Leo S, Szabadkai G, Rizzuto R.. The mitochondrial antioxidants MitoE(2) and MitoQ(10) increase mitochondrial Ca(2+) load upon cell stimulation by inhibiting Ca(2+) efflux from the organelle. Ann N Y Acad Sci 2008;1147:264–274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pergola PE, Raskin P, Toto RD, et al.; BEAM Study Investigators . Bardoxolone methyl and kidney function in CKD with type 2 diabetes. N Engl J Med 2011;365:327–336 [DOI] [PubMed] [Google Scholar]
- 67.Hall DJ, Han SH, Chepetan A, Inui EG, Rogers M, Dugan LL. Dynamic optical imaging of metabolic and NADPH oxidase-derived superoxide in live mouse brain using fluorescence lifetime unmixing. J Cereb Blood Flow Metab 2012;32:23–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fernandes DC, Wosniak J Jr, Pescatore LA, et al. Analysis of DHE-derived oxidation products by HPLC in the assessment of superoxide production and NADPH oxidase activity in vascular systems. Am J Physiol Cell Physiol 2007;292:C413–C422 [DOI] [PubMed] [Google Scholar]
- 69.Kalyanaraman B, Dranka BP, Hardy M, Michalski R, Zielonka J. HPLC-based monitoring of products formed from hydroethidine-based fluorogenic probes—the ultimate approach for intra- and extracellular superoxide detection. Biochim Biophys Acta 2014;1840:739–744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vincent AM, Russell JW, Sullivan KA, et al. SOD2 protects neurons from injury in cell culture and animal models of diabetic neuropathy. Exp Neurol 2007;208:216–227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Boudina S, Sena S, O’Neill BT, Tathireddy P, Young ME, Abel ED. Reduced mitochondrial oxidative capacity and increased mitochondrial uncoupling impair myocardial energetics in obesity. Circulation 2005;112:2686–2695 [DOI] [PubMed] [Google Scholar]
- 72.Mogensen M, Sahlin K, Fernström M, et al. Mitochondrial respiration is decreased in skeletal muscle of patients with type 2 diabetes. Diabetes 2007;56:1592–1599 [DOI] [PubMed] [Google Scholar]
- 73.Dabkowski ER, Williamson CL, Bukowski VC, et al. Diabetic cardiomyopathy-associated dysfunction in spatially distinct mitochondrial subpopulations. Am J Physiol Heart Circ Physiol 2009;296:H359–H369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhang L, Yu C, Vasquez FE, et al. Hyperglycemia alters the Schwann cell mitochondrial proteome and decreases coupled respiration in the absence of superoxide production. J Proteome Res 2010;9:458–471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jornayvaz FR, Shulman GI. Regulation of mitochondrial biogenesis. Essays Biochem 2010;47:69–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sharma K, Karl B, Mathew AV, et al. Metabolomics reveals signature of mitochondrial dysfunction in diabetic kidney disease. J Am Soc Nephrol 2013;24:1901–1912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ling C, Del Guerra S, Lupi R, et al. Epigenetic regulation of PPARGC1A in human type 2 diabetic islets and effect on insulin secretion. Diabetologia 2008;51:615–622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Patti ME, Butte AJ, Crunkhorn S, et al. Coordinated reduction of genes of oxidative metabolism in humans with insulin resistance and diabetes: potential role of PGC1 and NRF1. Proc Natl Acad Sci U S A 2003;100:8466–8471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Choi J, Chandrasekaran K, Inoue T, Muragundla A, Russell JW. PGC-1α regulation of mitochondrial degeneration in experimental diabetic neuropathy. Neurobiol Dis 2014;64:118–130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chowdhury SK, Smith DR, Fernyhough P. The role of aberrant mitochondrial bioenergetics in diabetic neuropathy. Neurobiol Dis 2013;51:56–65 [DOI] [PubMed] [Google Scholar]
- 81.Carling D, Mayer FV, Sanders MJ, Gamblin SJ. AMP-activated protein kinase: nature’s energy sensor. Nat Chem Biol 2011;7:512–518 [DOI] [PubMed] [Google Scholar]
