Abstract
Aim
Facial aging is the union of multiple effects such as exposure to the sun, ambiental stress, smog, tobacco. It reflects the dynamic, cumulative effects of time on the skin, soft tissues, and deep structural components of the face showing skin textural changes and loss of facial volume. There are a multitude of techniques currently used to perform face lifts, but the unique objective is to achieve a good and safe result.
Methods
This paper describes a new safe approach to midfacial rejuvenation that combines the elements of superficial musculoaponeurotic system (SMAS) plication, about four vectors, with a blepharoplasty to achieve long-lasting improvement of the aging midface and a more natural effect. Plication of the SMAS over the suture, provides three vectors of elevation beneath the skin in midface rhytidectomy linked to the Lorè’s fascia and the third vector of elevation of platysma behind the ear.
Results
This new technique, called KOr.U technique, was used in 31 patients between October 2010 and October 2012, producing effective long-lasting results, returning a volume of midface with no injury.
Discussion
This simplified approach is safe and can be easily performed under local anesthesia as an isolated midface procedure, avoiding the facial nerve.
Keywords: KOr.U, Face lift, Vector, Blepharoplasty
Introduction
The effects of facial aging include elongation of lower eyelid, flattering of malar eminence, volumetric loss in submalar area of the cheek, prominence of the jowls and deepening of nasolabial fold. The retaining ligaments of the face support facial soft tissue in normal anatomic position, resisting gravitational change. A loss of zygomatic ligament support allows for inferior descent of the malar pad, influencing nasolabial fold prominence, whereas a loss of masseteric ligament support allows for the inferior descent of facial fat to the mandibular border. In 1976 Mits and Peyronie [1] described the superficial musculoaponeurotic system (SMAS) and after this date multiple surgical procedures were improved [2, 3]. This technique produces excellent result, but requires extensive dissection and has the potential for increased morbidity. The anatomical distribution of the facial nerve has been studied by various authors [4] and during surgical dissection must be considered the dangerous zone of the face. The frontal branch is one of the most commonly damaged nerves in plastic surgery. The path of the frontal branch can be drawn on the skin by two diverging lines which start from region of the ear lobulus and go [5] to the lateral end of the eye [6] and to the highest frontal crease. To locate the frontal branches it is useful look up the superficial temporal artery. The buccal and zygomatic nerve branches located deep down and at the nasolabial fold an excess of skin and fat is found which give more protection to the nerve below [7–9]. The mandibular branch [10] is located above the lower border of the mandible in 80 % of the cases, in the remaining 20 % it forms an arch beneath the lower border of this bone and always runs within or deep to the muscular fibers of platysma. Hence, in this zone, there is almost no danger of injuring the nerve. In this study we describe a new simple and safe face-lift technique, KOr.U technique, that we think optimal for our patient and easy to teach to young surgeons as a first approach to this surgical procedure during our courses on cadaver.
Materials and Methods
Thirty-one patients between October 2010 and October 2012 were treated by a new technique, called KOr.U face-lift technique. The age of the patients ranged between 35 and 64 years. There were 25 women and 6 men. All the patients were primary face-lift.
Description of Technique
The skin incision [11, 12] is made along the temporal hairline and extends in conventional face lift location into the post auricular sulcus, posteriorly it extends over the mastoid following a line of external auditory canal. The skin flap is elevated in a subcutaneous plane and the dissection extends until 2 cm to the labial commissure to respective buccal branches of the facial nerve. Inferiorly the dissection is made to expose the neck and the mandibular border, superiorly it extends to the orbital rim and over superior border of zygomatic bone. The authors suggest that the dissection is more safe and less difficult to find out the right plan of dissection if the surgeon started at the temporal region. All face lift procedures were associated with a blepharoplasty using Adamson et al. [13] and Mendelson [14] techniques. The plications of the SMAS are performed about four vectors: the first vector goes from external canthus to tragus and gives a vertical direction; the second vector goes from ear tuberculum to the oral commissure and gives a vertical/oblique direction; the third vector goes from mandible angle to the Lore’s fascia and the fourth vector goes from retro/sub-auricular platysma to the mastoid. The last two vectors giving a vertical direction and a definition of mandible angle drawing a U around the ear lobe (Figs. 1, 2, 3). The choice of these points of traction was according to zone of the face where the branches of the facial nerve are more deep to work on safely (Fig. 3). A suture of the plication performed between canthus and tragus was made to create a spindle to restore the volume of the cheek. The suture takes less tissue on marginal zone in the direction of canthus and tragus and takes more tissue in the central zone of placation. In this way we can restore the loss of volume in a point of major projection of the face and confer a well-rounded 3D topography that is delineated by series of arcs and convexities [2, 3, 7–9, 11, 15–19] (Fig. 2). Subcutaneous sutures were made by Vicryl 3/0 while cutaneous sutures were made by Nylon 6/0 on antitragus incision and by Nylon 5/0 on temporal incision and retro-auricular incision. On these last two sections of the cut sutures were continuous whip-stitch suture while on antitragus incision was continuous intradermal.
