Introduction
Fibromuscular dysplasia (FMD) is a nonatherosclerotic disease of medium‐sized vessels that can present with arterial stenosis, beading, dissection, and aneurysm. While the most common sites of FMD are the renal and extracranial carotid and vertebral arteries, FMD has been reported in most arterial segments.1 FMD does not affect the venous system. During the past decade, there has been a resurgence of research in understanding this uncommon and often misunderstood disease. Here, we highlight new developments in FMD research and clinical care, including a recently published multidisciplinary statement from the American Heart Association, a European Consensus document on FMD, and new insights regarding this disease derived from findings of the French and United States Registry for Fibromuscular Dysplasia (US Registry).1–3
Pattern of Vascular Involvement and Clinical Presentation
Until recently, renal FMD, generally presenting as early‐onset or difficult to control hypertension, was thought to account for the majority of cases, while cerebrovascular FMD was thought to account for less than one‐third of cases.4 Data from the US Registry for FMD has led to a paradigm shift. In the registry cohort, nearly 80% of registrants had renal FMD and almost three‐quarters had carotid FMD.2 Vertebral FMD was the third most common site affected (36.6%). Other reported sites of involvement included the mesenteric arteries, iliac arteries, intracranial vessels, and upper extremity (brachial) arteries. Multivessel involvement among patients with FMD is common. In the registry, 65% of patients with renal artery FMD who underwent cerebrovascular imaging had evidence of vertebral or carotid involvement, and 64% of patients with cerebrovascular FMD with renal imaging demonstrated evidence of renal artery FMD.2 Though registry data may be subject to the bias of tertiary care referral centers, cerebrovascular FMD is much more common than previously reported in the literature, and a significant percentage of FMD patients have >1 vascular territory involved. As discussed later, these data have led to an evolution in clinical practice, leading to more comprehensive arterial imaging of at‐risk vascular beds for patients with FMD.
The symptoms and signs of FMD depend on the arteries involved and the severity of the arterial lesions. Table 1 illustrates the frequency of symptoms reported among patients in the US Registry for FMD. Given the observational nature of the registry, however, the FMD‐specific causality of these symptoms, some of which are common clinical complaints, cannot be definitively determined.2 Patients with renal FMD classically present with hypertension but may also present with headache. Flank pain may indicate aneurysm or dissection and infarction of the renal artery (especially if of acute onset) but can also be present among patients with renal FMD without either of these complications. Renal insufficiency is a rare clinical manifestation of FMD in adults (2% of patients in the US Registry).2
Table 1.
Frequency of Presenting Signs and Symptoms of Patients in the US Registry for Fibromuscular Dysplasia
| Presenting Symptoms | n (%) |
|---|---|
| Hypertension | 285 (63.8) |
| Headache | 234 (52.4) |
| Pulsatile tinnitus | 123 (27.5) |
| Dizziness | 116 (26.0) |
| Cervical bruit | 99 (22.2) |
| Neck pain | 99 (22.2) |
| Tinnitus | 84 (18.8) |
| Chest pain or shortness of breath | 72 (16.1) |
| Flank/abdominal pain | 70 (15.7) |
| Aneurysms | 63 (14.1) |
| Cervical artery dissection | 54 (12.1) |
| Epigastric bruit | 42 (9.4) |
| Hemispheric TIA | 39 (8.7) |
| Postprandial abdominal pain | 35 (7.8) |
| Stroke | 31 (6.9) |
| Claudication | 23 (5.2) |
| Amaurosis fugax | 23 (5.2) |
| Weight loss | 23 (5.2) |
| Horner syndrome | 21 (4.7) |
| Renal artery dissection | 14 (3.1) |
| Azotemia | 9 (2) |
| Myocardial infarction | 8 (1.8) |
| Mesenteric ischemia | 6 (1.3) |
| No symptoms or signs | 25 (5.6) |
Reprinted with permission from Olin et al.2 TIA indicates transient ischemic attack.
Patients with carotid and/or vertebral FMD can present with diverse symptoms ranging from headache, neck pain, and pulsatile tinnitus to arterial dissection, transient ischemic attack or stroke, or, less commonly, subarachnoid hemorrhage.2 A significant number of patients in the US Registry sustained a neurological event: 13.4% of patients experienced a hemispheric transient ischemic attack, 12.1% suffered a cervical artery dissection, and 9.8% had a stroke. The combined frequency of carotid, vertebral, cerebral, and basilar artery aneurysms was ≈7%; however, the frequency of subarachnoid hemorrhage was very low (1.1%).2 Pulsatile tinnitus (a pulsatile swooshing noise in the ear) has recently been recognized as a highly prevalent manifestation of this disease, reported as a presenting symptom of 32% of patients in the US Registry.5 Pulsatile tinnitus is associated with cerebrovascular involvement, cervical artery dissection, and multivessel FMD.5 For many patients, this is a highly annoying symptom that can impair quality of life and contribute to the morbidity of this disease.
There are no consistent diagnostic physical examination findings in FMD. In some patients, cervical, abdominal, or femoral bruit may be the only sign present. However, presence of a bruit over the affected artery is not a sensitive indicator of disease. In the US Registry, 30.5% of registrants presented with a cervical bruit, 17.5% with an epigastric bruit, and 6.1% with flank bruit.2,6 The sensitivity of a cervical bruit for the diagnosis of extracranial carotid and/or vertebral FMD was only 45%, and the sensitivity of an epigastric or flank bruit for the diagnosis of renal and/or mesenteric FMD was only 24%.6 Pulse deficits are uncommon in FMD, and a significant pulse deficit was noted in the dorsalis pedis and/or posterior tibial arteries in only 5% of patients in the US FMD Registry.2 Pulse deficits in the brachial arteries were noted in <1% of patients.2 To summarize, there is no physical examination finding that is adequately sensitive for diagnosis of FMD in a specific vascular bed. Because of this, comprehensive vascular imaging is required in the evaluation of FMD patients.
Evolving Nomenclature
Historically, FMD has been classified histopathologically into categories based on the dominant arterial layer involved (media, intima, or adventitia) and the composition of the arterial lesion (collagen deposition, known as fibroplasia, or, less commonly, hyperplasia of smooth muscle cells).7–9 Harrison, McCormack, and colleagues correlated pathological classification to angiographic findings.7–9 Medial fibroplasia presents as the classic “string of beads” on angiography. Intimal and adventitial fibroplasia commonly present as tubular or focal stenosis. Classifying FMD based on histopathologic findings has become increasingly difficult. In this era of advanced imaging and endovascular procedures, few patients have pathological specimens available for examination. The 2012 European Consensus proposed a simplified angiographic classification system of multifocal, tubular, and unifocal FMD.10 Savard and colleagues demonstrated that a binary (multifocal versus unifocal) classification system for renal FMD lesions can practically distinguish between 2 distinct clinical phenotypes.11 Patients with focal renal lesions were younger (30 years versus 49 years at diagnosis of FMD) with higher blood pressure at presentation, more frequently smokers (50% versus 26%), and more likely to be male (31% versus 17%), all P<0.02.11 The recently published AHA Scientific Statement proposed a classification of FMD that distinguishes patients with multifocal (beading) FMD from patients with focal lesions (Table 2 and Figure 1).1 It is hoped that this simplified classification will improve communication between clinicians and researchers and provide a more clinically oriented distinction between FMD subtypes.
