Abstract
Past research on idioms of distress among U.S. Latinos has revealed that ataque de nervios and altered perceptions, such as hearing and seeing things when alone, are independent markers of higher morbidity and mental health utilization despite having no one-to-one relationships with any single psychiatric diagnosis. It has been proposed that the idioms exert this effect because they are signs of distressing dissociative capacity associated with traumatic exposure. This study examines the relationships in an ethnically diverse Latino psychiatric outpatient sample (N = 230) among interpersonal trauma, posttraumatic stress disorder (PTSD), major depressive disorder, dissociative capacity and four cultural idioms of distress associated with the popular overall category of nervios. We particularly explore how these relationships change with varied measures of traumatic exposure, including trauma severity and timing or persistence of trauma. A series of adjusted bivariate regressions assessed the matrix of associations between the idioms and the clinical variables. In this highly traumatized population, we identified a strong ‘nexus’ of associations between dissociation and three of the idioms: currently being ill with nerves, ataque de nervios and altered perceptions. These idioms were largely independent from PTSD and depression and were associated with trauma persistence and severity. A fourth idiom, being nervous since childhood, was not associated with any other variable and may represent a personality trait rather than a diagnosable condition. Our results validate the clinical utility of the construct of nervios as a set of specific idioms associated with dissociation that are useful markers of mental health need among Latinos independently of their association with clinical diagnoses.
Keywords: Idioms of distress, Ataque de nervios, Dissociation, Trauma, Posttraumatic stress disorder, Altered perceptions, Latinos
Introduction
Research on the empirical relationship between popular categories of mental and emotional suffering—idioms of distress (Nichter 1981)—and DSM-defined psychiatric disorders has become increasingly precise in recent years. Three research approaches have dominated the field. The first approach involves amassing large community-based samples with sufficient statistical power to examine the independent effects of a series of indicators—such as language fluency, ethnonational origin or use of religious or spiritual sources of care—on the presence of the idioms and on their association with psychiatric disorders (Guarnaccia et al. 1993, 2005, 2010; Lewis-Fernández et al. 2009; Salgado de Snyder et al. 2000; Takeuchi et al. 2002). The second approach entails classifying clinical samples of mental health or general medicine patients who endorse the idiom on the basis of their psychiatric symptoms and disorders in order to clarify the conceptual overlap between the popular and professional nosologies (Chang et al. 2005; Hinton et al. 2001; Lewis-Fernández et al. 2002; Liebowitz et al. 1994; Salmán et al. 1998). A third approach involves preselecting a discrete set of potential psychological mechanisms—such as dissociative capacity, catastrophic cognitions or anxiety sensitivity—because of their association with a psychiatric disorder that is phenomenologically similar to the idiom being investigated. Researchers then proceed to compare the matrices of associations among the idiom of distress, the psychiatric disorder and the potential mechanisms in order to clarify the extent of the apparent phenomenological similarity between the idiom and the disorder (Hinton et al. 2006; Lewis-Fernández et al. 2002).
Each of these approaches has been used to study various idioms of distress common in Latino communities. The best-studied idiom in this regard is ataque de nervios (attack of nerves), which is particularly prominent among Latinos from the Caribbean, but recognized among many Hispanic groups (Guarnaccia et al. 1993, 1996; Lewis-Fernández 1996). Commonly reported elements of ataques include screaming and shouting uncontrollably, attacks of crying, trembling, heat in the chest rising into the head and becoming verbally and physically aggressive. Dissociative experiences, seizure-like or fainting episodes and suicidal gestures are prominent in some ataques but absent in others. Attacks frequently occur as a direct result of a stressful event relating to the family, such as news of the death of a close relative, conflicts with a spouse or children or witnessing an accident involving a family member. For a minority of individuals, no particular social event triggers their ataques; instead, their vulnerability to losing control comes from the accumulated experience of suffering (APA 2000; Guarnaccia et al. 1996).
Epidemiological studies with representative national samples in Puerto Rico and the United States have found that ataques are fairly common among community-based Latinos: the lifetime prevalence in adults is between 5 and 15%, depending on the Latino group and the measure used (Guarnaccia et al. 1993, 2010). Age and gender are associated with ataque endorsement, as ataques tend to be more prevalent in older adolescent girls in child samples and women over 45 years of age in adult samples (Guarnaccia et al. 1993, 2005). No one-to-one relationship has been found between ataque and any given psychiatric disorder, although certain disorders, such as panic disorder and dissociative disorder not otherwise specified, have a special overlap with ataque phenomenology (Guarnaccia et al. 1993; Lewis-Fernández et al. 2002). Ataques are associated instead with diverse anxiety, depressive, dissociative and somatoform disorders (Guarnaccia et al. 1993, 2005, 2010). In community samples, lifetime endorsement of ataque is associated with greater suicidal ideation, disability due to mental health problems, and outpatient psychiatric utilization, even after adjusting for the contribution of psychiatric diagnoses, traumatic exposure and other clinical and demographic covariates (Lewis-Fernández et al. 2009). This greater morbidity associated with ataque may be due to its relationship to dissociativity, which is elevated in psychiatric outpatients reporting greater ataque frequency and severity (Hinton et al. 2008a; Lewis-Fernández et al. 2002). Dissociation is a psychological process characterized by a disruption in the usually integrated functions of consciousness, memory, identity or perception that is usually precipitated by a traumatic exposure (APA 2000). Its presence has been associated with higher clinical morbidity in the case of various psychiatric disorders (Johnson et al. 2006); for example, when a person has a dissociative reaction immediately or soon after a traumatic event and subsequently develops posttraumatic stress disorder (PTSD), the severity of PTSD tends to be greater than in those without this “peritraumatic” dissociation (Ozer et al. 2003).
It has been suggested that ataque may be associated with traumatic exposure and PTSD (Lewis-Fernández 1994; Lewis-Fernández et al. 2002; Schechter et al. 2000) based on its relationship with acutely stressful events and dissociative processes, in addition to its resemblance to pseudoseizures [convulsions that are associated with childhood trauma and dissociativity (Brown et al. 2007; Martínez-Taboas et al. 2001)]. However, this relationship has rarely been tested. When it has, the results have not been completely consistent. In Puerto Rico, ataque was associated with PTSD in a community sample of adults (OR = 5.3) and a clinical sample of children (OR = 8.65) but not among community-based children (Guarnaccia et al. 1993, 2005). These odds ratios are not dissimilar in magnitude to those quantifying the relationship of ataque with other anxiety and depressive disorders, suggesting a general rather than a specific association with PTSD.
Research on the association of trauma, PTSD, and ataque in clinical settings has also found mixed results. Schechter and colleagues (2000) examined the relationship of ataque with childhood trauma in an opportunistic sample of 70 adult Latino psychiatric outpatients (mostly Dominican and Puerto Rican). Over half (57%) endorsed a history of childhood trauma on the Brief Physical and Sexual Abuse Questionnaire (BPSAQ), and 74% reported ataques on a semistructured interview. The rate of childhood trauma was significantly higher in the group with ataques (63%) than in the group without ataques (39%). The authors hypothesized that ataque may represent a cultural expression of extreme affect dysregulation associated with childhood trauma. The association between ataque and PTSD was not assessed.
Lewis-Fernández et al. (2002) tested the association of ataque with childhood trauma and PTSD in a sample of 29 adult first-generation Puerto Rican women seeking psychiatric care. Ataque and childhood trauma were assessed via in-depth semistructured interviews, which were coded on the basis of audiotapes (Lewis-Fernández et al. 2002). Contrary to the findings of Schechter and colleagues, most participants endorsed a history of childhood trauma, and the mean number of traumatic exposures did not differ across three categories of lifetime ataque status: none, a few (one to five ataques) and frequent (more than five ataques). The association between ataque status and PTSD was also nonsignificant, although the prevalence of PTSD in participants with frequent ataques was elevated (63%) compared to the other two groups (25–33%). By contrast, the relationship between ataque status and dissociativity was highly significant in this traumatized sample, whether assessed via the self-report Dissociative Experiences Scale or the clinician-administered Structured Clinical Interview for DSM-III-R. The authors concluded that frequent ataques may indicate the presence of psychiatric disorders characterized by dissociative symptoms. The relationship with childhood trauma remained unclear, however. Given the frequency of traumatic exposure in this clinical sample, it is possible that childhood trauma is a necessary precondition of frequent ataques. Yet childhood traumatic exposure is clearly not sufficient by itself to cause frequent ataques or diagnosable dissociative reactions. Instead, additional factors appear necessary, and the interrelationship between ataque and dissociation raises the question whether these behaviors share common precipitating factors (Lewis-Fernández et al. 2002). The relationship between ataque and dissociativity has been confirmed in a different sample of 70 psychiatric outpatients from diverse Latino subgroups (Hinton et al. 2008a).
Other idioms of distress common among Caribbean Latinos have received much less research attention. Two syndromes related to the general category of nervios (nerves) have been initially described. The first is “ser nerviosa(o)” (being nervous), a chronic condition usually starting in childhood, when it is called “ser nerviosa(o) desde chiquita(o)” or “desde niña(o)” (being nervous since childhood). This is characterized by substantial vulnerability to life’s problems, the inability to solve them and chronic worry as a result, associated with various anxiety and somatic symptoms (e.g., trembling, irritability, headaches, gastrointestinal distress) (Guarnaccia et al. 2003). This idiom is understood based on a stress-diathesis model, arising because of adversity (e.g., chronic stress or traumatic exposure starting in childhood), inherited causes (e.g., a genetic predisposition or a gestational insult such as maternal alcohol abuse in utero) or a combination of the two. The relationship to trauma, PTSD, and other psychiatric disorders, such as depression, has not been examined.
