Abstract
Purpose/Objectives
The aims of this study were to (1) Identify the predictors of symptoms of anxiety, and (2) Evaluate the differential association of somatic and non-somatic symptoms of depression on anxiety over time in persons with multiple sclerosis (MS).
Methods/Design
Participants were 513 persons with MS who previously enrolled in a study exploring the experience of living with MS and completed a 4-month follow-up survey. The main outcome measure used was the Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Demographic, disease-associated variables (time since onset of MS, EDSS, pain and fatigue), and time 1 psychological variables (somatic and non-somatic symptoms of depression) were entered into a hierarchical regression model to examine predictors at baseline for anxiety symptoms at time 2.
Results
Of the 513 participants in this study a large portion of the sample was white (92%), female (82%), and had relapsing-remitting MS (57%). After adjusting for demographic and disease related variables, anxiety (β <.001), employment (β =.07) and non-somatic depressive symptoms (β =.10) at baseline significantly predicted anxiety at time 2, ps<.05. Interactions revealed significant effects for time since onset of MS and somatic symptoms as well as time since onset and non-somatic symptoms, ps<.05. Non-somatic symptoms were more linked to anxiety early in the disease and somatic symptoms were more prominently linked to anxiety later in the disease.
Conclusions
Findings suggest that non-somatic symptoms of depression and employment predict anxiety in MS. The relationship between different aspects of depression and anxiety may change over the course of the disease.
Keywords: Multiple Sclerosis, Anxiety, Depression
Multiple sclerosis (MS) is a chronic neurologic condition that impacts as many as 2.3 million individuals worldwide (“Atlas of MS Database,” 2013). The disease course and symptom profile varies significantly between individuals and usually progressively worsens over time. Typically, patients experience multiple symptoms resulting in physical, cognitive and psychological difficulties. Although a wealth of research has focused on depression and its treatments in MS, little is known about symptoms of anxiety and risk factors for its development in MS. Hence, currently there exists no unified theoretical conceptualization of the experience of anxiety in MS and how that may change over time. This is a surprising gap in the literature, especially given that prevalence of anxiety disorders in MS ranges from 14% to 45% (Korostil & Feinstein, 2007; Wood et al., 2013) and may result in poorer medication adherence (Turner, Williams, Sloan, & Haselkorn, 2009), higher pain intensity and pain interference with health- related quality of life (Bruce & Arnett, 2009; Kalia & O’Connor, 2005), lower quality of life (Garfield & Lincoln, 2012), and suicidal intent (Korostil & Feinstein, 2007).
Identification of risk factors for anxiety in MS would lay a critical foundation for developing an advanced conceptualization of the experience of anxiety in MS over time. This holds tremendous practical implications in that such a theoretical advancement would enhance clinical efforts directed towards the prevention, screening, and treatment of anxiety and concomitant secondary symptoms. In the absence of prior risk factor research for anxiety in MS, it is informative to consider if the cross-sectional variables associated with anxiety in MS may also be predictive of symptoms over time. Higher anxiety has been associated with female gender (Jones et al., 2012), younger age (Wood et al., 2013), a diagnosis of relapsing-remitting MS (Jones et al., 2012), longer time since onset of MS (though results are mixed; Feinstein, O’Connor, Gray, & Feinstein, 1999; Janssens et al., 2006), greater MS-related disability (Jones et al., 2012), higher levels of fatigue (Beiske et al., 2008), MS exacerbations (rapid onset or an increase in symptoms; Burns, Nawacki, Siddique, Pelletier, & Mohr, 2013; Feinstein et al., 1999), and depression (Garfield & Lincoln, 2012; Wood et al., 2013). Investigation is needed to identify if these cross-sectional correlates may represent predictive risk factors that have an extended impact on the development, maintenance, or exacerbation of anxiety symptoms over time.
A challenge for identifying risk factors of anxiety is the high comorbidity between anxiety and depression (Almeida et al., 2012; Burns, Siddique, Fokuo, & Mohr, 2010). Evidence suggests that individuals with a history of depression may be at a higher risk of experiencing anxiety over time (Korostil & Feinstein, 2007). A further challenge is that anxiety, depression, and MS include overlapping somatic symptoms (e.g., sleep disturbance, fatigue, concentration difficulties). Similarly, reports of ‘numbness and tingling,’ ‘feeling unsteady,’ and ‘wobbliness in legs’ might be attributed to anxiousness or the MS disease process (Feinstein et al., 1999). A number of studies have discussed the importance of removing somatic symptoms from both depression and anxiety scales to avoid this confound (Benedict, Fishman, McClellan, Bakshi, & Weinstock-Guttman, 2003; Donnchadha et al., 2013). Recommendations include utilizing an outcome measure comprised only of non-somatic items (i.e., excessive worry, fear of losing control, unable to relax, etc.) of anxiety (Donnchadha et al., 2013; Zigmond & Snaith, 1983) or utilizing a two-factor model of somatic vs. non-somatic depression symptoms (Richardson & Richards, 2008).
