Abstract
Background
Upper body subcutaneous neck fat (UBSF) is a unique fat depot anatomically separate from visceral abdominal fat that appears to be associated with cardiometabolic risk above and beyond generalized adiposity. We sought to develop a protocol to quantify UBSF using multidetector computed tomography measurements.
Methods and Results
Protocol development was performed in participants from the Framingham Heart Study who had participated in the multidetector computed tomography scanning substudy, consisting of chest scans. Volumetric assessment of UBSF was defined by 40 contiguous 0.625‐mm slices superior to the body of the sternum. The reader manually traced the chest to identify total neck fat. Breast tissue exterior to the chest wall was excluded. Subcutaneous and visceral fat volumes were obtained using standard protocols. Age‐ and sex‐adjusted Pearson correlation coefficients were used to assess the association among UBSF, traditional adiposity measures, and cardiometabolic risk factors. Inter‐ and intrareader reproducibility was assessed using intraclass correlation coefficients. Volumetric assessments were obtained in 92 participants because 8 scans were not readable (51% women; mean age: 59 years [women], 58 years [men]). The mean volume of UBSF was 310 cm3 for women and 345 cm3 for men. Intra‐ and interreader class correlation coefficients were 0.99 and 0.99, respectively. UBSF was correlated with waist circumference (r=0.90), neck circumference (r=0.75), body mass index (r=0.89), subcutaneous adipose tissue (r=0.87), and visceral adipose tissue (r=0.86).
Conclusions
UBSF can be quantified reproducibly using computed tomography in a community‐dwelling sample from the Framingham Heart Study.
Keywords: fat distribution, multidetector computed tomography, upper body subcutaneous neck fat
Introduction
The prevalence of obesity in the United States has reached epidemic proportions and continues to rise.1 Numerous harmful sequelae of obesity including increased cardiometabolic risk2–4 and overall mortality5 have been demonstrated. Variations in body fat distribution, independent of generalized adiposity, may be associated with differential metabolic risk. Visceral adipose tissue (VAT) is a fat depot that has been associated with an increased risk of metabolic syndrome, insulin resistance, and type 2 diabetes.2–3 However, studies have demonstrated only modest correlations between cardiometabolic risk factors and visceral adiposity, leading investigators to hypothesize that other fat depots may confer additional risk for the development of cardiovascular disease.2,6 Upper body subcutaneous neck fat (UBSF) is a unique fat depot located in a separate anatomic compartment and has been associated with insulin resistance independent of VAT.7–8 Consequently, this fat depot may be associated with differential cardiometabolic risk above and beyond generalized adiposity and visceral fat.
Traditional measures of obesity have included anthropometric measurements including body mass index (BMI) and waist circumference, both of which have been correlated with increased risk of obesity‐related morbidity.2,9 Further research, including data from our group, has shown that neck circumference has been correlated with cardiometabolic risk factors even after adjusting for levels of visceral adiposity and BMI,6 suggesting the significance of UBSF in the pathogenesis of obesity. In addition, we have also shown that neck circumference is associated with carotid atherosclerotic disease above and beyond other measures of adiposity10; however, neck circumference is only a proxy for UBSF. We aimed to develop a protocol to quantify UBSF using multidetector computed tomography (MDCT) in a community‐dwelling sample from the Framingham Heart Study.
Methods
Study Participants
The original Framingham Heart Study cohort was first established in 1948 with the original cohort recruited from Framingham, Massachusetts. The Offspring and Third Generation cohorts were recruited subsequently and have been well described previously.11–12
The MDCT substudy consists of 1333 participants from the Offspring cohort and 1431 participants from the Third Generation cohort who underwent computed tomography imaging as part of a comprehensive assessment of vascular calcification. Participants for our current analysis are drawn from the MDCT 2 substudy who underwent scanning from September 2008 to December 2011. Clinical characteristics were obtained at Offspring exam 8 and Third Generation exam 2. Inclusion criteria included an age of >35 years for men and >40 years for nonpregnant women. All participants weighed <450 lb because of MDCT scanner specifications.
A sample of 100 participants was selected from the study population for the purposes of the present analysis. This sample was randomly selected to include 50 women and 50 men evenly spread across the ages and divided between the Offspring and Third Generation cohorts. The institutional review boards of Boston University Medical Center and Massachusetts General Hospital approved the study protocol, and all participants provided written consent.
