Abstract
Background Context
Central cord syndrome (CCS) is a common cause of incomplete spinal cord injury. However, to date, national trends in the management and mortality following central cord syndrome are not fully understood.
Purpose
To analyze how patient, surgical and institutional factors influence surgical management and mortality following CCS.
Study Design/Setting
Retrospective cohort analysis
Patient Sample
The Nationwide Inpatient Sample (NIS) was queried for records of patients with a diagnosis of CCS from 2003 through 2010.
Outcome Measures
In-hospital mortality and surgical management, including anterior cervical decompression and fusion (ACDF), posterior cervical decompression and fusion (PCDF), and posterior cervical decompression (PCD).
Methods
Using ICD9-CM codes, patient records with a diagnosis of CCS from 2003–2010 were selected from the NIS database and sorted by in-patient mortality and surgical management. Demographic information (age, gender, race) and hospital characteristics were evaluated with χ2-tests for categorical variables and T-tests for continuous variables. Multivariate logistic regression models controlled for confounding. The authors report no sources of funding or conflicts of interest related to this study.
Results
In this sample of 16,134 patients, a total of 39.7% of patients (6,351) underwent surgery. ACDF was most common (19.4%), followed by PCDF (7.4%) and PCD (6.8%). From 2003–10, surgical management increased by an average of 40% each year. The overall inpatient mortality rate was 2.6%
Increasing age and comorbidities were associated with higher rates of patient mortality and a decreasing surgical rate (p < 0.01). Hospitals greater than 249 beds (p < 0.01) and the south (p < 0.01) were associated with a higher surgical rate. Rural hospitals (p < 0.01) and persons in the second income quartile (p < 0.01) were associated with higher inpatient mortality.
Conclusion
Elderly patients with medical comorbidities are associated with a lower surgical rate and a higher mortality rate. Surgical management was more prevalent in the south and large hospitals. Mortality was higher in rural hospitals. It is important for surgeons to understand how patient, surgical and institutional factors influence surgical management and mortality.
Introduction
Central cord syndrome (CCS), the most common incomplete spinal cord injury, is a debilitating disorder with an incidence of approximately 11,000 cases a year.1 CCS commonly affects older adults with underlying cervical spondylosis who sustain a hyperextension injuries.2 Spinal cord pathology is primarily associated with the medial portion of the lateral corticospinal tract in the cervical spine.3
Historically initial treatment was often conservative. Physical/occupational therapy and corticosteroid therapy have been commonly encouraged prior to the decision for surgery.4 However, it has been shown that many CCS patients plateau prior to worsening.5 Moreover the STASCIS study, published in 2012, has demonstrated the benefits of early decompression (<24 hrs) in regaining motor strength compared to late decompression (>24 hours) following cervical spinal cord injury.6
The extent of neurological deficit often correlates with surgical urgency.7 CCS may be managed surgically with anterior cervical decompression and fusion (ACDF), posterior cervical decompression and fusion (PCDF), and/or posterior cervical decompression (PCD) alone. Most agree that surgical management is safe and prudent in the treatment of acute fractures and disc herniations, but there is still some disagreement regarding the role of surgery in classic CCS.
CCS has not been examined on a national scale except for a recent analysis by Yoshihara and Yoneoka.8 The present study examined national inpatient surgical and mortality characteristics in a population of cervical CCS patients using discharge data from the Nationwide Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality.9 Awareness of associations between patient demographics, comorbidities, hospital characteristics, and outcomes on an epidemiological level may influence the care of CCS patients. The aim of our study was to analyze how patient, surgical and institutional factors influence surgical management and mortality.
Materials/Methods
Data source
Nationwide Inpatient Sample (NIS) hospital discharge data from the Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality (AHRQ), Rockville, MD was used in this study.9 The NIS is the largest all-payer inpatient care administrative database in the United States, containing discharge records organized according to the procedure and diagnostic codes from the International Classification of Diseases, Ninth Revision, Clinical Modification. Each annual data set is approximately 8 million records and represents a 20% random sample of hospitals in the country, stratified by geographic region, teaching status, hospital size, and other characteristics. Discharge weights were applied to all records in the appropriate strata to extrapolate to the entire United States population, and the 2010 data was most recent at the time of analysis.
Inclusion criteria
For the years 2003–2010, 16,134 discharge records with a cervical Central Cord Syndrome diagnosis were selected (ICD9-CM codes 952.03 and 952.08).
Patient characteristics
Patient characteristics (age, sex, race, median household income by zip code, insurance type, comorbidities, fractures) and outcomes (length of stay, discharge disposition and inpatient death) were selected from the data set. All demographic information is listed in Table 1.