The present study sought to extend the literature on anxiety in MS by conducting a evaluation of current demographic, disease-related characteristics and psychological factors that contribute to anxiety symptom severity at a 4-month follow-up. In the absence of prior longitudinal research on anxiety among the MS population, we hypothesized that variables cross-sectionally associated with anxiety would also remain predictors during 4-month follow-up: age, level of disability, time since onset, and depression. To account for the concerns of somatic overlap, we utilized an anxiety measure that focuses on cognitions (and excludes somatic items), and a two-factor measure of depression that differentiates somatic and non-somatic symptoms. We hypothesized that the non-somatic depression symptoms would be associated with anxiety symptom severity due to the substantial overlap between the affective/cognitive symptoms of anxiety and depression derived from the shared distress and negative affect (Kendler et al., 1995; Watson & Clark, 1984; Watson, Clark, & Carey, 1988). Finally, since there is considerable reason to believe that both depression and anxiety may be influenced by age (Janssens et al., 2006; Jones et al., 2012; Mattioli, Bellomi, Stampatori, Parrinello, & Capra, 2011; Williams et al., 2005; Wood et al., 2013), time since onset (Chwastiak et al., 2002; Forman & Lincoln, 2010; Janssens et al., 2006; Korostil & Feinstein, 2007; Williams et al., 2005), and disability (Beiske et al., 2008; Mattioli et al., 2011; Moore et al., 2012), we explored the potential synergistic (i.e., interaction) effect between depression and age, time since onset, and disability on anxiety over time to determine if a differential pattern of association would emerge between these factors.
Methods
Recruitment and Procedures
Participants were individuals enrolled in a large study examining the experience of living with MS who completed a series of self-report questionnaires (described below). The data for the present analysis represent two time points, 4-months apart. Detailed information on recruitment is reported elsewhere (Amtmann et al., 2012). Briefly, participants were recruited from the Greater Northwest chapter of the National Multiple Sclerosis Society. Of the 1,628 who were mailed invitations, 1,367 met eligibility criteria (age 18 years or older with self-reported MS) and were mailed a paper survey or a link to the online survey. Of the 1,270 individuals who completed this baseline assessment, 562 randomly selected participants were invited to continue participating in the survey. A total of 513 individuals (93% response rate) completed the four-month follow-up survey either online (n=119) or on paper (n=394). All participants provided informed consent and received $25 per completed survey. Procedures were approved by the Human Subjects Division of the primary research institution.
Measures
Demographics
Participants provided demographic and basic medical information, including age, sex, race/ethnicity, education, employment, and time since onset of MS.
Disability Status
Participants completed the self-reported Expanded Disability Status Scale Mobility (EDSS-Mobility; (Bowen, Gibbons, Gianas, & Kraft, 2001). A continuous score (range 1–9) was used for all analyses. For descriptive purposes, participants were divided into three categories: no mobility aid (≤ 4, minimal severity), bilateral or unilateral mobility aid (4.5–6.5, intermediate severity), and use of a wheelchair for mobility (≥ 7, advanced severity).
Pain
The Numeric Rating Scale (NRS) assessed pain severity, with participants rating the intensity of their pain over the past week from 0 (no pain) to 10 (highest pain imaginable). This single item NRS is widely utilized and is well validated (Jensen & Karoly, 2011).
Fatigue
The Fatigue Severity Scale (FSS) was utilized to measure the severity and impact of fatigue. The FSS includes nine items ranging from 1 (no symptoms) to 7 (severe fatigue), with higher scores indicating greater levels of fatigue. The FSS has high sensitivity and good internal consistency (Cronbach’s α = .88; Krupp, LaRocca, Muir-Nash, & Steinberg, 1989).
Anxiety
The Hospital Anxiety and Depression Scale-Anxiety (HADS-A) is a 7-item measure of anxiety symptom severity. Items are rated on a 4-point Likert scale, with higher scores indicating greater anxiety symptoms (Zigmond & Snaith, 1983). The HADS-A has been validated for use in identifying anxiety in individuals with MS (Honarmand & Feinstein, 2009).
Depression
The Patient Health Questionnaire – 9-item (PHQ-9) is a measure of depression symptom severity developed in parallel with the diagnosis of Major Depressive Disorder in the DSM-IV (Spitzer, Kroenke, & Williams, 1999). Items are rated according to how persistent the symptom has been in the past two weeks: 0 (not at all), 1 (several days), 2 (more than half the days), or 3 (nearly every day). The PHQ-9 demonstrates good internal consistency (Cronbach’s α = .89) and test-retest reliability (r =. 84; Kroenke, Spitzer, & Williams, 2001).
