Abstract
Background
Variability in the duration of attempted in‐hospital cardiopulmonary resuscitation (CPR) is high, but the factors influencing termination of CPR efforts are unknown.
Methods and Results
We examined the association between patient and hospital characteristics and CPR duration in 45 500 victims of in‐hospital cardiac arrest who did not experience return of spontaneous circulation (ROSC) and who were enrolled in the Get With the Guidelines registry between 2001 and 2010. In a secondary analysis, we performed analyses in 46 168 victims of in‐hospital cardiac arrest who experienced ROSC. We used ordered logistic regression to identify factors associated with CPR duration. Analyses were conducted by tertile of CPR duration (tertiles: ROSC group: 2 to 7, 8 to 17, and 18 to 120 minutes; no‐ROSC group: 2 to 16, 17 to 26, 27 to 120 minutes). In those without ROSC, younger age (aged 18 to 40 versus >65 years; odds ratio [OR] 1.81; 95% CI 1.69 to 1.95; P<0.001), female sex (OR 1.05; 95% CI 1.02 to 1.09; P=0.005), ventricular tachycardia or fibrillation (OR 1.50; 95% CI 1.42 to 1.58; P<0.001), and the need to place an invasive airway (OR 2.59; 95% CI 2.46 to 2.72; P<0.001) were associated with longer CPR duration. In those with ROSC, ventricular tachycardia or fibrillation (OR 0.89; 95% CI 0.85 to 0.93; P<0.001) and witnessed events (OR 0.87; 95% CI 0.82 to 0.91; P<0.001) were associated with shorter duration.
Conclusions
Age and sex were associated with attempted CPR duration in patients who do not experience ROSC after in‐hospital cardiac arrest but not in those who experience ROSC. Understanding the mechanism of these interactions may help explain variability in outcomes for in‐hospital cardiac arrest.
Keywords: cardiopulmonary resuscitation, heart arrest, resuscitation, survival
Introduction
Approximately 200 000 in‐hospital cardiac arrests (IHCAs) occur in the United States annually, and outcomes remain poor.1–2 Detailed guidelines dictate how cardiopulmonary resuscitation (CPR) should be performed (eg, rate and depth of compressions, number of breaths), but comparatively little is known about when resuscitation should be terminated. American Heart Association CPR guidelines do not make specific recommendations regarding the timing of CPR termination in IHCA.3 No diagnostic tests reliably indicate which patients will survive a cardiac arrest. Consequently, health care providers must rely on other factors to determine when to terminate CPR. The process by which this decision making occurs is not well understood. In the event of return of spontaneous circulation (ROSC), CPR is terminated because the patient is no longer in cardiac arrest. For patients without ROSC, the decision to continue or terminate CPR is more difficult in the absence of standardized and objective measures of futility.
Recent studies suggest that the duration of resuscitation may be associated with survival. In a recent analysis by Goldberger et al,4 hospitals with a longer median duration of resuscitation were found to have higher rates of survival. It is possible that the wide variability in outcome after IHCA is related to differences in how clinicians decide when to start and stop CPR. Although the contribution of various patient factors to outcomes in IHCA has been well documented, little is known about the factors that affect the duration of attempted CPR after IHCA.5–16 Some studies have shown that age and sex may affect both the decision to perform CPR and CPR duration,17–18 but these studies were limited by small sample size. Furthermore, it is not known whether other patient‐ or hospital‐level factors affect attempted CPR duration.
We hypothesized that patient‐level factors, such as age, race, and sex, are related to attempted CPR duration in IHCA. To evaluate this hypothesis, we used the largest and most comprehensive registry of IHCA events, the Get With The Guidelines–Resuscitation (GWTG‐R) registry. In our primary analyses, we evaluated only those without ROSC after IHCA, a group in which CPR lasts until a decision is made to terminate. In secondary analyses, we evaluated the association between patient‐ and hospital‐level factors and CPR duration in patients with ROSC after IHCA. In this group, CPR is terminated because resuscitation was successful rather than as the result of a physician or team decision to stop unsuccessful efforts.
Methods
The GWTG‐R registry is a multicenter database of IHCA events maintained by the American Heart Association. In this retrospective study, data from the GWTG‐R registry were used to determine the predictors of CPR duration in hospitalized patients.
Briefly, data in the GWTG‐R registry are collected according to standardized Utstein definitions.19 Cardiac arrest is defined as the absence of a palpable central pulse, apnea, and unresponsiveness. Cardiac arrests are identified by review of cardiac arrest flow sheets, review of paging system logs, routine checks of CPR carts, and screening for charges from hospital billing offices. The records of patients with documented cardiac arrest and without active do‐not‐resuscitate orders are reviewed by dedicated study staff members, and deidentified data are transmitted to a central database. Additional details about the GWTG‐R registry have been described previously.20
Study Population
The study cohort included all subjects with treated cardiac arrest in the GWTG database from 2001 to 2010. Initially, 137 691 patients with detailed information on IHCA were identified (Figure 1). We excluded those aged <18 years (n=3) and hospital employees (n=192). We also excluded patients with implantable cardioverter‐defibrillators (n=2273) and events that occurred in emergency departments; operating rooms or postoperative areas; and procedural, ambulatory, and rehabilitation areas (n=23 388). Events <2 minutes or >120 minutes in duration (n=3260) were excluded from the analyses. We also excluded events that were not the first event in the index admission (n=16 575) and that occurred at hospitals that reported <6 months of data and had <10 cardiac arrests during the study period (n=342). A total of 91 658 events were included in the final analyses.
Figure 1.