Table 1.
Patient, Hospital, and Outcome Characteristics Summary
| Characteristic | No. of Patients | (%) | |
|---|---|---|---|
| Age | 0–49 | 4,455 | 27.6% |
| 50–64 | 5,662 | 35.1% | |
| 65–79 | 4,120 | 25.5% | |
| ≥80 | 1,896 | 11.8% | |
|
| |||
| Sex | Male | 12,048 | 74.7% |
| Female | 4,086 | 25.3% | |
|
| |||
| Race | White | 11,217 | 69.5% |
| Black | 3,024 | 18.7% | |
| Hispanic | 1,021 | 6.3% | |
| Other | 872 | 5.4% | |
|
| |||
| Income Quartile* | Q1 | 4,770 | 29.6% |
| Q2 | 3,963 | 24.6% | |
| Q3 | 3,865 | 24.0% | |
| Q4 | 3,535 | 21.9% | |
|
| |||
| Primary Payer | Private | 6,110 | 37.9% |
| Medicare | 5,934 | 36.8% | |
| Medicaid | 1,648 | 10.2% | |
| Other | 2,442 | 15.1% | |
|
| |||
| Location, hospital | Rural | 807 | 5.0% |
| Urban | 15,327 | 95.0% | |
|
| |||
| Region, hospital | NE | 3,456 | 21.4% |
| MW | 2,993 | 18.6% | |
| S | 6,560 | 40.7% | |
| W | 3,124 | 19.4% | |
|
| |||
| Teaching status | Non-teaching | 5,195 | 32.2% |
| Teaching | 10,939 | 67.8% | |
|
| |||
| Bed size | Small (1–249) | 700 | 4.3% |
| Medium (250–449) | 3,209 | 19.9% | |
| Large (≥450) | 12,226 | 75.8% | |
|
| |||
| Associated Fracture | Upper Limb | 397 | 2.5% |
| Lower Limb | 241 | 1.5% | |
| Hip | 37 | 0.2% | |
|
| |||
| Comorbidities | 0 | 3,567 | 22.1% |
| 1 | 4,075 | 25.3% | |
| 2 | 3,579 | 22.2% | |
| ≥3 | 4,913 | 30.5% | |
|
| |||
| Length of Stay | < 5 days | 10,478 | 64.9% |
| ≥5 days | 5,656 | 35.1% | |
|
| |||
| Discharge | Routine | 6,013 | 37.3% |
| Disposition | Not Routine | 10,121 | 62.7% |
|
| |||
| In-patient mortality | 414 | 2.6% | |
| Surgical Treatment | 6,351 | 39.4% | |
Median household income national quartile for patient zip code
The CCS sample was overwhelmingly male (74.7%), and predominantly Caucasian (69.5%), African American (18.7%), and Hispanic (6.3%). The mean age was 58.9 (CI: 58.1–59.6; SE: 0.4). 27.6% of patients were below 50 years of age, 35.1% were between 50 and 64, 25.5% between 65 and 79, and 11.8% over 80 years. The household income quartile by zip code estimates are updated on an annual basis. The 2010 quartiles were: $1–$40,999; $41,000–$50,999; $51,000–$66,900; $67,000+. In this population, 29.6% of patients were listed in Q1, followed by 24.6% in Q2, 24.0% in Q3 and 21.9% in Q4. Regarding the primary payer, 37.9% were classified as private, 36.8% as Medicare, 10.2% as Medicaid, and 15.1% as other.
A total of 29 comorbidities according to Elixhauser, et al. were selected.10 Additionally, associated fracture data was divided into four categories: hip, upper limb, lower limb, and combinations of the above possibilities. Fractures were defined by the diagnostic Clinical Classifications Software for ICD-9 CM. Upper limb fractures were most common (2.5%), followed by lower limb (1.5%) and hip fractures (0.2%) (Table 1). The mean hospital length of stay (LOS) was 10.4 days (CI: 9.8–11.0; SE: 0.3), and inpatient mortality rate was 2.6% (CI: 2.0%–3.1%; SE: 0.3%) for the entire sample.
Surgical Characteristics
Patients were grouped based on surgical treatment (ACDF, PCDF, PCD ICD-9 CM procedure codes 81.02, 8103, and 0309, respectively). For those patients receiving surgery (n=6,351), ACDF was most common (19.4%), followed by PCDF (7.4%) and then PCD (6.8%). Combinations of these surgeries occurred at a lower proportion of the time (PCDF, PCD: 2.4%; ACDF, PCDF: 2.3%; ACDF, PCD: 0.9%; ACDF, PCDF, PCD: 0.2%). 60.6% of the sample was managed non-operatively.