The second idiom that has been described among Caribbean Latinos is a version of the pan-Latin American construct of nervios, labeled “padecer de los nervios” (suffering from nerves) in its general form and “estar enfermo de los nervios” (being ill with nerves) in its more severe form (Guarnaccia et al. 2003). Acknowledged precipitants for this condition are similar to those for “being nervous since childhood,” except that “the stressful events occur more in adulthood, are more severe, and particularly come together in an overwhelming way” (Guarnaccia et al. 2003, p. 351). The idiom is characterized by symptoms of anxiety, depression and somatization, such as having “too many thoughts,” irritability, sadness, fearfulness, and a predisposition to explosive anger; in severe cases, psychosis may also be present (Guarnaccia et al. 2003). The relationship of “being ill with nerves” to traumatic exposure and to psychiatric diagnoses is unexamined in the Hispanic Caribbean. In Mexico and Costa Rica, nervios idioms have been associated predominantly with depressive and anxiety disorders (Low 1981; Salgado de Snyder et al. 2000) but have not been studied particularly with respect to PTSD and traumatic exposure.
A final idiom of distress whose relationship to psychiatric diagnoses and potential precipitants such as traumatic exposure has been initially investigated is a set of perceptual experiences commonly reported by Latinos of various national backgrounds. These experiences are not identified by a single cultural label but, rather constitute a loose set of visual, auditory and tactile perceptions that are frequently triggered by stress, such as “seeing celajes” (shadows), “hearing someone call you” and “feeling a presencia” (presence) (Guarnaccia et al. 1992; Lewis-Fernández et al. 2005). We refer to this idiom under the rubric of “altered perceptions” throughout this article. Among primary care outpatients in Puerto Rico referred to mental health care, altered auditory and visual perceptions of this type are very common, endorsed by 70–77% of a consecutive sample of 81 outpatients (Lewis-Fernández et al. 2005). Unlike ataque and the other nervios-related idioms, research on this idiom has usually not been conducted under a cultural label but, rather, with symptom scales intended to detect psychosis (Lewis-Fernández et al. 2009), particularly the items tapping visual and auditory hallucinations (e.g., “Did you ever see a vision that other people could not see?”). Over 90% of Latinos endorsing these perceptual symptoms do not meet the criteria for psychotic disorder on structured diagnostic instruments, however, suggesting that these altered perceptions constitute a nonspecific idiom of distress. Empirical comparison confirms this, revealing that they are associated with diverse anxiety, depressive and substance use disorders (Lewis-Fernández et al. 2009; Olfson et al. 2002). Nevertheless, as in the case of ataque, endorsing lifetime pseudopsychotic experiences is associated independently with higher clinical morbidity in primary care and community-based samples of U.S. Latinos—including greater suicidal ideation, mental-health-related disability and outpatient mental health service utilization—after adjusting for associated psychiatric disorders and other covariates (Lewis-Fernández et al. 2009; Olfson et al. 2002). This suggests that some aspect of the idiom is responsible for additional morbidity in clinical samples. The fact that ataque and the altered perceptions are correlated in primary care and community samples suggests that dissociation might constitute this aspect associated with higher morbidity (Lewis-Fernández et al. 2005, 2009).
As with the other idioms discussed above, the relationship of the altered perceptions with trauma and PTSD remains unclear. Lifetime traumatic exposure in U.S. Latinos is associated with pseudo-psychotic symptoms in bivariate but not multivariate analyses, while the relationship with anxiety disorders (including PTSD) remains significant in both types of analyses (Lewis-Fernández et al. 2009), suggesting the higher specificity of the latter association. A stronger relationship of psychotic symptoms with PTSD and depression in Latinos relative to non-Latino whites has been reported in U.S. regional studies (David et al. 1999; Mueser and Butler 1987; Posternak and Zimmerman 2005). This might be due to the misattribution of the altered perceptions to psychotic processes when they present in the context of PTSD and depression. However, the association of altered perceptions with PTSD, depression and dissociation, including in the context of traumatic exposure, has not been tested directly.
This study was designed, in part, to address these limitations in the research base on these idioms of distress. The primary aim of this article is to clarify the relationships among four cultural idioms of distress (being nervous since childhood, currently being ill with nerves, ataques de nervios and altered perceptions), trauma-related psychiatric diagnoses (PTSD and major depressive disorder [MDD]) and psychological processes (dissociation) in a Latino psychiatric outpatient sample. We explore how these relationships change with varied measures of traumatic exposure, including trauma severity and timing or persistence of trauma. We hypothesize that people who experience more persistent interpersonal trauma (i.e., both during childhood and adulthood) will exhibit stronger associations between the idioms of distress and dissociation, PTSD and MDD, than those who experience trauma only during childhood. To our knowledge, no studies to date have simultaneously explored the relationships among traumatic exposure, PTSD, MDD, dissociation and these four idioms of distress. In fact, this may be the first study to empirically examine multiple idioms of distress at once with respect to trauma exposure or to a psychiatric disorder.
Methods
This study was conducted at the Hispanic Treatment Program of the New York State Psychiatric Institute (NYSPI) Anxiety Disorders Clinic, a research program in northern Manhattan focusing on anxiety and depressive disorders. Participants (n = 230) were adult Spanish-dominant Latinos from varied ethnonational backgrounds who were scheduled for a Structured Clinical Interview for DSM-IV (SCID; First et al. 1996) as part of their intake evaluation for possible participation in research protocols. As detailed under Results, most participants had low household incomes and nearly all were Latin American immigrants. Conditions that met the criteria for an Axis I diagnosis over the past 12 months were recorded. Patients with current substance use disorder, dementia or a history of psychosis were excluded. A diagnosis of psychosis was made on the SCID based on meeting full criteria on the SCID B/C modules for psychotic disorder, rather than on endorsement of isolated psychotic symptoms; this assessment was made blind to the results of the idioms questionnaires and the Dissociative Experiences Scale. Participants who endorsed a traumatic event were administered the PTSD module, focusing on the event that “most affected” the participant. Prior to the SCID, all patients completed a demographic questionnaire. Language dominance was determined by participants’ preference to carry out the evaluation in Spanish.
All participants were evaluated with several diagnostic tools and questionnaires: a demographic questionnaire, the Brief Physical and Sexual Abuse Questionnaire (BPSAQ), the Dissociative Experiences Scale (DES), a nervios questionnaire and a questionnaire regarding altered perceptions. Results from all instruments were originally available in English except for the three altered perception items, which were composed in Spanish. Translation for all measures followed standard translation methodology of forward-translation, back-translation, and bilingual committee consensus. The study was approved by the NYSPI Institutional Review Board and written informed consent was obtained from all participants.
Those who agreed to participate in the study were given a packet containing three self-report instruments: the DES, the nervios questionnaire and the altered perceptions questionnaire. The DES is a 28-item scale assessing current dissociative capacity, including normal and pathological dissociative experiences. It is coded on an 11-point Likert format (0–100%) indicating the percentage of time that the person has the experience, where 0% = “never” and 100% = “always.” It has shown adequate psychometric properties in diverse cultural samples, including among Puerto Rican psychiatric outpatients (Lewis-Fernández et al. 2007; Martínez-Taboas 1995); Cronbach’s αfor the DES in our sample (N = 230) is 0.91. DES scores are presented as means of the full scale and generally range from ≤10 in normal samples to > 30 in persons with dissociative pathology; scores between 10 and 15 are typical of depressive and anxiety disorders, except for persons with PTSD, who usually score around 30 (Putnam et al. 1996). There is some evidence of cross-cultural validity for these scores, including in Puerto Rico, Turkey and the Netherlands (Lewis-Fernández et al. 2007).
Participants also completed a five-item questionnaire tapping various idioms related to nervios, including “being nervous since childhood,” “currently being ill with nerves” and “ever having ataques de nervios.” Those who endorsed the ataque item were asked to quantify their lifetime number of ataques. This questionnaire has been published previously as part of a discussion of a popular nosology of nervios and ataques de nervios (Guarnaccia et al. 2003).
Patients also completed three items on the current frequency of altered perceptions as part of a scale under development tapping diverse experiences in the Hispanic Caribbean associated with spiritual practices and unusual perceptions. The wording for the three items is presented in Table 1. Following the DES format, scores for each item range from 0 to 100%, and a mean score is presented for the three items combined (Cronbach’s αin our sample = 0.91). Patients were also dichotomized into those who did and those who did not answer positively (≥10%) on any of the three altered perceptions.
Table 1.
