Abstract
Objective
While current practice guidelines promote exercise for chronic back and neck pain, little is known about exercise prescription in routine care. The objective of this study was to describe exercise prescription in routine clinical practice for individuals with chronic back or neck pain.
Methods
Computer-assisted telephone survey of a representative sample of individuals with chronic back or neck pain who saw a physician (MD), chiropractor (DC) and/or physical therapist (PT) in the past 12 months (n=684). Individuals were asked whether they were prescribed exercise, the amount of supervision received, and type, duration, and frequency of the prescribed exercise. Descriptive and multivariable regression analyses were conducted.
Results
48% of subjects were prescribed exercise. Of those prescribed exercise, 46% received the prescription from a PT, 29% from an MD, 21% from a DC, and 4% from other. In multivariable analyses, seeing a PT or a DC were the strongest predictors of exercise prescription. Being female, more educated, and on worker’s compensation also increased the likelihood of exercise prescription. Relative to MDs and DCs, PTs were more likely to provide supervision and prescribe strengthening exercises. Relative to MDs, PTs were more likely to prescribe stretching exercises.
Conclusions
Our findings suggest that exercise is being underutilized as a treatment for chronic back and neck pain and, to some extent, that the amount of supervision and types of exercises prescribed do not follow current practice guidelines. Exercise prescription provided by PTs appears to be most in line with current guidelines.
Exercise is a common treatment for individuals with chronic low back or neck pain and is used to improve physical function and decrease symptoms (e.g., pain, stiffness). Exercise has also been used to minimize disability by decreasing individuals’ fears about pain during movement and by reshaping their attitudes and beliefs about their pain. The latter goal is common in cognitive behavioral and functional restoration programs that typically use a quota-based, non-pain contingent approach to exercise.1
In the past decade, a number of randomized trials, systematic reviews, and clinical practice guidelines have supported the use of exercise for the treatment of chronic low back pain (LBP) 2–14 and chronic neck pain.15–19 While there is still much to learn about the types and intensity of exercises that are most effective, recent meta-analyses by Hayden and colleagues suggest individually tailored, supervised exercise programs that include stretching and strengthening are associated with the best outcomes for individuals with chronic LBP.5, 6 Hayden et al. also found that exercise in combination with other conservative treatments and “high dose” exercise, defined as an exercise intervention with a total time of 20 hours or more, improved pain and function more than exercise alone or “low dose” exercise.6
The findings for chronic neck pain are similar, though somewhat less definitive, with data suggesting that certain types of exercise are most effective and supervised exercise is more effective than non-supervised exercise. According to evidence statements on the treatment of chronic neck pain published by the Bone and Joint Decade 2000–2010 Task Force on Neck Pain, supervised and home exercise plus advice is marginally more effective than advice alone for chronic whiplash associated disorders; a neck exercise program alone or in combination with spinal manipulation is more effective than spinal manipulation alone, TENS, or usual care for chronic “non-specific” neck pain; and both endurance (repetitive, submaximal resistance exercises) and strengthening exercises (repetitive, maximal resistance exercises) are effective treatments for chronic “non-specific” neck pain.19 Data also suggest that aerobic exercise and stretching alone are less effective than endurance and strengthening exercises,20, 21 and that stretching exercises for the neck are as effective as manual therapy.22 Evidence on the additive effect of other conservative treatments in combination with exercise for the treatment of chronic neck pain is less clear. There are some data to suggest that multimodal approaches that include exercise may be more effective than single treatment approaches.23, 24
While the past decade has led to gains in our understanding of the efficacy of exercise for chronic low back and neck pain, less is known about exercise prescription in routine clinical practice. Who is prescribing it? Who is getting it? What is being prescribed? Such information would be useful in assessing the translation of research findings to clinical practice and in identifying areas to target for increased promotion of exercise as an effective treatment.
We analyzed data from a population-based survey of healthcare provider and treatment use by individuals with chronic low back or neck pain to gain a better understanding of the use of exercise in the treatment of these conditions. Our specific objectives were: 1) to determine the extent to which exercise is prescribed by physicians, physical therapists (PTs), and chiropractors for the treatment of chronic low back and neck pain; 2) to identify demographic, insurance, work, and health-related characteristics associated with exercise prescription; 3) to describe the amount of supervision provided and types of exercises prescribed for each provider type; and 4) to determine the extent to which other conservative treatments are used in combination with exercise.
PATIENTS and METHODS
Data for this study come from a larger study on back and neck pain prevalence and health care use in North Carolina.25 A cross-sectional, computer-assisted telephone survey of a representative sample of North Carolina residents was conducted in the parent study to identify a sample of adults with chronic low back or neck pain. These individuals were then surveyed on their health and health care use, including exercise prescription.