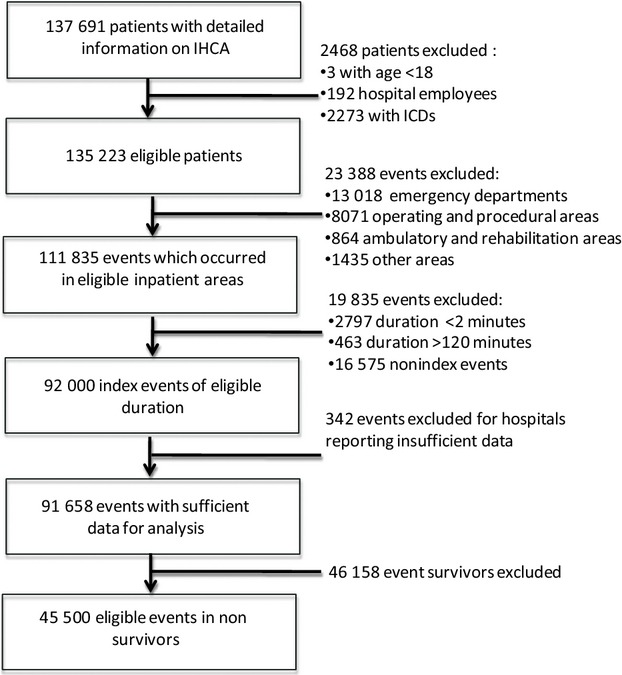
Study cohort with associated inclusion and exclusion variables. ICD indicates implantable cardioverter‐defibrillator; IHCA, in‐hospital cardiac arrest.
CPR Duration
Based on the GWTG‐R protocol, a start time and an end time for CPR were collected from the resuscitation sheet. For the purposes of this study, CPR duration was defined as the entire time of CPR in minutes from the start to the end of the event. The distribution of the CPR duration was determined, and CPR length was divided into tertiles to categorize events as short duration, medium duration, and long duration.
Study Variables
Coding of study variables was performed by the hospitals at which the events occurred. Patient‐level factors (demographics, comorbidities, intra‐arrest factors) hypothesized to influence IHCA CPR duration were evaluated. These factors included those previously shown to be associated with outcome after IHCA in this cohort and others. Demographic factors included age, race, and sex. Comorbidities were defined as cardiac (arrhythmia, congestive heart failure, and myocardial infarction), pulmonary (respiratory insufficiency and pneumonia), neurological (acute stroke, central nervous system depression, acute nonstroke neurologic events), renal (renal insufficiency), or metastatic or hematologic malignancy. Patients who had known prior cardiac arrest were identified.
Intra‐arrest factors evaluated included arrest location, initial rhythm, presence of witnesses, temporal arrest characteristics, and etiology. The location of the event was identified as 1 of the following areas: unmonitored hospital bed, monitored hospital bed, or intensive care unit. The initial rhythm (asystole, pulseless electrical activity, or ventricular tachycardia or fibrillation) was recorded. The absence or presence of at least 1 defibrillation during the event was recorded. Events were categorized as occurring on a weekend (11:00 pm Friday through 6:59 am Monday) or nonweekend day and as occurring during the day (7:00 am through 10:59 pm) or at night (11:00 pm through 6:59 am).
The presumed cause of the arrest was divided into the following categories: cardiac (active or evolving myocardial infarction, arrhythmia, pulmonary edema), respiratory (pulmonary embolus, acute respiratory insufficiency, inadequate natural or invasive airway, ventilator malfunction, and pneumothorax), neurological (acute stroke, status epilepticus), or systemic/metabolic (hypotension or hypoperfusion, hypothermia, metabolic or electrolyte abnormalities). Events could be classified as having >1 cause. In the coding instructions for this registry, hypotension or hypoperfusion is defined as systolic blood pressure <90 mm Hg or mean arterial pressure <60 mm Hg. Acute respiratory insufficiency is defined by the need for emergency assisted ventilation within 1 hour up to the time of the cardiopulmonary arrest, PaO2:FiO2 ratio <300, PaO2 <60 mm Hg, SaO2 <90%, PaCO2 >50 mm Hg, or a spontaneous respiratory rate >40 breaths per minute or <5 breaths per minute. Hypothermia is defined as a core temperature <34°C. Metabolic or electrolyte abnormalities were defined as blood glucose <60 mg/dL, lactate >2.5 mmol/L, magnesium >4 mEq/L, arterial pH <7.3 or >7.5, potassium <2.5 or >6 mEq/L, and sodium <125 or >150 mEq/L. The presence or absence of assisted ventilation (either a mechanical ventilator or invasive airway) and the need to place an invasive airway were evaluated.
Hospital Factors
CPR duration may be related to institutional factors like hospital policies and practices. Consequently, we evaluated several hospital factors to determine their impact on CPR duration: geographic region (Atlantic, north central, south central, Mountain–Pacific), inpatient‐bed volume (<250 beds [small], 250 to 499 beds [medium], >500 beds[large]), and academic training program status (presence or absence of residency or fellowship training programs). Also evaluated were urban versus rural status, for‐profit versus public status, and event volume. Hospitals were coded as high volume if the median IHCA volume was greater than the median in the entire study sample.
Outcome Measures
The main outcome variable was CPR duration in minutes.
Statistical Methods
The baseline characteristics of the study sample were evaluated using ANOVA for continuous variables and chi‐square tests for categorical variables. Summary statistics were used to characterize CPR duration, and a graph was used to determine the distribution. Differences in baseline characteristics by tertile of CPR duration were analyzed using ANOVA or chi‐square tests. Ordered logistic regression was used to examine the multivariable associations of patient‐ and hospital‐level factors with CPR duration. CPR duration was included in the model in tertiles.21 Multivariable analyses included CPR duration as the dependent variable and age, sex, race, pre‐existing comorbidities, prior cardiopulmonary arrest, prior intensive care unit stay, event location, initial rhythm, witnessed versus unwitnessed event, weekend versus nonweekend, night versus day, pre‐existing airway or mechanical ventilation, the need to place an invasive airway, cause of arrest, academic hospital status, hospital size, urban versus rural status, public versus for‐profit status, hospital location, and high versus low volume as the independent variables. To determine the proportion of the variability that occurred between hospitals, an intraclass correlation coefficient was calculated as between‐hospital variance divided by the sum of between‐hospital variance and within‐hospital variance. Events of <2 minutes in duration were included in the sample in a secondary analysis.
All statistical analyses were performed using SAS version 9.1 (SAS Institute Inc). This study was approved by the institutional review board at the Hospital of the University of Pennsylvania.
Results
The final study cohort, including those both with and without ROSC, consisted of 91 658 patients from 470 hospitals (Figure 1). Baseline characteristics of the study sample are shown in Table 1. Compared with the ROSC group, those without ROSC were older (mean age 67.1±16.1 versus 66.0±15.4 years; P<0.001) and more likely to be male (60% versus 56%; P<0.001).