Wording of the three altered perception items
| Hay personas que a veces tienen la experiencia de oír que las llaman por su nombre pero cuando miran no ven a nadie. Haga un círculo alrededor del número que indique la frecuencia con que esto le pasa a usted | ||||||||||
| Some people at times have the experience of hearing their name being called but when they look they do not see anyone. Circle a number to show what percentage of time this happens to you | ||||||||||
| 0% never |
10 | 20 | 30 | 40 | 50 | 60 | 70 | 80 | 90 | 100% always |
| Hay personas que a veces tienen la experiencia de ver de momento y por el rabo del ojo a una figura que pasa por su lado y que luego desaparece (“ven un celaje”). Haga un círculo alrededor del número que indique la frecuencia con que esto le pasa a usted | ||||||||||
| Some people at times have the experience of catching a glimpse, from the corner of their eye, of a shape that passes by their side and then disappears. Circle a number to show what percentage of time this happens to you | ||||||||||
| 0% never |
10 | 20 | 30 | 40 | 50 | 60 | 70 | 80 | 90 | 100% always |
| Hay personas que encuentran que a veces sienten la presencia de algo o alguien a su alrededor y cuando miran no ven a nadie. Haga un círculo alrededor del número que indique la frecuencia con que esto le pasa a usted | ||||||||||
| Some people find that sometimes they feel the presence of something or someone around them, and when they look they do not see anyone. Circle a number to show what percentage of time this happens to you | ||||||||||
| 0% never |
10 | 20 | 30 | 40 | 50 | 60 | 70 | 80 | 90 | 100% always |
In addition, the clinician who conducted the SCID also administered the BPSAQ, a questionnaire measuring the patient’s history of interpersonal trauma, with a focus on physical and sexual abuse during childhood. Using this measure, interpersonal trauma during childhood was defined as having experienced any of the following before age 16: traumatic separation from the primary caregiver for more than 1 month, the presence of a substance-abusing person in the household, the use of harsh discipline involving hitting with an object, physical injury to the patient or sibling resulting from punishment, witnessing physical violence between the caregivers, forced sexual contact with an older child or adult or forced sexual contact with a relative (Marshall et al. 1998). Interpersonal trauma during adulthood was defined as experiencing physical assault or sexual assault or rape at or after age 16. The presence or absence of trauma at any age was dichotomized on the basis of a positive answer to any item; in addition, the total number of traumatic event types was coded over the range of 1–9. Clinicians conducting the BPSAQ were blind to the results of the self-report scales but were aware of the SCID findings.
Statistical Analysis
Bivariate logistic and linear regression models were used to investigate the associations between the four idioms of distress and three trauma-related clinical categories: PTSD, MDD and dissociative capacity. To determine the influence of trauma in these relationships, we ran the bivariate models in several trauma subsamples and grouped the resulting models into graphic representations. In these analyses, the outcome variable was chosen using the following conventions: (1) in tests between a clinical variable and an idiom (clinical vs. idiom), the idiom was always designated the outcome variable; (2) in clinical versus clinical and idiom versus idiom analyses, the directionality is always toward the bottom of the page (i.e., for MDD vs. PTSD, PTSD is the outcome variable) and (3) in trauma versus clinical and trauma versus idiom analyses (Figs. 2 and 3), the clinical variable or idiom is always the outcome. We demonstrate these effects using figures depicting unidirectional arrows.
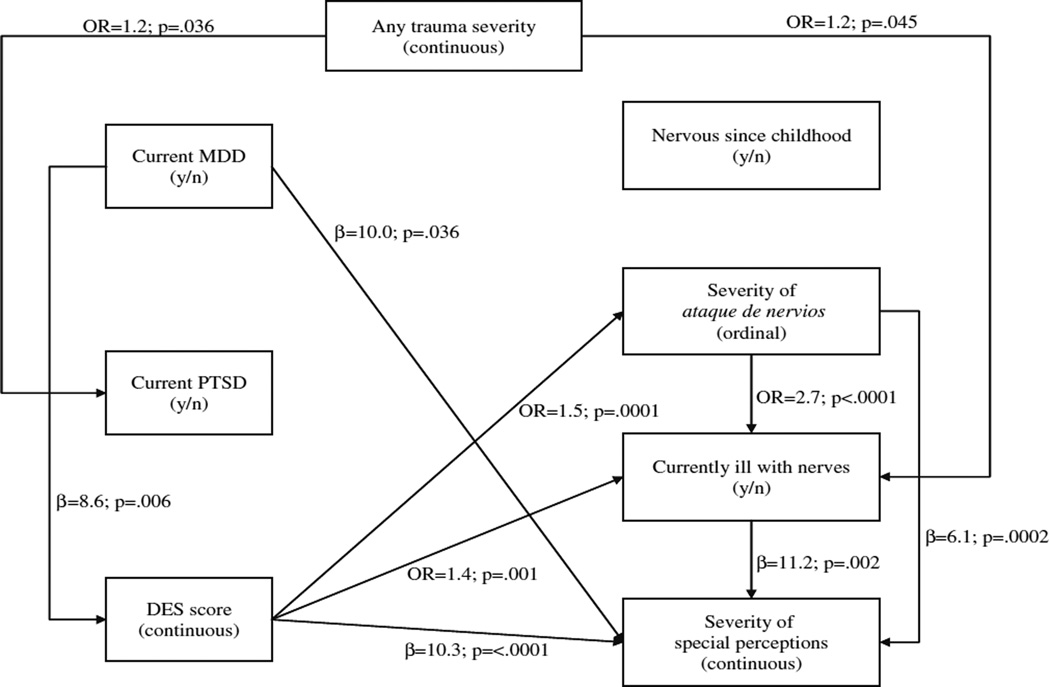
Fig. 2.
Any-trauma severity model 1: associations among severity of trauma, idioms of distress, current major depressive disorder (MDD) and posttraumatic stress disorder (PTSD) and dissociation score in people with any lifetime trauma, adjusted for age and gender (n = 202). DES Dissociative Experiences Scale, OR odds ratio
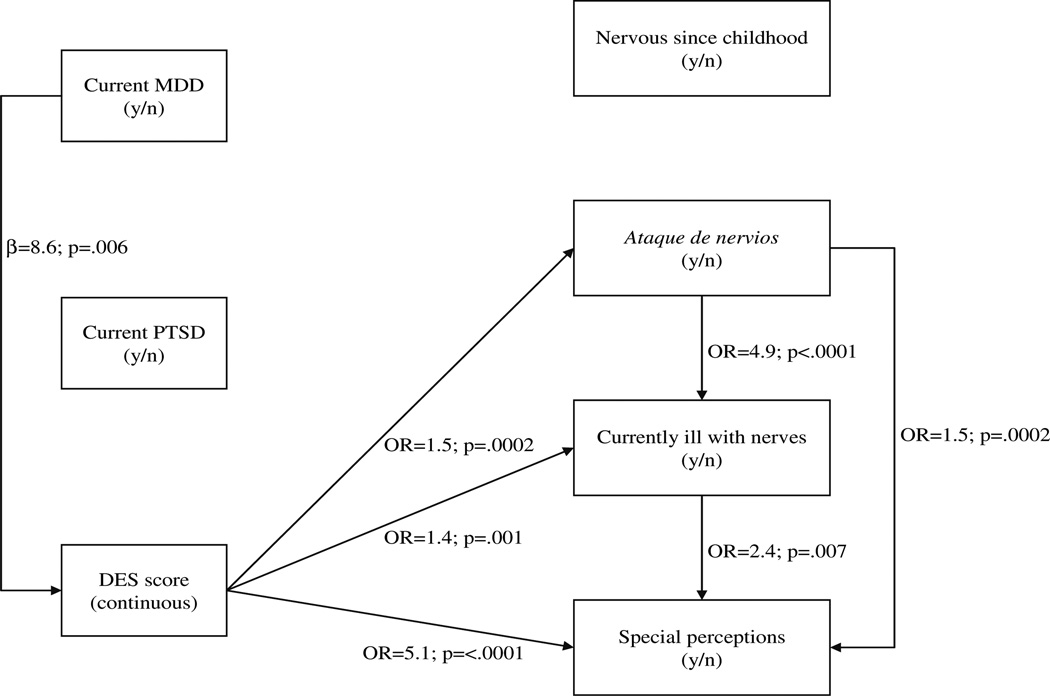
Fig. 3.
Any-trauma severity model 2: associations among severity of trauma, number of idioms of distress, current major depressive disorder (MDD) and posttraumatic stress disorder (PTSD) and dissociation score in people with any lifetime trauma, adjusted for age and gender (n = 202). DES Dissociative Experiences Scale, OR odds ratio
This analysis does not constitute a path analysis, as we do not hypothesize on causality or mediation among multiple variables. Rather, we are interested in exploring how the associations between individual markers of psychiatric vulnerability change with different measures of trauma; thus all analyses are bivariate, adjusting for age and gender.
We explored three aspects of traumatic experience: (1) any interpersonal trauma (dichotomous), (2) persistence of interpersonal trauma (dichotomous; childhood only vs. childhood and adult) and (3) severity of trauma. Participants who never experienced trauma were excluded from all analyses (n = 28) since the prevalence of trauma was very high (88%) in our sample. All regression models were adjusted for age and gender in light of the known association between these variables and ataque endorsement (Guarnaccia et al. 1993, 2005).
In the first set of models, we investigated the relationships between the three clinical categories and the four idioms of distress among participants with a history of any interpersonal trauma (n = 202). We ran a total of 21 regression models across all possible associations between the seven variables. Next, we explored trauma persistence by stratifying the sample into two time-dependent groups (childhood-only trauma, n = 103; and childhood and adult trauma, n = 91), and running the same 21 regression models as above. Eight individuals who experienced interpersonal trauma only during adulthood were excluded from this set of analyses.
