Abstract
Background and objective
Ankylosis of the temporomandibular joint is a clinical entity significant for a maxillofacial surgeon. Since time immemorial humanity is battling with this condition which is not just disfiguring the normal anatomy of the face but severely hampers the function of mastication. In this study we have tried to evaluate and correlate various factors leading to causation of ankylosis of TM Joint along with clinical manifestation and treatment planning as well as outcomes.
Study design
This is a retrospective study, records of 60 patients were selected out of which 28 patients reported for recall. Based on a predefined format, patients were evaluated and correlation was looked up on various accounts such as age of occurrence and age of reporting to the surgeon, probable etiology, sex distribution, treatment modality and postoperative outcome.
Results
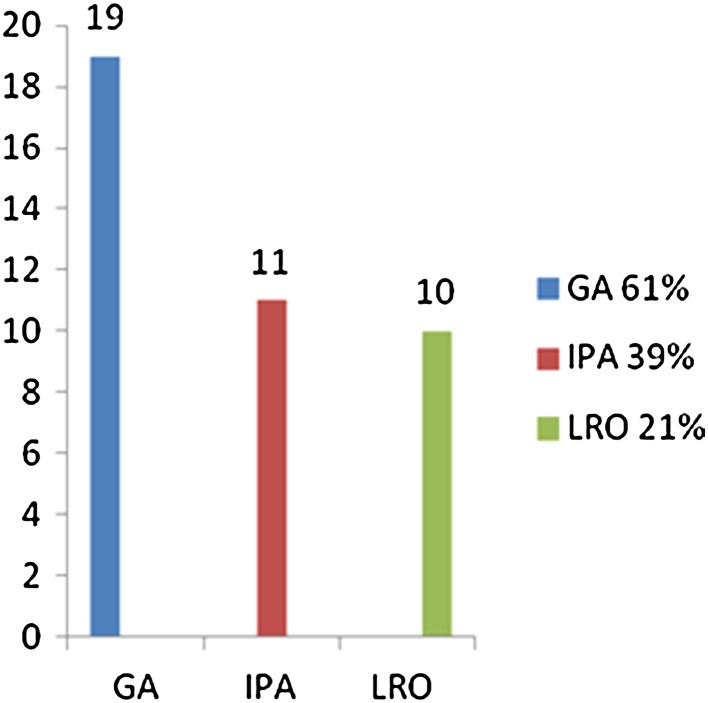
The mean age of onset or occurrence was 4–7 years of age whereas age of reporting to the clinic was 16–17 years. Highest percentage of patients had trauma as an etiology (64 %) and the lowest percentage had congenital deformity (21 %). Three surgical techniques were evaluated and compared for their post surgical mouthopening, gap arthroplasty was done in 61 %, interpositional arthroplasty in 39 % and low ramus osteotomy in 21 %.
Conclusion
This study was aimed at analyzing the clinical form and function of the post surgical patient reviewing the recent radiographs to analyze the surgical site. The data collected was (1) Age of occurrence and age of reporting with the deformity (2) Etiological history (3) Sex and Side predisposition (4) Procedure used for correction of deformity (5) Recall (follow up) data especially recurrence and physiotherapy. We arrived at a conclusion that mean age of occurrence of deformity was approximately 4.7 years and age at which patient reported to clinic was 16.2 years. The main etiological factor was trauma (51 %) and ear infection (21 %). 57 % patients presented with unilateral deformity, with both the sides equally effected. The effectiveness of gap arthroplasty, interpositional arthroplasty and low ramus osteotomy procedures was evaluated. Gap arthroplasty and interpositional arthroplasty were found to be effective procedures. The importance of post operative physiotherapy was emphasised yet again through this study.