MDCT Scan Acquisition
Subjects underwent MDCT imaging of the thorax in a supine position using a General Electric Discovery VCT 64‐slice PET/CT scanner (GE Healthcare). The entire chest from the lung base to the apices was imaged using a prospectively ECG‐triggered computed tomography scanning protocol during a single inspirational breath hold to enable lung and coronary assessment of the apices. The gantry rotation time was 0.35 seconds, the tube voltage was 120 kVp, and the tube current was 300 mA (subject weight ≤220 lb) or 350 mA (subject weight >220 lb). A detector width of 0.625 mm was used. The 210° scan reconstruction algorithm was used, providing 210° of raw scan data (tube rotation) with an optimized reconstruction technique that provided images of ≈175‐ms temporal resolution depending on the speed of gantry rotation (0.35 seconds).
Quantification of Upper Body Subcutaneous Neck Fat
MDCT slices were loaded onto a dedicated offline workstation (Aquarius 3D workstation; TeraRecon Inc). A predefined image display setting (−195 to −45 Hounsfield units; center: −120 Hounsfield units) was used to identify adipose tissue within these slices.
The anatomic region of interest was defined by 40 contiguous 0.625‐mm slices superior to the body of the sternum and covering an area of 25 mm. The sternal landmark was determined by the first single slice to show the bowtie shape of the sternum filled completely with trabecular bone (Figure 1A). Forty contiguous slices above the sternum were selected, and every 10th slice starting with the first slice was manually reviewed. The reader manually excluded the adipose tissue within the mediastinum (Figure 1B) for the total neck fat. The reader then outlined the adipose tissue exterior to the chest wall (Figure 1C) to exclude breast tissue. The final region of interest was defined as UBSF and was volumetrically measured (cubic centimeters). The full protocol appears in Data S1.
Figure 1.
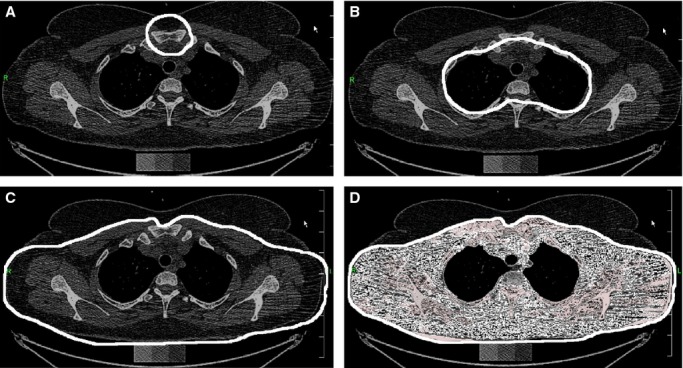
Chest computed tomography scans demonstrating upper body subcutaneous neck fat (UBSF) measurement technique. A, Example of the initial slice displaying the sternal landmark. B, Example of manual tracing to exclude mediastinal fat (total neck fat). C, Example of manual tracing to exclude breast tissue (breast fat). D, Example of total area of fat quantified (UBSF).
Assessment of Covariates
BMI, waist circumference, neck circumference, systolic blood pressure, diastolic blood pressure, fasting plasma glucose, and fasting lipids were determined based on study visit evaluations. BMI was calculated by dividing the weight (kilograms) by the square of height (meters). Waist circumference was measured to the nearest 0.25 inch at the level of the umbilicus. Neck circumference was measured to the nearest 0.25 inch below the laryngeal prominence and perpendicular to the long axis of the neck. Plasma glucose, insulin, and lipids were measured on fasting morning samples.
Diabetes was defined as a fasting plasma glucose ≥126 mg/dL or treatment with insulin or a hypoglycemic agent. Participants were considered to be current smokers if they smoked ≥1 cigarettes per day for the last year.
Among the representative preselected sample of 100 participants used for this analysis, 2 scans did not have adequate slices through the anatomic region of interest, 3 scans did not have the required 40 scans superior to the sternal landmark, and 3 had unusual anatomy disrupting the landmarks, resulting in a readable sample size of 92. This sample size of 92 was used to determine reproducibility. One participant did not attend the clinical examination, and no baseline characteristics were available; therefore, the sample characteristics are based on a sample size of 91.
Abdominal subcutaneous adipose tissue (SAT) and VAT volumes were previously determined using a protocol for abdominal adipose tissue quantification that was described previously.13
Statistical Analysis
The protocol was completed independently by 2 readers (K.J.R., K.E.T.) for interobserver variation and then repeated by the first reader (K.J.R.) for intraobserver variation. Inter‐ and intrareader reproducibility was evaluated using intraclass correlation coefficients. Pearson correlation coefficients were calculated to determine the association between UBSF and cardiometabolic risk factors. Statistical analyses were performed using SAS version 9.2 (SAS Institute Inc).