Fig. 1.
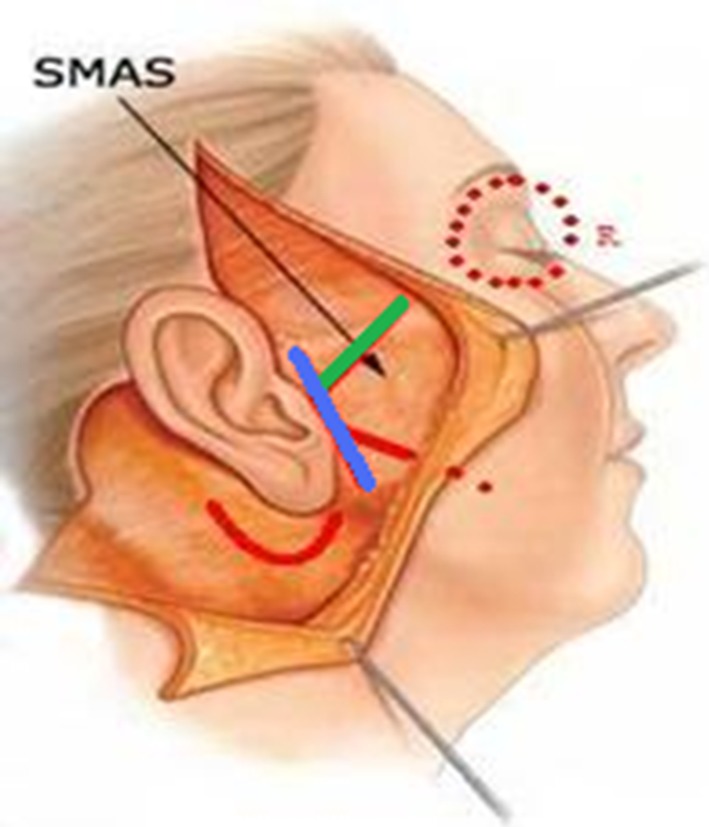
The plications of the SMAS are performed about four vectors: 1st vector green line; 3rd vector blue line; 2nd vector red straight line; 4th vector red U line (see text)
Fig. 2.
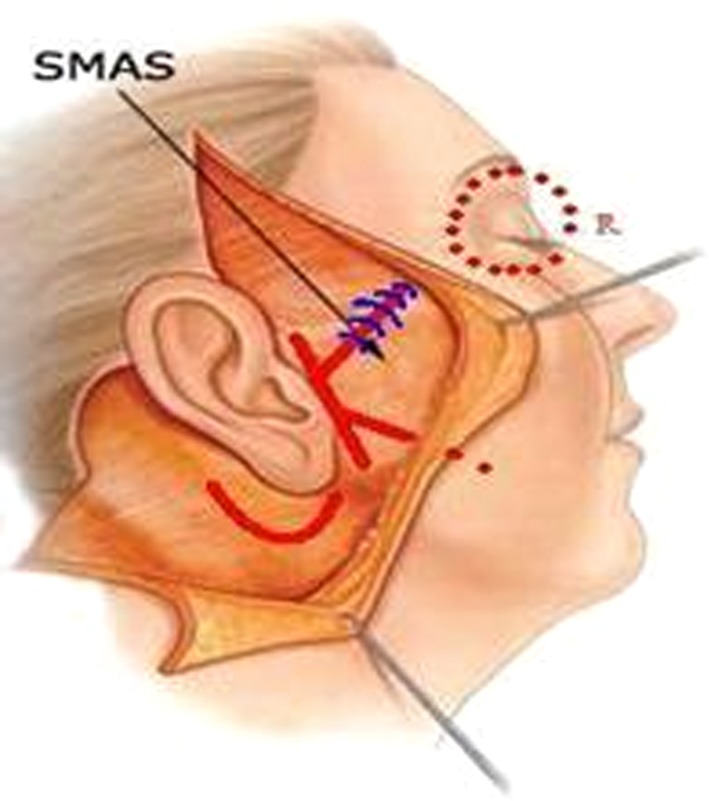
The suture takes less tissue on marginal zone in direction of cantus and tragus and takes more tissue in the central zone of placation, to restore the loss of volume in a point of major projection
Fig. 3.