Keywords: TMJ, Ankylosis, Osteotomy
Introduction
Ankylosis of the Temporomandibular Joint is an affliction which occasions much misery for the unfortunate victim, interfering with the mastication and digestion of food, denying the body of the benefits of a balanced diet and preventing participation in the pleasure traditionally associated with the culinary arts. If the condition develops in childhood, facial deformity brings psychological stress which adds to the physical handicap, thus disrupting family life and creating emotional disturbance. Trauma is well proven to be the predominant cause of temporomandibular joint ankylosis. The other causes that could lead to TMJ ankylosis are local or systemic infections (otitis media in childhood) and systemic diseases like ankylosing spondilitis, rheumatoid arthritis and psoriasis. The treatment of ankylosis differs considerably in a pediatric and an adult patient. Sawney [1] offered a lucid classification in children which is helpful in selecting the appropriate, corrective operation (Table 1). He suggests that ankylosis can be grouped in 4 well defined types depending upon the pathologic changes. This grading is very useful in deciding the extent of surgical treatment.
Table 1.
Sawney grading system
| Type I | Condylar head is present without much distortion. Fibrous union make movement much impossible |
| Type II | Bony fusion of the misshaped head and the articular surface. No involvement of sigmoid notch and coronoid process |
| Type III | Bony blocking bridge across the ramus and the zygomatic arch. Medially an atrophic dislocated fragment of the former head of the condyle is still found. Elongation of the coronoid process seen |
| Type IV | The normal anatomy of the TMJ is totally destroyed by complete bony block between the ramus and the skull base |
Whatsoever may be the type, early surgical correction and reconstruction of the deformity soon followed by jaw mobility exercise should be encouraged in children in order to get good results out of the surgery and also prevent future re ankylosis. Whereas in adults, besides correction of ankylosis, consideration must be given to possible simultaneous need for coronoidectomy. Role of physiotherapy cannot be overlooked even in adult patients.
Materials and Methods
Sixty patients who reported to the department during the 8 years of time span between 1992 and 2000, with a chief complaint of inability to open the mouth, were included in the study on the basis of clinical examination and only those patients who presented with restriction of mouth opening secondary to ankylosis were selected for the study. The presence of trismus due to various other causes like OSMF, internal derangement, inflammation and infection, tumor and cyst were not included in the study (Table 2).
Table 2.
a Age distribution. b Age of reporting
| Group | Age of occurrence (years) | Numbers |
|---|---|---|
| I | 0–5 | 19 |
| II | 6–10 | 04 |
| III | 11–15 | 04 |
| IV | 16–20 | 02 |
| Age on reporting (years) | Numbers |
|---|---|
| 1–5 | 02 |
| 6–10 | 05 |
| 11–15 | 05 |
| 16–20 | 09 |
| 21–25 | 04 |
| 26 and above | 03 |
The information gained mainly focused on age of occurrence of the condition and the age at which the patient reported to the clinic. Enquiries were made about any traumatic incidents in the past (childhood trauma), recurrent middle ear infection and forceps delivery. Questions were asked regarding stiffness in other joints other than TMJ (rheumatoid arthritis) or previous history of fever in the childhood (erysipelas). The main aim of this questionnaire was to arrive at a probable aetiology leading to ankylosis (Table 3).
Table 3.
Age relation
| Age | Occurrence | Reporting (years) |
|---|---|---|
| Min. age | Birth | 1 |
| Max. age | 19 years | 40 |
| Mean age | 4.7 years | 16.2 |
In clinical examination patients were looked up for facial asymmetry, facial profile, bird face deformity, deviation on mouth opening, painful mouth opening, interincisal opening and presence of antegonial notch (Fig. 1). In the radiological investigation OPG and PA view mandible were done. Since it is a retrospective study CT Scans were not considered due to unavailability or in affordability as main factors, as the condition is prevalent in lower socioeconomic group (Chart 1, 2).
Fig. 1.
a Facial profile. b Lateral profile. c Restricted mouth opening. d OPG
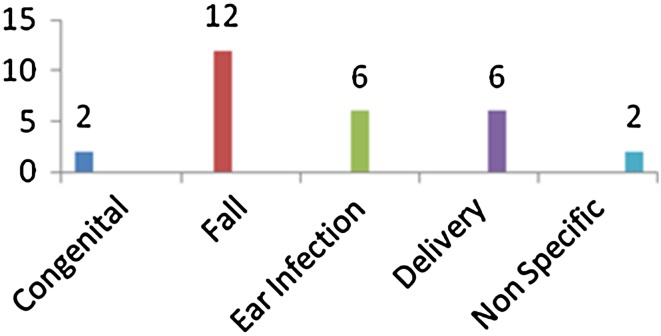
Chart 1.