A two-factor structure consisting of non-somatic and somatic items was used to comprise the two-dimensional construct (Richardson & Richards, 2008). Reliability analysis confirmed that the two constructs had sufficient internal consistency (Cronbach’s α = .81 for non-somatic scale and Cronbach’s α = .74 for somatic scale). Since the two subscales indicated acceptable reliability (Cronbach’s α of .70 or higher cutoff; Nunnally, 1978) we used the composite scores to form the two-dimensional scales in the current study.
Data Analytic Strategy
Statistical assumptions of the data were examined, including evaluation of descriptive statistics and histograms to assess normality and linearity. Collinearity diagnostics were conducted to help identify multicollinearity among predictors. A correlation matrix of all predictor variables are included in Table 1. Correlations among the variables were examined and Tolerance values and Variance Inflation Factor (VIF=1/T) were used to measure the impact of collinearity in the regression model. All Tolerance and VIF values were within an acceptable range (acceptable range: 0.2<T<2 and VIF < 10; (Belsley, Kuh, & Welsch, 2005). All predictors for the interaction were centered to reduce nonessential multicollinearity. Centered predictor variables were used for linear by linear interaction (Aiken & West, 1991).
Table 1.
Correlation coefficients, means and SD for study variables
| Anxiety | Non-Somatic Symptoms | Somatic Symptoms | Time since onset | EDSS | Age | Fatigue | Pain | Employment | M | SD | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Anxiety at Time 1 | - | 5.58 | 3.95 | ||||||||
| 2. Non-Somatic Sx of Depression | .541*** | - | 2.39 | 2.58 | |||||||
| 3. Somatic Sx of Depression | .519*** | .639*** | - | 4.98 | 3.40 | ||||||
| 4. Time since onset of MS | −.142*** | −.035 | −.078 | - | 13.45 | 9.77 | |||||
| 5. EDSS | .019 | .206*** | .235*** | .379*** | - | 4.18 | 2.81 | ||||
| 6. Age | −.178*** | −.053 | −.059 | .522*** | .354*** | - | 51.41 | 10.98 | |||
| 7. Fatigue | .250*** | .393*** | .523*** | .063 | .425*** | .130** | - | 5.14 | 1.47 | ||
| 8. Pain | .326*** | .377*** | .540*** | −.010 | .177*** | −.010 | .354*** | - | 2.83 | 2.73 | |
| 9. Employment | .015 | −.138*** | −.147*** | −.376*** | −.494*** | −.386*** | −.309*** | −.131** | - | 0.40 | 0.49 |
Note. Total Depression score measured by Patient Health Questionnaire-9 (PHQ-9) Mean= 7.38 and SD=5.42. Anxiety measured by the Hospital Anxiety and Depression Scale-Anxiety (HADS-A) with scores Range (0–20). Abbreviations: EDSS, Expanded Disability Status Scale Mobility
p < .05;
p < .01;
p < .001.
A hierarchical regression analysis was used to test the study hypotheses, with the model including time 1 variables as predictors and the time 2 variable (anxiety, at time 2) as the outcome. The model tested whether the participant’s “current” subset of biopsychosocial variables (time 1), predicted anxiety four months later (time 2). The predictors represented the “current” (time 1) set of variables for the participant. The first step included anxiety (time 1) to identify the extent to which current anxiety predicted future anxiety. Including anxiety at time 1 also allowed for identifying whether the step 2 variables contributed to the severity of anxiety at time 2 beyond what could be attributed to anxiety at time 1. The step 2 variables entered into the regression model included a selection of important biopsychosocial factors: demographic variables (age, sex, race, education, employment), disease-related characteristics (time since onset, disability, pain, fatigue) and psychological variables (somatic and non-somatic symptoms of depression). The third step in the specified regression model tested for interaction effects and determined how these interaction effects may predict worsening of anxiety symptoms. In step 3, the following a priori selected interaction terms were entered: age X somatic symptoms, age X non-somatic symptoms, time since MS onset X somatic symptoms, time since MS onset X non-somatic symptoms, disability X somatic symptoms, and disability X non-somatic symptoms.
