Abstract
Background
Multicenter studies on idiopathic or viral pericarditis and pericardial effusion (PPE) have not been reported in children. Colchicine use for PPE in adults is supported. We explored epidemiology and management for inpatient hospitalizations for PPE in US children and risk factors for readmission.
Methods and Results
We analyzed patients in the Pediatric Health Information System database for (1) a code for PPE; (2) absence of codes for underlying systemic disease (eg, neoplastic, cardiac, rheumatologic, renal); (3) age ≥30 days and <21 years; and (4) discharge between January 1, 2007, and December 31, 2012, from 38 hospitals contributing complete data for each year of the study period. Among 11 364 hospitalizations with PPE codes during the study period, 543 (4.8%) met entry criteria for idiopathic or viral PPE. Significantly more boys were noted, especially among adolescents. No temporal trends were noted. Median age was 14.5 years (interquartile range 7.3 to 16.6 years); 78 patients (14.4%) underwent pericardiocentesis, 13 (2.4%) underwent pericardiotomy, and 11 (2.0%) underwent pericardiectomy; 157 (28.9%) had an intensive care unit stay, including 2.0% with tamponade. Median hospitalization was 3 days (interquartile range 2 to 4 days). Medications used at initial admission were nonsteroidal anti‐inflammatory drugs (71.3%), corticosteroids (22.7%), aspirin (7.0%), and colchicine (3.9%). Readmissions within 1 year of initial admission occurred in 46 of 447 patients (10.3%), mostly in the first 3 months. No independent predictors of readmission were noted, but our statistical power was limited. Practice variation was noted in medical management and pericardiocentesis.
Conclusions
Our report provides the first large multicenter description of idiopathic or viral PPE in children. Idiopathic or viral PPE is most common in male adolescents and is treated infrequently with colchicine.
Keywords: colchicine, pediatric, pericardial disease, pericardial effusion, pericarditis, pericardium
Introduction
Idiopathic pericarditis accounts for 37% to 68% of inpatient admissions for pericardial effusions or acute pericarditis in children.1–3 The usual approach to initial management of acute pericarditis includes administration of nonsteroidal anti‐inflammatory agents. Colchicine has emerged as an important adjunct in management of recurrent pericarditis and acute pericarditis in adults.4–5 The European Society of Cardiology guidelines for management of pericarditis recommend use of colchicine in recurrent and acute pericarditis6; however, management may include other pharmacological agents, and invasive procedures for pericardial effusions are sometimes needed. Recurrence of pericarditis is common in both children and adults, with reports ranging from 15% to 40%.2–4,2–8 Higher recurrence rates have been observed in patients with a history of use of corticosteroids in the initial episode of pericarditis in adults.4,7 Data on epidemiology, management guidelines, and colchicine use in children for pericarditis are sparse.9–10
Most studies on pericarditis in children have been single‐center series.1,3,9 In the present multicenter study, we sought to characterize epidemiology, associated morbidities, inpatient management, and risk factors for readmission in idiopathic or viral pericarditis and pericardial effusion (PPE). Our analyses were performed using the Pediatric Health Information System (PHIS) database of freestanding children's hospitals in the United States.
Methods
Study Design
We performed a retrospective review and analysis of a multicenter database. Approval for the study was obtained from the institutional review board at the Boston Children's Hospital, which waived the informed consent requirement.
Data Source
Data were obtained from the PHIS database for the 6‐year period encompassing calendar years 2007–2012. The PHIS database is a resource utilization database from participating freestanding children's hospitals in the United States. It provides information for all hospital discharges including demographic data; diagnostic and procedural International Classification of Diseases, ninth revision (ICD‐9) codes (level 1) and resource utilization data (level 2) from charges for procedures, medications, imaging studies, laboratory tests, supplies, and other clinical services. The PHIS database allows longitudinal follow‐up of patients who have multiple admissions at the same hospital. The data quality is ensured through systematic monitoring.