Sample Selection
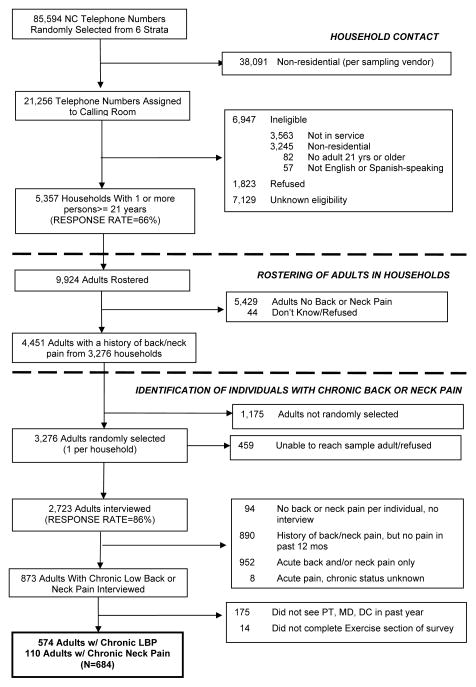
Figure 1 outlines the sampling strategy for the parent study and this study. A stratified, probability sample (stratified by region and race) of North Carolina telephone numbers was obtained from a sampling vendor.26 5,357 households were contacted and 9,924 adults 21 years or older were rostered. The household response rate was 66 percent, computed as the sum of households interviewed divided by the sum of eligible households plus an estimate of the proportion of households with unknown eligibility.27 Of the 9,924 rostered adults, 4,451 adults from 3,276 households had a history of back and/or neck pain, defined as any kind of back or neck problem in the past few years. One adult from each of these households was randomly selected to be interviewed in more detail (n=3,276) and 2,723 adults were interviewed for an individual response rate of 86 percent. Relative to responders, non-responders were similar in age and race, but were more likely to be male (chi square test, p<.001).
FIGURE 1.
2006 Sample Selection
Of adults interviewed, 873 had chronic low back or neck pain. Low back pain was defined as pain at the level of the waist or below, with or without buttock and/or leg pain. Neck pain was defined as pain in the neck area with or without pain in the shoulders or arms. Chronic pain was defined as pain and activity limitations for the past three months; or greater than 24 episodes of activity-limiting pain in the past year. Individuals were first asked about back pain and if chronic, completed the back pain module of the survey. These individuals may have had a history of neck pain. This approach was taken because one objective of the parent study was to emulate methods used by our group in an earlier study on back pain prevalence.28
The sample for this analysis consisted of individuals with chronic back or neck pain who saw one or more of the following providers: physician, chiropractor, or PT in the past year and who completed the exercise section of the survey (n=684, 574 chronic back and 110 chronic neck).
Survey Instrument
The survey instrument for this study was an expansion of a computer-assisted survey instrument fielded in 1992.28 The 1992 survey addressed the prevalence of acute and chronic low back pain and health care use in North Carolina. A Spanish version of the instrument was created because the Latino population of North Carolina had grown significantly since 1992. Prior to data collection, the University of North Carolina at Chapel Hill Survey Research Unit (UNC-SRU) piloted the survey instrument on a random sample of North Carolina residents (n=84). Subjects stated that the numerous questions relating each of the treatments to the provider who administered the treatment were cumbersome. Many of these questions, therefore, were eliminated.
The back pain module included a series of questions on symptoms (e.g. pain intensity, presence of extremity pain/weakness), general health status (Medical Outcomes Survey SF-12), functional status (Roland-Morris Disability Questionnaire)29, provider and treatment use in the past year, and medication use in the past 30 days. The module ended with more detailed questions on insurance, employment, and demographic characteristics. The neck pain module had a similar design with the Neck Disability Index30 as the condition-specific measure of functional status.
Exercise Section of Survey
Both the back and neck pain modules included a series of questions on exercise. Individuals were first asked whether they received exercise or posture instruction from a doctor or therapist in the past 12 months. Those who said yes were then asked to identify the provider type (response categories - medical doctor, chiropractor, PT, other) and the amount of supervision (response categories - supervised, on your own, both). For data analysis, the supervision data were dichotomized as supervised (“supervised” or “both”) or not supervised (“on your own”). Respondents were then asked whether they received instruction in each of the following types of exercise: walking, stretching, strengthening, range of motion, and posture. For each type of exercise, respondents were queried about the duration (number of minutes spent on the exercise) and frequency (number of times/week) that they performed the exercises.
Analytic Framework
We hypothesized that patients’ demographic, insurance, work, and health-related characteristics, along with types of providers seen in the past year, would be associated with exercise prescription. Variability in exercise prescription by demographic characteristics may represent underlying group differences in the attitudes/beliefs of the patients and/or providers regarding exercise prescription. Insurance and work-related characteristics may also influence whether a provider prescribes exercise. For example, individuals on worker’s compensation for back pain likely have physically demanding jobs and may require specific exercises/conditioning before they return to work. Health-related characteristics of the individuals may also influence whether a provider prescribes exercise. There are data to suggest that individuals with certain health-related characteristics are more or less likely to benefit from exercise.31–34 Finally, provider type seen may also be associated with exercise prescription. Exercises, for example, are a treatment often provided by PTs.35
The specific variables included in our analyses were chosen based on our analytic framework and availability. Demographic variables included age, sex, race, and education. Insurance and work-related variables included whether subjects had any one of the following: private insurance, Medicare, Medicaid, Worker’s Compensation, disability insurance, no insurance/compensation; and whether the subject was employed in the past year. Providers seen included whether the individual saw a physician, PT, or chiropractor in the past year. Health-related characteristics included average pain intensity in the past three months (0–10 scale), years with chronic pain, presence of extremity pain and weakness, fair/poor general health rating, SF-12 physical and mental component scores, Roland-Morris Disability scores, Neck Disability Index scores, narcotic medication use in the past 30 days, location of pain (i.e., neck or back), and whether the patient had spinal surgery in the past year.
