Several years ago a commentary published in IJO entitled “BMI, fat mass, abdominal adiposity and visceral fat: where is the ‘beef’?” introduced several concepts related to the measurement of obesity and described the relationships among anthropometric and more direct measurements of adiposity.1 The 2007 commentary served to highlight the similarity in correlations between body mass index (BMI), waist circumference (WC) and total and abdominal visceral fat (AVF). Despite significant progress in the characterization of obesity in the past several years, there remains confusion as to the value and relative merits of using anthropometric measures to estimate total and specific body fat depots in both adults and children.
Here we extend the results presented by Bouchard1 to children and adolescents, and expand the model to include results from dual-energy x-ray absorptiometry (DXA). Our sample included 82 white girls, 118 African American girls, 97 white boys, and 83 African American boys, 5–18 years of age, with a range of BMI (kg/m2) across normal weight, overweight and obese categories. WC and BMI were obtained by trained technicians using standard techniques, while fat mass (FM) and trunk fat were assessed using a whole-body DXA scanner (Hologic QDR 4500A; Bedford, MA). AVF mass was assessed using a series of 5 to 8 cross-sectional abdominal MRI images (GE Signa Excite; GE Medical Systems, Milwaukee, WI).2 Age-adjusted partial correlations among the body composition variables were computed using the SAS statistical package V9.3 (SAS Institute Inc., Cary, NC). Correlations were computed separately in the four race-by-sex groups, and correlation means weighted by the number of subjects in each group were computed.
The results of the correlation analysis are presented in Figure 1. Within each of the four race-by-sex groups, the age-adjusted correlations between BMI and WC were very high (r = 0.96; range 0.93–0.97) as were correlations between fat mass and both BMI (r = 0.96; range 0.95–0.96) and WC (r = 0.95; range 0.94–0.97). Further, correlations between trunk fat and BMI (r = 0.94; range 0.92–0.96) and WC (r = 0.95; range 0.93–0.97) were also very high. As expected, correlations between AVF and BMI (r = 0.84 range 0.82–0.87), WC (r = 0.81; range 0.79–0.82) and FM (r = 0.83; range 0.81–0.84) were somewhat lower than the correlations with FM and trunk fat but were still quite strong. Further, the narrow ranges around each mean correlation demonstrate that there were no differences in the correlation patterns among the four race-by-sex groups.
Figure 1.
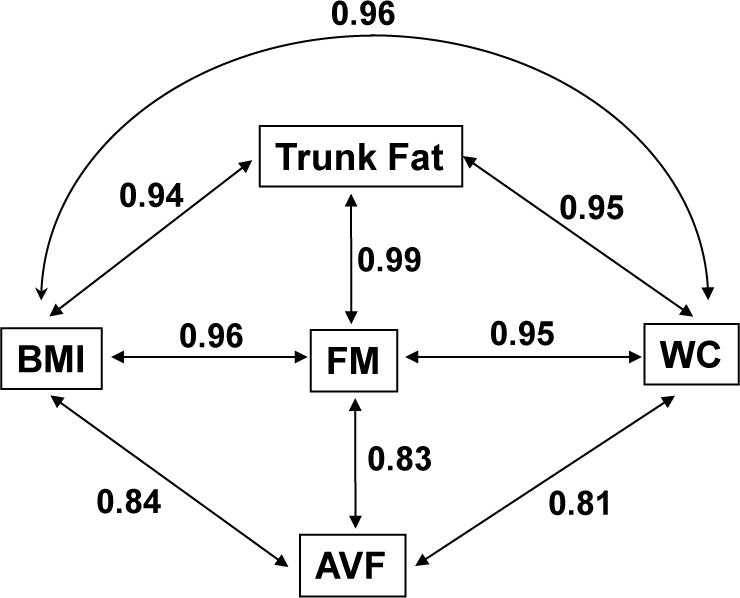
Age-adjusted partial correlations among body composition variables in a sample of 380 white and African American children and adolescents 5 to 18 years of age. Each correlation represents the weighted mean of the four age-by-race group correlations.
The results we have presented among children and adolescent are very similar to those presented for adults in the original commentary by Bouchard and the correlations are of comparable magnitude.1 Among adults, WC and abdominal sagittal diameter have often been identified as the best anthropometric markers of AVF among those available3,4, but WC is by far the most commonly used. However, as was previously shown among adults1,5 and now among children, WC is only partially representative of AVF level. Rather, WC is more highly correlated with total fat mass and BMI than it is with AVF, and should therefore first and foremost be considered a marker of total adiposity rather than AVF per se. Further, our analysis has shown that BMI and WC are equally correlated with AVF in children, albeit at a lower level than with total fat mass.