Table 1.
Baseline Characteristics of the Study Participants and Hospital Characteristics in the Entire Sample and by Survival Status
| Entire Sample N=91 658 | No ROSC n=45500 | ROSC n=46 158 | P Value (ROSC vs No ROSC) | |
|---|---|---|---|---|
| Patient‐level characteristics | ||||
| CPR duration in minutes, median (IQR) | 17 (18) | 21 (17) | 12 (15) | <0.001 |
| Male sex, n (%) | 53 049 (58) | 27 136 (60) | 25 913 (56) | <0.001 |
| Age in years, mean±SD | 66.5±15.8 | 67.1±16.1 | 66.0±15.4 | <0.001 |
| Black race, n (%) | 18 496 (20) | 9649 (21) | 8847 (19) | <0.001 |
| Pre‐existing diagnoses, n (%) | ||||
| Neurological | 20 680 (23) | 10 377 (23) | 10 303 (22) | 0.08 |
| Cardiac | 55 503 (61) | 26 455 (58) | 29 048 (63) | <0.001 |
| Pulmonary | 45 232 (49) | 22 210 (49) | 23 022 (50) | 0.001 |
| Renal | 32 741 (36) | 15 642 (34) | 17 099 (37) | <0.001 |
| Metastatic or hematologic malignancy | 12 367 (13) | 6809 (15) | 5558 (12) | <0.001 |
| Prior cardiac arrest | 1895 (2) | 747 (2) | 1148 (2) | <0.001 |
| Arrest location, n (%) | ||||
| ICU | 53 546 (58) | 25 672 (56) | 27 874 (60) | <0.001 |
| Monitored | 19 382 (21) | 9225 (20) | 10 157 (22) | |
| Unmonitored | 18 730 (20) | 10 603 (23) | 8127 (18) | |
| Initial rhythm, n (%) | ||||
| VT/VF | 17 551 (19) | 6585 (14) | 10 966 (24) | <0.001 |
| PEA | 39 580 (43) | 19 516 (43) | 20 064 (43) | |
| Asystole | 34 527 (38) | 19 399 (43) | 15 128 (33) | |
| Weekend, n (%) | 29 633 (32) | 15 200 (33) | 14 433 (31) | <0.001 |
| Night, n (%) | 32 448 (35) | 17 298 (38) | 15 150 (33) | <0.001 |
| Witnessed arrest, n (%) | 72 688 (79) | 34 595 (76) | 38 093 (83) | <0.001 |
| Interventions present at time of arrest, n (%) | ||||
| Mechanical/assisted ventilation | 28 776 (31) | 14 508 (32) | 14 268 (31) | 0.002 |
| Invasive airway | 28 609 (31) | 14 233 (31) | 14 376 (31) | 0.66 |
| Need to place an airway at time of arrest | 48 386 (53) | 24 367 (54) | 24 019 (52) | <0.001 |
| Cause of event, n (%) | ||||
| Cardiac | 57 569 (63) | 27 455 (60) | 30 114 (65) | <0.001 |
| Respiratory | 38 383 (42) | 18 986 (42) | 19 397 (42) | 0.36 |
| Neurological | 871 (1) | 386 (1) | 485 (1) | 0.002 |
| Systemic/metabolic | 41 486 (45) | 21 083 (46) | 20 403 (44) | <0.001 |
| Hospital‐level characteristics | ||||
| Academic hospital, no. of events (%) | 60 409 (66) | 29 194 (64) | 31 215 (68) | <0.001 |
| Urban hospital, no. of events (%) | 86 346(94) | 42 614 (94) | 43 732 (95) | <0.001 |
| For‐profit hospital, no. of events (%) | 10 484 (11) | 5431 (12) | 5053 (11) | <0.001 |
| High CPR volume*, no. of events (%) | 79 985 (87) | 39 016 (86) | 41 969 (89) | <0.001 |
| Hospital size, no. of events (%) | ||||
| Small (<250 beds) | 19 243 (21) | 10 473 (23) | 8770 (19) | <0.001 |
| Medium (250 to 499 beds) | 39 454 (43) | 19 686 (43) | 19 768 (43) | |
| Large (≥500 beds) | 32 961 (36) | 15 341 (34) | 17 620 (38) | |
| Hospital location, no. of events (%) | ||||
| Atlantic | 37 816 (41) | 19 489 (43) | 18 327 (40) | <0.001 |
| North central | 22 037 (24) | 10 501 (23) | 11 536 (25) | |
| South central | 16 898 (18) | 8373 (18) | 8525 (18) | |
| Mountain–Pacific | 14 907 (16) | 7137 (16) | 7770 (17) | |
CPR indicates cardiopulmonary resuscitation; ICU, intensive care unit; IQR, interquartile range; PEA, pulseless electrical activity; ROSC, return of spontaneous circulation; VT/VF, ventricular tachycardia/fibrillation.
High CPR volume defined as cardiopulmonary arrest volume greater than median volume for the entire sample.
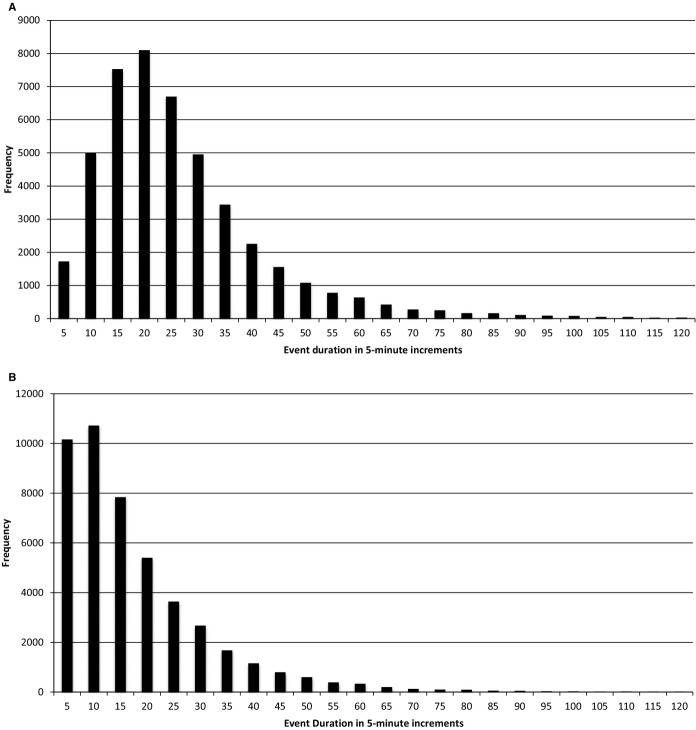
Attempted CPR duration was highly variable, and the distribution was right‐skewed in both groups (Figure 2). The median CPR duration in those who did not experience ROSC was 21 minutes (interquartile range: 17 minutes) compared with a median duration of 12 minutes (interquartile range: 15 minutes) for those who experienced ROSC. The tertiles of CPR duration were 2 to 7, 8 to 17, and 18 to 120 minutes for the ROSC group and 2 to 16 minutes, 17 to 26 minutes, and 27 to 120 minutes for the no‐ROSC group.