Institutional Characteristics
Hospital characteristics (type, size, region, hospital charges) were analyzed for all patients. The teaching status as designated by the AHA Annual Survey of Hospitals is given if a hospital has an AMA-approved residency program, is a member of the Council of Teaching Hospitals (COTH) or has a ratio of full-time equivalent interns and residents to beds of .25 or higher. 32.3% hospitals were associated with the teaching status in this sample. Additionally, large hospitals (> 449) beds held 75.8% of the CCS patients. Geographically, most patients were in the south (40.7%), followed by 21.4% in the northeast, 19.4% in the west, and 18.6% in the Midwest. Mean total charges were $77,178 (CI: $72,061–$82,295; SE: $2,606).
Statistical analysis
Patients were grouped based on inpatient mortality and surgical treatment. Frequency differences between groups for all characteristics were compared using χ2-tests analysis for categorical variables and Independent Sample T-tests for continuous variables (Table Two). In order to control for other variables while assessing associations, multivariate logistic regression was performed for the binary variables surgical treatment (Yes/No) and inpatient mortality (Yes/No). These associations were described with odds ratios (Table Three, Table Four). The independent variables used in the multivariate analysis were chosen based on univariate significance. P ≤ 0.05 was considered significant for all tests. A record was excluded from the model if missing values were present. Stata software (version 12.0; StataCorp, College Station, TX, USA) running on Mac OS X was used for all statistical analyses.
Table 2.
Patient, Hospital, and Outcome Characteristics; Comparison in Mortality and Surgical Treatment Groups
| Characteristic | Surgery (ACDF, PCDF, or PCD) | P-Value | In-Patient Mortality | P-Value | |||
|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | ||||
| Age (Years) | Mean (SE) | 58.5 (.43) | 59.1 (.47) | 0.33 | 73.7 (1.2) | 58.5 (.37) | < 0.01 |
| 95% CI | 57.7 – 59.4 | 58.2–60.0 | 71.3–76.1 | 57.8–59.2 | |||
|
| |||||||
| Age (%) | 0–49 | 27.1% | 28.0% | < 0.01 | 3.6% | 28.2% | < 0.01 |
| 50–64 | 37.8% | 33.3% | 20.8% | 35.5% | |||
| 65–79 | 27.4% | 24.4% | 40.8% | 25.1% | |||
| ≥80 | 7.8% | 14.3% | 34.8% | 11.1% | |||
|
| |||||||
| Sex (%) | Male | 76.1% | 73.7% | 0.12 | 76.8% | 74.6% | 0.63 |
| Female | 23.9% | 26.3% | 23.2% | 25.4% | |||
|
| |||||||
| Race (%) | White | 68.0% | 69.9% | 0.08 | 76.3% | 69.3% | 0.488 |
| Black | 19.8% | 18.4% | 15.7% | 18.8% | |||
| Hispanic | 7.0% | 6.2% | 3.4% | 6.4% | |||
| Other | 5.2% | 5.5% | 4.6% | 5.4% | |||
|
| |||||||
| Income quartile | Q1 | 30.6% | 28.9% | 0.26 | 16.7% | 29.9% | < 0.01 |
| Q2 | 25.2% | 24.2% | 39.9% | 24.2% | |||
| Q3 | 24.1% | 23.9% | 25.1% | 23.9% | |||
| Q4 | 20.1% | 23.1% | 18.4% | 22.0% | |||
|
| |||||||
| Primary Payer | Private | 38.8% | 37.3% | 0.054 | 19.8% | 38.3% | < 0.01 |
| Medicare | 35.4% | 37.7% | 63.3% | 36.1% | |||