Intraoperatorial view
Results
From October of 2010 to October of 2012, 31 KOr.U face lift were performed. In no case there were infection, there is minimal tension on the suture line. There is minimal postoperative edema, as well as minimal postoperative ecchymoses. This technique produce effective results, regives a volume of midface with no injury to the facial nerve. This study showed a new and safe approach to midfacial rejuvenation that combines the elements of SMAS placation with a blepharoplasty to achieve long-lasting improvement of the aging midface and a more natural effect (Fig. 4). The low incidence of morbidity and a rapid convalescence has allowed many patients to return to employment and social activities sooner with excellent satisfaction. This technique is optimal to edit the mid face and the lower third of the face and to stretch the neck to a global refreshment (Fig. 5).
Fig. 5.

A transposition of cutaneous vectors in preoperative view. The continuous line indicates the limit of limit of skin lifting by layer below
Fig. 4.

A case: pre and post op. Follow up at 3 months
Discussion
After the description of the SMAS in 1976 [1] surgical attempts to correct aging were directed towards techniques of tightening the SMAS. Hamra’s [20] introduction of the deep plane rhytidectomy in 1990 focused attention on an entirely new concept of rejuvenation by composite repositioning of facial tissues. The peripheral course of the facial nerve has been studied intensively by various anatomical studies; they analyzed the anatomical distribution of the branches and the different types of nerve connections that exist between them. In this paper a new and safe face lift technique is described that preserves the facial nerve and could be performed more easily. This procedure opened the possibilities of further morbidity in midface lifting. The dissection of skin flap started by temporal region incision [17], the placation of the SMAS was performed by three sutures that describe three vectors, as shown in cadaveric dissection (Fig. 6). The superior suture which goes from external canthus to tragus is made to produce more malar augmentation, while the suture of platysma on mastoid gives minimal tension on the suture line. Colombo and Ruvolo, the authors, always associate SMAS plication to blepharoplasty about Adamson and a fat sliding about Mendelson. An adjunctive technique for lower lid blepharoplasty is performed. This operative procedure uses the principle of anchoring the upper margin of the lower lid by suturing a triangular muscle flap from it to the lateral-superior part of the orbital rim. This gives more effective support for the lower lid margin and permits one to excise more redundant tissue without getting an ectropion [13]. The concept of replacing the bulging fat of the lower lid back into the orbit and maintaining it there by strengthening the orbital septum is appealing because it epitomizes the goal of aesthetic surgery to restore the youthful ideal by reversing the structural changes of aging. This concept contrasts with that of standard blepharoplasty procedures that use a simple excisional and tightening approach to achieve superficial improvement [14]. About our experience we believe that SMAS plication and SMAS imbrication give similar results [16, 18] so we choose only plication procedure with blepharoplasty obtaining the important outcome as an excellent aesthetic result with a high level of patient satisfaction (Fig. 4). This technique is optimal to edit the mid face, central zone and lower third of the face and stretching of the neck to a global refreshment. The KOr.U face lift technique influencing on the midface, on the orbital zone and on the neck gives a global refreshing to the face, giving a natural look.
Fig. 6.

Plication of smas in cadaveric dissection. The range between two instruments shows the plication suture and the lifting of smas
Acknowledgments
The authors thank Dr. Valentina Pagliarulo, Cranio Maxillo Facial Surgeon, Resident of Second University of Naples, who provided description of this technique. This article would not have been possible without her help.
Contributor Information
Giuseppe Colombo, Email: info@aesthetic-koru.it, http://www.aesthetic-koru.it.
Vittorio Ruvolo, Email: info@aesthetic-koru.it, http://www.aesthetic-koru.it.
Valentina Pagliarulo, Email: dott.pagliarulo@gmail.com.