Figure 2.
Distribution of cardiopulmonary resuscitation duration. The y‐axis represents the frequency of occurrences, and the x‐axis represents the median duration of the resuscitation event. A, Patients who did not experience ROSC after IHCA. B, Patients who experienced ROSC after IHCA. IHCA indicates in‐hospital cardiac arrest; ROSC, return of spontaneous circulation.
Primary analyses were limited to those without ROSC. This group was predominantly male (60%, n=27 136), and 21% were black (n=9649). The most common pre‐existing conditions at the time of the arrest were cardiac (58%, n=26 455) and pulmonary (49%; n=22 210), with fewer patients having neurological (23%; n=10 377) or renal (34%; n=15 642) diagnoses. The most common initial rhythms were pulseless electrical activity (43%; n=19 516) and asystole (43%; n=19 399). Most events (76%; n=34 595) were witnessed, and 33% (n=15 200) occurred on the weekend. The most common etiology of arrest was a cardiac cause in 60% (n=27 455). The majority of events occurred at academic (64%; n=29 194) and urban (94%; n=42 614) hospitals.
Association of Factors With CPR Duration in Patients With No ROSC
Patient‐level factors
In multivariable analyses (Table 2), female sex (odds ratio [OR] 1.05; 95% CI 1.02 to 1.09; P=0.005) and younger age (aged 18 to 40 versus >65 years; OR 1.81; 95% CI 1.69 to 1.95; P<0.001) were associated with longer CPR duration. There was no association between black race and CPR duration (OR 0.99; 95% CI 0.95 to 1.03; P=0.61). Events with ventricular tachycardia or fibrillation as the presenting rhythm (OR 1.50; 95% CI 1.42 to 1.58; P<0.001), events that occurred in an intensive care unit (OR 1.24; 95% CI 1.17 to 1.31; P<0.001), witnessed events (OR 1.25; 95% CI 1.20 to 1.32; P<0.001), and events that occurred at night (OR 1.05; 95% CI 1.01 to 1.09; P=0.007) were associated with longer CPR duration. The need to place an invasive airway (OR 2.59; 95% CI 2.46 to 2.74; P<0.001) was also associated with longer CPR duration. Pre‐existing renal disease (OR 0.94; 95% CI 0.91 to 0.98; P=0.002), pulmonary disease (OR 0.95; 95% CI 0.91 to 0.98; P=0.005), neurological disease (OR 0.82; 95% CI 0.79 to 0.86; P<0.001), and metastatic or hematologic malignancy (OR 0.79; 95% CI 0.75 to 0.82; P<0.001) were associated with shorter CPR duration. Results were not substantively different when events <2 minutes in duration were included in the sample, with the exception of a strengthened association between the need to place an invasive airway and CPR duration (analyses excluding events <2 minutes: OR 2.59; 95% CI 2.46 to 2.72; P<0.001; analyses including events <2 minutes: OR 2.97; 95% CI 2.83 to 3.13; P<0.001) and the presence of an association between high hospital CPR volume and CPR duration (analyses excluding events <2 minutes: OR 1.01; 95% CI 0.95 to 1.06; P=0.82; analyses including events <2 minutes: OR 1.02; 95% CI 1.02 to 1.03; P<0.001).
Table 2.
The Association of Patient and Hospital Level Factors With CPR Duration
| No ROSC | ROSC | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P Value | OR | 95% CI | P Value | |
| Patient factors | ||||||
| Female sex | 1.05 | 1.02 to 1.09 | 0.005 | 0.97 | 0.94 to 1.01 | 0.11 |
| Age | ||||||
| ≤40 years | 1.81 | 1.69 to 1.95 | <0.001 | 1.00 | 0.93 to 1.07 | 0.93 |
| 40 to 65 years | 1.40 | 1.35 to 1.45 | <0.001 | 1.01 | 0.98 to 1.05 | 0.49 |
| >65 years | Referent | Referent | Referent | Referent | Referent | Referent |
| Black race | 0.99 | 0.95 to 1.03 | 0.61 | 0.99 | 0.95 to 1.03 | 0.61 |
| Pre‐existing comorbidities | ||||||
| Neurological | 0.82 | 0.79 to 0.86 | <0.001 | 0.89 | 0.85 to 0.92 | <0.001 |
| Cardiac | 1.14 | 1.10 to 1.19 | <0.001 | 1.00 | 0.96 to 1.04 | 0.85 |
| Pulmonary | 0.95 | 0.91 to 0.98 | 0.005 | 0.98 | 0.94 to 1.02 | 0.25 |
| Renal | 0.94 | 0.91 to 0.98 | 0.002 | 1.02 | 0.98 to 1.05 | 0.38 |
| Metastatic or hematologic malignancy | 0.79 | 0.75 to 0.82 | <0.001 | 0.98 | 0.92 to 1.03 | 0.33 |
| Prior cardiac arrest | 1.10 | 0.96 to 1.27 | 0.15 | 1.06 | 0.95 to 1.18 | 0.31 |
| Arrest location | ||||||
| ICU | 1.24 | 1.17 to 1.31 | <0.001 | 0.74 | 0.70 to 0.78 | <0.001 |
| Monitored | 1.22 | 1.16 to 1.29 | <0.001 | 0.85 | 0.85 to 0.96 | <0.001 |