Results
Sample Characteristics
Baseline characteristics for the sample are presented in Table 1. The mean age was 58.8 years for women and 57.9 years for men. Women composed 51% of the sample. The mean BMI was 27.1 kg/m2 for women and 27.8 kg/m2 for men.
Table 1.
Study Sample Characteristics
| Women (n=45)* | Men (n=46)* | |
|---|---|---|
| Mean (SD) | ||
| Continuous characteristics | ||
| Age, y | 58.6 (10.0) | 57.6 (11.1) |
| BMI, kg/m2 | 27.1 (5.0) | 27.8 (4.7) |
| Waist circumference, cm | 96.7 (14.4) | 100.2 (11.8) |
| Neck circumference, cm* | 33.6 (2.2) | 41.3 (3.1) |
| VAT, cm3 | 1589 (943) | 2784 (1328) |
| SAT, cm3 | 3672 (1605) | 2779 (1266) |
| Fasting glucose, mg/dL | 97 (10.1) | 105 (30.4) |
| SBP, mm Hg | 119 (14.1) | 125 (17.2) |
| HDL cholesterol, mg/dL | 63 (19.6) | 52 (16.3) |
| Triglycerides, mg/dL | 120 (165.3) | 122 (95.3) |
| Total neck fat | 438 (108.7) | 429 (86.8) |
| Breast fat | 128 (45.6) | 83 (25.4) |
| Upper body subcutaneous neck fat* | 310 (71.0) | 345 (65.6) |
| Categorical characteristics | ||
| Current smoker, % | 6.5 | 13.3 |
| Diabetes, % | 0 | 6.7 |
Data presented as mean (SD) for continuous characteristics and mean (SD) or median (quartile 1, quartile 3) for categorical characteristics. BMI, indicates body mass index; HDL, high‐density lipoprotein; SAT, subcutaneous adipose tissue; SBP, systolic blood pressure; VAT, visceral adipose tissue.
Based on a sample size of 91 because 1 participant did not attend the clinical examination and thus no baseline clinical characteristics were available.
Data on neck circumference was available for 42 patients because it was not measured in Offspring exam 8.
Upper body subcutaneous neck fat equals total neck fat minus breast fat.
Distribution of Upper Body Subcutaneous Neck Fat
The mean volume of total neck fat was 438 cm3 for women and 429 cm3 for men. The mean volume of breast tissue fat was 128 cm3 for women and 83 cm3 for men. The anatomic area of interest, UBSF, was defined by the total neck fat minus the breast fat (Figure 1). The mean volume of UBSF was 310 cm3 for women and 345 cm3 for men.
Intra‐ and Interreader Reproducibility
Intra‐ and interreader measurements are plotted in Figure 2. The intrareader intraclass correlation coefficient was 0.99, and the interreader intraclass correlation coefficient was 0.99.
Figure 2.
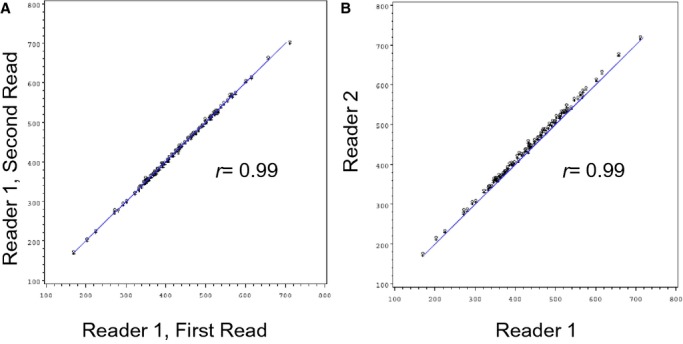
Intrareader (A) and interreader (B) upper body subcutaneous neck fat measurement.
Correlation of Upper Body Subcutaneous Neck Fat With Cardiometabolic Risk
Age‐ and sex‐adjusted Pearson correlation coefficients for UBSF and cardiometabolic risk factors are presented in Table 2. UBSF was strongly correlated with waist circumference (r=0.90), BMI (r=0.89), SAT (r=0.87), and VAT (r=0.86). UBSF also correlated with neck circumference (r=0.75).
Table 2.