Selection Process
From the PHIS database, we selected all inpatient hospital discharges between January 1, 2007, and December 31, 2012, with ICD‐9 codes suggesting PPE at a hospital that contributed both level 1 and level 2 data to PHIS for each year of the study period. Inclusion criteria were age <21 years at admission; ICD‐9 diagnosis codes indicating PPE or procedure codes indicating pericardiocentesis, pericardiotomy, or pericardiectomy (see Table S1); and no prior admission with pericarditis codes in the preceding year.
Etiologies for PPE
We identified patients with underlying systemic diseases, neonatal problems, and cardiac surgery as having potential causes for PPE and assigned the following appropriate etiologic categories (see Tables S2 and S3):
ICD‐9 codes for underlying systemic diseases or other potential causes for PPE (eg, neoplastic, cardiac, myocarditis, endocarditis, rheumatic, rheumatologic, chronic renal, endocrine, immunologic, chest trauma, organ transplant, nonviral infection, hematologic, gastrointestinal, hematologic, and perinatal) were used to generate categories for possible etiology of pericarditis.
Underlying neonatal problems such as birth asphyxia, hydrops fetalis, prematurity (<36 weeks of gestation), low birth weight (<2500 g), and patients aged <31 days were noted.
Repair of congenital heart defect in the past 6 months, as defined by the entry criteria for the Risk Adjusted classification for Congenital Heart Surgery (RACHS‐1) method, and placement of a pacemaker (epicardial and transvenous) were noted.11
From the cohort of patients with PPE, we identified patients with likely idiopathic or viral PPE by excluding all those with other potential causes for PPE (see Table S4).
Data Obtained
Variables collected from the PHIS database were patient age, sex, birth weight, center of care, race, geographic region, dates of admission and discharge, stay in the intensive care unit, mortality, principal and secondary diagnosis codes, procedure codes, medications (anti‐inflammatory medications and antacids). The study period was divided by year and by quarter to assess uniformity in the number of pericarditis discharges over time.
Initial Admission
Initial admission was defined as admission with qualifying diagnosis or procedure codes for PPE if the patient was not admitted with qualifying diagnosis or procedure codes in the preceding year (including up to 2006).
Readmission
Readmission was defined as subsequent admission with qualifying diagnosis or procedure codes for PPE within 1 year of initial admission. We limited our sample to those patients whose initial admission was between 2007 and 2011, allowing for a complete year of follow‐up. Readmissions at same center with PPE were identified using unique patient identifiers in the PHIS database.
Statistical Analysis
Patient and procedural characteristics were summarized using frequencies and percentages for categorical variables and medians with 25th and 75th percentiles (interquartile range) for continuous variables. The chi‐square goodness of fit test was used to explore uniformity with respect to the number of discharges throughout time (quarterly and yearly). Logistic regression was used to assess relationships between patient factors and the outcome of readmission within 12 months. Odds ratios with 95% confidence intervals are reported. Variables significant at the 0.10 level were considered for inclusion in a multivariable model. P≤0.05 was considered significant. SAS v9.3 (SAS Institute, Cary NC) was used for data analysis.
Results
A total of 11 364 eligible patients were noted in the 38 centers that contributed both level 1 and level 2 data to the PHIS during each of the 6 years studied. Of these, we excluded 10 802 patients who had codes for diseases known to be associated with pericarditis (see Table S4) and 19 patients aged <31 days. The remaining 543 patients were presumed to have idiopathic or viral PPE and constituted the cohort for our study. The demographic and clinical characteristics of our study cohort are shown in Table 1.
Table 1.
Demographic and Clinical Characteristics of Patients With Idiopathic or Viral Pericarditis and Pericardial Effusion
| Characteristic (N=543) | Median (IQR) or n (%) |
|---|---|
| Demographic | |
| Female | 157 (28.9) |
| Age, y | 14.5 (7.3 to 16.6) |
| Race | |
| Black | 113 (20.8) |
| Hispanic or Latino | 75 (13.8) |
| White | 277 (51.0) |
| Other or unknown | 78 (14.4) |
| Clinical | |
| Hospital length of stay (days) | 3 (2 to 4) |
| Intensive care unit stay | 157 (28.9) |
| Cardiac tamponade | 11 (2.0) |
| Pericardial drainage procedure* | 96 (17.7) |
IQR indicates interquartile range.