| Unmonitored | Referent | Referent | Referent | Referent | Referent | Referent |
| Initial rhythm | ||||||
| VT/VF | 1.50 | 1.42 to 1.58 | <0.001 | 0.89 | 0.85 to 0.93 | <0.001 |
| PEA | 1.45 | 1.40 to 1.51 | <0.001 | 0.80 | 0.76 to 0.83 | <0.001 |
| Asystole | Referent | Referent | Referent | Referent | Referent | Referent |
| Weekend | 0.99 | 0.96 to 1.04 | 0.97 | 1.03 | 0.99 to 1.07 | 0.11 |
| Night | 1.05 | 1.01 to 1.09 | 0.007 | 1.08 | 1.04 to 1.12 | <0.001 |
| Witnessed arrest | 1.25 | 1.20 to 1.32 | <0.001 | 0.87 | 0.82 to 0.91 | <0.001 |
| Cause of event | ||||||
| Cardiac | 1.09 | 1.05 to 1.13 | <0.001 | 0.98 | 0.94 to 1.02 | 0.28 |
| Respiratory | 1.08 | 1.04 to 1.12 | <0.001 | 0.96 | 0.93 to 1.00 | 0.04 |
| Neurologic | 1.07 | 0.88 to 1.28 | 0.51 | 0.89 | 0.75 to 1.05 | 0.18 |
| Systemic/metabolic | 0.97 | 0.93 to 1.00 | 0.09 | 1.24 | 1.20 to 1.29 | <0.001 |
| Interventions at time of arrest | ||||||
| Assisted ventilation | 1.01 | 0.95 to 1.08 | 0.69 | 1.14 | 1.08 to 1.21 | <0.001 |
| Invasive airway | 1.15 | 1.08 to 1.22 | <0.001 | 1.23 | 1.16 to 1.30 | <0.001 |
| Need to place an invasive airway | 2.59 | 2.46 to 2.72 | <0.001 | 2.64 | 2.51 to 2.76 | <0.001 |
| Hospital factors | ||||||
| Academic hospital | 1.36 | 1.30 to 1.41 | <0.001 | 1.07 | 1.03 to 1.12 | 0.001 |
| Urban hospital | 1.20 | 1.12 to 1.30 | <0.001 | 1.10 | 1.02 to 1.20 | 0.01 |
| For‐profit hospital | 0.93 | 0.88 to 0.98 | 0.01 | 0.95 | 0.90 to 1.01 | 0.07 |
| High CPR volume | 1.01 | 0.95 to 1.06 | 0.82 | 0.81 | 0.77 to 0.86 | <0.001 |
| Geographic location | ||||||
| Atlantic | 1.36 | 1.30 to 1.41 | 0.19 | 1.12 | 1.07 to 1.18 | 0.001 |
| North central | 1.12 | 1.06 to 1.18 | <0.001 | 1.04 | 0.99 to 1.10 | 0.13 |
| South central | 1.23 | 1.16 to 1.31 | <0.001 | 1.13 | 1.07 to 1.20 | <0.001 |
| Mountain–Pacific | Referent | Referent | Referent | Referent | Referent | Referent |
| Hospital size | ||||||
| <250 beds | Referent | Referent | Referent | Referent | Referent | Referent |
| 250 to 499 beds | 1.02 | 0.97 to 1.07 | 0.48 | 0.92 | 0.88 to 0.97 | 0.001 |
| ≥500 beds | 1.06 | 1.00 to 1.11 | 0.04 | 0.92 | 0.88 to 0.98 | 0.004 |
CPR indicates cardiopulmonary resuscitation; ICU, intensive care unit; OR, odds ratio; PEA, pulseless electrical activity; ROSC, return of spontaneous circulation; VT/VF, ventricular tachycardia/fibrillation.
Hospital‐level factors and CPR duration
Academic hospital status was associated with longer CPR duration (OR 1.36; 95% CI 1.30 to 1.41; P<0.001), as was urban location (OR 1.20; 95% CI 1.12 to 1.30; P<0.001). There was no association between higher IHCA volume (OR 1.01; 95% CI 0.95 to 1.06; P=0.82) and CPR duration.
Association of Factors With CPR Duration in Those Who Experienced ROSC
Patient‐level factors
In a secondary analysis, we examined the association of patient‐level factors and CPR duration in the group that experienced ROSC. There was no association between sex (OR 0.97; 95% CI 0.94 to 1.01; P=0.11), age (aged ≤40 versus age >65 years; OR 1.00; 95% CI 0.93 to 1.07; P=0.93), or black race (OR 0.99; 95% CI 0.95 to 1.03; P=0.61) and CPR duration (Table 2). Overnight events were associated with longer CPR duration (OR 1.08; 95% CI 1.04 to 1.12; P<0.001). Either the presence of assisted ventilation or an invasive airway at the time of the arrest (assisted ventilation: OR 1.14, 95% CI 1.08 to 1.21; P<0.001; invasive airway: OR 1.23; 95% CI 1.16 to 1.30; P<0.001) or the need to place an invasive airway at the time of the event (OR 2.64; 95% CI 2.51 to 2.76; P<0.001) were also associated with longer CPR duration. Compared with asystole, ventricular tachycardia or fibrillation (OR 0.89; 95% CI 0.85 to 0.93; P<0.001) and pulseless electrical activity (OR 0.80; 95% CI 0.76 to 0.83; P<0.001) were associated with shorter CPR duration, as were events that occurred in the intensive care unit (OR 0.74; 95% CI 0.70 to 0.78; P<0.001) and witnessed events (OR 0.87; 95% CI 0.82 to 0.91; P<0.001).
Hospital‐level factors
Both academic hospital status and urban location were associated with longer CPR duration (academic hospital: OR 1.07; 95% CI 1.03 to 1.12; P=0.001; urban location: OR 1.10; 95% CI 1.02 to 1.20; P=0.01). Higher IHCA volume was associated with shorter CPR duration (OR 0.81; 95% CI 0.77 to 0.86; P<0.001).