Data Analysis
All analyses were conducted using sampling weights and the survey commands in Stata (ver 9.2; Stata Corporation, 4905 Lakeway Drive, College Station, TX). Missing data ranged from 0 to 9 percent. With the exception of SF-12 scores, these missing values were not imputed, resulting in casewise exclusion from statistical analyses. For individuals with fewer than six missing items on the SF-12 (n=33), a regression-based multi-pattern imputation using the available items was conducted.36
Descriptive statistics were used to characterize individuals by whether they received exercise prescription. Two sample t-tests and chi-square tests of proportions were conducted to determine differences in the characteristics of the two groups. Multivariable logistic regression analyses were then conducted to determine the demographic, insurance, work-related, health-related, and provider use characteristics associated with exercise prescription. Because type of provider seen appeared to be a strong predictor of exercise prescription, we estimated two models, one that included only demographic, insurance, work and health characteristics; and one that included these variables and the provider use variables. For the multivariable analyses, the following health-related variables were not included because they were not applicable to all individuals: pain duration, Roland-Morris Disability score, and Neck Disability Index scores. The latter two variables were also highly correlated with the SF-12 PCS scores.
For individuals who were prescribed exercise, descriptive statistics on the amount of supervision, types of exercise, and duration and frequency of exercise were generated by provider type. For each individual, we also calculated a measure of total exercise time/week by summing the exercise intensity (duration X frequency) for each prescribed exercise. Tests of differences in means and proportions of the three groups were conducted using logistic regression analyses, with the exercise characteristic as the dependent variable and provider types as the independent variables. For individuals who were prescribed exercise, we also generated descriptive statistics on other types of conservative treatments used in the past year.
RESULTS
Forty-eight percent of subjects who saw a physician, PT, and/or chiropractor in the past year were prescribed exercise. Of those who were prescribed exercise, 46.0 percent received the prescription from a PT, 28.6 percent from a physician, 20.9 percent from a chiropractor, and 4.6 percent from other (more than one provider or not specified).
Table 1 presents descriptive data on exercise prescription by provider type, conditional on seeing the provider. Of those who saw a PT, 63.8 percent were prescribed exercise. Of those who saw a chiropractor, 33.1 percent were prescribed exercise; and of those who saw a physician, 14.4 percent were prescribed exercise. When we stratified our analyses by location (i.e., back or neck) the percentages were similar and not statistically different.
Table 1.
Exercise Prescription By Provider Type
| PROVIDER TYPE | SAW PROVIDER IN PAST YR. Percentage (95% CI) | PRESCRIBED EXERCISEa Percentage (95% CI) |
|---|---|---|
| Physician ((MD) | 94. 4 (92.0 – 96.1) | 14.4 (11.6 – 17.7) |
| Physical Therapist (PT) | 34.2 (30.4 – 38.3) | 63.8 (56.7 – 70.3) |
| Chiropractor (DC) | 30.0 (26.1 – 34.1) | 33.1 (26.0 – 41.2) |
| MD, PT, or DC | 100 | 47.5 (43.3 – 51.8) |
conditional on seeing provider
While most subjects in the sample saw a physician, only 14.4 percent were prescribed exercise. Some individuals who saw a physician and were not prescribed exercise saw a PT who did. Of those subjects who saw a physician and did not receive exercise instruction, 26.3 percent saw a PT who did prescribe exercise and 9.7 percent saw a chiropractor who did prescribe exercise.
Table 2 presents the demographic, insurance, work-related, and health-related characteristics of the sample by exercise prescription. In bivariate comparisons, individuals who were female, more educated, on worker’s compensation, employed in the past year, saw a PT, or saw a chiropractor were more likely to receive exercise prescription. The number of patient visits also increased the likelihood of exercise prescription by chiropractors. Individuals who were on Medicare, reported poorer general health, or reported greater physical disability were less likely to be prescribed exercise. Variables that approached significance and were associated with an increased likelihood of exercise prescription were younger age, private insurance, not taking narcotics, and more physical therapy visits.
Table 2.
Demographic and Clinical Characteristics by Exercise Prescription (N=684)
| CHARACTERISTIC | Exercise Prescription
|
P value | |
|---|---|---|---|
| NO (N=361) | YES (N=323) | ||
| Demographic Characteristics | |||
| Mean age (yrs.) | 53.4 | 51.6 | .15 |
| Sex (%): | |||
| Female | 57.7 | 66.5 | .04 |
| Race (%): | |||
| Non-Hispanic White | 73.5 | 73.3 | |
| Non-Hispanic Black | 16.9 | 16.4 | .31 |
| Non-Hispanic Other | 6.5 | 4.2 | |
| Hispanic | 3.2 | 6.1 | |
| Education (%): | |||