In the third set of analyses, we investigated the associations among trauma severity, clinical variables and idioms of distress in our traumatized sample (n = 202) using a total of 28 regression models. Trauma severity was defined as the number of distinct types of traumatic events experienced over a lifetime. It was calculated as the sum of the items on the BPSAQ and had a range of 1–9. In this set of analyses, we also looked at the severity of lifetime ataque experience and of current altered perceptions. Severity of ataque was defined as the total number of ataques reported by study participants during their lifetime. We divided this continuous measure based on the median of the sample (2 ataques), excluding “0” (n = 129) and “too many to count” (n = 41), and determined three distinct ataque categories: none (0), a few (1–2) and frequent (> 2). Severity of current altered perceptions was defined as the mean value of the Likert scales of the three perceptual items combined (0–100%). In the last set of models, we tested the associations among trauma severity, the clinical categories and the number of idioms of distress (10 regression models in total).
Item nonresponse was addressed using multiple-imputation data manipulation (Allison 2001; Little and Rubin 2002; Schafer 1997). Missing data were replaced by random draws from a distribution of plausible values using SAS Proc MI to create five imputed data sets. We then analyzed each imputed data set with logistic and linear regression models and the resulting findings were summarized using SAS Proc MIANALYZE to combine the variation across the five imputed data sets. All statistical analyses were performed with SAS version 9.1 and SPSS version 16. All sample sizes reported are based on the first imputation of the data.
Results
We present several tables with demographic and clinical data and figures which depict the relationships of interest. Figures 1, 2, and 3 depict a graphic representation of the results from age- and gender-adjusted bivariate logistic and linear regressions (odds ratios and βs, respectively), with the directionality of the arrows signifying the direction of association.
Fig. 1.
Any-trauma model: associations among current major depressive disorder (MDD) and posttraumatic stress disorder (PTSD), dissociation score and dichotomous idioms of distress in people with any lifetime trauma, adjusted for age and gender (n = 202). DES Dissociative Experiences Scale, OR odds ratio
Sample Characteristics
The demographic and cultural characteristics of the sample are presented in Table 2. There is a slight preponderance of women, the majority is currently unmarried, the median age of the sample is 40 and there is a broad range of ethnonational backgrounds. As expected in this overwhelmingly first-generation sample affected by the challenges of immigration, their household income is very low, with 83% of households earning less than $20,000, despite the fact that 38% of respondents have at least some college education.
Table 2.
Sample demographics (n = 230)
| Patient characteristic | n | % | Mean | SD |
|---|---|---|---|---|
| Demographics | ||||
| Gender | ||||
| Male | 103 | 45 | ||
| Female | 127 | 55 | ||
| Age | 40 | 10.9 | ||
| Marital status | ||||
| Single | 63 | 27 | ||
| Married | 91 | 40 | ||
| Divorced/widowed | 76 | 33 | ||
| Education | ||||
| Less than high school | 78 | 34 | ||
| Graduated high school | 65 | 28 | ||
| Some college | 51 | 22 | ||
| Graduated college | 26 | 12 | ||
| More than college | 10 | 4 | ||
| Household income ($) | ||||
| Public assistance | 28 | 12 | ||
| <10,000 | 78 | 34 | ||
| 10,000–19,999 | 84 | 37 | ||
| ≥20,000 | 40 | 17 | ||
| Birth nation | ||||
| USA/Canada | 3 | 1 | ||
| Latin America/Caribbean | 219 | 95 | ||
| Europe/Asia | 8 | 4 | ||
| Country of residence up to age 16 | ||||
| Dominican Republic | 82 | 36 | ||
| Other Caribbean | 18 | 8 | ||
| Mexico and Central America | 44 | 19 | ||
| South America | 81 | 35 | ||
| Othera | 5 | 2 |
United States (n = 3) and Spain (n = 2)
Table 3 presents the clinical characteristics of the full sample along with detail on traumatic exposure. All four idioms of distress are frequently reported. Perceptual experiences are the most frequent (68%), followed by currently being ill with nerves (62%), being nervous since childhood (53%) and ataque de nervios (44%). The mean number of idioms endorsed by participants is 2.3. Patients have an average of two current mental health diagnoses; 80% meet the criteria for MDD and 25% have PTSD. Other anxiety disorders are also frequent, in keeping with the study site, which focuses on anxiety and depressive disorders, particularly social phobia, in which the clinic has an active research interest. However, since our focus is on trauma-related disorders, we did not include social phobia in our analyses. The mean dissociation score is 17.9 (range: 0–91), consistent with the mix of psychiatric diagnoses that characterizes the sample.
Table 3.
Clinical characteristics and interpersonal trauma (n = 230)
| Clinical or trauma variable | n | % | Meana | SDa |
|---|---|---|---|---|
| Idioms of distress | ||||
| Nervous since childhood | 123 | 53 | ||
| Ataque de nervios | 101 | 44 | ||
| Currently ill w/nerves | 142 | 62 | ||
| Altered perceptions | 157 | 68 | 19.5 | 25.2 |
| Number of idioms | 2.3 | 1.2 | ||
| Clinical profile | ||||
| Major depressive disorder (MDD) | 185 | 80 | ||
| Posttraumatic stress disorder (PTSD) | 57 | 25 | ||
| Social phobia | 98 | 43 | ||
| Generalized anxiety disorder (GAD) | 34 | 15 | ||
| Panic disorder | 19 | 8 | ||
| Number of psychiatric diagnoses | 2.0 | 1.1 | ||
| Dissociative Experiences Scale (DES) score | 17.9 | 16.5 | ||
| Interpersonal trauma | ||||
| None | 28 | 12 | ||
| Any trauma | 202 | 88 | 3.1 | 1.8 |
| Childhood only | 103 | 45 | 2.2 | 1.3 |
| Childhood and adult | 91 | 40 | 4.4 | 1.5 |
| Adult only | 8 | 3 | 1.0 | 0 |
| Type of traumatic event—childhood | ||||
| Traumatic separation from primary caregiver for ≥1mo | 45 | 20 | ||
| Substance-abusing person in the household | 76 | 33 | ||
| Harsh discipline of children in household involving hitting with an object | 114 | 50 | ||
| Physical injury to the patient or sibling resulting from punishment | 91 | 40 | ||
| Witness to physical violence between caregivers | 85 | 37 | ||
| Forced sexual contact with a nonrelative older child or adult | 27 | 12 | ||
| Forced sexual contact with a relative | 0 | 0 | ||
| Type of traumatic event—adult | ||||
| Physical assault after age 16 | 92 | 40 | ||
| Sexual assault after age 16 | 23 | 10 |
Mean and SD for “interpersonal trauma” refer to number of traumatic events
In terms of traumatic exposure, 88% of participants report at least one lifetime traumatic event. Most trauma experiences took place during childhood, with 45% of the sample reporting trauma only in childhood and 40% reporting trauma both in childhood and adulthood. Only eight participants (3%) experienced traumatic events exclusively during adulthood. In terms of specific traumatic events, a striking number of patients reported some form of physical punishment or injury during either childhood or adulthood. During childhood, half of the sample experienced harsh physical punishment, and over one-third witnessed physical violence between caregivers or lived in a household where the patient or a sibling was injured due to physical punishment. In addition, 40% of the sample reported physical assault after age 16. The reported frequency of sexual abuse was lower than that of physical abuse during both childhood and adulthood.
Any-Trauma Model
We first present a model of associations between the idioms of distress and the clinical categories (MDD, PTSD and dissociation) among the 202 participants who experienced interpersonal trauma at any point in their life, adjusting for age and gender (Fig. 1). The presence of MDD is positively associated with dissociation, with higher mean DES scores among individuals with current MDD (p < 0.01). Contrary to our expectation, the only clinical category associated with any of the idioms of distress is dissociation, which is associated with ataque de nervios, currently feeling ill with nerves and altered perceptions (p ≤ 0.001). Being nervous since childhood is not associated with dissociation and is distinct from the other idioms, which are all associated with one another (p < 0.01). The model is remarkable for the absence of relationship between PTSD and any of the idioms of distress, dissociation or MDD.
Persistence of Trauma
Next we fit two models of association between the idioms and the clinical categories, adjusting for age, gender and the persistence of trauma. First, we examined individuals who experienced trauma only in childhood (less persistent trauma; n = 103). In this subsample, the model remains essentially the same as in the any-trauma group, with the following exceptions. Current MDD and dissociation are no longer associated, while dissociation remains associated with ataque (OR = 1.5, p = 016), currently feeling ill with nerves (OR = 1.5, p = 020) and altered perceptions (β = 5.6, p = 0001). Among the idioms of distress, only ataque and currently feeling ill with nerves remain associated in this sample (OR = 5.8, p = 0006).
Next, we examined the associations between idioms and clinical categories among participants who experienced trauma both during childhood and adulthood (more persistent trauma; n = 91). The model is identical to that for the any-trauma sample, other than some minor changes in the values of the coefficients and odds ratios (data available upon request).
Severity of Trauma
Figure 2 presents the associations between severity of trauma, MDD, PTSD and dissociation and the idioms of distress (n = 202), adjusting for age and gender. In this model, we used the number of ataques de nervios and the mean score on the perceptions items to approximate the severity of these idioms. Severity of trauma is positively associated with the presence of PTSD (p < 0.05) and with currently being ill with nerves (p < 0.05). As in the dichotomous model, dissociation is associated with the presence of MDD (p < 0.01) and with the number of reported lifetime ataques, the severity of the altered perceptions and currently being ill with nerves (p ≤ 0.001). MDD is also associated with the severity of the altered perceptions (p < 0.05). Among the idioms of distress, the severity measures for ataque and for the altered perceptions and the report of currently being ill with nerves are all strongly associated (p < 0.01). Being nervous since childhood again shows no significant associations with the other idioms or clinical categories.