Contribution of Factors to CPR Duration
In patients who did not experience ROSC, the intraclass correlation coefficient was 0.03. In those with ROSC, the intraclass correlation coefficient was 0.07. Moreover, 3.29% of the variance in CPR duration was related to hospital‐level factors in victims of IHCA who did not experience ROSC versus 7.28% in those with ROSC. The remainder of the variance in CPR duration was related to differences among patients, independent of facility. The c statistic for the model, including both patient‐ and hospital‐level factors, was 0.64 in those without ROSC and 0.63 in the ROSC group.
Discussion
We examined factors associated with CPR duration in this large, registry‐based sample of >91 000 victims of cardiopulmonary arrest. Our findings are 3‐fold. First, CPR duration was highly variable. Second, in patients who did not experience ROSC after IHCA, this variability was explained in part by patient factors such as age and sex but was not associated with race. Third, hospital factors, such as academic status, hospital size, and urban location, were associated with resuscitation duration but explained only a small proportion of the variance in CPR duration seen in this study.
A fundamental difference between victims of IHCA with and without ROSC is that when the patient demonstrates ROSC, the decision to stop CPR is made because it was successful and is no longer needed. In victims of IHCA who never develop ROSC, a decision must be made at some point to terminate unsuccessful resuscitation efforts. The timing of this decision is often ambiguous. Because the goal of this paper was to identify factors associated with CPR duration in patients in whom a decision to terminate CPR was made, the primary analyses were focused on patients without ROSC after IHCA. We performed secondary analyses in patients with ROSC to assess important differences in predictors of CPR duration between these 2 groups. To our knowledge, this study is the first to directly assess patient‐ and hospital‐level determinants of CPR duration in a large sample of hospitalized patients. Because recent research by other authors has shown an association between longer duration of resuscitation and survival, these findings may have important implications for patient care.
Prior data suggest that prolonged resuscitation is associated with a decreased chance of survival22–25; however, these studies had several important limitations, including small sample size and single‐center study design. In a recent analysis from the GWTG‐R registry, Goldberger et al stratified hospitals by the median duration of resuscitation among nonsurvivors. The authors demonstrated that hospitals with higher median resuscitation times had higher likelihood of ROSC after IHCA and higher probability of survival to discharge.4
These data suggest that the differences in the duration of resuscitation may have implications for patient outcomes. Importantly, health care providers may not be well prepared to make decisions about when to terminate resuscitation. Physicians at all levels of training perform poorly when asked to assess the probability of survival after IHCA. Jones et al found that <50% of medical students, residents, and attending physicians were able to accurately assess the probability of survival after an IHCA.26 Patients and families may also overestimate the probability of survival after an arrest.27 This difficulty in prognostication, combined with the lack of reliable indicators about when to terminate CPR, suggests that health care providers may have difficulty making an informed decision about when to end resuscitation.
We found that younger age and female sex were associated with longer duration of resuscitation in those who did not experience ROSC after cardiac arrest. It is possible that this finding is related to a perception among health care providers that these groups have a higher probability of survival and therefore merit a longer trial of CPR. Previous data examining the association of sex with outcome after cardiac arrest are conflicting,28–30 but some authors have found that sex may be a factor in the decision to perform CPR.18 Our finding that age is associated with CPR duration is supported by the results of an analysis by Fried et al, who studied 122 patients after IHCA at a single center. In this study, the authors found that both older age and dependent functional status were associated with a shorter trial of CPR.17 Our data, taken in aggregate with this previous work, suggest that CPR duration may contribute to differences in outcome based on sex and age and should be taken into account in future work examining sex and outcome after cardiac arrest.
Several other factors were associated with CPR duration in our primary analyses. Witnessed cardiopulmonary arrests, which have been associated with a higher probability of survival in other studies, were associated with longer resuscitation times.7 CPR duration may be longer in patients who did not experience ROSC after witnessed arrest because providers believed that the likelihood of survival is higher after a witnessed arrest. Similarly, ventricular tachycardia or fibrillation, which is associated with a higher probability of survival than other presenting rhythms,31 was associated with longer CPR duration. Nighttime events, which have been associated with a lower probability of survival in the GTWG‐R registry,13 were associated with longer CPR duration in our analyses. This suggests that the poor outcomes observed after nighttime IHCA are not related to differences in CPR duration. Finally, the need to place an invasive airway at the time of the event was associated with longer CPR duration, perhaps because of the time required to complete that process.
Our analyses identified several hospital factors that were associated with CPR duration. Both academic status and urban location of cardiac arrest were associated with longer duration of resuscitation in those both with and without ROSC. This finding may be related to differences in unmeasured patient factors; to process measures, such as the presence or absence of a hospitalwide CPR team32; or to the presence of trainees during resuscitation. Importantly, we found that differences in measured hospital‐level factors were responsible for only 3% of the variability in CPR duration in those without ROSC, a small proportion. This suggests that future interventions to address variability in CPR duration should focus on patient factors and other factors not measured in this analysis such as process measures and provider factors.
In secondary analyses, we examined factors associated with CPR duration in victims of IHCA who experienced ROSC. We found several important differences between these patients and those who did not experience ROSC. In contrast to our findings in those without ROSC, we found no association between age or sex and CPR duration. Furthermore, multiple factors associated with longer CPR duration in those who did not experience ROSC were found to be associated with shorter CPR duration in the ROSC group. These included intensive care unit or monitored location, ventricular tachycardia or fibrillation as the presenting rhythm, and witnessed events. CPR duration may be shorter in patients with ROSC who have these characteristics because of more immediate access to interventions such as chest compressions and defibrillation. Conversely, CPR duration may be longer in those who did not experience ROSC because a higher perceived likelihood of survival encourages health care providers to continue resuscitation. Nighttime events were associated with longer CPR duration in both groups after IHCA, perhaps because of differences in staffing at that time of day.5
Several issues are important to consider when interpreting the results of our study. Strengths of our study include the use of a large, multisite registry with comprehensive adjudication of cases of cardiac arrest. Our study encompassed a diverse cohort from a variety of hospitals of varying sizes and locations. Detailed patient information, including pre‐existing comorbidities and clinical outcomes, were available as part of this study. However, there are inherent limitations to retrospective, registry‐based analyses of cardiopulmonary arrests. We are unable to assess decision making at the time of the arrest. Importantly, we cannot determine how much information, such as age or pre‐existing comorbidities, was available to health care providers at the time of the event. We are unable to determine the mechanism of association between factors identified in this study and CPR duration. Family members' wishes may also have affected CPR duration and were not measured by this study. Patient characteristics were obtained by retrospective chart review, and it is possible that not all data were captured or that misclassification of data occurred. Our ability to assess hospital characteristics was limited, and it is possible that relevant differences were missed. Importantly, we could not assess the presence of hospitalwide code blue teams, which may improve outcomes and minimize disparities in IHCA outcomes.33 Information about physician characteristics, such as specialty and years in practice, was not available for analysis. We examined data from cardiac arrests that occurred between 2001 and 2010. There may have been changes in systemic or patient factors over this period of time that were unmeasured in the current analysis. Although the large sample size is a strength of the study, it also increases the likelihood of statistically significant findings regardless of the clinical significance. Finally, many of the ORs observed in this study were close to 1, demonstrating that the impact of each individual factor on CPR duration was small, and the calculated c statistics are consistent with models that are only modestly predictive. This suggests that a significant amount of the variability in CPR duration is not accounted for by our model in either those with or without ROSC after IHCA.