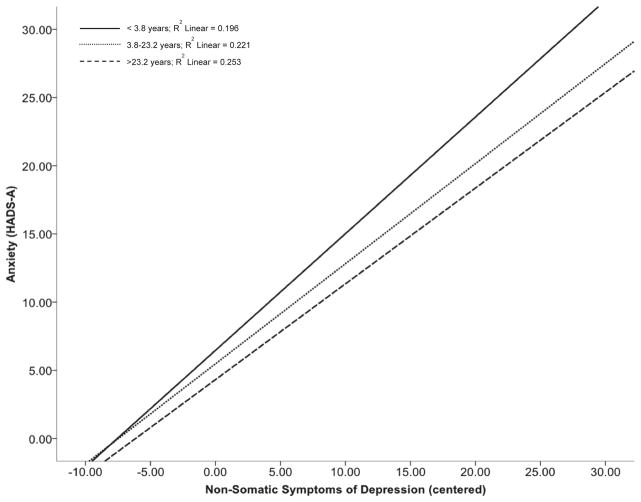
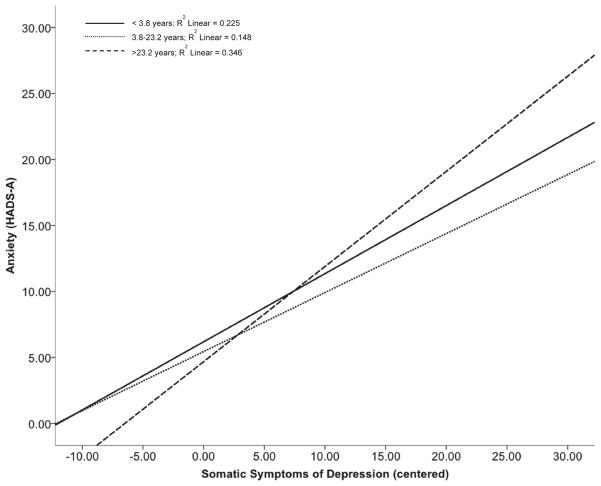
For graphical representations of the significant interaction effects for time since onset of MS and somatic or non-somatic symptoms of depression on anxiety, groups were created reflecting three different categories of time since onset of disease (Aiken & West, 1991): (1) < −1 standard deviation (SD; <3.8 years) below the mean; (2) between −1 SD (>3.8 years) and +1 SD (<23.2 years); and (3) > +1 SD (> 23.2 years) above the mean. All statistical analyses were conducted using the Statistical Package for the Social Sciences (SPSS), 20th edition.
Results
Sample Characteristics
Participants were 513 individuals with a self-reported diagnosis of MS. Consistent with the MS population at large (“Atlas of MS Database,” 2013) the sample was predominantly non-Hispanic white (92%) and female (82%). The average participant was 51 years old with mean time since onset of MS of 13.5 years (SD = 9.77; range=1–60). Relapsing-remitting MS was most common (57%) followed by secondary-progressive, primary-progressive, and progressive-relapsing MS (see Table 2).
Table 2.
Participant characteristics
| N (%) | |
|---|---|
| Total sample | 513 |
| Sex | |
| Male | 93 (18.2) |
| Female | 417 (81.8) |
| Ethnicity | |
| Non-Hispanic white | 468 (91.8) |
| Other ethnicity | 42 (8.2) |
| Education | |
| ≤ High School | 115 (22.5) |
| College and above | 392 (76.9) |
| Employment | |
| Yes | 306 (60) |
| No | 201 (39.4) |
| MS Type | |
| Relapsing-remitting | 284 (55.7) |
| Secondary-progressive | 103 (20.2) |
| Primary-progressive | 64 (12.5) |
| Progressive-relapsing | 49 (9.6) |
| Not known | 10 (2.0) |
| EDSS | |
| ≤ 4.0 | 169 (32.9) |
| 4.5–6.5 | 247 (48.1) |
| ≥7.0 | 97 (18.9)
|
|
M (SD)
|
|
| Age | 51.4 (10.9)
|
| Time since onset of MS | 13.5 (9.8) |
Note. Participant characteristic of the entire sample. Values Are expressed as mean (SD) for continues variables and total N (%) for all categorical variables. Abbreviations: EDSS, Expanded Disability Status Scale Mobility
Risk Factors for Anxiety Symptom Severity
The multiple regression analysis assessing the relationship of risk factors with anxiety indicated that the predictors accounted for 63% variance in the final model (R2 = .63, F(18, 459) = 42.58, p<.001; see Table 3 for all model parameters). As expected, there was a significant main effect for anxiety at time 1 (β=.70, p<.001) such that greater anxiety at time 1 was associated with greater anxiety at time 2. There were no significant main effects for age, time since MS onset, and EDSS; however, results indicated that employment status at time 1 significantly predicted anxiety symptoms at time 2, with participants who were employed reporting higher anxiety (β =.07, p=.03). Non-somatic symptoms of depression also significantly predicted anxiety (β =.10, p=.02); greater levels of non-somatic depressive symptoms at time 1 were associated with greater anxiety at time 2. There were no other significant main effects in the model.
Table 3.