Number of Idioms of Distress
Figure 3 presents the relationship structure among severity of trauma, number of idioms of distress, presence of PTSD and MDD and severity of dissociation. Grouping the idioms of distress as a continuous measure, we see a clear picture of associations emerge. Severity of trauma is positively associated with the number of idioms endorsed (p < 0.01) and with the presence of PTSD (p < 0.05). In turn, the number of idioms of distress is strongly associated with dissociation (p = 0.0001), which is associated with a diagnosis of MDD (p < 0.01). However, PTSD has no relationship with dissociation or with the idioms of distress. Table 4 presents the relationship of the mean trauma and dissociation scores and the number of idioms of distress. Each of these two clinical measures increases in an essentially monotonic fashion as the number of idioms increases, indicating a positive correlation. Assessed numerically (Pearson’s r), the correlation between BPSAQ scores and the number of idioms is r = 0.20 (p = 0.005) and that between DES score and the number of idioms is r = 0.42 (p < 0.0001).
Table 4.
Trauma score and DES score by number of idioms of distress in people with any lifetime trauma (n = 202)
| No. of idioms |
n | Mean (SD) | |
|---|---|---|---|
| BPSAQa | DESb | ||
| 0 | 17 | 2.76 (1.71) | 7.08 (7.72) |
| 1 | 30 | 2.57 (1.55) | 11.44 (12.97) |
| 2 | 62 | 2.98 (1.81) | 15.51 (11.77) |
| 3 | 56 | 3.39 (1.70) | 23.82 (18.57) |
| 4 | 37 | 3.68 (1.90) | 28.83 (18.21) |
Brief Physical and Sexual Abuse Questionnaire
Dissociative Experiences Scale
Discussion
This study is the first to examine simultaneously the relationship among diverse Latino idioms of distress, interpersonal traumatic exposure, PTSD, major depression and dissociativity. The data confirm several of our expectations but contradict others. Taken together, our results help clarify the interrelationship among these idioms, precipitants and clinical categories and provide useful guidance to clinicians evaluating Spanish-speaking Latino adults presenting with these idioms of distress. The data can be summarized into four main findings.
First, ataque de nervios, currently being ill with nerves and altered perceptions (auditory, visual and tactile experiences) are highly correlated in Spanish-speaking Latino psychiatric outpatients reporting interpersonal trauma. This is consistent with previous ethnographic research in Puerto Rico revealing that people who “suffer from nerves” are more likely to experience an ataque (Guarnaccia et al. 2003). Additionally, the association between endorsement of altered perceptions and ataque supports previous evidence of a correlation between ataque and this idiom, whether measured directly among Puerto Rican psychiatric outpatients (Lewis-Fernández et al. 2005) or by proxy scales intended to capture psychotic symptoms among a representative community sample of U.S. Latinos (Lewis-Fernández et al. 2009). To our knowledge, this is the first quantitative support for the correlation among three idioms of distress in a Latino sample. Their correlation confirms ethnographic findings linking these three concepts under the general rubric of “nervios” (nerves)-related conditions (Guarnaccia et al. 2003; Lewis-Fernández et al. 2005) and suggests that future studies pay more attention to this comprehensive label, of which the particular idioms studied so far may represent specific but interrelated components.
Curiously, being nervous since childhood was found to be an independent idiom of distress not correlated with the other three idioms, at least in this clinical sample exposed to interpersonal trauma. This finding contradicts previous ethnographic evidence with a community sample in Puerto Rico linking this idiom with other nervios-related constructs (Guarnaccia et al. 2003). It is possible that the differences between the samples (clinical vs. community, Puerto Rican vs. a mixed group of Latinos) are responsible for this discrepancy. Or “being nervous since childhood” may constitute a subcategory of a more general idiom of “being nervous,” which has a closer relationship than the “childhood” idiom to other nervios conditions. Alternatively, being nervous since childhood may be more a label of self-identity or a personality trait than an overt syndrome, or may be a milder condition than the other idioms. This possibility is supported by the lack of relationship between being nervous since childhood and any of the three clinical conditions (MDD, PTSD and elevated dissociativity) investigated in this study.
Second, the three interrelated idioms are highly correlated with dissociation in all trauma models. Whether these idioms are precursors of or concurrent with dissociative experience is unclear, due to our cross-sectional design. Our results confirm the findings of prior studies which also show a comorbid relationship between ataque and dissociative symptoms and disorders in U.S. Latinos from diverse national backgrounds (Hinton et al. 2008a; Lewis-Fernández et al. 2002). This study extends that observed association to two other idioms, currently being ill with nerves and the altered perceptions. One potential explanation for the relationship between dissociativity and these idioms of distress is that dissociative idioms are prevalent among Latinos due to cultural interpretations about the dangerousness of strong negative emotions, which are feared to lead to loss of control, insanity and violence (Hinton et al. 2009; Lewis-Fernández 1998). When emotions of sadness, grief, rage and fear are evoked by adversity—especially of traumatic proportions—Latinos may express dissociative idioms as a way of distancing themselves from the negative consequences of the disturbing affect through the mechanisms of depersonalization, emotional numbing or amnesia. These dissociative mechanisms may allow the person to mute the experienced emotional charge and at least partially disavow responsibility for the acute expression of emotionality (Chu and Dill 1990; Hinton et al. 2009; Lewis-Fernández 1998). The depersonalized expression, “That was not me,” when describing the person’s role in carrying out the violent ataque behavior, and the ego-dystonic and despairing quality of some severe auditory perceptions (“Kill yourself!”) represent potential examples of dissociated affect and cognition that could be related to traumatic antecedents. Alternatively, given the cross-sectional nature of our analysis, it is possible that dissociativity constitutes a primary diathesis unrelated to a fear of negative emotionality and that it is this predisposition that leads to the emergence of the idioms in vulnerable individuals.
The finding that participants who endorse a greater number of idioms of distress are more likely to dissociate is particularly striking (Table 4). DES scores rise from around 7 for participants who report no idioms of distress to about 29 for those who endorse all four idioms, a moderate correlation of r = 0.42. This represents a progression from normal to frankly pathological indexes of dissociativity, typically associated with PTSD and certain dissociative disorders (Putnam et al. 1996). Our discovery of a ‘nucleus’ of association, composed of three cultural idioms of distress and dissociation, is robust and persists across various categories of trauma exposure. The clinical implications of this phenomenological nucleus should be assessed in larger study samples.
Third, our study provides partial support for the association between the presence of the idioms and trauma persistence and severity. (We are unable to examine the association of presence vs. absence of trauma exposure and the models assessed here due to the very high rate of trauma in our sample, which limits our variability to examine these associations.) In terms of persistence, the associations among the three idioms of distress are present in all the models examined, except for the group reporting trauma only during childhood, in which only ataque and currently being ill with nerves are associated. This raises the question whether the association between the other idioms is specifically dependent on the presence of persistent trauma (in both childhood and adulthood). When we examine the association with the idioms with respect to trauma severity, the number of idioms reported is indeed associated with trauma severity (Fig. 3 and Table 4), but the magnitude of the correlation is small (r = 0.20). Only the idiom currently being ill with nerves seems to be associated with trauma severity (OR = 1.2). Moreover, unlike the DES score, which rises dramatically with the number of idioms, BPSAQ score rises only slightly, by 0.92 mean trauma experience over the range of reported idioms. In other words, the group with four idioms had experienced only about one more type of lifetime traumatic exposure than the group with no reported idioms. Comparing the percentage of the variance in idiom expression due to interpersonal trauma versus that due to dissociation reveals a higher contribution from the DES score (R2 = 17%) than from the BPSAQ (R2 = 4%). These findings suggest that there is indeed a relationship between the idioms and the degree of traumatic exposure, whether assessed as the number of distinct traumatic events (any-trauma severity) or as the persistence of trauma over time (child and adult trauma). The more salient finding, however, is that the group of patients at risk for the idioms in the context of interpersonal trauma is the group also at risk for dissociative reactions. This is consistent with a multifactorial model of the generation of dissociation and of idioms of distress, where traumatic exposure may be necessary for their generation but is clearly not sufficient (Hinton et al. 2009; Lewis-Fernández et al. 2002; van Ijzendoorn and Schuengel 1996).
To explore whether the associations we uncovered in the traumatized sample applied equally to the group without traumatic exposure, we ran the adjusted dichotomous model from Fig. 1 with the sample of participants with no trauma (n = 28). The only associations that held were between DES score and MDD and between DES score and altered perceptions (data available upon request). Although we lack the power to present these findings as proof of a “true” correlation among ataque, currently being ill with nerves and dissociation only in the context of traumatic exposure, this model does raise the question whether the relationships uncovered in this study largely depend on the presence of interpersonal trauma. Future studies with samples reporting greater variability in traumatic exposure should be conducted to examine this issue further.
Fourth, we are intrigued by the lack of relationship between the idioms of distress and the risk of current PTSD. The association between ataque and PTSD in a community sample in Puerto Rico (Guarnaccia et al. 1993) and the suggestive finding of a near association between ataque and PTSD in a much smaller but highly traumatized Spanish-dominant clinical sample of Puerto Rican immigrants (Lewis-Fernández et al. 2002) had led us to expect otherwise. In fact, current PTSD is not associated with any variable other than any-trauma severity in this study.