Table 2.
2014 American Heart Association Classification of FMD
| Multifocal FMD | Focal FMD | |
|---|---|---|
| Angiographic appearance | Alternating dilatation and constriction of the vessel (string of beads) Areas of dilatation are larger than the normal caliber of the artery Occurs in the mid and distal portion of the renal, internal carotid, and vertebral arteries May occur in any other artery in the body* |
Focal concentric or tubular stenosis* |
| Typical histology | Medial fibroplasia (most common) Perimedial fibroplasia (rare)* |
Intimal fibroplasia (most common) Adventitial (periarterial) fibroplasia (rare) Medial hyperplasia (rare) |
| Associated features | Aneurysm, dissection, and vessel tortuosity of medium‐sized arteries may be present; multifocal and focal lesions may coexist in the same patient |
Reprinted with permission from Olin et al.1 FMD indicates fibromuscular dysplasia.
Lesions are not necessarily confined to the mid or distal portion of the artery (ie, can occur in any arterial segment).
There are no cases of aortic FMD that are well documented pathologically.
This rare form of FMD typically occurs in young girls (eg, those 5 to 15 years of age). Although there is a beaded appearance to the renal arteries, the beads are smaller than the normal renal artery and less numerous. Histologically, collagen deposition is localized to the outer portion of the medial layer.
Figure 1.
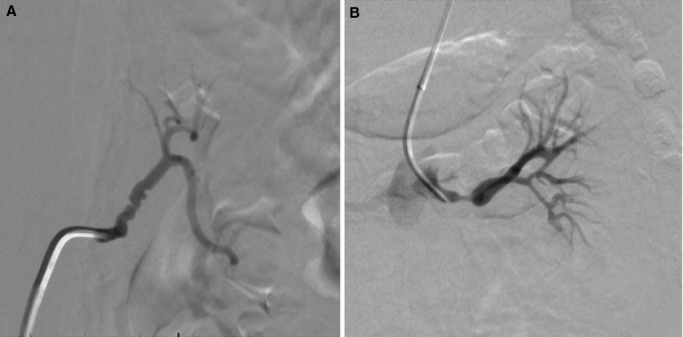
Angiographic images of multifocal (A) and focal (B) lesions in the renal artery.
Epidemiology
FMD has historically been considered a rare disease and has been recognized by the National Organization for Rare Diseases as such, a designation that requires an estimated prevalence of <200 000 US residents.12 Recent data, however, suggest FMD is more common than previous estimates indicate. A meta‐analysis based on kidney donor data found FMD in ≈4% of the potential kidney donor population.13–16 A recently published single‐center retrospective review of 1940 potential kidney donors (58% female) found evidence of FMD in 3.9% in potential female kidney donors.13 Most of these patients were asymptomatic, as only 2 (3.7%) of 54 patients were started on new or additional antihypertensive agents following the screening.13 Renal donor screening studies may not accurately reflect the prevalence of FMD in the general population, because potential kidney donors tend to have few health issues, such as hypertension or chronic kidney disease (underestimation of prevalence), but may also enrich for familial FMD because most potential kidney donors have a family member with severe chronic kidney disease (overestimation of prevalence).13
As discussed earlier, the US Registry has demonstrated that cerebrovascular FMD is nearly as common as renal FMD, although there are little data available regarding the estimated prevalence of cerebrovascular FMD. A study examining consecutive cerebral angiograms estimated the prevalence of cerebrovascular FMD to be 0.3% to 3.2%,17 but this study was limited to patients undergoing invasive imaging, presumably for symptomatic disease or major risk factors.
The US Registry has highlighted the potential for FMD patients to be entirely asymptomatic. In the registry, 5.6% of patients were diagnosed with FMD based on imaging conducted for another reason and were entirely asymptomatic at the time of diagnosis (including absence of bruits on physical examination).2 Thus, FMD may have a significant prevalence in the general population and likely represents a spectrum of disease with a number of patients having “silent” or minimally symptomatic lesions. Study of the prevalence of FMD has been identified as a top research priority in a recently published AHA Scientific Statement.1 (Table 3).
Table 3.
Top Research Priorities in FMD
|
|
|
|
|
|
|
|
|
|
|
Reprinted with permission from Olin et al.1 FMD indicates fibromuscular dysplasia; TIA, transient ischemic attack.
FMD is primarily a disease of women. In the initial reports of the US Registry, 92% of registrants were female.2,18 Men with FMD have a distinctive clinical presentation as reported in a study by Kim and colleagues based on data from the US Registry. In this analysis, men with FMD were more likely to present with visceral involvement than were women, including flank/abdominal pain, renal insufficiency, and renal infarction (43.8% versus 14.3%, 9.1% versus 2.2%, and 42.9% versus 4.3%, respectively, all P<0.05).18 Women were more likely to present with classic signs and symptoms of extracranial cerebrovascular FMD: pulsatile tinnitus, neck pain, and cervical bruit (all P<0.05). Male FMD patients had a 2‐fold increase in prevalence of arterial aneurysm (40.8% versus 20.4%, P=0.002) and arterial dissection (39.6% versus 20.0%, P=0.0031) compared with female FMD patients.18 Men with FMD are also more likely to have focal disease.11 It appears that FMD may have a more aggressive vascular course and has a predilection for involvement of the renal and mesenteric arteries in men.