Age‐ and Sex‐Adjusted Pearson Correlation Coefficients for Upper Body Subcutaneous Neck Fat and Cardiometabolic Risk Factors
| Neck Circumference* | Upper Body Subcutaneous Neck Fat* | |
|---|---|---|
| Age | 0.17 (P=0.28) | 0.14 (P=0.19) |
| BMI | 0.73 (P<0.001) | 0.89 (P<0.001) |
| Waist circumference | 0.65 (P<0.001) | 0.90 (P<0.001) |
| Neck circumference | NA | 0.75 (P<0.001) |
| VAT | 0.71 (P<0.001) | 0.86 (P<0.001) |
| SAT | 0.56 (P<0.001) | 0.87 (P<0.001) |
| Fasting glucose | 0.39 (P=0.011) | 0.46 (P<0.001) |
| SBP | 0.60 (P<0.001) | 0.36 (P<0.001) |
| HDL | −0.35 (P=0.028) | −0.29 (P=0.005) |
| Triglycerides | 0.31 (P=0.046) | 0.31 (P=0.003) |
BMI, indicates body mass index; HDL, high‐density lipoprotein; NA, not available; SAT, subcutaneous adipose tissue; SBP, systolic blood pressure; VAT, visceral adipose tissue.
Data on neck circumference was available for 42 patients because it was not measured in Offspring exam 8.
Upper body subcutaneous neck fat equals total neck fat minus breast fat.
Discussion
The findings of this study are 2‐fold. First, the quantification of UBSF using computed tomography is feasible and reproducible in a community‐dwelling sample from the Framingham Heart Study. Second, UBSF is correlated with cardiometabolic risk including strong correlations with other measures of adiposity in our feasibility study.
Traditional measures of obesity include anthropometric measurements such as BMI and waist circumference, both of which have been correlated with increased cardiometabolic risk and increased risk of obesity‐related morbidity.2,9 Although BMI is an excellent indicator of obesity, it does not account for regional fat distribution and cannot differentiate among fat compartments.2 Fat distribution studies have used imaging modalities such as computed tomography to quantify and differentiate abdominal adipose tissue depots.2–3 Both VAT and SAT have been associated with cardiometabolic risk, but VAT has been shown to be a particularly pathogenic fat depot.2–3 Data from the Framingham Heart Study showed that waist circumference was highly correlated with VAT (r=0.78 for women and r=0.73 for men) but also with SAT (r=0.87 for women and r=0.88 for men), suggesting that waist circumference cannot discriminate between VAT and SAT.2 Similar to previous studies of waist circumference, studies of neck circumference have shown an association between UBSF and insulin resistance, elevated blood pressure, and dyslipidemia6,14; however, neck circumference is only a proxy for UBSF. Direct volumetric quantification of this novel depot is needed to understand the full clinical implications.
We have developed a protocol for the quantification of UBSF that has high inter‐ and intrareader reproducibility. The present study adds a reproducible technique to the literature that allows for further evaluation of upper body fat. Through the use of this protocol, characterization of UBSF can be quantified, leading to the ability to assess the correlations of this fat depot with clinical characteristics and obesity outcomes. Ultimately, implementation of this protocol more broadly may help provide further insight into the role of regional fat distribution and better mechanistic understanding of obesity‐related complications related to UBSF.
Major strengths of our study include the use of a large, community‐dwelling population with comprehensively defined clinical characteristics. The use of 2 independent readers helped to establish the reproducibility of our protocol. To our knowledge, there are no other gold standard measurements of UBSF, and that limits our ability to assess measurement of validity. The study sample is predominantly of European ancestry, and generalizability to other ethnicities or populations enriched with UBSF is uncertain.
Conclusion
UBSF can be reproducibly quantified using computed tomography in a community‐dwelling sample from the Framingham Heart Study. UBSF is correlated with cardiometabolic risk and other measures of adiposity. Quantification of this unique fat depot may add to the mechanistic understanding of regional fat distribution.
Supplementary Material
Appendix Upper Body Subcutaneous Neck Fat Data Acquisition Protocol.
Sources of Funding
This research was conducted in part using data and resources from the FHS of the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health and Boston University School of Medicine. This work was partially supported by the NHLBI's FHS (Contract No. N01‐HC‐25195). Dr Rosenquist is supported through funding from the Whitaker Cardiovascular Institute (T32 HL007224).
Disclosures
None.