| <High school | 20.4 | 12.7 | |
| High school | 33.4 | 24.2 | <.001 |
| >High school | 46.2 | 63.2 | |
| Insurance & Work-Related Characteristics | |||
| Insurancea (%): | |||
| Private | 57.2 | 65.8 | .05 |
| Medicare & 62 years or older | 21.8 | 17.7 | .23 |
| Medicaid | 12.9 | 16.6 | .21 |
| Worker’s Compensation | 4.9 | 11.5 | .003 |
| Disability or Medicare & < 62 years | 27.7 | 21.4 | .10 |
| None | 14.3 | 11.8 | .42 |
| Employed in Past Yr. (%) | 18.2 | 26.7 | <.001 |
| Health-Related Characteristics | |||
| Pain Location (%): | |||
| Back | 84.8 | 81.5 | .32 |
| Neck | 15.3 | 18.5 | |
| Mean Duration of Problem (yrs.)b | 9.6 | 9.0 | .57 |
| Fair or poor general health (%) | 44.8 | 34.0 | .01 |
| Mean SF-12 Physical Health Component | 30.2 | 32.7 | .005 |
| Mean SF-12 Mental Health Component | 48.0 | 47.9 | .95 |
| Mean Roland-Morris Score c | 16.2 | 14.6 | .008 |
| Mean Neck Disability Index d | 33.1 | 32.0 | .72 |
| Mean Pain Ratinge in Past 3 mos. | 6.8 | 6.6 | .26 |
| Have Extremity Pain (%) | 69.9 | 72.9 | .45 |
| Have Extremity Weakness (%) | 57.4 | 56.3 | .81 |
| Taking Narcotics for Back or Neck Pain (%) | 60.2 | 52.3 | .07 |
| Had Spinal Surgery in Past Yr. (%) | 7.5 | 9.0 | .52 |
| Providers Seen | |||
| Saw a physician in past year (%) | 94.5 | 94.2 | .86 |
| Mean visitsf | 9.2 | 9.7 | .73 |
| Saw a physical therapist in past year (%) | 12.5 | 58.2 | <.001 |
| Mean visitsf | 12.7 | 17.9 | .11 |
| Saw a chiropractor in past year (%) | 18.2 | 43.0 | <.001 |
| Mean visitsf | 16.2 | 27.4 | .02 |
categories not mutually exclusive;
n=619, excludes subjects who reported >24 episodes of pain in past year;
n=574, back pain only;
n=110, neck pain only;
on 0–10 scale;
conditional on seeing provider
Table 3 presents the results of the multivariable logistic regression analyses. In model 1, being female, more educated, on worker’s compensation, on Medicaid, or employed in the past year increased the likelihood of receiving exercise prescription. Location of pain (back or neck) was not related to exercise prescription. When provider use variables were added (Model 2), being female, more educated, or on worker’s compensation continued to increase the likelihood of exercise prescription. The types of provider seen in the past year were the strongest predictors of exercise prescription. None of the health-related variables were associated with exercise prescription.
Table 3.
Multivariable Logistic Regression Analysis of Patient-Level Characteristics Associated with Exercise Prescription
| MODEL 1 | MODEL 2 | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| CHARACTERISTIC | Odds Ratio | 95% C.I. | P Value | Odds Ratio | 95% C.I. | P Value |
| Demographic | ||||||
| Age | 0.99 | (0.97 – 1.01) | 0.477 | 0.99 | (0.96 – 1.01) | 0.240 |
| Female | 1.80 | (1.20 – 2.71) | 0.005 | 2.04 | (1.26 – 3.28) | 0.004 |
| White | 1.26 | (0.82 – 1.94) | 0.297 | 1.38 | (0.82 – 2.33) | 0.226 |
| > HS education | 1.83 | (1.24 – 2.69) | 0.002 | 1.85 | (1.19 – 2.88) | 0.007 |
| Insurance & Work | ||||||
| Private | 1.54 | (0.83 – 2.87) | 0.174 | 1.50 | (0.65 – 3.46) | 0.341 |
| Medicare | 1.37 | (0.67 – 2.81) | 0.394 | 1.66 | (0.73 – 3.81) | 0.228 |
| Medicaid | 2.33 | (1.21 – 4.48) | 0.011 | 1.84 | (0.82 – 4.13) | 0.139 |
| WC Ins. | 2.55 | (1.24 – 5.25) | 0.011 | 2.39 | (1.23 – 4.67) | 0.011 |
| Disability Ins. | 1.16 | (0.66 – 2.03) | 0.607 | 1.58 | (0.84 – 2.99) | 0.159 |
| No Insurance | 1.21 | (0.53 – 2.79) | 0.654 | 1.71 | (0.61 – 4.83) | 0.310 |
| Employed past yr. | 1.89 | (1.18 – 3.03) | 0.008 | 1.63 | (0.96 – 2.76) | 0.068 |
| Health-Related | ||||||
| SF-12 PCS | 1.02 | (1.00 – 1.05) | 0.071 | 1.01 | (0.99 – 1.04) | 0.366 |
| SF-12 MCS | 1.00 | (0.98 – 1.02) | 0.753 | 1.00 | (0.98 – 1.02 | 0.703 |
| Extremity Pain | 1.35 | (0.87 – 2.10) | 0.183 | 0.99 | (0.61 – 1.63) | 0.983 |
| Extremity Weak | 1.27 | (0.83 – 1.94) | 0.271 | 1.25 | (0.77 – 2.03) | 0.364 |
| Pain Intensity | 1.00 | (0.91 – 1.11) | 0.951 | 1.02 | (0.91 – 1.13) | 0.778 |
| Taking Narcotics | 0.81 | (0.54 – 1.20) | 0.294 | 0.70 | (0.44 – 1.13) | 0.141 |
| Surgery in Past Yr. | 1.12 | (0.57 – 2.20) | 0.751 | 0.67 | (0.29 – 1.55) | 0.350 |
| Back Pain | 1.09 | (0.65 – 1.82) | 0.753 | 1.39 | (0.73 – 2.62) | 0.313 |
| Providers Seen | ||||||
| Saw MD | 2.01 | (0.76 – 5.31) | 0.161 | |||
| Saw PT | 11.96 | (7.15 – 20.01) | <.001 | |||
| Saw DC | 4.40 | (2.55 – 7.57) | <.001 | |||
There were some differences in the amount of supervision and types exercises prescribed by the different providers (Table 4). PTs were more likely to provide supervision relative to physicians and chiropractors. PTs were also more likely than physicians to prescribe stretching. Findings that approached significance included PTs being more likely to prescribe strengthening exercises and less likely to prescribe walking. There were few differences among providers in regard to duration of exercise with the exception of PTs prescribing walking for a shorter and stretching for a longer duration. There were no differences in exercise frequency, generally fives times/week. The total exercise time per week also did not vary by provider and was generally about 3.5 hours/week.