| Medicaid | 10.8% | 9.8% | 3.6% | 10.4% | |||
| Other | 15.0% | 15.2% | 13.3% | 15.2% | |||
|
| |||||||
| Charges (US $) | Mean (SE) | 117,106 (4,362) | 51,260 (1,968) | <0.01 | 137,223 (16,541) | 75,597 (2,630) | <0.01 |
| 95% CI | 108,540–125,673 | 47,395–55,125 | 104,746–169,701 | 70,433–80,762 | |||
|
| |||||||
| Location (%) | Rural | 4.2% | 5.5% | 0.79 | 9.7% | 4.9% | < 0.05 |
| Urban | 95.4% | 94.5% | 90.3% | 95.1% | |||
|
| |||||||
| Region (%) | NE | 19.9% | 22.4% | < 0.05 | 27.6% | 21.3% | 0.32 |
| MW | 16.9% | 19.6% | 22.0% | 18.5% | |||
| S | 44.9% | 37.9% | 36.3% | 40.8% | |||
| W | 18.3% | 20.1% | 14.0% | 19.5% | |||
|
| |||||||
| Teaching status (%) | Non-teach. | 30.8% | 33.1% | 0.291 | 27.5% | 32.3% | 0.37 |
| Teaching | 69.2% | 66.9% | 72.5% | 67.7% | |||
|
| |||||||
| Bed size (%) | Small (1–249) | 2.7% | 5.4% | < 0.01 | 5.3% | 4.3% | 0.28 |
| Medium (250–449) | 20.4% | 19.6% | 26.2% | 19.7% | |||
| Large (≥450) | 76.9% | 75.0% | 68.5% | 76.0% | |||
|
| |||||||
| Associated Fracture | Upper Limb | 1.9% | 2.5% | 0.23 | 1.2% | 2.3% | 0.35 |
| Lower Limb | 1.0% | 1.5% | 2.6% | 1.3% | |||
| Hip | 0.0% | 0.2% | 0.0% | 0.2% | |||
| Combination* | 0.3% | 0.2% | 1.1% | 0.2% | |||
|
| |||||||
| Comorbidities | 0 | 21.1% | 22.7% | 0.738 | 12.8% | 22.4% | < 0.05 |
| 1 | 26.0% | 24.7% | 19.8% | 25.4% | |||
| 2 | 22.2% | 22.1% | 22.7% | 22.2% | |||
| ≥3 | 30.6% | 30.4% | 44.7% | 30.1% | |||
|
| |||||||
| Average LOS (Days) | Mean (SD) | 11.6 (.50) | 9.7 (.35) | < 0.01 | 14.1 (1.97) | 10.3 (.30) | < 0.05 |
| 95% CI | 10.6–12.6 | 8.9–10.3 | 10.3–17.9 | 9.8–10.9 | |||
|
| |||||||
| LOS (%) | < 5 days | 73.3% | 59.5% | < 0.01 | 79.5% | 64.6% | < 0.01 |
| ≥ 5 days | 26.7% | 40.5% | 20.5% | 35.4% | |||
|
| |||||||
| Discharge Type (%) | Routine | 32.9% | 40.1% | < 0.01 | 0.0% | 38.3% | < 0.01 |
| Not Routine | 67.1% | 59.9% | 100.0% | 61.7% | |||
|
| |||||||
| In-patient mortality rate | 3.0% | 1.9% | 0.045 | 100.0% | 0.0% | - | |
Combination denotes any patient with concomitant upper, lower, and/or hip fractures.
Table 3.
Odds ratios and 95% CIs for patient and hospital characteristics in the multivariate analyses predictive of the likelihood of surgery
| Characteristic | Surgery (ACDF, PCF, or PCD) | |||
|---|---|---|---|---|
| OR | CI | p | ||
| Age | 0–49* | - | - | - |
| 50–64 | 1.1 | 0.9–1.3 | 0.4 | |
| 65–79 | 1.2 | 0.9–1.6 | 0.6 | |
| ≥80 | 0.7 | 0.5–0.9 | < 0.01 | |
|
| ||||
| Region, hospital | NE* | - | - | - |
| MW | 1.1 | 0.8–1.5 | 0.6 | |
| S | 1.3 | 1.1–1.7 | < 0.01 | |
| W | 1.1 | 0.8–1.4 | 0.5 | |
|
| ||||
| Bed size (%) | Small (1–249)* | - | - | - |
| Medium (250–449) | 1.9 | 1.1–3.2 | < 0.01 | |
| Large (≥450) | 1.9 | 1.2–3.2 | < 0.01 | |
|
| ||||
| Discharge Type (%) | Routine* | - | - | - |
| Not Routine | 1.3 | 1.1–1.5 | < 0.01 | |
|
| ||||
| Anemia Deficiency | 0.8 | 0.6–1 | < 0.05 | |
| Renal Failure | 0.7 | 0.5–0.9 | < 0.05 | |
|
| ||||
| LOS | < 5 days* | - | - | - |
| ≥ 5 days | 0.6 | 0.5–0.7 | < 0.01 | |
Reference group for comparison
Table 4.