References
- 1.Mitz V, Peyronie M (1976) The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg 58(1):80–88 [DOI] [PubMed]
- 2.Wilhelmi BJ, Mowlavi A, Neumeister MW. The safe face lift with bony anatomic landmarks to elevate the SMAS. Plast Reconstr Surg. 2003;111:1723–1726. doi: 10.1097/01.PRS.0000054237.81611.D8. [DOI] [PubMed] [Google Scholar]
- 3.Mentz HA, III, Ruiz-Razura A, Patronella CK, Newall G. Facelift: measurement of superficial muscular aponeurotic system advancement with and without zygomaticus major muscle release. Aesthet Plast Surg. 2005;29:353–362. doi: 10.1007/s00266-005-0005-4. [DOI] [PubMed] [Google Scholar]
- 4.Correia P, Zani R. Surgical anatomy of the facial nerve, as related to ancillary operations in rhytidoplasty. Plast Reconstr Surg. 1973;52:549–552. doi: 10.1097/00006534-197311000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Baket TJ, Gordon H. Complications of rithidectomy. Plast Reconstr Surg. 1967;40:31. doi: 10.1097/00006534-196707000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Byars IT. Preservation of the facial nerve in operations for benign conditions of the parotid area. Ann Surg. 1952;136:412. doi: 10.1097/00000658-195209000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruess W, Owsley JQ. The anatomy of the skin and fascial layers of the face in aesthetic surgery. Clin Plast Surg. 1987;14:677–682. [PubMed] [Google Scholar]
- 8.Rohrich RJ, Pessa JE. The fat compartments of the face: anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119:2219–2227. doi: 10.1097/01.prs.0000265403.66886.54. [DOI] [PubMed] [Google Scholar]
- 9.Özdemir R, Kilinç H, Ünlü RE, Uysal AÇ, Sensöz O, Baran CN. Anatomicohistologic study of the retaining ligaments of the face and use in face lift: retaining ligament correction and SMAS plication. Plast Reconstr Surg. 2002;110:1134–1147. doi: 10.1097/00006534-200209150-00019. [DOI] [PubMed] [Google Scholar]
- 10.Nelson DW, Gingrass RP. Anatomy of the mandibular branches of the facial nerve. Plast Reconstr Surg. 1979;64:479–482. doi: 10.1097/00006534-197910000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Baker TJ, Stuzin JM. Personal technique of face lifting. Plast Reconstr Surg. 1997;100:502–508. doi: 10.1097/00006534-199708000-00038. [DOI] [PubMed] [Google Scholar]
- 12.Little JW. Three-dimensional rejuvenation of the midface: volumetric resculpture by malar imbrication. Plast Reconstr Surg. 2000;105:267–285. doi: 10.1097/00006534-200001000-00044. [DOI] [PubMed] [Google Scholar]
- 13.Adamson JE, McCraw JB, Carraway JH. Use of a muscle flap in lower blepharoplasty. Plast Reconstr Surg. 1979;63:359–363. doi: 10.1097/00006534-197903000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Mendelson BC. Fat preservation technique of lower-lid blepharoplasty. Aesthet Surg J. 2001;21:450–459. doi: 10.1067/maj.2001.119405. [DOI] [PubMed] [Google Scholar]
- 15.Coleman SR, Grover R (2006) The anatomy of the aging face: volume loss and changes in 3-dimensional topography. Aesthet Surg J 26 [DOI] [PubMed]
- 16.Kamer FM, Frankel AS. SMAS rhytidectomy versus deep plane rhytidectomy: an objective comparison. Plast Reconstr Surg. 1998;102:878–881. doi: 10.1097/00006534-199809010-00041. [DOI] [PubMed] [Google Scholar]
- 17.Massiha H. Short-scar face lift with extended SMAS platysma dissection and lifting and limited skin undermining. Plast Reconstr Surg. 2003;112:663–669. doi: 10.1097/01.PRS.0000070945.35807.CE. [DOI] [PubMed] [Google Scholar]
- 18.Webster RC, Smith RC, Papsidero MJ, Karolow WW, Smith KF. Comparison of SMAS plication with SMAS imbrication in face lifting. Laryngoscope. 1982;92:901–912. doi: 10.1288/00005537-198208000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Little JW. Volumetric perceptions in midfacial aging with altered priorities for rejuvenation. Plast Reconstr Surg. 2000;105:252–266. doi: 10.1097/00006534-200001000-00043. [DOI] [PubMed] [Google Scholar]
- 20.Hamra ST. The deep plane rhytidectomy. Plast Reconstr Surg. 1990;86:53. doi: 10.1097/00006534-199007000-00008. [DOI] [PubMed] [Google Scholar]