Table 4.
Exercise Characteristics by Providers Who Prescribed Exercise (n=684)
| EXERCISE CHARACTERISTIC | Physical Therapist (PT) | Physician (MD) | Chiropractor (DC) | Significant Differences (P<.10) |
|---|---|---|---|---|
| Provided Supervision (%) | 65.5 | 29.3 | 28.6 | PT > MD, DC (P<.001) |
| Type of Exercise (%): | ||||
| Walking | 52.2 | 70.1 | 50.8 | PT < MD (P=.09) |
| Stretching | 92.2 | 75.6 | 87.3 | PT > MD (P=.003) |
| Strengthening | 70.1 | 56.4 | 55.8 | PT > MD (P=.05) PT > DC (P=.08) |
| Range of Motion | 81.2 | 71.7 | 76.4 | NS |
| Posture | 43.3 | 37.6 | 39.5 | NS |
| Mean Duration (mins/session): | ||||
| Walking | 20.6 | 27.4 | 28.1 | PT < MD (P=.02) PT < DC (P=.08) |
| Stretching | 15.8 | 10.3 | 11.6 | PT > MD (P=.003) PT > DC (P=.04) |
| Strengthening | 17.8 | 16.8 | 13.9 | NS |
| Range of Motion | 13.5 | 10.7 | 10.9 | NS |
| Posture | 15.1 | 14.4 | 10.7 | NS |
| Mean Frequency (times/wk): | ||||
| Walking | 5.1 | 4.7 | 4.8 | NS |
| Stretching | 5.6 | 5.7 | 5.8 | NS |
| Strengthening | 4.7 | 5.4 | 4.7 | NS |
| Range of Motion | 4.8 | 5.5 | 5.9 | NS |
| Posture | 5.4 | 4.6 | 4.2 | NS |
| Mean total mins. of ex/wk | 266 | 228 | 210 | NS |
Of those prescribed exercise, 86 percent used one or more additional conservative, physical treatments with a mean of three treatments. Heat, cold and electrical stimulation were the most common additional treatments for subjects with back pain, while heat, cold, and manipulation were most common for subjects with neck pain. Medication use was also quite high in those prescribed exercise.
DISCUSSION
Less than 50 percent of the subjects in our sample were prescribed exercise, one of the few moderately effective therapies for the highly disabling illness of chronic back and neck pain. Provider type seen played a major role in whether individuals received exercise prescription and was more influential than any of the other patient-related factors. These findings agree with other studies on the care of back pain that have found that “who you see, is what you get.”37, 38
As might be expected, PTs were most likely to prescribe exercise; however, approximately one-third of individuals who saw a PT did not receive exercise prescription. Chiropractors were the next most likely to prescribe exercise and were more likely to do so if they saw the patient more often. While physicians were least likely to prescribe exercise, some patients who saw a physician were prescribed exercise by a PT or chiropractor. Patients who saw a PT were likely referred by a physician. Patients who saw a chiropractor, may have had a physician referral for chiropractic care, though this is not common.39 Still, less than half of the subjects who saw a physician were prescribed exercise by any provider. Considering current evidence on the efficacy of exercise, these findings demonstrate that exercise is being underutilized as a treatment for chronic back and neck pain.
In bivariate analyses, individuals with poorer measures of health and function were less likely to receive exercise prescription. However, in multivariate analyses, this relationship was not maintained. Contrary to what we hypothesized, none of the health-related characteristics predicted whether an individual was prescribed exercise. While there are some data to suggest that individuals with different degrees of impairment respond more or less favorably to exercise, 33, 34, 40–44 providers’ decisions to prescribe exercise did not appear to be influenced by the degree of impairment. Our findings disagree with the literature on factors associated with physician advice to exercise as a preventive intervention. Several studies have found that, in general population, individuals with poorer health status were more likely to receive physician advice to exercise.45–47
We also found that females, people with a higher education level, and those on worker’s compensation are more likely to be prescribed exercise, controlling for other demographic and health-related characteristics and provider type. Others have reported a positive association between physician prescription of physical activity and female gender and education level.45, 48 Studies also suggest that females and more educated individuals are more likely to be active participants in their care which in turn affects the way the provider interacts with the patient and ultimately leads to more commitment to treatment regimens.49, 50 Our findings regarding worker’s compensation seem reasonable, since individuals on worker’s compensation are likely physical laborers who were injured on the job and are being treated with the goal of return to work.
For those who were prescribed exercise, the type of provider seen determined the amount of supervision received and, to some extent, the types of exercises prescribed. PTs were much more likely to provide supervision and were more likely to prescribe stretching and strengthening exercises. Current systematic reviews and practice guidelines for the treatment of chronic LBP and neck pain suggest that exercise supervision and the inclusion of strengthening exercises lead to better outcomes.5, 6, 19 For chronic LBP, stretching exercises have also been included in recommendations.5, 6 In addition, there is evidence to support the combination of treatments and/or multimodal approaches to care.6, 23, 24 Most of the subjects in the study were using a combination of conservative treatments, with varying levels of evidence to support their use.3, 51
There was a tendency toward physicians being more likely to prescribe walking and less likely to prescribe strengthening exercises, relative to PTs. This finding may be related to time constraints and/or comfort level of the physician. Instructions on walking can be given fairly quickly with little explanation and no need for demonstration or performance by the patient.