Genetics
The genetics of FMD is an active area of research. As of yet, no etiologic genes have been identified. Early genetic data suggested an autosomal dominant inheritance pattern with variable penetrance.19–21 In a series of 20 cases, Rushton classified 60% as familial; however, positive family members were identified based on cardiovascular events and early‐onset hypertension rather than definitive confirmation of FMD on imaging.20 Few studies provide radiographic proof of familial inheritance. Perdu and colleagues studied 13 cases and 47 first‐degree relatives in 6 families screened for FMD using high‐resolution carotid ultrasound.22 High‐resolution echo tracking measurements of carotid arterial wall parameters were used to develop an arterial scoring system. Elevated arterial scores served as a surrogate marker for FMD. Segregation analysis showed 52% of descendants had an elevated arterial score consistent with an autosomal dominant transmission.22 However, no family member demonstrated classic vascular lesions clinically associated with FMD, such as beading or stenosis, and the carotid ultrasound score is not widely accepted as a marker for FMD. Thus, the prevalence of familial FMD is likely overestimated in these studies. In a study with imaging confirmation of FMD diagnosis, 11% of FMD cases were familial.23 All familial cases were siblings, and no vertical transmission was reported.23 In the US Registry, only 7.3% of patients report a confirmed diagnosis of FMD in ≥1 first‐ or second‐degree family members.2 However, the high prevalence of aneurysms (23.5%), sudden death (19.8%), and stroke (53.5%) among first‐ and second‐degree family members in the US Registry suggests FMD may represent an inherited systemic arteriopathy with a diverse clinical phenotype. Larger family studies with vascular imaging are needed to better identify the inheritance pattern of FMD. Understanding the genetic (and biological) determinants of FMD has been identified as another top research priority in the AHA Scientific Statement (Table 3).1
It is hypothesized that FMD may have overlapping features with vascular connective tissue diseases, such as Loeys‐Dietz syndrome or the vascular type of Ehlers‐Danlös syndrome. However, the prevalence of genetic mutations associated with connective tissue disease was negligible in a cohort of clinically confirmed FMD patients who underwent genetic testing.24 Two patients in this cohort were found to have distinct novel point mutations in TGFβ receptor type 1 gene.24 Both of these patients had a history of arterial dissection and had aortic ectasia or aneurysm. Ganesh, Morrisette, and colleagues found elevated secretion of transforming growth factor (TGF)‐β1 and TGF‐β2 by fibroblasts derived from FMD patients compared with matched controls (P=0.0009 and P=0.0001, respectively). FMD patients also had elevated plasma levels of circulating TGF‐β1 and TGF‐β2 relative to matched controls (P=0.009 and P=0.004, respectively).25 The potential involvement of TGF‐β pathways in the pathogenesis of FMD is an area for future investigation, especially as this pathway could provide a potential target for disease‐modifying medical therapies.
Evidence supports that gene–environment interactions influence FMD susceptibility. Smoking and estrogen are 2 proposed interactions.1,26 Savard and colleagues demonstrated that patients with renal FMD have a much higher rate of smoking compared with matched hypertensive controls.26 The striking predilection of female patients in the FMD population (>90%) suggests estrogen and other hormonal factors as major contributors to the development of FMD.
Coronary FMD, Spontaneous Coronary Artery Dissection, and the Spontaneous Coronary Artery Dissection–FMD Paradox
An emerging area of investigation involves coronary manifestations of FMD. Several case reports previously described sudden death associated with the histopathologic finding of FMD of the coronary arteries on autopsy.27–29 Supporting these case reports, Hill and colleagues found histological findings of FMD in 2% of patients with unexplained sudden cardiac death.28 However, Zack and colleagues investigated the incidence of histopathologically confirmed FMD of the nodal arteries in patients who sustained non–cardiac sudden death (eg, accidents, suicides) and found microscopic alterations of the sinus node arteries in 52 of 100 cases, atrioventricular nodal arteries in 63 of 100 cases, and 60 of 100 small vessels consistent with FMD.30 Therefore, it seems likely that histopathologic findings of the nodal arteries mimicking FMD seen in other vascular territories is a potential incidental autopsy finding and is likely disease causing. It is our opinion and those of the authors of the AHA Scientific Statement these pathological findings do not represent the clinical disease process of FMD discussed in this manuscript.1
The association of spontaneous coronary artery dissection (SCAD) with FMD has recently been described (Figure 2). SCAD most commonly presents as biomarker‐positive acute coronary syndrome (non–ST‐segment elevation or ST‐segment elevation myocardial infarction). The most common coronary artery involved is the left anterior descending coronary artery in its mid to distal segment.31–32 In a case series published by Saw and colleagues, 86% (43 of 50) of patients with SCAD had angiographic findings of FMD in the noncoronary vasculature: renal (58.1%), iliac (48.8%), and cerebrovascular (46.5%) arteries. Of the 7 patients not found to have FMD, 5 had not completed screening for all 3 major vascular territories (iliac, renal, cerebrovascular), and 2 were found to be negative after complete screening.31
Figure 2.
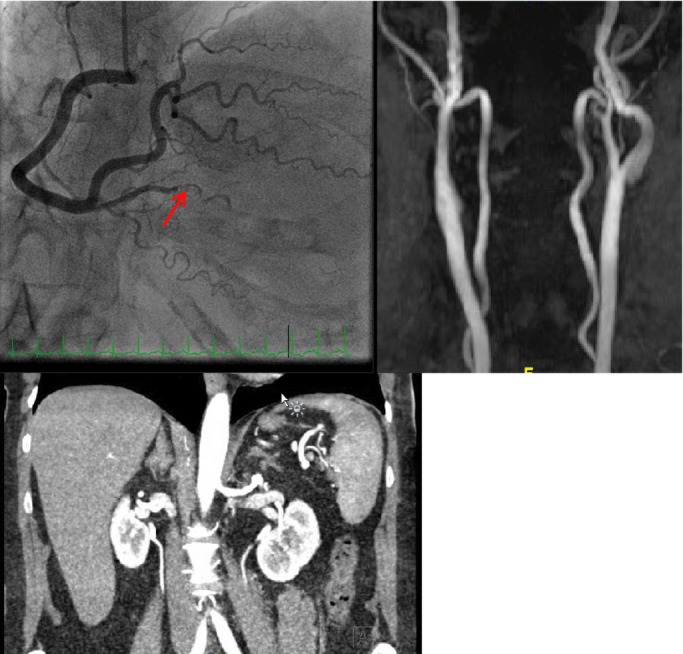
Angiogram of coronary arteries (top left) demonstrating spontaneous coronary artery dissection of the posterior descending artery in a 58‐year‐old woman presenting with non–ST‐segment elevation myocardial infarction. MRA demonstrated bilateral internal carotid artery multifocal FMD (top right), and CTA demonstrated a left renal 6‐mm aneurysm (bottom left) with mild FMD of the right renal artery (bottom left). MRA indicates magnetic resonance angiography; FMD, fibromuscular dysplasia; CTA, computed tomography angiography.
In contrast to the high prevalence of FMD in the Vancouver SCAD cohort, Toggweiler and colleagues found evidence of renal artery abnormalities in only 3 of 12 patients with SCAD who underwent head‐to‐pelvis imaging.33 Two patients had multifocal FMD and 1 patient had a spontaneous renal artery dissection. However, patients in this series underwent magnetic resonance angiography (MRA) imaging, which has decreased sensitivity for diagnosis of mild FMD lesions compared with catheter‐based angiography.