- 82.Declèves AE, Mathew AV, Cunard R, Sharma K. AMPK mediates the initiation of kidney disease induced by a high-fat diet. J Am Soc Nephrol 2011;22:1846–1855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Declèves AE, Zolkipli Z, Satriano J, et al. Regulation of lipid accumulation by AMP-activated kinase [corrected] in high fat diet-induced kidney injury. Kidney Int 2014;85:611–623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Eid AA, Ford BM, Block K, et al. AMP-activated protein kinase (AMPK) negatively regulates Nox4-dependent activation of p53 and epithelial cell apoptosis in diabetes. J Biol Chem 2010;285:37503–37512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pearson KJ, Baur JA, Lewis KN, et al. Resveratrol delays age-related deterioration and mimics transcriptional aspects of dietary restriction without extending life span. Cell Metab 2008;8:157–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Roy Chowdhury SK, Smith DR, Saleh A, et al. Impaired adenosine monophosphate-activated protein kinase signalling in dorsal root ganglia neurons is linked to mitochondrial dysfunction and peripheral neuropathy in diabetes. Brain 2012;135:1751–1766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ola MS, Berkich DA, Xu Y, et al. Analysis of glucose metabolism in diabetic rat retinas. Am J Physiol Endocrinol Metab 2006;290:E1057–E1067 [DOI] [PubMed] [Google Scholar]
- 88.Palomer X, Salvadó L, Barroso E, Vázquez-Carrera M. An overview of the crosstalk between inflammatory processes and metabolic dysregulation during diabetic cardiomyopathy. Int J Cardiol 2013;168:3160–3172 [DOI] [PubMed] [Google Scholar]
- 89.Xie Z, Lau K, Eby B, et al. Improvement of cardiac functions by chronic metformin treatment is associated with enhanced cardiac autophagy in diabetic OVE26 mice. Diabetes 2011;60:1770–1778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chen K, Li G, Geng F, et al. Berberine reduces ischemia/reperfusion-induced myocardial apoptosis via activating AMPK and PI3K-Akt signaling in diabetic rats. Apoptosis 2014;19:946–957 [DOI] [PubMed] [Google Scholar]
- 91.Yan W, Zhang H, Liu P, et al. Impaired mitochondrial biogenesis due to dysfunctional adiponectin-AMPK-PGC-1α signaling contributing to increased vulnerability in diabetic heart. Basic Res Cardiol 2013;108:329. [DOI] [PubMed] [Google Scholar]
- 92.Choi CS, Befroy DE, Codella R, et al. Paradoxical effects of increased expression of PGC-1alpha on muscle mitochondrial function and insulin-stimulated muscle glucose metabolism. Proc Natl Acad Sci U S A 2008;105:19926–19931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sawada N, Jiang A, Takizawa F, et al. Endothelial PGC-1α mediates vascular dysfunction in diabetes. Cell Metab 2014;19:246–258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Damelin LH, Vokes S, Whitcutt JM, Damelin SB, Alexander JJ. Hormesis: a stress response in cells exposed to low levels of heavy metals. Hum Exp Toxicol 2000;19:420–430 [DOI] [PubMed] [Google Scholar]
- 95.Mackenzie RM, Salt IP, Miller WH, et al. Mitochondrial reactive oxygen species enhance AMP-activated protein kinase activation in the endothelium of patients with coronary artery disease and diabetes. Clin Sci (Lond) 2013;124:403–411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ristow M, Zarse K, Oberbach A, et al. Antioxidants prevent health-promoting effects of physical exercise in humans. Proc Natl Acad Sci U S A 2009;106:8665–8670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hatori M, Vollmers C, Zarrinpar A, et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab 2012;15:848–860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ghosh S, Khazaei M, Moien-Afshari F, et al. Moderate exercise attenuates caspase-3 activity, oxidative stress, and inhibits progression of diabetic renal disease in db/db mice. Am J Physiol Renal Physiol 2009;296:F700–F708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bherer L, Erickson KI, Liu-Ambrose T. A review of the effects of physical activity and exercise on cognitive and brain functions in older adults. J Aging Res 2013;2013:657508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wing RR, Bolin P, Brancati FL, et al.; Look AHEAD Research Group . Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med 2013;369:145–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lee MJ, Feliers D, Mariappan MM, et al. A role for AMP-activated protein kinase in diabetes-induced renal hypertrophy. Am J Physiol Renal Physiol 2007;292:F617–F627 [DOI] [PubMed] [Google Scholar]