Regression coefficients
| B | SE B | β | p | |
|---|---|---|---|---|
| Block 1 | ||||
| Anxiety at time 1 | .71 | .04 | .70 | <.001 |
| Block 2 | ||||
| Age | .01 | .01 | .03 | .47 |
| Race | .34 | .42 | .02 | .42 |
| Sex | .47 | .31 | .04 | .14 |
| Employment | .60 | .28 | .07 | .03 |
| Education | .09 | .28 | .07 | .75 |
| Pain | .09 | .05 | .06 | .09 |
| Fatigue | .06 | .10 | .02 | .57 |
| Time since onset | −.003 | .01 | −.01 | .86 |
| EDSS | −.07 | .05 | −.05 | .17 |
| Depression- Somatic | .001 | .05 | .001 | .99 |
| Depression- Non-somatic | .16 | .06 | .10 | .01 |
| Block 3 | ||||
| Age x Depression-Somatic | −.001 | .01 | −.01 | .92 |
| Age x Depression-Non-somatic | <.001 | .01 | .001 | .99 |
| EDSS x Depression-Somatic | −.02 | .02 | −.04 | .27 |
| EDSS x Depression-Non-somatic | −.01 | .02 | −.02 | .70 |
| Time since onset x Depression-Somatic | .01 | .01 | .10 | .02 |
| Time since onset x Depression-Non-somatic | −.02 | .01 | −.10 | .03 |
Note. N=478. Abbreviation: EDSS, Expanded Disability Status Scale Mobility. All coefficients presented in table are from the final model (model 3).
Analysis revealed significant interaction effects for time since onset of MS and non-somatic depressive symptoms (β =−.10, p=.03; see Figure 1). Participants with the shortest time since onset of MS experienced significantly more anxiety with more non-somatic depressive symptoms (see Figure 1). An interaction effect was also found with time since MS onset and somatic symptoms of depression (β =.10, p=.02; see Figure 2). Participants with the longest time since onset experienced significantly more anxiety with more somatic depressive symptoms (see Figure 2).
Figure 1.
Effects of time since onset of MS and non-somatic symptoms of depression on Anxiety overtime. Figure presented are based on the final model (model 3).
Figure 2.
Effects of time since onset of MS and somatic symptoms of depression on Anxiety overtime. Figure presented are based on the final model (model 3).
Discussion
This study identified several risk factors for anxiety symptoms in MS at a short-term follow-up. Results partially supported our hypothesis, such that non-somatic symptoms of depression (time 1) were associated with higher levels of anxiety symptoms (time 2). Additionally, employment status unexpectedly emerged as a significant predictor of anxiety symptoms. Surprisingly, many variables cross-sectionally associated with anxiety in the literature were not associated with worsening anxiety symptoms when examined during the short-term follow-up. Exploratory analyses revealed two important interaction effects. Specifically, results indicated that in the early stages after a MS diagnosis, individuals experience greater severity of non-somatic symptoms of depression and this appears to exert a negative, synergistic effect that leads to worsening anxiety. However, over time (i.e., as time since MS diagnosis increases), there is a shift in reported coping associated with MS such that the somatic symptoms of depression emerge as more predominant, and this corresponds with heightened risk for anxiety symptoms.
The premise of the present study was the identification of variables at one time point that signal risk for anxiety symptoms worsening by a second time point, so future research could focus on developing clinical assessments and treatments focused on intervening early with at risk patients. As expected, the individual’s level of anxiety (time 1) was a significant predictor of anxiety at the second time point (Janssens et al., 2006). However, beyond initial level of anxiety, the individual’s current non-somatic symptoms of depression and employment status were also risk factors for higher anxiety symptom severity at 4-month follow-up. These findings serve an important purpose from a clinical assessment perspective: while the presence of anxiety might be an obvious reason to be concerned about future anxiety, clinicians might also pay attention to the presence of non-somatic depressive symptoms and employment status.
The current findings are only a first step towards clinical interventions; important future research is needed to understand why these risk factors are important. For example, one might consider whether the impact of non-somatic symptoms of depression on anxiety symptoms is due to a shared mechanism and/or the exacerbating effects of having anxiety and depression simultaneously. Similarly, we cannot determine why employment is impactful from these findings. However, we might speculate the involvement of several factors: practical concerns (e.g., finances), emotional concerns (e.g., feeling overwhelmed with demands at work in the context of worsening MS symptoms), and/or social concerns (e.g., the human interaction that is built in to many workplaces; Busche, Fisk, Murray, & Metz, 2003; Jellie, Sweetland, Riazi, Cano, & Playford, 2014). By understanding why these variables are important, intervention research can then focus on the value of intervening on specific factors that impact anxiety and, more importantly, on early intervention on these factors in an effort to decrease the presence and severity of anxiety symptoms.
We were equally intrigued that there were no significant findings for the predictive nature of biomedical variables to anxiety symptom severity. The examined relationships of MS disease course, time since diagnosis (Feinstein et al., 1999; Forman & Lincoln, 2010; Janssens et al., 2006; Korostil & Feinstein, 2007), and MS symptoms (Kalia & O’Connor, 2005) to anxiety symptom severity were all non-significant. Perhaps the most probable explanation for these unexpected findings are (a) while the nature of MS (e.g., uncertainty and uncontrollability; Janssens et al., 2003; Kroencke, Denney, & Lynch, 2001) may contribute to anxiety, it may not impact variability in anxiety symptom severity over time; and/or (b) disease-related factors did not change significantly in the span of the study hence their capacity to influence anxiety over time may have been methodologically limited. More research is needed to understand the contribution of MS-specific variables to anxiety.