Odds ratios and 95% CIs for patient and hospital characteristics in the multivariate analyses predictive of in-patient mortality
| Characteristic | Inpatient Mortality | |||
|---|---|---|---|---|
| OR | CI | p | ||
| Age | 0–49* | - | - | - |
| 50–64 | 4.4 | 1.2–16.3 | < 0.05 | |
| 65–79 | 13.6 | 2.7–67.7 | < 0.01 | |
| ≥80 | 20.4 | 4.0–104.2 | < 0.01 | |
|
| ||||
| Income Quartile | Q1* | - | - | - |
| Q2 | 3.4 | 1.8–6.6 | < 0.01 | |
| Q3 | 1.9 | 0.9–3.8 | 0.1 | |
| Q4 | 1.7 | 0.8–3.7 | 0.2 | |
|
| ||||
| Location, Hospital | Rural* | - | - | - |
| Urban | 0.5 | 0.2–0.8 | < 0.01 | |
|
| ||||
| Congestive Heart Failure | 2.9 | 1.3–6.7 | < 0.01 | |
| Coagulation Deficiency | 2.9 | 1.1–7.6 | < 0.05 | |
| Diabetes Mellitus, uncomp. | 2.0 | 1.3–4.6 | < 0.05 | |
| Weight Loss | 3.4 | 1.6–7.2 | < 0.01 | |
Reference group for comparison
Results
Factors associated with surgical management
In terms of patient characteristics, the operative group’s mean age was 58.5 compared to a mean age of 59.1 for the non-operative group; the difference in mean age was not significant (p>0.05) (Table 2). Multivariate analysis demonstrated decreased odds for surgery in the greater than 79 age group relative to the younger than 50 group (OR: 0.7; CI: 0.5–0.9; p<0.01) (Table 3). The Medicaid population had the highest surgical rate, private insurance was second, and Medicare was third; differences in surgical rate between primary payer groups approached significance at p=0.054. Decreased surgical management was associated with anemia deficiency (OR:0.76; CI:0.59–0.97; p<0.05) and renal failure (OR: 0.70; CI: 0.49–0.99; p<0.05).
When comparing the operative to the non-operative group, the mean LOS was longer (11.6 vs 9.7 days; p<0.01) and average total charges were higher ($117,106, SE: $4,362 vs $51,206, SE: $1,968; p<0.01) (Table 2). Univariate and multivariate analysis demonstrated that, compared to the non-operative cohort, a higher proportion of operative patients were in the hospital for less than 5 days (p<0.01, OR: 0.6) (Table 2, 3).
Surgery was more common at medium (250–449 beds) and large (>449 beds) hospitals compared to the small counterparts (less than 250 beds) (OR: 1.9; CI: 1.2–3.2; p<0.01 and OR: 1.9; CI: 1.2–3.1; p<0.01) (Table 2). Multivariate analysis also demonstrated that surgical treatment was more common in the south (OR: 1.3; CI: 1.1–1.7; p<0.01) relative to the northeast (Table 3).
Univariate analysis did not show a significant difference in surgery between sex, race, income quartiles, primary payer, location (rural/urban), teaching status, associated fractures, or number of comorbidities (Table 2).
Factors associated with mortality
Univariate analysis demonstrated significant associations between inpatient mortality and age (p<0.01, Table 2). In the group that experienced mortality, 34.8% of patients were older than 79 years. Comparatively, 11.1% of the survival group was in this age category (Table 2). A significantly smaller proportion of the group less than 50 years old experienced mortality. Each of the age groups above 49 years had incrementally greater odds of inpatient mortality relative to the group under age 50 (Age 50–64 OR: 4.4, CI: 1.2–16.3, p<0.05; 65–79 OR: 13.6, CI: 2.7–67.7, p<0.01; 80 and above OR: 20.4; CI: 4.0–104.2, p<0.01) (Table 4).
Not accounting for age, there was a significant increase in mortality for patients using Medicare relative to those enrolled in Medicaid and private insurance (p<0.01) (Table 2). When all other variables were held constant in the logistic regression, the primary payer was not detected as a significant factor for the prediction of inpatient mortality.
A significant difference in groups was noted in which the bottom quartile and top quartile had the lowest mortality rates, while the second income quartile showed an increase in mortality rate (p<0.01) (Table 2). Patients in the second income quartile had 2.8 times the risk of mortality relative to those in the first quartile (OR: 2.8; CI: 1.4–5.7) (Table 4). Additionally, rural hospitals were associated with a higher mortality rate (OR: 0.5; CI: 0.2–0.8; p<0.05) (Table 4).
Increased mortality was associated with congestive heart failure (OR: 2.9; CI: 1.3–6.6; p<0.01), weight loss (OR:3.4; CI:1.6–7.2; p<0.01), coagulation deficiency (OR: 2.93; CI:1.4–7.6; p<0.05), and uncomplicated diabetes mellitus (OR: 2.0; CI:1.0–3.8; p<0.05).