Includes pericardiocentesis, pericardiotomy, and pericardiectomy procedures.
Subjects’ median age was 14.5 years (interquartile range 7.3 to 16.6 years). In the adolescent age group, idiopathic or viral PPE was significantly more frequent in boys than in girls (Figure 1), and male adolescents constituted about half of our study cohort. The Northeast region had a significantly higher number of hospital discharges with idiopathic or viral PPE per 100 000 hospital discharges (P<0.001) (Figure 2); however, we found no significant quarterly or yearly association in the number of pericarditis discharges during the study period (Figure 3).
Figure 1.
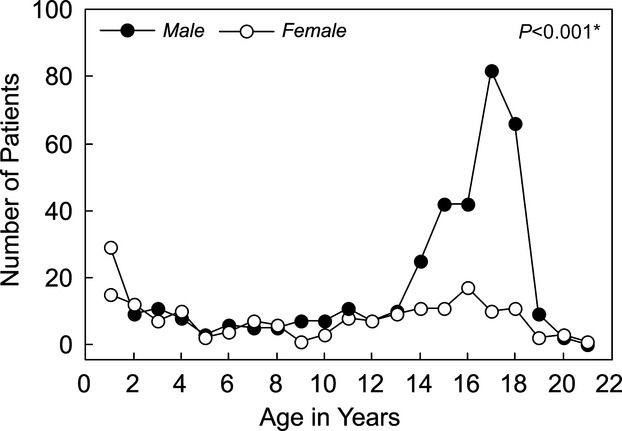
Age and sex at initial admission. *Wilcoxon rank sum test.
Figure 2.
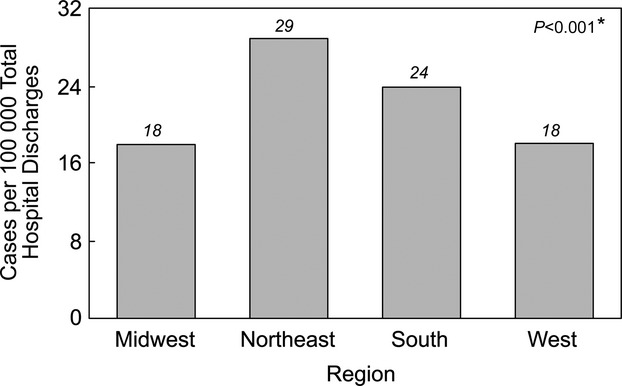
Geographic distribution at initial admission. *Chi‐square test.
Figure 3.
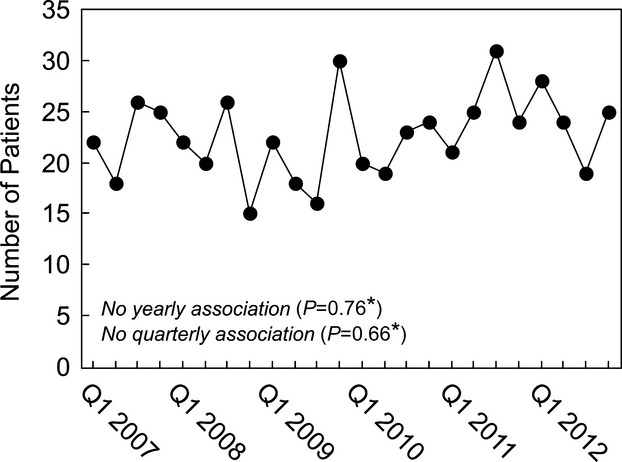
Trends for initial admission by quarters of each year of the study period. *Chi‐square test. Q1 indicates first quarter.
Hospital Course
There were no inpatient deaths in our cohort. The median length of hospital stay was 3 days (interquartile range 2 to 4 days). Care in an intensive care unit was noted for 157 patients (28.9%), and cardiac tamponade was coded for 11 (2.0%). A pericardial drainage procedure was performed in 96 patients (17.7%), including (not mutually exclusive) pericardiocentesis in 78 (14.4%), pericardiotomy in 13 (2.4%), and pericardiectomy in 11 (2.0%).