In our close examination of the relationship of depression with anxiety symptoms, we found a significant relationship of non-somatic symptoms of depression with symptoms of anxiety. The association of non-somatic symptoms suggests a shared cognitive and affective overlap, whereby a person with more depressive cognitions may be at greater risk for also having more anxious cognitions. This was particularly notable in participants with a more recent diagnosis of MS, such that participants with the shortest time since onset of MS experienced significantly more anxiety with more non-somatic depressive symptoms. The association of non-somatic depressive and anxious symptoms should be a focus for future research, as it carries important clinical implications. Specifically, it may be important clinically to determine if these are the same cognitions observed through different lenses (i.e., a single cognition that at times is observed as depressive, but at other times is observed as anxious) or whether these are unique cognitions but these individuals are more predisposed to maladaptive thought patterns. Having a shared cognition manifesting differently over time would suggest the importance of developing trans-diagnostic interventions targeting those shared cognitions, rather than intervening on “anxiety” or “depression.” Findings indicate the relationship between symptoms of depression and anxiety may change over the MS disease course in another way: Individuals seem to report a stronger link between somatic symptoms of depression with symptoms of anxiety later in the disease. Possibly, somatically experienced depression symptoms contribute to the symptoms of anxiety associated with the overall burden of MS, and as the disease burden increases over time, so does the importance of these symptoms. Overall these findings highlight how the correlation between depression and anxiety may change over time such that early in the disease process they are linked by cognitive appraisal, and late in the disease they are linked by somatic experiences. This has interesting clinical implications, as psychologists treating people with MS can expect that at first individuals will be worried and sad as they grapple with the uncertainty of what might happen to them. Later in the disease they are worried and sad as they come to terms with what is happening to them. This process is less a function of maturity (age) or actual disability (EDSS) as it is the amount of time the person has had to live with the disease.
Study Limitations
We acknowledge several limitations to the present study. First, the sample includes individuals with MS who voluntarily participated in a broad study of life with MS. Results may be subject to selection and response bias and may not generalize to other populations of individuals with MS. The favorable response rate (92.9%) and large sample size (N = 513) partially mitigates these concerns. Additionally, the complex relationship that may exist between age and time since onset of MS requires a systematic and comprehensive analysis to determine whether one or both of these variables may add unique variance to the prediction of anxiety symptoms. While our findings do support some association between the interaction of time since MS onset, depression and anxiety, this relationship cannot be uniquely parceled out from the effect of aging. Finally, it is important to consider that this study describes anxiety symptom severity, but not anxiety disorders, as the HADS-A is not a diagnostic measure. An exploration of risk factors for anxiety disorders, as well as differences between types of anxiety disorders, is worthy of future research.
CONCLUSIONS
The present study provides important, novel information on predictors of anxiety in individuals with MS. Whereas previous research identified variables that are associated with anxiety cross-sectionally, the present study identified variables that may signal a heightened risk of worsening anxiety symptoms over time. These identified risk factors serve an important clinical purpose, highlighting areas that are worth extra scrutiny, much as how certain laboratory values or blood pressure might indicate increased scrutiny for certain medical conditions (Almeida et al., 2012). Finally, this study serves as a starting point for future research on interventions for anxiety in MS. In particular, research is needed to better understand why the present variables are important and how intervening on these variables could alter an individual’s prognosis regarding future anxiety and coping with MS over time.
Impact.
The present study extends beyond existing cross-sectional research by identifying predictors associated with heightened risk of anxiety symptoms in MS.
Although future research is needed to confirm these findings, this study preliminarily identified three risk factors (anxiety symptoms, depression symptoms and employment status) that may be highly associated with worsening anxiety symptoms in individuals with MS.
This study also highlights how the correlation between depression and anxiety may change over time such that early in the disease process they are linked by cognitive appraisal, and late in the disease they are linked by somatic experiences.
Acknowledgments
Acknowledgment of financial support, including grant numbers:
The contents of this article were developed under grants from the Department of Education, NIDRR grant numbers H133B031129 & H133B080025. However, these contents do not necessarily represent the policy of the Department of Education, and you should not assume endorsement by the Federal Government. In addition, the work reported in this manuscript was supported by a grant from the National Institutes of Health through the NIH Roadmap for Medical Research, Grant 5U01AR052171-03 to University of Washington, Amtmann (PI), and by grants from the National Multiple Sclerosis Society Grant MB 0008 (Dawn Ehde, PI) and MB0026 (Aaron Turner, PI).
Footnotes
Acknowledgment of any presentation of this material:
Presented in part at the 16th Annual Rehabilitation Psychology Conference 2014, San Antonio, Texas on March 1, 2014.
Reprints:
Reprints are not available from the author.
Explanation of any conflicts of interest:
We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated. We certify that all financial and material support for this research and work are clearly identified in the title page of the manuscript. (Narineh Hartoonian, Ph.D., M.S., Alexandra L. Terrill, Ph.D., Meghan L. Beier, Ph.D., Aaron P. Turner, Ph.D. & Kevin N. Alschuler, Ph.D.).