The following characteristics showed significant differences between mortality groups in univariate testing but did not show significance in logistic regression: LOS, discharge type, location (rural/urban), and charges. Univariate analysis did not show significant differences in the following characteristics: sex, race, region, teaching status, bed size, or associated fractures.
Discussion
Our study substantiates and extends the existing body of CCS research, as we are able to stratify our CCS sample on a variety of variables, including age and comorbidities. The present study found the following patterns:
Inpatient mortality
In the current study, the population of patients was predominantly men, with an overall inpatient mortality rate of 2.6%. Patients who died in the hospital were on average older (73.7 vs. 58.5; p<0.01). Medicare patients, the oldest payer cohort, faced an increased rate of mortality.
Increased mortality risk among the elderly is likely related to this group’s elevated rate of comorbidities. Several comorbidities were associated with a significant increase in mortality (congestive heart failure, weight loss, coagulation deficiency, and uncomplicated diabetes mellitus). These risk factors that should be taken into account in the surgical decision-making process.
Negative prognosis may be related to increasing levels of atherosclerosis in the vertebral vasculature in the elderly, leading to greater levels of cervical spondylosis and cord ischemia. Prior studies have identified increasing age and comorbidities as negatively associated with CCS outcome. 7,11,12,13,14,15,16 In a retrospective study with 32 patients, Newey et al. show that patients greater than 70 have increased rates of adverse outcomes.13 Tow and Kong show that the absence of spasticity and younger age are associated with improved functional outcomes.14 Lenehan demonstrates that both motor and sensory improvements following traumatic CCS were greatest in patients less than 50 years of age.7 Penrod et al. showed that younger patients recover ambulation more frequently than the older cohort.15 In both conservative and surgically managed groups, Aito noted that patients older than 65 suffer from a greater neurologic deterioration than the younger age group.16
It was unexpected to find the highest rate of mortality in the second income quartile. This finding deserves further study. Furthermore, patients who died in the hospital incurred charges significantly greater than the cohort that survived ($137,223 vs. $75,597; p< 0.01). This was likely associated with more costly end-of-life treatment efforts. Patients who died were also more likely to have a shorter LOS (14.1 vs. 10.3 days, p<0.05). Additionally, the finding that rural hospitals are associated with a higher rate of mortality meshes with existing knowledge (Table 4). Rural areas have been reported to have worse levels of health and higher levels of inactivity and obesity.17 The combination of these factors can lead to higher rates of co-morbidities and subsequent higher rates of mortality.
Surgical management
The surgical component of our study described several factors associated with an increased likelihood of surgical management. 39.4% of the hospitalized CCS patient population was managed surgically. Increasing age was associated with decreased surgical prevalence (Table 3). The decreasing surgical trend with increasing age is reasonable given the increasing rates of adverse outcomes noted above.
Anemia deficiency and renal failure were associated with decreased surgical management (Table 3). As would be expected several studies have noted improvement in neurologic function18 and neuropathic pain16 following surgery. Increased surgical rates were noted at medium and large hospitals compared to smaller hospitals (Table 3). The higher rate of surgery at larger hospitals may represent surgical capabilities being available at larger hospitals as compared to smaller hospitals. Initial patient transport to larger hospitals by first responders as well smaller hospitals transferring patients to larger hospitals could also contribute to the higher surgical rates seen.
In an analysis of National Hospital Discharge Survey between 1990 and 1999, Angevine et al. showed patients with cervical disc disease in the south had the highest rates of fusion while those in the northeast had the lowest.19 The present study selects for a unique population and finds the same regional inclination. Higher rates of surgery in the south could be due to a higher distribution of surgeons and the larger population in the South.20 The Southern region, per the U.S Census of 2010, has a population of 114,555,744 as compared to 55,317,240 in the Northeast, 66,927,001 in the Midwest and 71,945,553 in the West. The South is composed of 16 States and the District of Columbia and 37% of the US population is located in this region.
The surgical cohort was also associated with a LOS less than 5 days and an increased prevalence of non-routine discharges (OR: 0.6; CI: 0.5–0.7; p<0.01; OR: 1.3; CI: 1.1–1.5; p<0.01) (Table 3). This is likely rooted in the careful selection of good surgical candidates. Also, the surgical treatment group was associated with increased mean charges ($117,106 vs. 51,260; p<0.01) (Table 2).