Medications
At least 1 anti‐inflammatory medication was used in 433 patients (79.7%). Nonsteroidal anti‐inflammatory drugs were used most commonly (387 patients, 71.3%), followed by corticosteroids (123 patients, 22.7%), aspirin (38 patients, 7%), colchicine (21 patients, 3.9%), and methotrexate (2 patients, 0.4%). Use of these medications was not mutually exclusive. Other immunosuppressants, such as anakinra, azathioprine, cyclophosphamide, cyclosporine, and rituximab, were not used in initial admissions. Pharmacological management in initial admission is shown in Table 2. More than 1 anti‐inflammatory medication was used in 100 patients (18.4%). Aspirin or nonsteroidal anti‐inflammatory drugs were used alone in more than half of cases, followed by their combination with corticosteroids (14.6%). Colchicine was always used in combination with other anti‐inflammatory medications. These medications could have been used either simultaneously or sequentially at any time during admission. Use of antacids was noted in 60.6% of initial admissions.
Table 2.
Pharmacological Management at Initial Admission
| Medications (N=543) | Discharges, n (%) |
|---|---|
| No NSAID/aspirin, corticosteroid, or colchicine | 110 (20.2) |
| NSAID/aspirin only | 294 (54.2) |
| Corticosteroid only | 39 (7.2) |
| Colchicine only | 0 (0.0) |
| NSAID/aspirin+corticosteroids | 79 (14.6) |
| NSAID/aspirin+colchicine | 16 (2.9) |
| NSAID/aspirin+corticosteroids+colchicine | 4 (0.7) |
| Corticosteroids+colchicine | 1 (0.2) |
NSAID indicates nonsteroidal anti‐inflammatory drug.
Practice Variation in Management During Initial Admission
Figure 4 depicts the variability in the use of corticosteroids (Figure 4A), colchicine (Figure 4B), and pericardial drainage procedures (Figure 4C) across centers. We explored the percentage of patients within each center in whom corticosteroids were used. Two centers did not administer corticosteroids to patients with idiopathic or viral PPE, and 8 centers administered corticosteroids to >40% of