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; 1991. [Google Scholar]
- Almeida OP, Draper B, Pirkis J, Snowdon J, Lautenschlager NT, Byrne G, Pfaff JJ. Anxiety, depression, and comorbid anxiety and depression: risk factors and outcome over two years. Int Psychogeriatr. 2012;24(10):1622–1632. doi: 10.1017/S104161021200107X. [DOI] [PubMed] [Google Scholar]
- Amtmann D, Bamer AM, Noonan V, Lang N, Kim J, Cook KF. Comparison of the psychometric properties of two fatigue scales in multiple sclerosis. Rehabil Psychol. 2012;57(2):159–166. doi: 10.1037/a0027890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atlas of MS Database. 2013 Retrieved October 28, 2013, from http://www.atlasofms.org/index.aspx.
- Beiske AG, Svensson E, Sandanger I, Czujko B, Pedersen ED, Aarseth JH, Myhr KM. Depression and anxiety amongst multiple sclerosis patients. Eur J Neurol. 2008;15(3):239–245. doi: 10.1111/j.1468-1331.2007.02041.x. [DOI] [PubMed] [Google Scholar]
- Belsley DA, Kuh E, Welsch RE. Regression diagnostics: Identifying influential data and sources of collinearity. Vol. 571. John Wiley & Sons; 2005. [Google Scholar]
- Benedict RH, Fishman I, McClellan MM, Bakshi R, Weinstock-Guttman B. Validity of the Beck Depression Inventory-Fast Screen in multiple sclerosis. Mult Scler. 2003;9(4):393–396. doi: 10.1191/1352458503ms902oa. [DOI] [PubMed] [Google Scholar]
- Bowen J, Gibbons L, Gianas A, Kraft GH. Self-administered Expanded Disability Status Scale with functional system scores correlates well with a physician-administered test. Mult Scler. 2001;7(3):201–206. doi: 10.1177/135245850100700311. [DOI] [PubMed] [Google Scholar]
- Bruce JM, Arnett P. Clinical correlates of generalized worry in multiple sclerosis. J Clin Exp Neuropsychol. 2009;31(6):698–705. doi: 10.1080/13803390802484789. [DOI] [PubMed] [Google Scholar]
- Burns MN, Nawacki E, Siddique J, Pelletier D, Mohr DC. Prospective Examination of Anxiety and Depression Before and During Confirmed and Pseudoexacerbations in Patients With Multiple Sclerosis. Psychosomatic Medicine. 2013;75(1):76–82. doi: 10.1097/PSY.0b013e3182757b2b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns MN, Siddique J, Fokuo JK, Mohr DC. Comorbid anxiety disorders and treatment of depression in people with multiple sclerosis. Rehabil Psychol. 2010;55(3):255–262. doi: 10.1037/a0020492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busche KD, Fisk JD, Murray TJ, Metz LM. Short term predictors of unemployment in multiple sclerosis patients. Can J Neurol Sci. 2003;30(2):137–142. doi: 10.1017/s0317167100053403. [DOI] [PubMed] [Google Scholar]
- Chwastiak L, Ehde DM, Gibbons LE, Sullivan M, Bowen JD, Kraft GH. Depressive symptoms and severity of illness in multiple sclerosis: epidemiologic study of a large community sample. Am J Psychiatry. 2002;159(11):1862–1868. doi: 10.1176/appi.ajp.159.11.1862. [DOI] [PubMed] [Google Scholar]
- Donnchadha SO, Burke T, Bramham J, O’Brien MC, Whelan R, Reilly R, Tubridy N. Symptom overlap in anxiety and multiple sclerosis. Mult Scler. 2013;0(0):1–6. doi: 10.1177/1352458513476742. [DOI] [PubMed] [Google Scholar]
- Feinstein A, O’Connor P, Gray T, Feinstein K. The effects of anxiety on psychiatric morbidity in patients with multiple sclerosis. Mult Scler. 1999;5(5):323–326. doi: 10.1177/135245859900500504. [DOI] [PubMed] [Google Scholar]
- Forman AC, Lincoln NB. Evaluation of an adjustment group for people with multiple sclerosis: a pilot randomized controlled trial. Clin Rehabil. 2010;24(3):211–221. doi: 10.1177/0269215509343492. [DOI] [PubMed] [Google Scholar]
- Garfield AC, Lincoln NB. Factors affecting anxiety in multiple sclerosis. Disabil Rehabil. 2012;34(24):2047–2052. doi: 10.3109/09638288.2012.667503. [DOI] [PubMed] [Google Scholar]
- Honarmand K, Feinstein A. Validation of the Hospital Anxiety and Depression Scale for use with multiple sclerosis patients. Multiple Sclerosis. 2009;15(12):1518–1524. doi: 10.1177/1352458509347150. [DOI] [PubMed] [Google Scholar]
- Janssens AC, Buljevac D, van Doorn PA, van der Meche FG, Polman CH, Passchier J, Hintzen RQ. Prediction of anxiety and distress following diagnosis of multiple sclerosis: a two-year longitudinal study. Mult Scler. 2006;12(6):794–801. doi: 10.1177/1352458506070935. [DOI] [PubMed] [Google Scholar]