All types of providers appeared to provide therapeutic levels of exercise duration, with patients instructed to exercise for a total of approximately 3.5 hours a week. Following these guidelines for 6 weeks would achieve the high dosage rate of 20 hours that has been recommended for the treatment of chronic LBP.6
This study has some limitations, the most significant one being that we relied on patient self-report regarding exercise prescription, type, frequency, and duration. Responses to the questions may have been subject to social desirability bias. In debriefing of pilot respondents during instrument pre-testing, understanding of the exercise questions was good. A few subjects were unclear on what was meant by range of motion exercises. Nonetheless, we are unable to verify the accuracy with which subjects categorized their exercises and recalled instructions on duration and frequency. More importantly, we have no data on the duration that they actually exercised. There may also have been issues with subject recall (i.e., not remembering they were prescribed exercise). While not specific to the exercise questions, we did conduct a pilot study to assess how well individuals recalled number of provider visits in the past year. When compared with chart abstraction, the correlation between the two measures of visit number was 0.83.
We believe our population-based study provides valuable information that is currently lacking in the literature regarding exercise prescription in every day practice. Our findings suggest that exercise is being underutilized as a treatment for chronic back and neck pain and, to some extent, that the amount of supervision and types of exercises prescribed do not follow current practice guidelines. While exercise prescription provided by PTs appears to be most in line with current guidelines, there is much room for improvement by all types of providers who prescribe exercise for patients with chronic back and neck pain.
Future research should utilize other research designs (e.g., cohort) and sources of data (e.g., provider report, claims data) to gather information regarding exercise prescription. Future research should also further explore provider-level characteristics and additional patient-level characteristics associated with exercise prescription, as well as barriers to prescription of and adherence to exercise treatments. Barriers to exercise prescription may include practitioner knowledge, organizational aspects of the practice, and relatively poor reimbursement for exercise instruction compared with other modes of back and neck treatment. Patient-provider collaborative models of care, provider-provider collaborative models of care, and provider training models should also be explored to determine models that are most effective in facilitating the initiation of and compliance with an exercise program.
Table 5.
Use of Other Physical Treatments and Medications by Those Prescribed Exercise (N=684)
| Back | Neck | |||
|---|---|---|---|---|
|
| ||||
| Percentage | 95% C.I. | Percentage | 95% C.I. | |
| Physical Treatment | ||||
| Heat | 55.5 | (48.9 – 62.1) | 73.2 | (59.4 – 86.9) |
| Cold | 53.0 | (46.6 – 59.5) | 52.5 | (36.1 – 68.9) |
| Electrical Stimulation | 34.9 | (28.7 – 41.2) | 40.1 | (23.8 – 56.3) |
| Manipulation | 32.1 | (25.8 – 38.4) | 48.9 | (34.1 – 63.8) |
| Massage | 26.7 | (20.7 – 32.6) | 37.2 | (21.4 – 53.0) |
| TENS | 25.1 | (19.3 – 31.0) | 34.6 | (18.7 – 50.5) |
| Ultrasound | 24.1 | (18.4 – 29.8) | 39.2 | (23.2 – 55.3) |
| Acupuncture | 10.6 | (6.3 – 14.9) | 2.3 | (0.0 – 5.5) |
| Traction | 9.0 | (5.0 – 13.0) | 22.6 | (8.2 – 36.9) |
| Medications | ||||
| Over-the-counter pain medications | 96.9 | (94.7 – 99.1) | 95.7 | (88.8 – 102.5) |
| Narcotics | 55.5 | (48.8 – 62.2) | 37.0 | (21.2 – 52.8) |
| Prescription NSAIDS | 43.9 | (37.3 – 50.6) | 32.9 | (18.3 – 47.4) |
| Muscle relaxants | 31.5 | (25.2 – 37.7) | 31.3 | (16.6 – 46.0) |
| Anti-depressants | 31.5 | (25.2 – 37.8) | 27.5 | (13.4 – 41.5) |
| TCA/Anti-convulsant | 21.3 | (15.7 – 26.8) | 6.0 | (0.00 – 12.8) |
Acknowledgments
Financial Support:
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) R01 AR051970
National Research Service Award (NRSA) Institutional Training Grant from the Agency for Healthcare Research and Quality (T32 HS000032)
National Research Service Award (NRSA) Institutional Training Grant from the National Institute of Nursing Research (NINR) T32 NR08856
References
- 1.Rainville J, Hartigan C, Martinez E, Limke J, Jouve C, Finno M. Exercise as a treatment for chronic low back pain. Spine J. 2004;4:106–15. doi: 10.1016/s1529-9430(03)00174-8. [DOI] [PubMed] [Google Scholar]
- 2.Airaksinen O, Brox JI, Cedraschi C, et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 15(Suppl 2):S192–300. doi: 10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chou R, Huffman LH. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147:492–504. doi: 10.7326/0003-4819-147-7-200710020-00007. [DOI] [PubMed] [Google Scholar]
- 4.Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 147:478–91. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 5.Hayden JA, van Tulder MW, Malmivaara AV, Koes BW. Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med. 2005;142:765–75. doi: 10.7326/0003-4819-142-9-200505030-00013. [DOI] [PubMed] [Google Scholar]