their initial admissions. Colchicine was used in only 7 of the 31 centers over the study period. Within centers, the median percentage of patients who underwent pericardial drainage procedures was 16.5% (interquartile range 9.1% to 23.1%); 28 centers used these procedures for >10% of their initial admissions.
Figure 4.
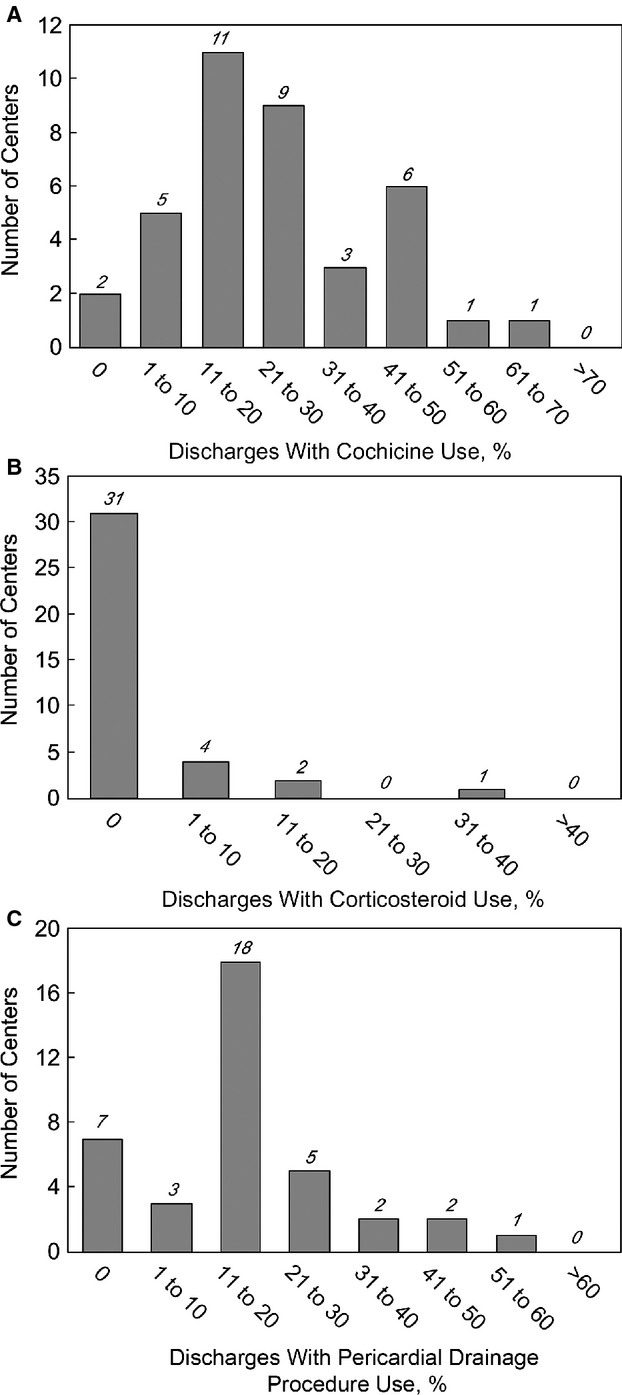
Practice variation in management in initial admission. A, Practice variation in corticosteroid use in initial admission. B, Practice variation in colchicine use in initial admission. C, Practice variation in pericardial drainage procedure use in initial admission.
Readmissions
Readmission at least once within 1 year of initial admission with ICD‐9 codes for PPE occurred in 46 of 447 patients who had at least 1 year of follow‐up (10.3%). Most of these patients had only a single readmission (n=33, 71.7%). Multiple readmissions within 1 year of initial admission were noted in 13 patients: 2 readmissions were noted for 8 patients, 3 readmissions were noted for 4, and 4 readmissions were noted for 1. Figure 5 shows the time to readmission for these patients. Most (78.3%) were readmitted within 3 months of the initial admission.
Figure 5.
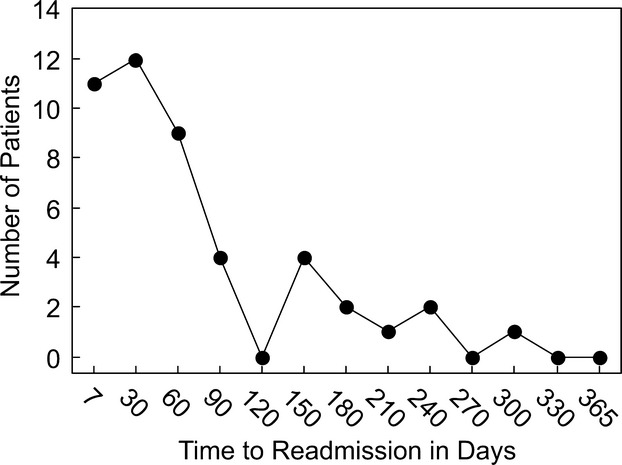
Time to first readmission since initial admission.
Risk factors for readmission are summarized in Table 3. On univariate analysis, geographic region had a borderline association with readmission (P=0.051); the highest odds ratio for readmission, compared with the West, occurred in the Midwest region (5.47; 95% CI, 1.53 to 19.5). We did not find significant associations of readmission with other factors, including sex, age, race, intensive care unit admission, hospital lengths of stay, or use of pericardial drainage procedures on first admission. None of the medications used in initial admission was significantly associated with readmission. Multivariable analysis demonstrated that region continued to have a borderline association with readmission (P=0.05).
Table 3.