Why PTSD is not associated with DES score, as MDD is in nearly every model (except childhood-only trauma), is particularly curious. The relationships among trauma exposure, risk of PTSD and dissociation in diverse racial/ethnic samples are well documented and highly correlated (Carlson and Rosser-Hogan 1991; Johnson et al. 2001). We suggest three reasons why DES score and risk of current PTSD may not be associated in our traumatized sample. First, DES score is not always associated with risk of PTSD among trauma survivors (e.g., Chu and Dill 1990; Dancu et al. 1996; Realmuto et al. 1992), and this may be due in part to the type of dissociation assessed by the DES. Instruments that measure more state-like dissociation focused specifically on the traumatic exposure (e.g., “peritraumatic dissociation”) seem to show stronger correlations with PTSD than those, like the DES, which assess a person’s trait-like generalized dissociative capacity (Briere et al. 2005; Murray et al. 2002). The DES may not cover symptoms, such as numbing or stupor, which are highly prevalent acute reactions to trauma (Dancu et al. 1996), or DES scores may reflect a tendency to more transient dissociative experiences that may or may not become persistent with trauma (Murray et al. 2002). The present study may have failed to uncover a significant correlation between dissociation and PTSD diagnosis by focusing on generalized rather than trauma-specific dissociative experiences. Nevertheless, many studies have found an association between PTSD and dissociation using the DES (Bremner et al. 1992; Briere et al. 2005; Putnam et al. 1996).
Alternatively, the sensitivity of the SCID for current PTSD in this Spanish-dominant Latino sample may be reduced due to assessment limitations. Participants were asked about PTSD symptom endorsement resulting from one traumatic event identified by a single-item question on the SCID. Given the multiple traumatization experienced by this sample (mean number of traumas = 3.1), additional cases of PTSD might have been uncovered by a more comprehensive assessment of traumatic exposures. A recent study compared the rate of PTSD obtained by the SCID using a single-item assessment (25% of sample) versus that obtained using the multi-item Traumatic Life Events Questionnaire (TLEQ; 33% of sample). The authors attributed the higher rates obtained with the TLEQ to its multi-item approach to eliciting traumatic events, which may have facilitated participants’ recall of PTSD symptoms (Peirce et al. 2009). Moreover, PTSD symptoms can vary across cultures, especially the rate of avoidance symptoms (Hinton and Lewis-Fernández 2010a; Marsella et al. 1996). It is possible that differences in the salience of specific clusters of PTSD symptoms across Latino groups may have led to lower sensitivity of SCID diagnoses. This may in turn mask a potentially significant relationship between PTSD and the remaining variables, including dissociation.
A third explanation for the lack of association between dissociativity and PTSD involves growing evidence that this association depends in part on the type or mix of traumas and the cultural and psychological context in which the traumas occur. Certain traumas, such as nonsexual assault and childhood interpersonal trauma, may predict a relationship between dissociation and PTSD more strongly than other trauma types (Bryant 2007; Dancu et al. 1996). This may be due to the enhancement of dissociative defenses by early exposure to trauma or to the severe nature of some traumas, such as rape, which overwhelm dissociative defenses and break through into PTSD regardless of dissociative capacity. The association between dissociation and PTSD would then be reserved only for milder traumas (e.g., nonsexual assault), where dissociative reactions identify those survivors at greater risk for PTSD (Dancu et al. 1996). It is possible that we did not find an association between dissociation and PTSD because the elevated exposure to childhood trauma in our sample (85%) limited the variability of the effect of trauma on dissociativity. Moreover, other psychological factors could affect the relationship between dissociation and PTSD, including factors occurring before, during and after the traumatic exposure. These include affective regulation, tendency to hyperarousal, peritraumatic distress and cognitive style, including rumination and data-driven (as opposed to conceptual) processing of trauma memories (Briere et al. 2005; Bryant 2007; Murray et al. 2002). These factors are all affected by cultural parameters and were not measured in our study.
Taken together, our findings suggest that three of the idioms of distress we examined in this clinical sample of Spanish-dominant, immigrant Latinos—ataques de nervios, currently being ill with nerves and altered perceptions—are associated with each other and with generalized dissociative capacity. These relationships may depend in part on the presence of persistent or severe traumatic exposure. This nexus of associations suggests that dissociativity may be implicated in the excess morbidity associated with two of these idioms (ataque and altered perceptions) in a community sample of U.S. Latinos (Lewis-Fernández et al. 2009). Our finding that the relationship between the idioms and dissociation is largely independent of any relationship with PTSD or MDD is consistent with earlier studies showing that the morbidity associated with the idioms persists after adjusting for the effect of psychiatric disorder. Exactly what aspect of the relationship between the idioms and dissociativity is associated with excess morbidity remains to be clarified. Perhaps the level of catastrophizing about the dissociativity represented by the idioms is more important in this respect than simply their relationship to dissociation (Hinton et al. 2009). This would be consistent with cognitive findings on the key role of appraisal in moderating the pathogenic impact of panic-like experiences (which include the dissociative symptoms of depersonalization and derealization) in generating and maintaining psychiatric disorders (Clark 1986; Hinton et al. 2006, 2008b). Further research is needed to explore these issues.
Clinicians should remember that endorsement of the idioms in clinical settings could be a useful marker for the presence of dissociativity and possibly of trauma severity, independently of the presence or absence of PTSD or MDD. There is growing awareness of the clinical utility of including assessment of cultural idioms of distress in a mental health evaluation. Independently of their relationship to psychiatric diagnoses, idioms of distress can offer very useful information on the presence of interpersonal conflicts, economic distress, poor psychosocial functioning and severity of traumatization, among other factors (Hinton and Lewis-Fernández 2010b). Our findings suggest, in particular, that patients reporting ataques or altered perceptions should be assessed for suicidal ideation and behavior, given the salience of these associations in primary care and community settings (Lewis-Fernández et al. 2009; Olfson et al. 2002). Screening for the idioms should therefore accompany standard psychiatric evaluations of all Latino patients. Although our study focused on Spanish-dominant Latino immigrants, epidemiological surveys reveal even higher prevalence of ataques and altered perceptions among English-dominant, U.S.-born Latinos (Guarnaccia et al. 2010; Lewis-Fernández et al. 2009). The relationship between these idioms and dissociativity in English-speaking cohorts should be the focus of future studies.
The present study has several limitations. First, due to the limited sample size, we could not disaggregate the different Latino groups and retain sufficient power to examine the matrix of correlations. Second, the high prevalence of traumatic exposure in the sample did not allow us to test the associations between the variables in the absence of trauma. Likewise, low variability in the presence of MDD may have affected our ability to detect a relationship between MDD and the idioms of distress. This, however, was not the case with PTSD, and the results were similar with respect to both diagnoses. Third, we lack data on the lifetime prevalence of MDD and PTSD. It is possible that an association with the idioms would have been found if lifetime diagnoses were included. However, our approach has the advantage of focusing on current disorders, which are most relevant to clinical care. Fourth, the BPSAQ contains a more detailed assessment of childhood than adult trauma, and in fact only eight patients reported trauma only in adulthood. It is possible that an even more detailed evaluation of adult trauma would have affected our results, if the association of the idioms with traumatic exposure differed across time periods. In addition, the BPSAQ only assesses interpersonal trauma, which would limit our ability to detect a relationship between the idioms and other forms of trauma. Finally, the retrospective, self-reported data gathered for this study is subject to recall and other bias. Several factors, such as older age, psychological disorder or other comorbid conditions, can result in inaccurate recall. Dissociative experience itself, for instance, can inhibit one’s ability to remember past experiences (Marshall and Schell 2002). A prospective design would be necessary to address this limitation.
In conclusion, our data support the value of assessing idioms of distress in mental health evaluations alongside psychiatric disorders. Far from uninformed attributions superimposed on a universalistic set of syndromes, the idioms add useful clinical information, pointing to additional sources of morbidity and even potential psychological mechanisms that underlie and help shape the clinical presentation. Their broader inclusion in mental health research may help explain some of the missing variance in the relationship between symptomatology and levels of morbidity and distress. Future studies should focus on the mechanisms by which the idioms impact this relationship, such as through the patterning of culture-specific appraisals and interpretations of precipitants and reactions, including trauma-related conditions.
Acknowledgments
The authors wish to thank Ivan Balán, Gabriel Pantol, Lynne Matte, José Hernández, Paula Yáñez, Ashley Henderson, Michelle Bell and Melissa Rosario for their help conducting the study. This study was supported in part by the National Alliance for Research on Schizophrenia and Depression (NARSAD) and by institutional funds from the New York State Psychiatric Institute.
Contributor Information
Roberto Lewis-Fernández, Email: rlewis@nyspi.cpmc.columbia.edu, New York State Psychiatric Institute, 1051 Riverside Drive, New York, NY 10032, USA; Department of Psychiatry, Columbia College of Physicians & Surgeons, New York, NY, USA.
Magdaliz Gorritz, New York State Psychiatric Institute, 1051 Riverside Drive, New York, NY 10032, USA.
Greer A. Raggio, New York State Psychiatric Institute, 1051 Riverside Drive, New York, NY 10032, USA
Clara Peláez, Hospital Puerta de Hierro, Madrid, Spain.
Henian Chen, Department of Biostatistics, Winthrop University Hospital, Stony Brook University Medical School, Stony Brook, NY, USA.