Conclusion
CPR duration is highly variable and is associated with multiple factors. Understanding the mechanism of these interactions may help explain variability in IHCA outcomes.
Appendix
American Heart Association Get With the Guidelines‐Resuscitation (GWTG‐R) Investigators
Robert A. Berg, Graham Nichol, Vinay M. Nadkarni (study author), Mary Ann Peberdy, Paul S. Chan, Tim Mader, Karl B. Kern, Sam Warren, Emilie Allen, Brian Eigel, Elizabeth A. Hunt, Joseph P. Ornato, Scott Braithwaite, Romergryko G. Geocadin, Mary E. Mancini, Jerry Potts, Tanya Lane Truitt.
Sources of Funding
NIH, K23 Grant 10714038 (Merchant). None of the above funding sources were involved in the design or conduct of the study, collection, management, analysis, or interpretation of the data, or preparation, review, or approval of the manuscript.
Disclosures
Dr Groeneveld: US Government federal employee. Dr Nadkarni: No conflicts of interest to disclose: Grant/Research support not related to this manuscript: NIH UO1 THAPCA: Therapeutic Hypothermia After Pediatric Cardiac Arrest; NIH UO1 HALF‐PINT: Heart and Lung Failure‐Pediatric Insulin Titration Trial; Laerdal Foundation for Acute Care Medicine; Laerdal Medical Inc; AHRQ. Dr Merchant: Grant/Research support: NIH, K23 Grant 10714038, Pilot funding: Physio‐Control Seattle, Washington; Zoll Medical, Boston MA; Cardiac Science, Bothell, Washington; Philips Medical Seattle, Washington. The other authors have no conflicts to disclose.
Acknowledgments
We wish to thank Amy Praestgaard, MS for her assistance with data analysis.
References
- 1.Merchant RM, Yang L, Becker LB, Berg RA, Nadkarni V, Nichol G, Carr BG, Mitra N, Bradley SM, Abella BS, Groeneveld PW. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011; 39:2401-2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ebell MH, Afonso AM. Pre‐arrest predictors of failure to survive after in‐hospital cardiopulmonary resuscitation: a meta‐analysis. Fam Pract. 2011; 28:505-515. [DOI] [PubMed] [Google Scholar]
- 3.Field JM, Hazinski MF, Sayre MR, Chameides L, Schexnayder SM, Hemphill R, Samson RA, Kattwinkel J, Berg RA, Bhanji F, Cave DM, Jauch EC, Kudenchuk PJ, Neumar RW, Peberdy MA, Perlman JM, Sinz E, Travers AH, Berg MD, Billi JE, Eigel B, Hickey RW, Kleinman ME, Link MS, Morrison LJ, O'Connor RE, Shuster M, Callaway CW, Cucchiara B, Ferguson JD, Rea TD, Vanden Hoek TL. Part 1: executive summary: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010; 122:S640-S656. [DOI] [PubMed] [Google Scholar]
- 4.Goldberger ZD, Chan PS, Berg RA, Kronick SL, Cooke CR, Lu M, Banerjee M, Hayward RA, Krumholz HM, Nallamothu BK. Duration of resuscitation efforts and survival after in‐hospital cardiac arrest: an observational study. Lancet. 2012; 380:1473-1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed time to defibrillation after in‐hospital cardiac arrest. N Engl J Med. 2008; 358:9-17. [DOI] [PubMed] [Google Scholar]
- 6.Chan PS, Nichol G, Krumholz HM, Spertus JA, Jones PG, Peterson ED, Rathore SS, Nallamothu BK. Racial differences in survival after in‐hospital cardiac arrest. JAMA. 2009; 302:1195-1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brady WJ, Gurka KK, Mehring B, Peberdy MA, O'Connor RE. In‐hospital cardiac arrest: impact of monitoring and witnessed event on patient survival and neurologic status at hospital discharge. Resuscitation. 2011; 82:845-852. [DOI] [PubMed] [Google Scholar]
- 8.Brindley PG, Markland DM, Mayers I, Kutsogiannis DJ. Predictors of survival following in‐hospital adult cardiopulmonary resuscitation. CMAJ. 2002; 167:343-348. [PMC free article] [PubMed] [Google Scholar]
- 9.Martinell L, Larsson M, Bang A, Karlsson T, Lindqvist J, Thoren AB, Herlitz J. Survival in out‐of‐hospital cardiac arrest before and after use of advanced postresuscitation care: a survey focusing on incidence, patient characteristics, survival, and estimated cerebral function after postresuscitation care. Am J Emerg Med. 2010; 28:543-551. [DOI] [PubMed] [Google Scholar]
- 10.Fredriksson M, Aune S, Bang A, Thoren AB, Lindqvist J, Karlsson T, Herlitz J. Cardiac arrest outside and inside hospital in a community: mechanisms behind the differences in outcome and outcome in relation to time of arrest. Am Heart J. 2010; 159:749-756. [DOI] [PubMed] [Google Scholar]
- 11.Larkin GL, Copes WS, Nathanson BH, Kaye W. Pre‐resuscitation factors associated with mortality in 49,130 cases of in‐hospital cardiac arrest: a report from the National Registry for Cardiopulmonary Resuscitation. Resuscitation. 2010; 81:302-311. [DOI] [PubMed] [Google Scholar]
- 12.Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, Nichol G, Lane‐Truitt T, Potts J, Ornato JP, Berg RA. First documented rhythm and clinical outcome from in‐hospital cardiac arrest among children and adults. JAMA. 2006; 295:50-57. [DOI] [PubMed] [Google Scholar]