Risk Factors for Readmission on Univariate Analysis
| Variable (N=447) | Odds Ratio (95% CI) | P Value |
|---|---|---|
| Female sex | 0.66 (0.32 to 1.37) | 0.26 |
| Region | ||
| Midwest | 5.47 (1.53 to 19.49) | 0.05 |
| Northeast | 2.70 (0.71 to 10.33) | |
| South | 3.32 (0.95 to 11.62) | |
| West | 1 | |
| Race | ||
| Black | 1.65 (0.78 to 3.46) | 0.6 |
| Hispanic or Latino | 1.41 (0.57 to 3.52) | |
| White | 1.0 | |
| Other or unknown | 1.13 (0.43 to 2.93) | |
| 1 year increase in age | 0.97 (0.93 to 1.02) | 0.28 |
| ICU admission | 0.99 (0.50 to 1.95) | 0.98 |
| 1 day increase in hospital LOS | 0.99 (0.92 to 1.05) | 0.67 |
| Pericardial procedure | 1.57 (0.76 to 3.24) | 0.23 |
| Antacid | 1.90 (0.96 to 3.78) | 0.07 |
| Corticosteroid | 1.56 (0.80 to 3.04) | 0.20 |
| Aspirin | 1.22 (0.41 to 3.65) | 0.72 |
| NSAID | 1.26 (0.62 to 2.57) | 0.52 |
| Colchicine | 1.80 (0.50 to 6.45) | 0.37 |
ICU indicates intensive care unit; LOS, length of stay; NSAID, nonsteroidal anti‐inflammatory drug.
Discussion
Using the PHIS database from 2007 to 2012, we describe the epidemiology of idiopathic or viral PPE in children requiring inpatient care in freestanding children's hospitals. Adolescents, particularly boys, were most commonly affected. We found no temporal trends. Although codes for cardiac tamponade were uncommon, pericardial drainage procedures were used in 18% of patients on initial admission. Nonsteroidal anti‐inflammatory drugs or aspirin were used most commonly, either alone or in combinations with other medications, followed by corticosteroid use; however, colchicine was uncommonly administered. Practice variation appeared to be marked, although small numbers prevented us from testing statistical significance. Readmission with PPE was noted for 1 in 10 patients, mostly within 3 months of initial admission. Although use of corticosteroids in adults with pericarditis has been associated with a higher complication rate including increased recurrence rate, we could not identify significant risk factors for readmission in our cohort with very limited power.4,12–13 Our data do not allow us to understand the trend toward higher odds of readmission in the Midwest region, although practice variation may be a contributing factor.
Although the incidence of idiopathic or viral PPE appeared to rise during adolescence in both sexes, the spike in male adolescents was especially striking. Although we could not find previous reports of a male predilection for idiopathic or viral PPE, male predominance has been noted in cases of viral myocarditis.14 Myocarditis and pericarditis may share common viral etiologic agents. Moreover, mouse models of myocarditis have demonstrated the influence of sex‐associated steroid hormones on viral concentration, disease susceptibility, and immune response to infection.15–17 The interplay of hormonal changes in adolescence and male susceptibility to viral infections is likely to play a role; however, we cannot exclude other etiologic factors for male predominance.
The use of colchicine was concentrated in a few pediatric centers; however, colchicine has been shown to reduce recurrence rate, duration of symptoms, and hospitalization rate in multiple adult studies, including a recent randomized double‐blind placebo‐controlled trial in adults with acute pericarditis.4,18 Moreover, addition of colchicine to nonsteroidal anti‐inflammatory drugs or aspirin has not been associated with a greater rate of serious adverse side effects.4,18–19 Colchicine has been recommended in acute (class 2a) and recurrent (class 1) pericarditis by the European Society of Cardiology since 2004.6 These guidelines and adult studies demonstrating benefits of colchicine use without significant adverse effects predate our study cohort. Colchicine has been used in children with familial Mediterranean fever.20 Its use has also been reported in small pediatric series of pericarditis.9–10 Our data suggest that the practice of colchicine use in adults with pericarditis or PPE has not yet translated to pediatric practice. The infrequent use of colchicine in children with viral or idiopathic PPE might be related to the paucity of published pediatric studies on its use or to a lack of familiarity with this drug in pediatric cardiologic practice.