- 102.Zou MH, Xie Z. Regulation of interplay between autophagy and apoptosis in the diabetic heart: new role of AMPK. Autophagy 2013;9:624–625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yu X, Zhang L, Yang X, et al. Salvianolic acid A protects the peripheral nerve function in diabetic rats through regulation of the AMPK-PGC1α-Sirt3 axis. Molecules 2012;17:11216–11228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kubota S, Ozawa Y, Kurihara T, et al. Roles of AMP-activated protein kinase in diabetes-induced retinal inflammation. Invest Ophthalmol Vis Sci 2011;52:9142–9148 [DOI] [PubMed] [Google Scholar]
- 105.Sharma K, Ramachandrarao S, Qiu G, et al. Adiponectin regulates albuminuria and podocyte function in mice. J Clin Invest 2008;118:1645–1656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zhou G, Myers R, Li Y, et al. Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Invest 2001;108:1167–1174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Feng X, Luo Z, Ma L, et al. Angiotensin II receptor blocker telmisartan enhances running endurance of skeletal muscle through activation of the PPAR-δ/AMPK pathway. J Cell Mol Med 2011;15:1572–1581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hawley SA, Fullerton MD, Ross FA, et al. The ancient drug salicylate directly activates AMP-activated protein kinase. Science 2012;336:918–922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zhang LN, Xu L, Zhou HY, et al. Novel small-molecule AMP-activated protein kinase allosteric activator with beneficial effects in db/db mice. PLoS ONE 2013;8:e72092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kume S, Kitada M, Kanasaki K, Maegawa H, Koya D. Anti-aging molecule, Sirt1: a novel therapeutic target for diabetic nephropathy. Arch Pharm Res 2013;36:230–236 [DOI] [PubMed] [Google Scholar]
- 111.Kume S, Haneda M, Kanasaki K, et al. Silent information regulator 2 (SIRT1) attenuates oxidative stress-induced mesangial cell apoptosis via p53 deacetylation. Free Radic Biol Med 2006;40:2175–2182 [DOI] [PubMed] [Google Scholar]
- 112.Nemoto S, Fergusson MM, Finkel T. SIRT1 functionally interacts with the metabolic regulator and transcriptional coactivator PGC-1{alpha}. J Biol Chem 2005;280:16456–16460 [DOI] [PubMed] [Google Scholar]
- 113.Gurd BJ. Deacetylation of PGC-1α by SIRT1: importance for skeletal muscle function and exercise-induced mitochondrial biogenesis. Appl Physiol Nutr Metab 2011;36:589–597 [DOI] [PubMed] [Google Scholar]
- 114.Eirin A, Li Z, Zhang X, et al. A mitochondrial permeability transition pore inhibitor improves renal outcomes after revascularization in experimental atherosclerotic renal artery stenosis. Hypertension 2012;60:1242–1249 [DOI] [PubMed] [Google Scholar]
- 115.Inoki K, Mori H, Wang J, et al. mTORC1 activation in podocytes is a critical step in the development of diabetic nephropathy in mice. J Clin Invest 2011;121:2181–2196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Eid AA, Ford BM, Bhandary B, et al. Mammalian target of rapamycin regulates Nox4-mediated podocyte depletion in diabetic renal injury. Diabetes 2013;62:2935–2947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lee MJ, Feliers D, Sataranatarajan K, et al. Resveratrol ameliorates high glucose-induced protein synthesis in glomerular epithelial cells. Cell Signal 2010;22:65–70 [DOI] [PMC free article] [PubMed] [Google Scholar]