In the Mayo Clinic SCAD cohort of 87 patients, 9% of patients with SCAD had an incidental finding of iliac (n=8) FMD seen on femoral angiograms taken before catheter removal.34 Based on the growing association between SCAD and FMD, a specialized computed tomography angiography (CTA) protocol of the neck, chest, abdomen, and pelvis was developed for assessment for FMD and other vascular findings, including arterial aneurysm or dissection at this institution.35 In this study, 69% of patients with SCAD had extracoronary vascular abnormalities, the majority of which were consistent with FMD.35
Despite the significant prevalence of FMD among patients with SCAD, it is important to note that SCAD and acute coronary syndrome seem to be an uncommon events among all comers with a diagnosis of FMD. Indeed, there seems to be an SCAD–FMD paradox: while 25% to 86% of SCAD patients in the largest published case series have imaging evidence of FMD,31,33,35–36 in the US Registry, any significant coronary artery disease (including atherosclerotic disease) was reported in only 6.5% of patients, and only 3.1% of patients in the US Registry had a history of myocardial infarction.2 To summarize, SCAD seems to be the primary coronary artery manifestation of FMD, and unlike other vascular beds, coronary FMD infrequently presents as a “string of beads.”37 While underlying FMD is common among patients who have sustained an SCAD event, only a small percentage of patients with FMD develop coronary events during follow‐up. Future research efforts are needed to determine the predictors of SCAD among FMD patients and to further understand this SCAD–FMD paradox.
Surveillance and Screening
Optimal diagnostic imaging and surveillance strategies for FMD are unknown. Catheter‐based digital subtraction angiography remains the gold standard for diagnosis of FMD in all vascular beds.1 However, catheter‐based angiography is an invasive procedure, and other less‐invasive imaging modalities are available for diagnosis and surveillance.
Renal Artery Imaging
In patients with hypertension and clinical suspicion of renal artery stenosis, duplex ultrasound offers a noninvasive, first‐line screening test.1,3 Duplex ultrasound is a readily available, low‐cost, and low‐risk imaging modality that can give data on the flow characteristics within a vessel. However, there have been no published validation studies of duplex ultrasound versus angiography for the diagnosis of renal (or carotid) FMD. Although duplex ultrasound has limitations (i.e., technologist and interpreter expertise, patient body habitus, bowel gas), in experienced vascular laboratories, vascular ultrasound plays a central role in the diagnosis and surveillance of patients with renal FMD. Ultrasound features suggestive of renal FMD include elevated velocities and color and spectral turbulence in the mid and distal segments of the renal artery. In the case of severe lesions, there may be delayed systolic upstroke in the spectral Doppler waveform of arterial segments distal to the stenosis. Because of the limitations of ultrasound, confirmation by using another imaging modality is often required.
Once the diagnosis of renal artery FMD is made, ultrasound is a useful tool for surveillance, allows for periodic monitoring of renal artery velocities and kidney size, and can be used to monitor for restenosis after angioplasty.
CTA and MRA demonstrate good sensitivity and specificity for the diagnosis of renal artery FMD in small published case series performed in expert imaging centers (93% to 100%), although accuracy for assessment of “severity” of FMD lesions is limited.38–41 At the present time, the choice of technique between the 2 modalities for clinical practice should be determined by local technology and expertise with FMD imaging. Both CTA and MRA may miss mild FMD lesions and do not give information regarding the hemodynamic significance of lesions. These modalities also have low sensitivity for detecting FMD in the branch vessels. Thus, digital subtraction angiography remains the gold standard but is rarely required for diagnostic confirmation. Digital subtraction angiography is reserved for symptomatic patients for whom intervention is contemplated or for cases with an uncertainty in diagnosis or disease severity despite noninvasive imaging.1,3 When a renal intervention is planned, translesional pressure gradients should be measured to assess the severity of stenosis across multifocal or focal FMD lesions with angioplasty reserved for those patients with a significant pressure gradient.1
Carotid Artery Imaging
Little data exist regarding the use of noninvasive imaging to confirm the diagnosis of carotid and vertebral artery FMD, and no published study has validated duplex ultrasound, CTA, or MRA compared with digital subtraction angiography for the detection of cerebrovascular FMD.1,3 As in renal artery FMD, carotid duplex ultrasound provides a noninvasive and low‐cost screening tool. Carotid FMD can be identified with velocity shifts, spectral broadening, and turbulent color Doppler flow in the mid to distal cervical internal carotid artery and vertebral arteries (although detection of vertebral FMD by ultrasound may be difficult). Recently, tortuosity and redundancy of the internal carotid artery in an “S‐curve” configuration were described by Sethi and colleagues.42 Ultrasound findings of carotid FMD are in contrast to atherosclerotic lesions, which are visualized as plaque with corresponding velocity shifts at the carotid bifurcation or proximal segment of the internal carotid artery. Of note, carotid atherosclerosis and FMD can coexist; therefore, to detect cervical FMD, it is necessary to investigate the entire cervical internal carotid artery, especially the most distal segments.
Unlike atherosclerotic disease, it is not possible to show accurate percentage stenosis for carotid FMD on a duplex ultrasound report, because of the complex nature of the tandem lesions with areas of webbing and stenosis followed by dilatation in multifocal FMD. In general, it is recommended that ultrasound reports not attribute a specific percentage stenosis category (eg, 50% to 69%, >70%) to a case of internal carotid artery FMD and instead report that findings are consistent with fibromuscular dysplasia.
As in renal FMD, ultrasound has limitations and, therefore, additional noninvasive imaging is often necessary. For complete imaging of the carotid arteries above the skull base, the vertebral arteries, and the intracranial vessels, MRA or CTA is required. The European Consensus on FMD recommends MRA or CTA to establish the diagnosis of cerebrovascular FMD.3 Digital subtraction angiography remains the gold standard for diagnosing cerebrovascular FMD; however, its use is reserved for patients in whom the diagnosis is highly suspected despite inconclusive noninvasive imaging results.1
Screening for Occult Aneurysms in Patients With FMD
Once the diagnosis of FMD has been established in a vascular territory (eg, the renal and/or carotid arteries), it is our clinical practice to perform one‐time brain‐to‐pelvis imaging study(ies) to screen for occult aneurysms with either CTA or MRA. This practice is based on the significant prevalence of aneurysms among FMD patients reported in the US Registry. Seventeen percent of registrants had an aneurysm of ≥1 vessel.2,43 The most common sites were renal, carotid, and aortic arteries.2,43 A surprisingly high number (3.4%) of registrants were found to have an aortic aneurysm given the age and sex of the population. On the basis of these data, in our clinical practice, we routinely screen patients once for aortic, visceral, and intracranial aneurysms. However, it is important to note that there is need for more data regarding the cost effectiveness and clinical benefit of this practice. A large meta‐analysis and retrospective study by Cloft and colleagues found the prevalence of intracranial aneurysms in patients with cervical FMD to be ≈7%, which is lower than previous estimates but increased compared with that in the general population.44 Given the risk for significant morbid events, screening for intracranial aneurysms in all patients with FMD is recommended by the 2014 Scientific Statement Writing Group.1
Based on the location and significance of FMD lesions, the presence or absence of aneurysms or dissections that require imaging follow‐up, and the patient's clinical symptoms, a program of surveillance imaging is customized for each FMD patient.