Over the study period increased trends of surgery for the management of central cord syndrome were noted (Figure 1). In 2010 more than 2000 patients underwent surgery for central cord syndrome compared to nearly 500 patients having surgery in 2003. This increased trend in surgery for central cord syndrome may be due to studies demonstrating improvement in motor function with surgical decompression in the setting of spinal cord injury. The STASCIS is a recent study that enrolled 313 patients with cervical spinal cord injury, including central cord syndrome, and randomized them into early surgery (<24 hrs) and late surgery (>24 hrs) groups. The early surgical group had significant improvements in ASIA impairment scale as compared to the late group at 6 month follow-up.6 A non-operative cohort was not present in this study but would have been interesting to quantify if there was any neurological improvement in central cord patients management non-operatively. A recent systemic review and expert opinion paper on the surgical management of central syndrome noted that 46% of surgeons would operate on an ASIA D central cord patient and 63% would operate on an ASIA C central cord patient.21 Thus, practice patterns may be changing towards surgery for central cord syndrome and the role of surgery for central cord syndrome is an area of active research.
Figure 1.
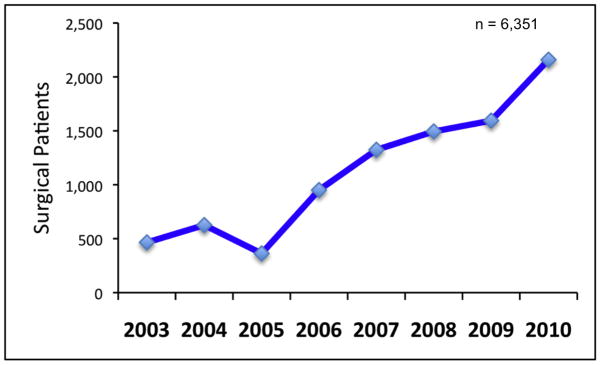
Trends in surgical management of central cord syndrome 2003 to 2010.
Although many studies on central cord syndrome are retrospective studies from single-institutions, our study has several limitations. First, our study was mainly descriptive and we were unable to extrapolate operative rationale. Operative vs. non-operative treatment follow a set of very specific prognostic factors such as ASIA score, signal intensity on MRI showing spinal cord edema and hemorrhage. We also could not analyze patient preferences, which are also crucial in surgical decision-making. Second, we examined a limited number of outcome variables. Though we were able to describe LOS, mortality, and charges, we did not capture a variety of factors regarding quality of life and activities of daily living. We were unable to examine post-discharge events like disease progression or improvement. Third, our study is built on discharge data instead of actual patient records. The discharge as a proxy may lead to overestimation of single-patient hospital visits. Fourth, we did not endeavor to compare different surgical techniques. This area has been examined in the literature without conclusive evidence and is an important area of further research. Prospective randomized trials will be imperative to compare outcomes associated with surgical vs. medical management. Fifth, this study did not examine annual trends in the data. This would be a very useful analysis, especially in the current environment of rapidly increasing costs.
In summary, we used the largest, all-payer database in the nation to extract a population of 16,134 CCS patients and elucidate characteristics associated with fusion/decompression and inpatient mortality. Surgery and mortality are stratified by age, comorbidities, and other variables in order to better understand clinical associations. These relationships may help clinicians to better understand the role of CCS on a national scale. These results are valuable in health-care settings across the United States and will assist clinicians when discussing risks with a diverse set of patients. Lastly our study provided a unique risk assessment perspective.
Footnotes
Author Attribution: David Brodell wrote the first draft of this manuscript. Addisu Mesfin, John Elfar, and Amit Jain approved the content of the final draft. This report has not been previously published in the literature. There was no outside funding for this work.
Conflict of Interest:
David Brodell has no conflicts of interest.
Addisu Mesfin MD, Fellowship Funding from AO Spine.