- Janssens AC, van Doorn PA, de Boer JB, van der Meche FG, Passchier J, Hintzen RQ. Impact of recently diagnosed multiple sclerosis on quality of life, anxiety, depression and distress of patients and partners. Acta Neurol Scand. 2003;108(6):389–395. doi: 10.1034/j.1600-0404.2003.00166.x. [DOI] [PubMed] [Google Scholar]
- Jellie B, Sweetland J, Riazi A, Cano SJ, Playford ED. Staying at work and living with MS: a qualitative study of the impact of a vocational rehabilitation intervention. Disabil Rehabil. 2014 doi: 10.3109/09638288.2013.854842. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk DC, Melzack R, editors. Handbook of Pain Assessment. 3. Guildford Press; 2011. pp. 19–44. [Google Scholar]
- Jones KH, Ford DV, Jones PA, John A, Middleton RM, Lockhart-Jones H, Noble JG. PLoS One. Vol. 7. United States: 2012. A Large-Scale Study of Anxiety and Depression in People with Multiple Sclerosis: A Survey via the Web Portal of the UK MS Register; p. e41910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalia LV, O’Connor PW. Severity of chronic pain and its relationship to quality of life in multiple sclerosis. Mult Scler. 2005;11(3):322–327. doi: 10.1191/1352458505ms1168oa. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Walters EE, Neale MC, Kessler RC, Heath AC, Eaves LJ. The structure of the genetic and environmental risk factors for six major psychiatric disorders in women. Phobia, generalized anxiety disorder, panic disorder, bulimia, major depression, and alcoholism. Arch Gen Psychiatry. 1995;52(5):374–383. doi: 10.1001/archpsyc.1995.03950170048007. [DOI] [PubMed] [Google Scholar]
- Korostil M, Feinstein A. Anxiety disorders and their clinical correlates in multiple sclerosis patients. Mult Scler. 2007;13(1):67–72. doi: 10.1177/1352458506071161. [DOI] [PubMed] [Google Scholar]
- Kroencke DC, Denney DR, Lynch SG. Depression during exacerbations in multiple sclerosis: the importance of uncertainty. Mult Scler. 2001;7(4):237–242. doi: 10.1177/135245850100700405. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of general internal medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46(10):1121–1123. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- Mattioli F, Bellomi F, Stampatori C, Parrinello G, Capra R. Depression, disability and cognitive impairment in multiple sclerosis: a cross sectional Italian study. Neurol Sci. 2011;32(5):825–832. doi: 10.1007/s10072-011-0624-2. [DOI] [PubMed] [Google Scholar]
- Moore P, Hirst C, Harding KE, Clarkson H, Pickersgill TP, Robertson NP. Multiple sclerosis relapses and depression. J Psychosom Res. 2012;73(4):272–276. doi: 10.1016/j.jpsychores.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Nunnally JC. Psychometric theory. NY: McGraw-Hill; 1978. [Google Scholar]
- Richardson EJ, Richards JS. Factor structure of the PHQ-9 screen for depression across time since injury among persons with spinal cord injury. Rehabil Psychol. 2008;53(2):243. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. Jama. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Turner AP, Williams RM, Sloan AP, Haselkorn JK. Injection anxiety remains a long-term barrier to medication adherence in multiple sclerosis. Rehabil Psychol. 2009;54(1):116–121. doi: 10.1037/a0014460. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Negative affectivity: the disposition to experience aversive emotional states. Psychol Bull. 1984;96(3):465–490. [PubMed] [Google Scholar]
- Watson D, Clark LA, Carey G. Positive and negative affectivity and their relation to anxiety and depressive disorders. J Abnorm Psychol. 1988;97(3):346–353. doi: 10.1037//0021-843x.97.3.346. [DOI] [PubMed] [Google Scholar]
- Williams RM, Turner AP, Hatzakis M, Jr, Bowen JD, Rodriquez AA, Haselkorn JK. Prevalence and correlates of depression among veterans with multiple sclerosis. Neurology. 2005;64(1):75–80. doi: 10.1212/01.WNL.0000148480.31424.2A. 64/1/7510.1212/01.WNL.0000148480.31424.2A. [DOI] [PubMed] [Google Scholar]
- Wood B, van der Mei IAF, Ponsonby AL, Pittas F, Quinn S, Dwyer T, Taylor BV. Prevalence and concurrence of anxiety, depression and fatigue over time in multiple sclerosis. Multiple Sclerosis Journal. 2013;19(2):217–224. doi: 10.1177/1352458512450351. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]