Our study should be interpreted in light of its limitations. Related to the use of administrative databases, limitations include omission of diagnoses or medications because of errors in data entry or coding as well as coding of only limited clinical data. Because children's weights are not available, we were unable to report doses of medications. Our data derived from a database of pediatric inpatients admitted to freestanding children's hospitals and may not be generalizable to pediatric admissions in other inpatient settings or to outpatient management. Patients transferred to PHIS hospitals after initial treatment elsewhere may be incorrectly captured as initial cases. The inability to track patients across centers could have contributed to underestimation of readmissions. The recurrence rate of pericarditis could be further underestimated by the absence of data on outpatient management and evaluation in the emergency room. Eleven patients had codes for pericardiectomy on initial admission as defined in our entry criteria, yet pericardiectomy is usually performed in patients with chronic recurrent pericarditis. We are unable to exclude the possibility that this finding is due to coding error or misclassification, for example, because of our inability to track patients across centers. Finally, the small number of readmissions limited our power to find significant predictors of readmission in our study.
In conclusion, we report the first large multicenter description of idiopathic or viral PPE in children and explore the risk factors for readmission. Our data suggest that idiopathic or viral PPE is most common in adolescents, particularly boys, and that practices in the care of these patients vary across centers. Further multicenter studies or a prospective registry would be helpful in formulating recommendations for therapy in children.
Supplementary Material
Supplementary Table 1. ICD-9 Diagnosis and Procedure codes along with their description, used for selection of discharges with pericarditis or pericardial effusion.
Supplementary Table 2. ICD-9 Codes categorized for possible etiologies for pericarditis.
Supplementary Table 3. Categorization of possible etiologies.
Supplementary Table 4. Distribution of excluded patients with potential causes for pericarditis according to a hierarchical model.
Sources of Funding
This work was supported by the Kostin Family Innovation Fund and the Farb Family Fund.
Disclosures
None.
References
- 1.Kuhn B, Peters J, Marx GR, Breitbart RE. Etiology, management, and outcome of pediatric pericardial effusions. Pediatr Cardiol. 2008; 29:90-94. [DOI] [PubMed] [Google Scholar]
- 2.Mok GC, Menahem S. Large pericardial effusions of inflammatory origin in childhood. Cardiol Young. 2003; 13:131-136. [DOI] [PubMed] [Google Scholar]
- 3.Ratnapalan S, Brown K, Benson L. Children presenting with acute pericarditis to the emergency department. Pediatr Emerg Care. 2011; 27:581-585. [DOI] [PubMed] [Google Scholar]
- 4.Imazio M, Bobbio M, Cecchi E, Demarie D, Demichelis B, Pomari F, Moratti M, Gaschino G, Giammaria M, Ghisio A, Belli R, Trinchero R. Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial. Circulation. 2005; 112:2012-2016. [DOI] [PubMed] [Google Scholar]
- 5.Imazio M, Bobbio M, Cecchi E, Demarie D, Pomari F, Moratti M, Ghisio A, Belli R, Trinchero R. Colchicine as first‐choice therapy for recurrent pericarditis: results of the CORE (COlchicine for REcurrent pericarditis) trial. Arch Intern Med. 2005; 165:1987-1991. [DOI] [PubMed] [Google Scholar]
- 6.Maisch B, Seferovic PM, Ristic AD, Erbel R, Rienmüller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004; 25:587-610. [DOI] [PubMed] [Google Scholar]