Contributor Information
David W. Brodell, University of Rochester School of Medicine and Dentistry, Rochester, New York
Amit Jain, Resident in Orthopedics, Johns Hopkins School of Medicine, Baltimore Maryland
John C. Elfar, Assistant Professor, Spinal Surgery Division, University of Rochester School of Medicine and Dentistry, Rochester New York
Addisu Mesfin, Assistant Professor, Spinal Surgery Division, Assistant Professor, Cancer Center, University of Rochester School of Medicine and Dentistry, Rochester, New York
References
- 1.Harrop JS, Sharan A, Ratliff J. Central cord injury: pathophysiology, management, and outcomes. Spine J. 2006;6(6 Suppl):198S–206S. doi: 10.1016/j.spinee.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 2.Ishida Y, Tominaga T. Predictors of neurologic recovery in acute central cervical cord injury with only upper extremity impairment. Spine. 2002;27:1652–7. doi: 10.1097/00007632-200208010-00011. [DOI] [PubMed] [Google Scholar]
- 3.Jimenez O, Marcillo A, Levi AD. A histopathological analysis of the human cervical spinal cord in patients with acute traumatic central cord syndrome. Spinal Cord. 2000;38:532–537. doi: 10.1038/sj.sc.3101052. [DOI] [PubMed] [Google Scholar]
- 4.Nowak DD, Lee JK, Gelb DE, et al. Central cord syndrome. J Am Acad Orthop Surg. 2009;17:756–765. doi: 10.5435/00124635-200912000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Bosch A, Stauffer ES, Nickel VL. Incomplete traumatic quadriplegia: a ten-year review. JAMA. 1971;216:473–8. [PubMed] [Google Scholar]
- 6.Fehlings MG, Vaccaro A, Wilson JR, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS) PLoS ONE. 2012;7:e32037. doi: 10.1371/journal.pone.0032037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lenehan B, Street J, O’Toole P, et al. Central cord syndrome in Ireland: the effect of age on clinical outcome. Eur Spine J. 2009;18:1458–1463. doi: 10.1007/s00586-009-1107-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoshihara H, Yoneoka D. Trends in the treatment for traumatic central cord syndrome without bone injury in the United States from 2000 to 2009. J Trauma Acute Care Surg. 2013 Sep;75(3):453–8. doi: 10.1097/TA.0b013e31829cfd7f. [DOI] [PubMed] [Google Scholar]
- 9.HCUP Nationwide Inpatient Sample (NIS) Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality; Rockville, MD: 2003–2010. www.hcup-us.ahrq.gov/nisoverview.jsp. [PubMed] [Google Scholar]
- 10.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Dvorak MF, Fisher CG, Hoekema J, et al. Factors predicting motor recovery and functional outcome after traumatic central cord syndrome: a long-term follow-up. Spine (Phila Pa 1976) 2005;30:2303–2311. doi: 10.1097/01.brs.0000182304.35949.11. [DOI] [PubMed] [Google Scholar]
- 12.Dai LY. Acute central cervical cord injury: the effect of age upon prognosis. Injury. 2001;32:195–199. doi: 10.1016/s0020-1383(00)00176-5. [DOI] [PubMed] [Google Scholar]
- 13.Newey ML, Sen PK, Fraser RD. The long-term outcome after central cord syndrome: a study of the natural history. J Bone Joint Surg Br. 2000;82:851–855. doi: 10.1302/0301-620x.82b6.9866. [DOI] [PubMed] [Google Scholar]
- 14.Tow AM, Kong KH. Central cord syndrome: functional out- come after rehabilitation. Spinal Cord. 1998;36:156–160. doi: 10.1038/sj.sc.3100618. [DOI] [PubMed] [Google Scholar]
- 15.Penrod LE, Hegde SK, Ditunno JF., Jr Age effect on prognosis for functional recovery in acute, traumatic central cord syndrome. Arch Phys Med Rehabil. 1990;71:963–968. [PubMed] [Google Scholar]
- 16.Aito S, D’Andrea M, Werhagen L, et al. Neurological and functional outcome in traumatic central cord syndrome. Spinal Cord. 2007;45:292–297. doi: 10.1038/sj.sc.3101944. [DOI] [PubMed] [Google Scholar]
- 17.Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the United States: findings from NHANES (2005–2008) J Rural Health. 2012 Fall;28(4):392–7. doi: 10.1111/j.1748-0361.2012.00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen L, Yang H, Yang T, et al. Effectiveness of surgical treatment for tramatic central cord syndrome. J Neurosurg Spine. 2009;10(1):3–8. doi: 10.3171/2008.9.SPI0822. [DOI] [PubMed] [Google Scholar]
- 19.Angevine PD, Arons RR, McCormick PC. National and regional rates and variation of cervical discectomy with and without anterior fusion, 1990–1999. Spine (Phila Pa 1976) 2003;28:931–40. doi: 10.1097/01.BRS.0000058880.89444.A9. [DOI] [PubMed] [Google Scholar]
- 20. [Last accessed June 12th, 2014]; http://www.census.gov/popest/about/geo/terms.html.
- 21.Lenehan B, Fisher CG, Vaccaro A, Fehlings M, Aarabi B, Dvorak MF. The urgency of central cord decompression in acute central cord syndromes with spondylosis and without instability. Spine. 2010;21S:S180–S186. doi: 10.1097/BRS.0b013e3181f32a44. [DOI] [PubMed] [Google Scholar]