- 6.Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005;142:776–85. doi: 10.7326/0003-4819-142-9-200505030-00014. [DOI] [PubMed] [Google Scholar]
- 7.Long A, Donelson R, Fung T. Does it matter which exercise? A randomized control trial of exercise for low back pain. Spine. 2004;29:2593–602. doi: 10.1097/01.brs.0000146464.23007.2a. [DOI] [PubMed] [Google Scholar]
- 8.Machado LA, de Souza MS, Ferreira PH, Ferreira ML. The McKenzie method for low back pain: a systematic review of the literature with a meta-analysis approach. Spine. 2006;31:E254–62. doi: 10.1097/01.brs.0000214884.18502.93. [DOI] [PubMed] [Google Scholar]
- 9.Moffett JK, Torgerson D, Bell-Syer S, et al. Randomised controlled trial of exercise for low back pain: clinical outcomes, costs, and preferences. BMJ. 1999;319:279–283. doi: 10.1136/bmj.319.7205.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clare HA, Adams R, Maher CG. A systematic review of efficacy of McKenzie therapy for spinal pain. Aust J Physiother. 2004;50:209–16. doi: 10.1016/s0004-9514(14)60110-0. [DOI] [PubMed] [Google Scholar]
- 11.Hayden JA, van Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev. 2005:CD000335. doi: 10.1002/14651858.CD000335.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kool J, de Bie R, Oesch P, Knusel O, van den Brandt P, Bachmann S. Exercise reduces sick leave in patients with non-acute non-specific low back pain: a meta-analysis. J Rehabil Med. 2004;36:49–62. doi: 10.1080/16501970310020104. [DOI] [PubMed] [Google Scholar]
- 13.Liddle SD, Baxter GD, Gracey JH. Exercise and chronic low back pain: what works? Pain. 2004;107:176–90. doi: 10.1016/j.pain.2003.10.017. [DOI] [PubMed] [Google Scholar]
- 14.McNeely ML, Torrance G, Magee DJ. A systematic review of physiotherapy for spondylolysis and spondylolisthesis. Man Ther. 2003;8:80–91. doi: 10.1016/s1356-689x(02)00066-8. [DOI] [PubMed] [Google Scholar]
- 15.Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions for neck pain. Phys Ther. 2001;81:1701–17. [PubMed] [Google Scholar]
- 16.Gross AR, Goldsmith C, Hoving JL, et al. Conservative management of mechanical neck disorders: a systematic review. J Rheumatol. 2007;34:1083–102. [PubMed] [Google Scholar]
- 17.Kay TM, Gross A, Goldsmith C, Santaguida PL, Hoving J, Bronfort G. Exercises for mechanical neck disorders. Cochrane Database Syst Rev. 2005:CD004250. doi: 10.1002/14651858.CD004250.pub3. [DOI] [PubMed] [Google Scholar]
- 18.Verhagen AP, Karels C, Bierma-Zeinstra SM, et al. Exercise proves effective in a systematic review of work-related complaints of the arm, neck, or shoulder. J Clin Epidemiol. 2007;60:110–7. doi: 10.1016/j.jclinepi.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 19.Hurwitz EL, Carragee EJ, van der Velde G, et al. Treatment of neck pain: noninvasive interventions: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33:S123–152. doi: 10.1097/BRS.0b013e3181644b1d. [DOI] [PubMed] [Google Scholar]
- 20.Andersen LL, Kjaer M, Sogaard K, Hansen L, Kryger AI, Sjogaard G. Effect of two contrasting types of physical exercise on chronic neck muscle pain. Arthritis Rheum. 2008;59:84–91. doi: 10.1002/art.23256. [DOI] [PubMed] [Google Scholar]
- 21.Ylinen J, Takala EP, Nykanen M, et al. Active neck muscle training in the treatment of chronic neck pain in women: a randomized controlled trial. JAMA. 2003;289:2509–16. doi: 10.1001/jama.289.19.2509. [DOI] [PubMed] [Google Scholar]
- 22.Ylinen J, Kautiainen H, Wiren K, Hakkinen A. Stretching exercises vs manual therapy in treatment of chronic neck pain: a randomized, controlled cross-over trial. J Rehabil Med. 2007;39:126–32. doi: 10.2340/16501977-0015. [DOI] [PubMed] [Google Scholar]
- 23.Bronfort G, Haas M, Evans RL, Bouter LM. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine J. 2004;4:335–6. doi: 10.1016/j.spinee.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 24.Evans R, Bronfort G, Nelson B, Goldsmith CH. Two-year follow-up of a randomized clinical trial of spinal manipulation and two types of exercise for patients with chronic neck pain. Spine. 2002;27:2383–9. doi: 10.1097/00007632-200211010-00013. [DOI] [PubMed] [Google Scholar]
- 25.Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Arch Int Med. 2008 doi: 10.1001/archinternmed.2008.543. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.GENESYS-IDplus. GENESYS Sampling Services; [Accessed January 2, 2008]. Available at: http://www.m-s-g.com/genesys/genesys_products/genidplus.htm. [Google Scholar]
- 27.American Association for Public Opinion Research (APOR) Standard Definitions: Final Dispositions of Case Codes and Outcome Rages for Surveys. 4. Lenexa, Kansan: APOR; 2006. [Google Scholar]
- 28.Carey TS, Evans A, Hadler N, Kalsbeek W, McLaughlin C, Fryer J. Care-seeking among individuals with chronic low back pain. Spine. 1995;20:312–7. doi: 10.1097/00007632-199502000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine. 2000;25:3115–24. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 30.Pietrobon R, Coeytaux RR, Carey TS, Richardson WJ, DeVellis RF. Standard scales for measurement of functional outcome for cervical pain or dysfunction: a systematic review. Spine. 2002;27:515–22. doi: 10.1097/00007632-200203010-00012. [DOI] [PubMed] [Google Scholar]