Managing the FMD Patient
Care of the FMD patient consists of medical management, imaging surveillance of affected vascular beds, and referral for endovascular or surgical procedures when indicated. Location and severity of arterial lesion(s), symptoms, comorbidities, and previous vascular events due to FMD determine the type of therapy indicated.
There are little data regarding the optimal medical management of FMD patients, and clinical practice is often based on the management of patients with atherosclerotic disease. The 2011 multisocietal consensus guidelines for extracranial and vertebral artery disease gave antiplatelet therapy for carotid and vertebral FMD a Class IIa recommendation.45 No specific agent or dosing was recommended.45 Most experts prescribe 81 to 325 mg aspirin for patients with cerebrovascular FMD as long as the patient has no contraindication to antiplatelet therapy. There are no data on the use of clopidogrel or other antiplatelet agents for the management of patients with cerebrovascular FMD, although single‐agent clopidogrel may be used for select patients as an alternative to aspirin. For patients with carotid or vertebral artery dissection, treatment often consists of heparin (or low‐molecular‐weight heparin) followed by warfarin for 3 to 6 months, then, ultimately, antiplatelet therapy.1 The optimal medical therapy for carotid and vertebral artery dissection is also a matter of controversy. The ongoing trial Cervical Artery Dissection in Stroke Study (CADISS) is investigating antiplatelet therapy versus anticoagulation in patients with extracranial cervical artery dissection.46 Results from the nonrandomized arm of this trial demonstrated no significant difference between antiplatelet therapy and anticoagulation for the risk of recurrent stroke at 3 months.47 However, results from the entire randomized and nonrandomized cohort are pending. Patients with renal, mesenteric, or external iliac FMD are generally prescribed aspirin for thromboprophylaxis, although there are little data to support this practice. Expert consensus and clinical experience suggest that the use of angiotensin‐converting enzyme inhibitors and angiotensin II receptor blockers to be effective in treating hypertension attributable to renal artery FMD.1 Kidney function must be monitored when starting these medications due to the risk (although low) of acute kidney failure in the setting of significant bilateral renal artery stenosis. The recently reported data of elevated TGFβ1/TGFβ2 expression in a cohort of patients with FMD opens the door to future investigations of the role of TGF‐β signaling in this disease and potential pharmacological therapies that may act on this molecular pathway (ie, angiotensin II receptor blockers).25
Revascularization procedures can be beneficial in selected patients with renal FMD and hypertension. In a meta‐analysis of 70 studies of revascularization in patients with FMD involving >2600 patients, Trinquart and colleagues demonstrated that younger age and shorter duration of hypertension are associated with increased likelihood of cure with angioplasty or surgery.48 Patients with long‐standing hypertension and older patients are less likely to benefit from renal revascularization.48 In addition, factors associated with decreased likelihood of clinical benefit from renal percutaneous transluminal angioplasty (PTA) include abnormal renal function, smaller ipsilateral kidney, or metabolic abnormalities such as abnormal fasting glucose or hyperlipidemia.49 Interestingly, the reported hypertension cure rates in surgical and endovascular case series have declined by year of publication (Figure 3), perhaps reflecting less restrictive criteria for patient selection as these procedures (ie, balloon angioplasty) have become safer and more widely available. In 2014, the approach to renal FMD revascularization is generally PTA as first‐line therapy with surgical procedures reserved for patients with lesions not amenable to endovascular therapy, large aneurysms, or lesions that have not responded to prior intervention. Appropriate indications for revascularization in the setting of renal FMD, according to the 2014 Scientific Statement Writing Group, are shown in Table 4. In most circumstances, revascularization for FMD is performed for the management of hypertension, although in some cases, procedures may be undertaken for the treatment of sizable aneurysm or preservation of renal function (rare).
Figure 3.
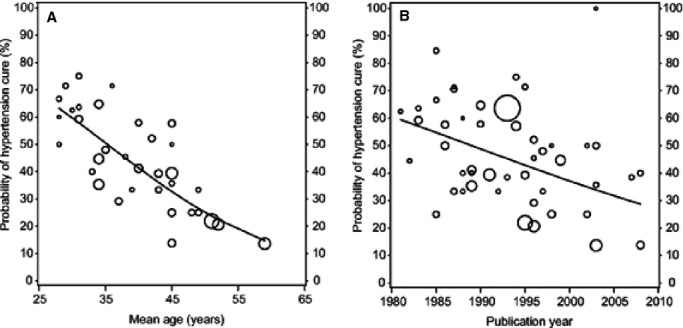
Meta‐regression analysis of published case series of renal FMD demonstrating the association between hypertension cure post PTA and mean age (A) and year of study publication (B). Size of the circle represents size of the case series. Adapted with permission from Trinquart et al.48 FMD indicates fibromuscular dysplasia; PTA, percutaneous transluminal angioplasty.
Table 4.
Indications for Renal Artery Revascularization
|
|
|
|
|
|
Reprinted with permission from Olin et al.1 PTA indicates percutaneous transluminal angioplasty.
Hemodynamic assessment (measurement of pressure gradients across the area of FMD) with or without procedure intravascular ultrasound is recommended before and after PTA to ensure there is hemodynamic significance of lesions present and that these lesions have been adequately treated with PTA. Admittedly, however, this recommendation is an extrapolation from previous studies in patients with atherosclerotic renal artery stenosis.51 No study to date has evaluated the effectiveness of hemodynamic‐guided versus traditional PTA in a cohort of FMD patients. Stenting of the renal artery is generally reserved for lesions that fail PTA or for management of flow‐limiting dissection. Two cases of FMD patients with renal artery stent fracture requiring bypass surgery have been recently reported.50 The European Consensus on FMD recommends against the use of cutting balloons in cases of PTA failure due to the risk of renal artery rupture.3
For patients with cerebrovascular FMD, surgical or endovascular therapy is reserved only for symptomatic patients, with the exception of those with intracranial aneurysms. The natural history of cerebrovascular FMD is different from that of atherosclerotic disease, and revascularization procedures are not indicated to treat asymptomatic lesions (eg, high velocities on an ultrasound examination), even for patients who have low procedural risk. It is uncommon for patients with cerebrovascular FMD to have neurological ischemic events while receiving antiplatelet therapy, although carotid or vertebral artery dissection may occur with resultant neurological events. The 2014 AHA Scientific Statement on FMD provides a detailed discussion of revascularization techniques for cerebrovascular FMD.1
Multispecialty Care for the Patient With FMD
Some clinical pearls for FMD clinical management are presented in Table 5. The care of the FMD patient requires a team‐based approach. Medical providers who may care for FMD patients include vascular medicine physicians, vascular surgeons, cardiologists, interventional radiologists, nephrologists, neurologists, and neurosurgeons, among others. In addition to the need for medical therapy and imaging surveillance and the potential need for revascularization or aneurysm repair, patients with FMD have many symptoms that can impair their quality of life. As discussed earlier, severe and frequent headaches, particularly migraines, are a common complaint among FMD patients. A specialized headache clinic can provide great clinical benefit. Often, these clinics can offer alternative treatments such as onabotulinumtoxinA (Botox) injections that can relieve severe chronic migraine symptoms.52 Investigation of migraine treatment in patients with FMD is an area ripe for research with no prospective studies on this population to date. In general, the use of ergotamines is avoided given the risk of sustained vasoconstriction in the FMD population at risk for stroke and arterial dissection. Triptan medications are prescribed with caution and generally avoided in FMD patients with history of myocardial infarction, stroke, or arterial dissection. Pulsatile tinnitus is another symptom that can be troublesome for FMD patients. Audiologists can assess for hearing loss and may help patients with strategies for symptom management. For some patients who present for evaluation of FMD but have physical features of a connective tissue disorder (eg, Loeys Dietz or Ehlers‐Danlös) and/or an extensive family history or aneurysm and dissection, evaluation by a clinical geneticist and genetic counselor may be of benefit.