Peter J. Guarnaccia, Institute for Health, Health Care Policy & Aging Research, Rutgers University, New Brunswick, NJ, USA
References
- Allison Paul D. Missing Data. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. Washington, DC: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- Bremner J Douglas, Southwick Steven, Brett Elizabeth, Fontana Alan, Rosenheck Robert, Charney Dennis S. Dissociation and Posttraumatic Stress Disorder in Vietnam Combat Veterans. American Journal of Psychiatry. 1992;149(3):328–332. doi: 10.1176/ajp.149.3.328. [DOI] [PubMed] [Google Scholar]
- Briere John, Scott Catherine, Weathers Frank. Peritraumatic and Persistent Dissociation in the Presumed Etiology of PTSD. American Journal of Psychiatry. 2005;162(12):2295–2301. doi: 10.1176/appi.ajp.162.12.2295. [DOI] [PubMed] [Google Scholar]
- Brown Richard J, Cardeña Etzel, Nijenhuis Ellert, Sar Vedat, van der Hart Onno. Should Conversion Disorder Be Reclassified as a Dissociative Disorder in DSM-V? Psychosomatics. 2007;48(5):369–378. doi: 10.1176/appi.psy.48.5.369. [DOI] [PubMed] [Google Scholar]
- Bryant Richard A. Does Dissociation Further Our Understanding of PTSD? Journal of Anxiety Disorders. 2007;21:183–191. doi: 10.1016/j.janxdis.2006.09.012. [DOI] [PubMed] [Google Scholar]
- Carlson Eve B, Rosser-Hogan Rhonda. Trauma Experiences, Posttraumatic Stress, Dissociation, and Depression in Cambodian Refugees. American Journal of Psychiatry. 1991;148(11):1548–1551. doi: 10.1176/ajp.148.11.1548. [DOI] [PubMed] [Google Scholar]
- Chang Doris F, Myers Hector F, Yeung Albert, Zhang Yalin, Zhao Jingping, Yu Shunying. Shenjing Shuairuo and the DSM-IV: Diagnosis, Distress, and Disability in a Chinese Primary Care Setting. Transcultural Psychiatry. 2005;42(2):204–218. doi: 10.1177/1363461505052660. [DOI] [PubMed] [Google Scholar]
- Chu James A, Dill Diana L. Dissociative Symptoms in Relation to Childhood Physical and Sexual Abuse. American Journal of Psychiatry. 1990;147(7):887–892. doi: 10.1176/ajp.147.7.887. [DOI] [PubMed] [Google Scholar]
- Clark David M. A Cognitive Approach to Panic. Behaviour Research and Therapy. 1986;24(4):461–470. doi: 10.1016/0005-7967(86)90011-2. [DOI] [PubMed] [Google Scholar]
- Dancu Constance V, Riggs David S, Hearst-Ikeda Diana, Shoyer Beth G, Foa Edna B. Dissociative Experiences and Posttraumatic Stress Disorder Among Female Victims of Criminal Assault and Rape. Journal of Traumatic Stress. 1996;9(2):253–267. doi: 10.1007/BF02110659. [DOI] [PubMed] [Google Scholar]
- David Daniella, Kutcher Gary S, Jackson Elizabeth I, Mellman Thomas A. Psychotic Symptoms in Combat-Related Posttraumatic Stress Disorder. Journal of Clinical Psychiatry. 1999;60(1):29–32. doi: 10.4088/jcp.v60n0106. [DOI] [PubMed] [Google Scholar]
- First Michael B, Spitzer Robert L, Gibbon Miriam, Williams Janet BW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I), Clinician Version, User’s Guide. Washington, DC: American Psychiatric Association; 1996. [Google Scholar]
- Guarnaccia Peter J, Guevara-Ramos Luz M, Gonzáles Gloria, Canino Glorisa J, Bird Héctor. Cross-Cultural Aspects of Psychotic Symptoms in Puerto Rico. Research in Community and Mental Health. 1992;7:99–110. [Google Scholar]
- Guarnaccia Peter J, Canino Glorisa, Rubio-Stipec Maritza, Bravo Milagros. The Prevalence of Ataques de Nervios in the Puerto Rico Disaster Study: The Role of Culture in Psychiatric Epidemiology. Journal of Nervous and Mental Disease. 1993;181(3):157–165. doi: 10.1097/00005053-199303000-00003. [DOI] [PubMed] [Google Scholar]
- Guarnaccia Peter J, Rivera Melissa, Franco Felipe, Neighbors Charlie. The Experiences of Ataques de Nervios: Towards an Anthropology of Emotions in Puerto Rico. Culture, Medicine and Psychiatry. 1996;20:343–367. doi: 10.1007/BF00113824. [DOI] [PubMed] [Google Scholar]
- Guarnaccia Peter J, Lewis-Fernández Roberto, Rivera Marano Melissa. Towards a Puerto Rican Popular Nosology: Nervios and Ataques de Nervios . Culture, Medicine and Psychiatry. 2003;27:339–366. doi: 10.1023/a:1025303315932. [DOI] [PubMed] [Google Scholar]
- Guarnaccia Peter J, Martínez Igda, Ramírez Rafael, Canino Gloria. Are Ataques de Nervios in Puerto Rican Children Associated with Psychiatric Disorder? Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44(11):1184–1192. doi: 10.1097/01.chi.0000177059.34031.5d. [DOI] [PubMed] [Google Scholar]
- Guarnaccia Peter J, Lewis-Fernández Roberto, Martínez Pincay Igda, Shrout Patrick E, Guo Jing, Torres Maria, Canino Glorisa, Alegría Margarita. Ataque de Nervios as a Marker of Social and Psychiatric Vulnerability: Results from the NLAAS. International Journal of Social Psychiatry. 2010 doi: 10.1177/0020764008101636. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton Devon E, Lewis-Fernández Roberto. The Cross-Cultural Validity of Posttraumatic Stress Disorder: Implications for DSM-V. Depression and Anxiety. 2010a doi: 10.1002/da.20753. Under review. [DOI] [PubMed] [Google Scholar]
- Hinton Devon E, Lewis-Fernández Roberto. “Idioms of Distress” (Culturally Salient Indicators of Distress) and Anxiety Disorders. In: Simpson Helen B, Neria Yuval, Lewis-Fernández Roberto, Schneier Frank S., editors. Anxiety Disorders: Theory, Research, and Clinical Perspectives. Cambridge: Cambridge University Press; 2010b. [Google Scholar]
- Hinton Devon, Um Khin, Ba Phalnarith. Kyol Goeu (“Wind Overload”) Part II: Prevalence, Characteristics, and Mechanisms of Kyol Goeu and Near-Kyol Goeu Episodes of Khmer Patients Attending a Psychiatric Clinic. Transcultural Psychiatry. 2001;38(4):433–460. doi: 10.1177/136346150103800402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton Devon E, Pich Vuth, Safren Steven A, Pollack Mark H, McNally Richard J. Anxiety Sensitivity Among Cambodian Refugees with Panic Disorder: A Factor Analytic Investigation. Journal of Anxiety Disorders. 2006;20(3):281–295. doi: 10.1016/j.janxdis.2005.02.006. [DOI] [PubMed] [Google Scholar]
- Hinton Devon E, Chong Roberto, Pollack Mark H, Barlow David H, McNally Richard J. Ataque de Nervios: Relationship to Anxiety Sensitivity and Dissociation Predisposition. Depression and Anxiety. 2008a;25(5):489–495. doi: 10.1002/da.20309. [DOI] [PubMed] [Google Scholar]
- Hinton Devon E, Hofmann Stefan G, Pitman Roger K, Pollack Mark H, Barlow David H. The Panic Attack-Posttraumatic Stress Disorder Model: Applicability to Orthostatic Panic Among Cambodian Refugees. Cognitive Behavior Therapy. 2008b;37(2):101–116. doi: 10.1080/16506070801969062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton Devon E, Lewis-Fernández Roberto, Pollack Mark H. A Model of the Generation of Ataque de Nervios: The Role of Fear of Negative Affect and Fear of Arousal Symptoms. CNS Neuroscience & Therapeutics. 2009;15(3):264–275. doi: 10.1111/j.1755-5949.2009.00101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson Dawn M, Pike Julie L, Chard Kathleen M. Factors Predicting PTSD, Depression, and Dissociative Severity in Female Treatment-Seeking Childhood Sexual Abuse Survivors. Child Abuse and Neglect. 2001;25(1):179–198. doi: 10.1016/s0145-2134(00)00225-8. [DOI] [PubMed] [Google Scholar]
- Johnson Jeffrey G, Cohen Patricia, Kasen Stephanie, Brook Judith S. Dissociative Disorders Among Adults in the Community, Impaired Functioning, and Axis I and II Comorbidity. Journal of Psychiatric Research. 2006;40(2):131–140. doi: 10.1016/j.jpsychires.2005.03.003. [DOI] [PubMed] [Google Scholar]
- Liebowitz Michael R, Salmán Ester, Jusino Carlos M, Garfinkel Robin, Street Linda, Cárdenas Dora L, Silvestre Joao, Fyer Abby J, Carrasco José L, Davies Sharon, Guarnaccia Peter, Klein Donald F. Ataque de Nervios and Panic Disorder. American Journal of Psychiatry. 1994;151(6):871–875. doi: 10.1176/ajp.151.6.871. [DOI] [PubMed] [Google Scholar]
- Lewis-Fernández Roberto. A Comparison About Ataque de Nervios Among Puerto Ricans and Possession Syndrome in India. In: Spiegel David., editor. Dissociation, Culture, Mind and Body. Washington, DC: American Psychiatric Press; 1994. pp. 123–171. [Google Scholar]