- 31.Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther. 2007;37:290–302. doi: 10.2519/jospt.2007.2498. [DOI] [PubMed] [Google Scholar]
- 32.Gudavalli MR, Cambron JA, McGregor M, et al. A randomized clinical trial and subgroup analysis to compare flexion-distraction with active exercise for chronic low back pain. Eur Spine J. 2006;15:1070–82. doi: 10.1007/s00586-005-0021-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Petersen T, Larsen K, Jacobsen S. One-year follow-up comparison of the effectiveness of McKenzie treatment and strengthening training for patients with chronic low back pain: outcome and prognostic factors. Spine. 2007;32:2948–56. doi: 10.1097/BRS.0b013e31815cda4a. [DOI] [PubMed] [Google Scholar]
- 34.Talo S, Puukka P, Rytokoski U, Ronnemaa T, Kallio V. Can treatment outcome of chronic low back pain be predicted? Psychological disease consequences clarifying the issue. Clin J Pain. 1994;10:107–21. doi: 10.1097/00002508-199406000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Battie MC, Cherkin DC, Dunn R, Ciol MA, Wheeler KJ. Managing low back pain: attitudes and treatment preferences of physical therapists. Phys Ther. 1994;74:219–26. doi: 10.1093/ptj/74.3.219. [DOI] [PubMed] [Google Scholar]
- 36.Liu H, Hays RD, Adams JL, et al. Imputation of SF-12 health scores for respondents with partially missing data. Health Serv Res. 2005;40:905–21. doi: 10.1111/j.1475-6773.2005.00391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cherkin DC, Deyo RA, Wheeler K, Ciol MA. Physician variation in diagnostic testing for low back pain. Who you see is what you get. Arthritis Rheum. 1994;37:15–22. doi: 10.1002/art.1780370104. [DOI] [PubMed] [Google Scholar]
- 38.Rainville J, Carlson N, Polatin P, Gatchel RJ, Indahl A. Exploration of physicians’ recommendations for activities in chronic low back pain. Spine. 2000;25:2210–20. doi: 10.1097/00007632-200009010-00012. [DOI] [PubMed] [Google Scholar]
- 39.Konrad TR, Fletcher GS, Carey TS. Interprofessional collaboration and job satisfaction of chiropractic physicians. J Manipulative Physiol Ther. 2004;27:245–52. doi: 10.1016/j.jmpt.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 40.Carosella AM, Lackner JM, Feuerstein M. Factors associated with early discharge from a multidisciplinary work rehabilitation program for chronic low back pain. Pain. 1994;57:69–76. doi: 10.1016/0304-3959(94)90109-0. [DOI] [PubMed] [Google Scholar]
- 41.Gross DP, Battie MC. Predicting timely recovery and recurrence following multidisciplinary rehabilitation in patients with compensated low back pain. Spine. 2005;30:235–40. doi: 10.1097/01.brs.0000150485.51681.80. [DOI] [PubMed] [Google Scholar]
- 42.Hildebrandt J, Pfingsten M, Saur P, Jansen J. Prediction of success from a multidisciplinary treatment program for chronic low back pain. Spine. 1997;22:990–1001. doi: 10.1097/00007632-199705010-00011. [DOI] [PubMed] [Google Scholar]
- 43.Merkesdal S, Mau W. Prediction of costs-of-illness in patients with low back pain undergoing orthopedic outpatient rehabilitation. Int J Rehabil Res. 2005;28:119–26. doi: 10.1097/00004356-200506000-00004. [DOI] [PubMed] [Google Scholar]
- 44.Rainville J, Sobel JB, Hartigan C, Wright A. The effect of compensation involvement on the reporting of pain and disability by patients referred for rehabilitation of chronic low back pain. Spine. 1997;22:2016–24. doi: 10.1097/00007632-199709010-00016. [DOI] [PubMed] [Google Scholar]
- 45.Honda K. Factors underlying variation in receipt of physician advice on diet and exercise: applications of the behavioral model of health care utilization. Am J Health Promot. 2004;18:370–7. doi: 10.4278/0890-1171-18.5.370. [DOI] [PubMed] [Google Scholar]
- 46.Kreuter MW, Scharff DP, Brennan LK, Lukwago SN. Physician recommendations for diet and physical activity: which patients get advised to change? Prev Med. 1997;26:825–33. doi: 10.1006/pmed.1997.0216. [DOI] [PubMed] [Google Scholar]
- 47.Damush TM, Stewart AL, Mills KM, King AC, Ritter PL. Prevalence and correlates of physician recommendations to exercise among older adults. J Gerontol A Biol Sci Med Sci. 1999;54:M423–7. doi: 10.1093/gerona/54.8.m423. [DOI] [PubMed] [Google Scholar]
- 48.Carroll JK, Fiscella K, Epstein RM, et al. Getting patients to exercise more: a systematic review of underserved populations. J Fam Pract. 2008;57:170–176. E171–173, 171. following E173. [PMC free article] [PubMed] [Google Scholar]
- 49.Street RL, Jr, Gordon H, Haidet P. Physicians’ communication and perceptions of patients: is it how they look, how they talk, or is it just the doctor? Soc Sci Med. 2007;65:586–98. doi: 10.1016/j.socscimed.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Street RL, Jr, Gordon HS, Ward MM, Krupat E, Kravitz RL. Patient participation in medical consultations: why some patients are more involved than others. Med Care. 2005;43:960–9. doi: 10.1097/01.mlr.0000178172.40344.70. [DOI] [PubMed] [Google Scholar]
- 51.Chou R, Huffman LH. Medications for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147:505–14. doi: 10.7326/0003-4819-147-7-200710020-00008. [DOI] [PubMed] [Google Scholar]