Table 5.
Clinical Pearls in Managing the Patient With FMD
|
|
|
|
|
|
|
|
FMD indicates fibromuscular dysplasia; MRA, magnetic resonance angiography; CTA, computed tomography angiography; PTA, percutaneous transluminal angioplasty.
In a study from our center investigating physical and mental quality of life scores among patients at a tertiary center, female patients with FMD had decreased quality of life compared with the general and healthy US population.53 Headache, neck pain, and abdominal pain were significant contributing factors to reduced quality of life scores. Thus, pain management is vitally important. Patients with chronic disease often experience psychological distress, and FMD is no exception. Compounding patient symptoms and potential need for invasive procedures is the anxiety related to having an uncommon disease with which many health care providers are entirely unfamiliar. Therefore, referral to psychology and/or psychiatry colleagues to develop healthy coping practices is appropriate for those patients experiencing significant distress. The FMD Society of America (www.fmdsa.org) provides an online source for patient and health care provider information and support.
Conclusion
FMD is a disease that causes arterial stenosis, beading, dissection, and aneurysm and can present with a broad spectrum of clinical manifestations. Many FMD patients are minimally symptomatic or are diagnosed when an imaging study is performed for another indication. Some FMD patients have mild or moderate nonspecific symptoms, such as pulsatile tinnitus and migraine headaches or hypertension requiring medication therapy. Other patients have experienced major morbid events such as cerebrovascular and coronary dissections, stroke, and aneurysms. Fortunately, there appears to be a relatively low mortality rate associated with FMD. To date, no patient enrolled in the US Registry has died from vascular complications.54 Medical management consisting of antiplatelet agents and antihypertensive therapy is important for FMD patients, and a multidisciplinary plan should be in place for management of symptoms such as headache. All FMD patients should be comprehensively screened for occult aneurysms. Careful patient selection for revascularization procedures can increase the likelihood of clinical benefit. While recent and ongoing efforts have advanced our scientific and clinical understanding of this condition, recognizing the symptoms of this disease and making the correct diagnosis in a timely fashion constitute a vital first step in improving outcomes for FMD patients.
Disclosures
Ms O'Connor has no disclosures. Dr Gornik serves as a nonpaid member of the Medical Advisory Board for the FMD Society of America.
References
- 1.Olin JW, Gornik HL, Bacharach JM, Biller J, Fine LJ, Gray BH, Gray WA, Gupta R, Hamburg NM, Katzen BT, Lookstein RA, Lumsden AB, Newburger JW, Rundek T, Sperati CJ, Stanley JC. Fibromuscular dysplasia: state of the science and critical unanswered questions: a scientific statement from the American Heart Association. Circulation. 2014; 129:1048-1078. [DOI] [PubMed] [Google Scholar]
- 2.Olin JW, Froehlich J, Gu X, Bacharach JM, Eagle K, Gray BH, Jaff MR, Kim ESH, Mace P, Matsumoto AH, McBane RD, Kline‐Rogers E, White CJ, Gornik HL. The United States Registry for Fibromuscular Dysplasia: results in the first 447 patients. Circulation. 2012; 125:3182-3190. [DOI] [PubMed] [Google Scholar]
- 3.Persu A, Giavarini A, Touze E, Januszewicz A, Sapoval M, Azizi M, Barral X, Jeunemaitre X, Morganti A, Plouin P, de Leeuw P. European consensus on the diagnosis and management of fibromuscular dysplasia. J Hypertens. 2014; 32:1367-1378. [DOI] [PubMed] [Google Scholar]
- 4.Olin JW, Sealove BA. Diagnosis, management, and future developments of fibromuscular dysplasia. J Vasc Surg. 2011; 3:826-836. [DOI] [PubMed] [Google Scholar]
- 5.Mahmood RZ, Olin J, Gu X, Kline‐Rogers E, Froehlich JB, Bacharach JM, Chi Y, Gray B, Jaff M, Katzen B, Kim E, Mace P, White C, Sharma A, White C, Gornik H. Unraveling pulsatile tinnitus in FMD: a report of the United States Registry for Fibromuscular Dysplasia. ACC. 2014. 10.1016/S0735‐1097(13)62078‐1 [Google Scholar]
- 6.Poloskey SL, Olin J, Froehlich J, Gu X, Bacharach JM, Gray B, Grise M, Jaff M, Kim SH, Kline‐Rogers E, Mace P, Matsumoto A, McBane R, Rooke T, Gornik H. Physical examination findings in fibromuscular dysplasia: a report of the United States Registry for Fibromuscular Dysplasia. J Am Coll Cardiol. 2012a; 59:E2075 [Google Scholar]
- 7.Harrison EG, McCormack LJ. Pathologic classification of renal arterial disease in renovascular hypertension. Mayo Clin Proc. 1971; 46:161-167. [PubMed] [Google Scholar]
- 8.Harrison EG, Hunt JC, Bernatz PE. Morphology of fibromuscular dysplasia of the renal artery in renovascular hypertension. Am J Med. 1967; 43:97-112. [DOI] [PubMed] [Google Scholar]
- 9.McCormack LJ, Poutasse EF, Meaney TF, Noto TJ, Dustan HP. A pathologic‐arteriographic correlation of renal artery disease. Am Heart J. 1966; 72:188-198. [DOI] [PubMed] [Google Scholar]
- 10.Persu A, Touzé E, Mousseaux E, Barral X, Joffre F, Plouin P. Diagnosis and management of fibromuscular dysplasia: an expert consensus. Eur J Clin Invest. 2012; 42:338-347. [DOI] [PubMed] [Google Scholar]
- 11.Savard S, Steichen O, Azarine A, Azizi M, Jeunemaitre X, Plouin P. Association between 2 angiographic subtypes of renal artery fibromuscular dysplasia and clinical characteristics. Circulation. 2012; 126:3062-3069. [DOI] [PubMed] [Google Scholar]
- 12.National Organization for Rare Diseases. 2014. Available at: http://rarediseases.org/. Accessed July 1, 2014.