- 7.Imazio M, Demichelis B, Parrini I, Cecchi E, Demarie D, Ghisio A, Belli R, Bobbio M, Trinchero R. Management, risk factors, and outcomes in recurrent pericarditis. Am J Cardiol. 2005; 96:736-739. [DOI] [PubMed] [Google Scholar]
- 8.Fowler NO. Recurrent pericarditis. Cardiol Clin. 1990; 8:621-626. [PubMed] [Google Scholar]
- 9.Raatikka M, Pelkonen PM, Karjalainen J, Jokinen EV. Recurrent pericarditis in children and adolescents: report of 15 cases. J Am Coll Cardiol. 2003; 42:759-764. [DOI] [PubMed] [Google Scholar]
- 10.Yazigi A, Abou‐Charaf LC. Colchicine for recurrent pericarditis in children. Acta Paediatr. 1998; 87:603-604. [DOI] [PubMed] [Google Scholar]
- 11.Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI. Consensus‐based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2002; 123:110-118. [DOI] [PubMed] [Google Scholar]
- 12.Lotrionte M, Biondi‐Zoccai G, Imazio M, Castagno D, Moretti C, Abbate A, Agostoni P, Brucato AL, Di Pasquale P, Raatikka M, Sangiorgi G, Laudito A, Sheiban I, Gaita F. International collaborative systematic review of controlled clinical trials on pharmacologic treatments for acute pericarditis and its recurrences. Am Heart J. 2010; 160:662-670. [DOI] [PubMed] [Google Scholar]
- 13.Imazio M, Cecchi E, Demichelis B, Ierna S, Demarie D, Ghisio A, Pomari F, Coda L, Belli R, Trinchero R. Indicators of poor prognosis of acute pericarditis. Circulation. 2007; 115:2739-2744. [DOI] [PubMed] [Google Scholar]
- 14.Ghelani SJ, Spaeder MC, Pastor W, Spurney CF, Klugman D. Demographics, trends, and outcomes in pediatric acute myocarditis in the United States, 2006 to 2011. Circ Cardiovasc Qual Outcomes. 2012; 5:622-627. [DOI] [PubMed] [Google Scholar]
- 15.Frisancho‐Kiss S, Davis SE, Nyland JF, Frisancho JA, Cihakova D, Barrett MA, Rose NR, Fairweather D. Cutting edge: cross‐regulation by TLR4 and T cell Ig mucin‐3 determines sex differences in inflammatory heart disease. J Immunol. 2007; 178:6710-6714. [DOI] [PubMed] [Google Scholar]
- 16.Frisancho‐Kiss S, Nyland JF, Davis SE, Frisancho JA, Barrett MA, Rose NR, Fairweather D. Sex differences in coxsackievirus B3‐induced myocarditis: IL‐12Rbeta1 signaling and IFN‐gamma increase inflammation in males independent from STAT4. Brain Res. 2006; 1126:139-147. [DOI] [PubMed] [Google Scholar]
- 17.Lyden DC, Olszewski J, Feran M, Job LP, Huber SA. Coxsackievirus B‐3‐induced myocarditis. Effect of sex steroids on viremia and infectivity of cardiocytes. Am J Pathol. 1987; 126:432-438. [PMC free article] [PubMed] [Google Scholar]
- 18.Imazio M, Brucato A, Cemin R, Ferrua S, Maggiolini S, Beqaraj F, Demarie D, Forno D, Ferro S, Maestroni S, Belli R, Trinchero R, Spodick DH, Adler YICAP Investigators. A randomized trial of colchicine for acute pericarditis. N Engl J Med. 2013; 369:1522-1528. [DOI] [PubMed] [Google Scholar]
- 19.Imazio M, Brucato A, Cemin R, Ferrua S, Belli R, Maestroni S, Trinchero R, Spodick DH, Adler YCORP (COlchicine for Recurrent Pericarditis) Investigators. Colchicine for recurrent pericarditis (CORP): a randomized trial. Ann Intern Med. 2011; 155:409-414. [DOI] [PubMed] [Google Scholar]
- 20.Kallinich T, Haffner D, Rudolph B, Schindler R, Canaan‐Kühl S, Keitzer R, Burmester GR, Roesen‐Wolff A, Roesler J. “Periodic fever” without fever: two cases of non‐febrile TRAPS with mutations in the TNFRSF1A gene presenting with episodes of inflammation or monosymptomatic amyloidosis. Ann Rheum Dis. 2006; 65:958-960. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1. ICD-9 Diagnosis and Procedure codes along with their description, used for selection of discharges with pericarditis or pericardial effusion.
Supplementary Table 2. ICD-9 Codes categorized for possible etiologies for pericarditis.
Supplementary Table 3. Categorization of possible etiologies.
Supplementary Table 4. Distribution of excluded patients with potential causes for pericarditis according to a hierarchical model.