- Cultural Formulation of Psychiatric Diagnosis. Case No. 02. Diagnosis and Treatment of Nervios and Ataques in a Female Puerto Rican Migrant. Culture, Medicine and Psychiatry. 1996;20:155–163. doi: 10.1007/BF00115860. [DOI] [PubMed] [Google Scholar]
- Eso No Estaba en Mí… No Pude Controlarme: El Control, la Identidad y las Emociones en Comunidades Puertorriqueñas [That Was Not in Me… I Could Not Control Myself: Control, Identity, and Emotion in Puerto Rican Communities] Revista de Ciencias Sociales (Puerto Rico) 1998;4:268–299. [Google Scholar]
- Lewis-Fernández Roberto, Garrido-Castillo Pedro, Bennasar Mari Carmen, Parrilla Elsie M, Laria Amaro J, Ma Guoguang, Petkova Eva. Dissociation, Childhood Trauma, and Ataque de Nervios Among Puerto Rican Psychiatric Outpatients. American Journal of Psychiatry. 2002;159(9):1603–1605. doi: 10.1176/appi.ajp.159.9.1603. [DOI] [PubMed] [Google Scholar]
- Lewis-Fernández Roberto, Guarnaccia Peter J, Patel Sapana, Lizardi Dana, Diaz Naelys. Ataque de Nervios: Anthropological, Epidemiological and Clinical Dimensions of a Cultural Syndrome. In: Georgiopoulos AM, Rosenbaum JF, editors. Perspectives in Cross-Cultural Psychiatry. Philadelphia: Lippincott Williams and Wilkins; 2005. pp. 63–85. [Google Scholar]
- Lewis-Fernández Roberto, Martínez-Taboas Alfonso, Sar Vedat, Patel Sapana, Boatin Adeline. The Cross-Cultural Assessment of Dissociation. In: Wilson JP, So-Kum Tang C, editors. The Cross-Cultural Assessment of Psychological Trauma and PTSD. New York: Springer; 2007. pp. 279–319. [Google Scholar]
- Lewis-Fernández Roberto, Horvitz-Lennon Marcela, Blanco Carlos, Guarnaccia Peter J, Cao Zhun, Alegría Margarita. Significance of Endorsement of Psychotic Symptoms by US Latinos. Journal of Nervous and Mental Disease. 2009;197(5):337–347. doi: 10.1097/NMD.0b013e3181a2087e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little Roderick JA, Rubin Donald B. Statistical Analysis with Missing Data. New York: John Wiley & Sons; 2002. [Google Scholar]
- Low Setha M. The Meaning of Nervios: A Sociocultural Analysis of Symptom Presentation in San Jose, Costa Rica. Culture, Medicine and Psychiatry. 1981;5:25–47. doi: 10.1007/BF00049157. [DOI] [PubMed] [Google Scholar]
- Marsella Anthony J, Friedman Matthew J, Gerrity Ellen T, Surfield Raymond M. Ethnocultural Aspects of PTSD: Some Closing Thoughts. In: Marsella AJ, Friedman MJ, Gerrity ET, Scurfield RM, editors. Ethnocultural Aspects of Posttraumatic Stress Disorder: Issues, Research, Clinical Applications. Washington, DC: American Psychological Association; 1996. pp. 529–538. [Google Scholar]
- Marshall Grant M, Schell Terry L. Reappraising the Link Between Peritraumatic Dissociation and PTSD Symptom Severity: Evidence from a Longitudinal Study of Community Violence Survivors. Journal of Abnormal Psychology. 2002;111(4):626–636. doi: 10.1037//0021-843x.111.4.626. [DOI] [PubMed] [Google Scholar]
- Marshall Randall D, Schneier Franklin R, Fallon Brian A, Knight Charles BG, Abbate Linda A, Goetz Deborah, Campeas Raphael, Liebowitz Michael R. An Open Trial of Paroxetine in Patients with Non-Combat-Related, Chronic Posttraumatic Stress Disorder. Journal of Clinical Psychopharmacology. 1998;18(1):10–18. doi: 10.1097/00004714-199802000-00003. [DOI] [PubMed] [Google Scholar]
- Martínez-Taboas Alfonso. The Use of the Dissociative Experiences Scale in Puerto Rico. Dissociation. 1995;8(1):14–23. [Google Scholar]
- Martínez-Taboas Alfonso, Lewis-Fernández Roberto, Sar Vedat, Agarwal Arun Lata. Cultural Aspects of Psychogenic Nonepileptic Seizures. In: Schachter Steven C, Curt LaFrance W., editors. Gates and Rowan’s Nonepileptic Seizures. 3rd Edition. Cambridge, UK: Cambridge University Press; 2001. pp. 121–130. [Google Scholar]
- Mueser Kim T, Butler Robert W. Auditory Hallucinations in Combat-Related Chronic Posttraumatic Stress Disorder. American Journal of Psychiatry. 1987;144(3):299–302. doi: 10.1176/ajp.144.3.299. [DOI] [PubMed] [Google Scholar]
- Murray James, Ehlers Anke, Mayou Richard A. Dissociation and Post-Traumatic Stress Disorder: Two Prospective Studies of Road Traffic Accident Survivors. British Journal of Psychiatry. 2002;180:363–368. doi: 10.1192/bjp.180.4.363. [DOI] [PubMed] [Google Scholar]
- Nichter Mark. Idioms of Distress: Alternatives in the Expression of Psychosocial Distress: A Case Study from South India. Culture, Medicine and Psychiatry. 1981;5:379–408. doi: 10.1007/BF00054782. [DOI] [PubMed] [Google Scholar]
- Olfson Mark, Lewis-Fernández Roberto, Weissman Myrna M, Feder Adriana, Gemeroff Marc J, Pilowsky Daniel, Fuentes Milton. Psychotic Symptoms in an Urban General Medicine Practice. American Journal of Psychiatry. 2002;159(8):1412–1419. doi: 10.1176/appi.ajp.159.8.1412. [DOI] [PubMed] [Google Scholar]
- Ozer Emily J, Best Suzanne R, Lipsey Tami L, Weiss Daniel S. Predictors of Posttraumatic Stress Disorder and Symptoms in Adults: A Meta-Analysis. Psychological Bulletin. 2003;129(1):52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Realmuto George M, Masten Ann, Carole Linda Flies, Hubbard Jon, Groteluschen Andrea, Chhun Bunchean. Adolescent Survivors of Massive Childhood Trauma in Cambodia: Life Events and Current Symptoms. Journal of Traumatic Stress. 1992;5(4):589–599. [Google Scholar]
- Peirce Jessica M, Burke Christopher K, Stoller Kenneth B, Neufeld Karin J, Brooner Robert K. Assessing Traumatic Event Exposure: Comparing the Traumatic Life Events Questionnaire to the Structured Clinical Interview for DSM-IV. Psychological Assessment. 2009;21(2):210–218. doi: 10.1037/a0015578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posternak Michael A, Zimmerman Mark. Elevated Rates of Psychosis Among Treatment-Seeking Hispanic Patients with Major Depression. Journal of Nervous and Mental Disease. 2005;193(1):66–69. doi: 10.1097/01.nmd.0000149222.02563.be. [DOI] [PubMed] [Google Scholar]
- Putnam Frank W, Carlson Eve B, Ross Colin A, Anderson Geri, Clark Patti, Torem Moshe, Bowman Elizabeth S, Coons Philip, Chu James A, Dill Diana L, Loewenstein Richard J, Braun Bennett G. Patterns of Dissociation in Clinical and Nonclinical Samples. Journal of Nervous and Mental Disease. 1996;194(11):673–679. doi: 10.1097/00005053-199611000-00004. [DOI] [PubMed] [Google Scholar]
- Salgado De Snyder V. Nelly, Díaz-Pérez De Jesús, Ojeda Victoria D. The Prevalence of Nervios and Associated Symptomatology hmong Inhabitants of Mexican Rural Communities. Culture, Medicine and Psychiatry. 2000;24:453–470. doi: 10.1023/a:1005655331794. [DOI] [PubMed] [Google Scholar]
- Salmán Ester, Liebowitz Michael R, Guarnaccia Peter J, Jusino Carlos M, Garfinkel Robin, Street Linda, Cárdenas Dora L, Silvestre João, Fyer Abby J, Carrasco José L, Davies Sharon O, Klein Donald F. Subtypes of Ataques de Nervios: The Influence of Coexisting Psychiatric Diagnosis. Culture, Medicine and Psychiatry. 1998;22:231–244. doi: 10.1023/a:1005326426885. [DOI] [PubMed] [Google Scholar]
- Schafer Joseph L. Analysis of Incomplete Multivariate Data. London: Chapman & Hall; 1997. [Google Scholar]
- Schechter Daniel S, Marshall Randall, Salmán Ester, Goetz Deborah, Davies Sharon, Liebowitz Michael R. Ataque de Nervios and History of Childhood Trauma. Journal of Traumatic Stress. 2000;13(3):529–534. doi: 10.1023/A:1007797611148. [DOI] [PubMed] [Google Scholar]
- Takeuchi David T, Chun Chi-Ah, Gong Fang, Shen Haikang. Cultural Expressions of Distress. Health: An Interdisciplinary Journal for the Social Study of Health, Illness and Medicine. 2002;6(2):221–235. [Google Scholar]
- van Ijzendoorn Marinus H, Schuengel Carlo. The Measurement of Dissociation in Normal and Clinical Populations: Meta-analytic Validation of the Dissociative Experiences Scale (DES) Clinical Psychological Review. 1996;16(5):365–382. [Google Scholar]