- 13.Lorenz EC, Vrtiska TJ, Lieske JC, Dillon JJ, Stegall MD, Li X, Bergstralh EJ, Rule AD. Prevalence of renal artery and kidney abnormalities by computed tomography among healthy adults. Clin J Am Soc Nephrol. 2010; 5:431-438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blondin D, Lanzman R, Schellhammer F, Oels M, Grotemeyer D, Baldus SE, Rump LC, Sandmann W, Voiculescu A. Fibromuscular dysplasia in living renal donors: still a challenge to computed tomographic angiography. Eur J Radiol. 2010; 75:67-71. [DOI] [PubMed] [Google Scholar]
- 15.Cragg AH, Smith TP, Thompson BH, Maroney TP, Stanson AW, Shaw GT, Hunter DW, Cochran ST. Incidental fibromuscular dysplasia in potential renal donors: long‐term clinical follow up. Radiology. 1989; 172:145-147. [DOI] [PubMed] [Google Scholar]
- 16.McKenzie GA, Oderich GS, Kawashima A, Misra S. Renal artery fibromuscular dysplasia in 2,640 renal donor subjects: a CT angiography analysis. J Vasc Interv Radiol. 2013; 24:1477-1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Touzé E, Oppenheim C, Trystram D, Nokam G, Pasquini M, Alamowitch S, Hervé D, Garnier P, Mousseaux E, Plouin P. Fibromuscular dysplasia of cervical and intracranial arteries. Int J Stroke. 2010; 5:296-305. [DOI] [PubMed] [Google Scholar]
- 18.Kim ESH, Olin JW, Froehlich JB, Gu X, Bacharach JM, Gray BH, Jaff MR, Katzen BT, Kline‐Rogers E, Mace PD, Matsumoto AH, McBane RD, White CJ, Gornik HL. Clinical manifestations of fibromuscular dysplasia vary by patient sex: a report of the United States registry for fibromuscular dysplasia. J Am Coll Cardiol. 2013; 61:2026-2028. [DOI] [PubMed] [Google Scholar]
- 19.Halpern MM, Sanford HS, Viamonte M., Jr Renal‐artery abnormalities in three hypertensive sisters: probable familial fibromuscular hyperplasia. JAMA. 1965; 194:512-513. [PubMed] [Google Scholar]
- 20.Rushton A. The genetics of fibromuscular dysplasia. Arch Intern Med. 1980; 140:233-236. [PubMed] [Google Scholar]
- 21.Major P, Genest J, Cartier P, Kuchel O. Hereditary fibromuscular dysplasia with renovascular hypertension. Ann Intern Med. 1977; 86:583. [DOI] [PubMed] [Google Scholar]
- 22.Perdu J, Boutouyrie P, Bourgain C, Stern N, Laloux B, Bozec E, Azizi M, Bonaiti‐Pellié C, Plouin PF, Laurent S, Gimenez‐Roqueplo AP, Jeunemaitre X. Inheritance of arterial lesions in renal fibromuscular dysplasia. J Hum Hypertens. 2007; 21:393-400. [DOI] [PubMed] [Google Scholar]
- 23.Pannier‐Moreau I, Grimbert P, Fiquet‐Kempf B, Vuagnat A, Jeunemaitre X, Corvol P, Plouin PF. Possible familial origin of multifocal renal artery fibromuscular dysplasia. J Hypertens. 1997; 12:1797-1801. [DOI] [PubMed] [Google Scholar]
- 24.Poloskey SL, Kim ES, Sanghani R, Al‐Quthami AH, Arscott P, Moran R, Rigelsky CM, Gornik HL. Low yield of genetic testing for known vascular connective tissue disorders in patients with fibromuscular dysplasia. Vasc Med. 2012b; 17:371-378. [DOI] [PubMed] [Google Scholar]
- 25.Ganesh SK, Morissette R, Xu Z, Schoenhoff F, Griswold BF, Yang J, Tong L, Yang M, Hunker K, Sloper L, Kuo S, Raza R, Milewicz DM, Francomano CA, Dietz HC, Van Eyk J, McDonnell NB. Clinical and biochemical profiles suggest fibromuscular dysplasia is a systemic disease with altered TGF‐ß expression and connective tissue features. FASEB J. 2014; 28:3313-3324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Savard S, Azarine A, Jeunemaitre X, Azizi M, Plouin P, Steichen O. Association of smoking with phenotype at diagnosis and vascular interventions in patients with renal artery fibromuscular dysplasia. Hypertension. 2013; 61:1227-1232. [DOI] [PubMed] [Google Scholar]
- 27.Maresi E, Becchina G, Ottoveggio G, Orlando E, Midulla R, Passantino R. Arrhythmic sudden cardiac death in a 3‐year‐old child with intimal fibroplasia of coronary arteries, aorta, and its branches. Cardiovasc Pathol. 2001; 10:43-48. [DOI] [PubMed] [Google Scholar]
- 28.Hill SF, Sheppard MN. Non‐atherosclerotic coronary artery disease associated with sudden cardiac death. Heart. 2010; 96:1119-1125. [DOI] [PubMed] [Google Scholar]
- 29.Roppoen KM, Alafuzoff I. A case of sudden death caused by fibromuscular dysplasia. J Clin Pathol. 1999; 52:541-542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zack F, Kutter G, Blaas V, Rodewald A, Büttner A. Fibromuscular dysplasia of cardiac conduction system arteries in traumatic and nonnatural sudden death victims aged 0 to 40 years: a histological analysis of 100 cases. Cardiovasc Pathol. 2014; 23:12-16. [DOI] [PubMed] [Google Scholar]
- 31.Saw J, Ricci D, Starovoytov A, Fox R, Buller CE. Spontaneous coronary artery dissection: prevalence of predisposing conditions including fibromuscular dysplasia in a tertiary center cohort. JACC Cardiovasc Interv. 2013; 6:44-52. [DOI] [PubMed] [Google Scholar]
- 32.Pate GE, Lowe R, Buller CE. Fibromuscular dysplasia of the coronary and renal arteries? Catheter Cardiovasc Interv. 2005; 64:138-145. [DOI] [PubMed] [Google Scholar]
- 33.Toggweiler S, Puck M, Thalhammer C, Manka R, Wyss M, Bilecen D, Corti R, Amann‐Vesti B, Luscher T, Wyss C. Associated vascular lesions in patients with spontaneous coronary artery dissection. Swiss Med Wkly. 2012; 142:000-0000. [DOI] [PubMed] [Google Scholar]
- 34.Tweet MS, Hayes SN, Pitta SR, Simari RD, Lerman A, Lennon RJ, Gersh BJ, Khambatta S, Best PJM, Rihal CS, Gulati R. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation. 2012; 126:579-588. [DOI] [PubMed] [Google Scholar]