- 13.Peberdy MA, Ornato JP, Larkin GL, Braithwaite RS, Kashner TM, Carey SM, Meaney PA, Cen L, Nadkarni VM, Praestgaard AH, Berg RA. Survival from in‐hospital cardiac arrest during nights and weekends. JAMA. 2008; 299:785-792. [DOI] [PubMed] [Google Scholar]
- 14.Skrifvars MB, Castren M, Nurmi J, Thoren AB, Aune S, Herlitz J. Do patient characteristics or factors at resuscitation influence long‐term outcome in patients surviving to be discharged following in‐hospital cardiac arrest? J Intern Med. 2007; 262:488-495. [DOI] [PubMed] [Google Scholar]
- 15.Skrifvars MB, Castren M, Aune S, Thoren AB, Nurmi J, Herlitz J. Variability in survival after in‐hospital cardiac arrest depending on the hospital level of care. Resuscitation. 2007; 73:73-81. [DOI] [PubMed] [Google Scholar]
- 16.Chan PS, Spertus JA, Krumholz HM, Berg RA, Li Y, Sasson C, Nallamothu BKGet With The Guidelines‐Resuscitation Registry Investigators FT. A validated prediction tool for initial survivors of in‐hospital cardiac arrest. Arch Intern Med. 2012; 172:947-953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fried TR, Miller MA, Stein MD, Wachtel TJ. The association between age of hospitalized patients and the delivery of advanced cardiac life support. J Gen Intern Med. 1996; 11:257-261. [DOI] [PubMed] [Google Scholar]
- 18.Goodlin SJ, Zhong Z, Lynn J, Teno JM, Fago JP, Desbiens N, Connors AF, Jr, Wenger NS, Phillips RS. Factors associated with use of cardiopulmonary resuscitation in seriously ill hospitalized adults. JAMA. 1999; 282:2333-2339. [DOI] [PubMed] [Google Scholar]
- 19.Skrifvars MB, Rosenberg PH, Finne P, Halonen S, Hautamaki R, Kuosa R, Niemela H, Castren M. Evaluation of the in‐hospital Utstein template in cardiopulmonary resuscitation in secondary hospitals. Resuscitation. 2003; 56:275-282. [DOI] [PubMed] [Google Scholar]
- 20.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, Berg RA, Nichol G, Lane‐Trultt T. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003; 58:297-308. [DOI] [PubMed] [Google Scholar]
- 21.Fullerton AS. A conceptual framework for ordered logistic regression models. Sociol Methods Res. 2009; 38:306-347. [Google Scholar]
- 22.Ballew KA, Philbrick JT, Caven DE, Schorling JB. Predictors of survival following in‐hospital cardiopulmonary resuscitation. A moving target. Arch Intern Med. 1994; 154:2426-2432. [PubMed] [Google Scholar]
- 23.Bedell SE, Delbanco TL, Cook EF, Epstein FH. Survival after cardiopulmonary resuscitation in the hospital. N Engl J Med. 1983; 309:569-576. [DOI] [PubMed] [Google Scholar]
- 24.Schultz SC, Cullinane DC, Pasquale MD, Magnant C, Evans SR. Predicting in‐hospital mortality during cardiopulmonary resuscitation. Resuscitation. 1996; 33:13-17. [DOI] [PubMed] [Google Scholar]
- 25.Shih CL, Lu TC, Jerng JS, Lin CC, Liu YP, Chen WJ, Lin FY. A web‐based Utstein style registry system of in‐hospital cardiopulmonary resuscitation in Taiwan. Resuscitation. 2007; 72:394-403. [DOI] [PubMed] [Google Scholar]
- 26.Jones K, Garg M, Bali D, Yang R, Compton S. The knowledge and perceptions of medical personnel relating to outcome after cardiac arrest. Resuscitation. 2006; 69:235-239. [DOI] [PubMed] [Google Scholar]
- 27.Jones GK, Brewer KL, Garrison HG. Public expectations of survival following cardiopulmonary resuscitation. Acad Emerg Med. 2000; 7:48-53. [DOI] [PubMed] [Google Scholar]
- 28.Topjian AA, Localio AR, Berg RA, Alessandrini EA, Meaney PA, Pepe PE, Larkin GL, Peberdy MA, Becker LB, Nadkarni VM. Women of child‐bearing age have better inhospital cardiac arrest survival outcomes than do equal‐aged men. Crit Care Med. 2010; 38:1254-1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Herlitz J, Rundqvist S, Bang A, Aune S, Lundstrom G, Ekstrom L, Lindkvist J. Is there a difference between women and men in characteristics and outcome after in hospital cardiac arrest? Resuscitation. 2001; 49:15-23. [DOI] [PubMed] [Google Scholar]
- 30.Fugate JE, Brinjikji W, Mandrekar JN, Cloft HJ, White RD, Wijdicks EF, Rabinstein AA. Post cardiac‐arrest mortality is declining: a study of the U.S. National inpatient sample 2001–2009. Circulation. 2012; 126:546-550. [DOI] [PubMed] [Google Scholar]
- 31.Meaney PA, Nadkarni VM, Kern KB, Indik JH, Halperin HR, Berg RA. Rhythms and outcomes of adult in‐hospital cardiac arrest. Crit Care Med. 2010; 38:101-108. [DOI] [PubMed] [Google Scholar]
- 32.Chan PS, Khalid A, Longmore LS, Berg RA, Kosiborod M, Spertus JA. Hospital‐wide code rates and mortality before and after implementation of a rapid response team. JAMA. 2008; 300:2506-2513. [DOI] [PubMed] [Google Scholar]
- 33.Qureshi SA, Ahern T, O'Shea R, Hatch L, Henderson SO. A standardized Code Blue Team eliminates variable survival from in‐hospital cardiac arrest. J Emerg Med. 2012; 42:74-78. [DOI] [PubMed] [Google Scholar]