Reference
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. J Am Med Assoc. 2010; 303:235-241. [DOI] [PubMed] [Google Scholar]
- 2.Fox CS, Massaro JM, Hoffman U, Pou KM, Maurovich‐Horvat P, Liu CY, Vasan RS, Murabito JM, Meigs JB, Cupples LA, D'Agostino RB, Sr, O'Donnell CJ. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation. 2007; 116:39-48. [DOI] [PubMed] [Google Scholar]
- 3.Goodpaster BH, Krishnaswami S, Harris TB, Katsiaras A, Kritchevsky SB, Simonsick EM, Nevitt M, Holvoet P, Newman AB. Obesity, regional body fat distribution, and the metabolic syndrome in older men and women. Arch Intern Med. 2005; 165:777-783. [DOI] [PubMed] [Google Scholar]
- 4.McLaughlin T, Abbasi F, Lamendola C, Reaven G. Heterogeneity in the prevalence of risk factors for cardiovascular disease and type 2 diabetes mellitus in obese individuals: effect of differences in insulin sensitivity. Arch Intern Med. 2007; 167:642-648. [DOI] [PubMed] [Google Scholar]
- 5.Pischon T, Boeing H, Hoffmann K, Bergmann M, Schulze MB, Overvad K, van der Schouw YT, Spencer E, Moons KG, Tjonneland A, Halkjaer J, Jensen MK, Stegger J, Clavel‐Chapelon F, Boutron‐Ruault MC, Chajes V, Linseisen J, Kaaks R, Trichopoulou A, Trichopoulos D, Bamia C, Sieri S, Palli D, Tumino R, Vineis P, Panico S, Peeters PH, May AM, Bueno‐de‐Mesquita HB, van Duijnhoven FJ, Hallmans G, Weinehall L, Manjer J, Hedblad B, Lund E, Agudo A, Arriola L, Barricarte A, Navarro C, Martinez C, Quiros JR, Key T, Bingham S, Khaw KT, Boffetta P, Jenab M, Ferrari P, Riboli E. General and abdominal adiposity and risk of death in Europe. N Engl J Med. 2008; 359:2105-2120. [DOI] [PubMed] [Google Scholar]
- 6.Preis SR, Massaro JM, Hoffmann U, D'Agostino RB, Sr, Levy D, Robins SJ, Meigs JB, Vasan RS, O'Donnell CJ, Fox CS. Neck circumference as a novel measure of cardiometabolic risk: the Framingham Heart Study. J Clin Endocrinol Metab. 2010; 95:3701-3710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grunfeld C, Rimland D, Gibert CL, Powderly WG, Sidney S, Shlipak MG, Bacchetti P, Scherzer R, Haffner S, Heymsfield SB. Association of upper trunk and visceral adipose tissue volume with insulin resistance in control and HIV‐infected subjects in the FRAM study. J Acquir Immune Defic Syndr. 2007; 46:283-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martin ML. Effects of body fat distribution on regional lipolysis in obesity. J Clin Investig. 1991; 88:609-613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cornier MA, Despres JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, Lopez‐Jimenez F, Rao G, St‐Onge MP, Towfighi A, Poirier P. Assessing adiposity. Circulation. 2011; 124:1996-2019. [DOI] [PubMed] [Google Scholar]
- 10.Rosenquist KJ, Massaro JM, Pencina KM, D'Agostino RB, Beiser A, O'Connor GT, O'Donnell CJ, Wolf PA, Polak JF, Seshadri S, Fox CS. Neck circumference, carotid wall intima‐media thickness, and incident stroke. Diabetes Care. 2013; 36:e153-e154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kannel W, Feinleib M, McNamara P, Garrison R, Castelli W. An investigation of coronary heart disease in families. The Framingham offspring study. Am J Epidemiol. 1979; 110:281-290. [DOI] [PubMed] [Google Scholar]
- 12.Splansky GL, Corey D, Yang Q, Atwood LD, Cupples LA, Benjamin EJ, D'Agostino RB, Sr, Fox CS, Larson MG, Murabito JM, O'Donnell CJ, Vasan RS, Wolf PA, Levy D. The third generation Cohort of the National Heart, Lung, and Blood Institute's Framingham Heart Study: design, recruitment, and initial examination. Am J Epidemiol. 2007; 165:1328-1335. [DOI] [PubMed] [Google Scholar]
- 13.Maurovich‐Horvat P, Massaro J, Fox CS, Moselewski F, O'Donnell CJ, Hoffmann U. Comparison of anthropometric, area‐ and volume‐based assessment of abdominal subcutaneous and visceral adipose tissue volumes using multi‐detector computed tomography. Int J Obes. 2006; 31:500-506. [DOI] [PubMed] [Google Scholar]
- 14.Fitch KV, Stanley TL, Looby SE, Rope AM, Grinspoon SK. Relationship between neck circumference and cardiometabolic parameters in HIV‐infected and non‐HIV‐infected adults. Diabetes Care. 2011; 34:1026-1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix Upper Body Subcutaneous Neck Fat Data Acquisition Protocol.