Based on this set of cross-sectional observations, it appears as though BMI performs as well as WC and DXA-derived fat mass in its association with AVF in youth. Recent advances using DXA have made the measurement of AVF more widely available.6,7 Thus, the assertion that anthropometric measurements can provide clinically relevant information with respect to AVF is doubtful and is based on a false assumption.
The present observations have considerable implications. For example, WC is a common component of clinical definitions of metabolic syndrome in both adults and children.8,9 Within the context of metabolic syndrome, WC is primarily viewed as a marker of “abdominal” obesity, as generalized obesity has not typically been considered as an important component of the syndrome.8,10 However, the degree to which WC contributes independent information regarding AVF per se to the definition of metabolic syndrome is likely minimal and doubtful, based on the results presented here. Indeed, the role of an “obesity marker” in the definition of metabolic syndrome in children and adolescents could be played equally well by BMI or a surrogate measure of total body fat, which WC ultimately is.
These results have implications for the diagnosis of obesity-related health concerns among children, as well as the assessment of total and regional adiposity in growth studies. For example, it is unlikely that we will be able to characterize age-related changes in depot-specific adiposity using anthropometric measurements. If the intention is to have an assessment of AVF in children, it is unlikely that WC or any other anthropometric measures can provide a valid quantification of the true size of the visceral fat depot. But WC is a better surrogate for total adiposity and it performs equally well as BMI in children and in adults.
Acknowledgments
The source of support for this work was provided by National Institutes of Health grant # RC1DK086881-01.
Footnotes
Clinical Trials Registration: ClinicalTrials.gov: identifier NCT01595100
Conflict of Interest: The authors declare no conflict of interest.
References
- 1.Bouchard C. BMI, fat mass, abdominal adiposity and visceral fat: where is the ‘beef’? Int J Obes Relat Metab Disord. 2007;31:1552–1553. doi: 10.1038/sj.ijo.0803653. [DOI] [PubMed] [Google Scholar]
- 2.Staiano AE, Broyles ST, Gupta AK, Katzmarzyk PT. Ethnic and sex differences in visceral, subcutaneous, and total body fat in children and adolescents. Obesity. 2013 doi: 10.1002/oby.20210. Epub Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rankinen T, Kim SY, Perusse L, Despres JP, Bouchard C. The prediction of abdominal visceral fat level from body composition and anthropometry: ROC analysis. Int J Obes Relat Metab Disord. 1999;23(8):801–809. doi: 10.1038/sj.ijo.0800929. [DOI] [PubMed] [Google Scholar]
- 4.Pouliot MC, Despres JP, Lemieux S, Moorjani S, Bouchard C, Tremblay A, et al. Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am J Cardiol. 1994;73(7):460–468. doi: 10.1016/0002-9149(94)90676-9. [DOI] [PubMed] [Google Scholar]
- 5.Barreira TV, Staiano AE, Harrington DM, Heymsfield SB, Smith SR, Bouchard C, et al. Anthropometric correlates of total body fat, abdominal adiposity, and cardiovascular disease risk factors in a biracial sample of men and women. Mayo Clin Proc. 2012;87(5):452–460. doi: 10.1016/j.mayocp.2011.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaul S, Rothney MP, Peters DM, Wacker WK, Davis CE, Shapiro MD, et al. Dual-energy X-ray absorptiometry for quantification of visceral fat. Obesity. 2012;20:1313–1318. doi: 10.1038/oby.2011.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Micklesfield LK, Goedecke JH, Punyanitya M, Wilson KE, Kelly TL. Dual-energy x-ray performs as well as clinical computed tomography for the measurement of visceral fat. Obesity. 2012;20:1109–1114. doi: 10.1038/oby.2011.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the Metabolic Syndrome. A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 9.Ford ES, Li C. Defining the metabolic syndrome in children and adolescents: will the real definition please stand up? J Pediatr. 2008;152(2):160–164. doi: 10.1016/j.jpeds.2007.07.056. [DOI] [PubMed] [Google Scholar]
- 10.Balkau B, Charles MA. Comment on the provisional report from the WHO consultation. European Group for the Study of Insulin Resistance (EGIR) Diabet Med. 1999;16(5):442–443. doi: 10.1046/j.1464-5491.1999.00059.x. [DOI] [PubMed] [Google Scholar]