- 35.Liang JJ, Prasad M, Tweet MS, Hayes SN, Gulati R, Breen JF, Leng S, Vrtiska TJ. A novel application of CT angiography to detect extracoronary vascular abnormalities in patients with spontaneous coronary artery dissection. J Cardiovasc Comput Tomogr. 2014; 8:189-197. [DOI] [PubMed] [Google Scholar]
- 36.Prasad M, Tweet M, Liang J, Hayes S, Breen J, Gulati R, Vrtiska T. Extracoronary vascular abnormalities are common in patients with spontaneous coronary dissection: analysis of 72 patients at a tertiary referral center. J Am Coll Cardiol. 2014; 6312_S10.1016/S0735‐1097(14)62060‐X [Google Scholar]
- 37.Camuglia A, Manins V, Taylor A, Hengel C. Case report and review: epicardial coronary artery fibromuscular dysplasia. Heart Lung Circ. 2009; 18:151-154. [DOI] [PubMed] [Google Scholar]
- 38.Sabharwal R, Vladica P, Colemen P. Multidetector spiral CT renal angiography in the diagnosis of renal artery fibromuscular dysplasia. Eur J Radiol. 2007; 61:520-527. [DOI] [PubMed] [Google Scholar]
- 39.Willoteaux S, Faivre‐Pierret M, Moranne O, Lions C, Bruzzi J, Finot M, Gaxotte V, Mounier‐Vehier C, Beregi JP. Fibromuscular dysplasia of the main renal arteries: comparison of contrast‐enhanced MR angiography with digital subtraction angiography. Radiology. 2006; 241:922-929. [DOI] [PubMed] [Google Scholar]
- 40.Heiserman JE, Drayer BP, Fram EK, Keller PJ. MR angiography of cervical fibromuscular dysplasia. AJNR Am J Neuroradiol. 1992; 13:1454-1457. [PMC free article] [PubMed] [Google Scholar]
- 41.Furie DM, Tien RD. Fibromuscular dysplasia of arteries of the head and neck: imaging findings. AJR Am J Roentgenol. 1994; 162:1205-1209. [DOI] [PubMed] [Google Scholar]
- 42.Sethi SS, Lau JF, Gustavson S, Olin JW. The S curve: a novel morphological finding in the internal carotid artery in patients with fibromuscular dysplasia. Vasc Med. 2014; 19:356-362. [DOI] [PubMed] [Google Scholar]
- 43.Gavin J, Gu X, Olin J, Gornik H, Kim SH, Gray B, Jaff M, McBane R, Katzen B, White C, Mace P, Kline‐Rogers E, Froehlich J. Prevalence of arterial aneurysms in patients with fibromuscular dysplasia: a report from the United States Registry for fibromuscular dysplasia. J Am Coll Cardiol. 2013; 6110.1016/S0735‐1097(13)62078‐1 [Google Scholar]
- 44.Cloft HJ, Kallmes DF, Kallmes MH, Goldstein JH, Jensen ME, Dion JE. Prevalence of cerebral aneurysms in patients with fibromuscular dysplasia: a reassessment. J Neurosurg. 1998; 88:436-440. [DOI] [PubMed] [Google Scholar]
- 45.Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL, Cates CU, Creager MA, Fowler SB, Friday G, Hertzberg VS, McIff EB, Moore WS, Panagos PD, Riles TS, Rosenwasser RH, Taylor AJ, Jacobs AK, Smith SC, Anderson JL, Adams CD, Albert N, Buller CE, Creager MA, Ettinger SM, Guyton RA, Halperin JL, Hochman JS, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura RA, Ohman EM, Page RL, Riegel B, Stevenson WG, Tarkington LG, Yancy CW. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. Catheter Cardiovasc Interv. 2013; 81:E76-E123. [DOI] [PubMed] [Google Scholar]
- 46.The CADISS Trial Investigators. Antiplatelet therapy vs. anticoagulation in cervical artery dissection: rationale and design of the cervical artery dissection in stroke study (CADISS). Int J Stroke. 2007; 2:292-296. [DOI] [PubMed] [Google Scholar]
- 47.Kennedy F, Lanfranconi S, Hicks C, Reid J, Gomperez P, Price C, Kerry S, Norris J, Marks HSCADISS Investigators. Antiplatelets vs anticoagulation for dissection: CADISS nonrandomized arm and meta‐analysis. Neurology. 2012; 79:686-689. [DOI] [PubMed] [Google Scholar]
- 48.Trinquart L, Mounier‐Vehier C, Sapoval M, Gagnon N, Plouin P. Efficacy of revascularization for renal artery stenosis caused by fibromuscular dysplasia: a systematic review and meta‐analysis. Hypertension. 2010; 56:525-532. [DOI] [PubMed] [Google Scholar]
- 49.Davies MG, Saad WE, Peden EK, Mohiuddin IT, Naoum JJ, Lumsden AB. The long‐term outcomes of percutaneous therapy for renal artery fibromuscular dysplasia. J Vasc Surg. 2008; 48:865-871. [DOI] [PubMed] [Google Scholar]
- 50.Raju MG, Bajzer CT, Clair DG, Kim ESH, Gornik HL. Renal artery stent fracture in patients with fibromuscular dysplasia: a cautionary tale. Circ Cardiovasc Interv. 2013; 6:e30-e31. [DOI] [PubMed] [Google Scholar]
- 51.Mangiacapra F, Trana C, Sarno G, Davidavicius G, Protasiewicz M, Muller O, Ntalianis A, Misonis N, Van Vlem B, Heyndrickx GR, DeBruyne B. Translesional pressure gradients to predict blood pressure response after renal artery stenting in patients with renovascular hypertension. Circ Cardiovasc Interv. 2010; 3:537-542. [DOI] [PubMed] [Google Scholar]
- 52.Aurora SK, Winner P, Freeman MC, Spierings EL, Heiring JO, DeGryse RE, VanDenburgh AM, Nolan ME, Turkel CC. OnabotulinumtoxinA for treatment of chronic migraine: pooled analyses of the 56‐week PREEMPT clinical program. Headache. 2011; 51:1358-1373. [DOI] [PubMed] [Google Scholar]
- 53.Fendrikova Mahlay F, Shao M, Kim ESH, Sanghani R, Pozuelo L, Gornik HL. Determinants of quality of life among women with fibromuscular dysplasia (abstract). Vasc Med. 2013; 18:163 [Google Scholar]
- 54.O'Connor S, Olin J, Gu X, Bacharach JM, Chi Y, Froehlich J, Gray B, Kim SH, Kline‐Rogers E, Mace P, McBane R, Sharma A, Gornik H. Morbidity and mortality for fibromuscular dysplasia: a report of the fibromuscular dysplasia registry. Society of Vascular Medicine Annual Meeting, San Diego, CA. 2014. (abstract).