Etiology
Chart 2.

Sex distribution
In the end operative procedures were looked for, like approaches used, procedure of interpositional arthroplasty, gap arthroplasty (Fig. 2), gap arthroplasty and low ramus osteotomy. Forcible mouth opening on the operating table was recorded. Immediate post surgical mouth opening and any post surgical complications were also recorded. Records were strictly evaluated for exercise/physiotherapy, history of recurrence and the correlation between patient compliance with physiotherapy exercise and recurrence of the condition.
Fig. 2.
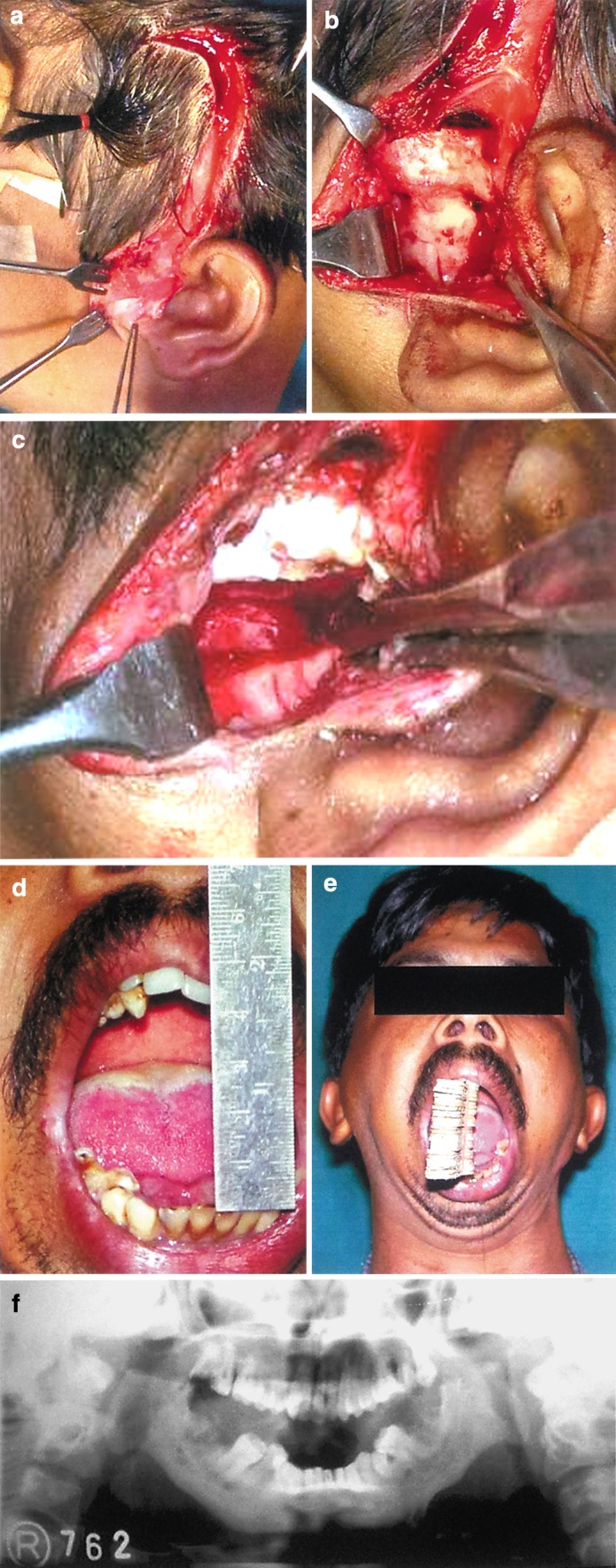
a Endural incision with temporal extension. b Site of bony ankylosis exposed. c Gap created with help of bur and osteotome. d Post operative mouth opening of 6 cm. e Postoperative physiotherapy. f Immediate post op OPG
Twenty-eight out of 60 patients turned up for a delayed follow up. On the recall visit all the patients were checked for the latest forcible inter incisal and inter molar opening and OPG and PA mandible views were repeated to evaluate the present status of the operated site (Fig.3).
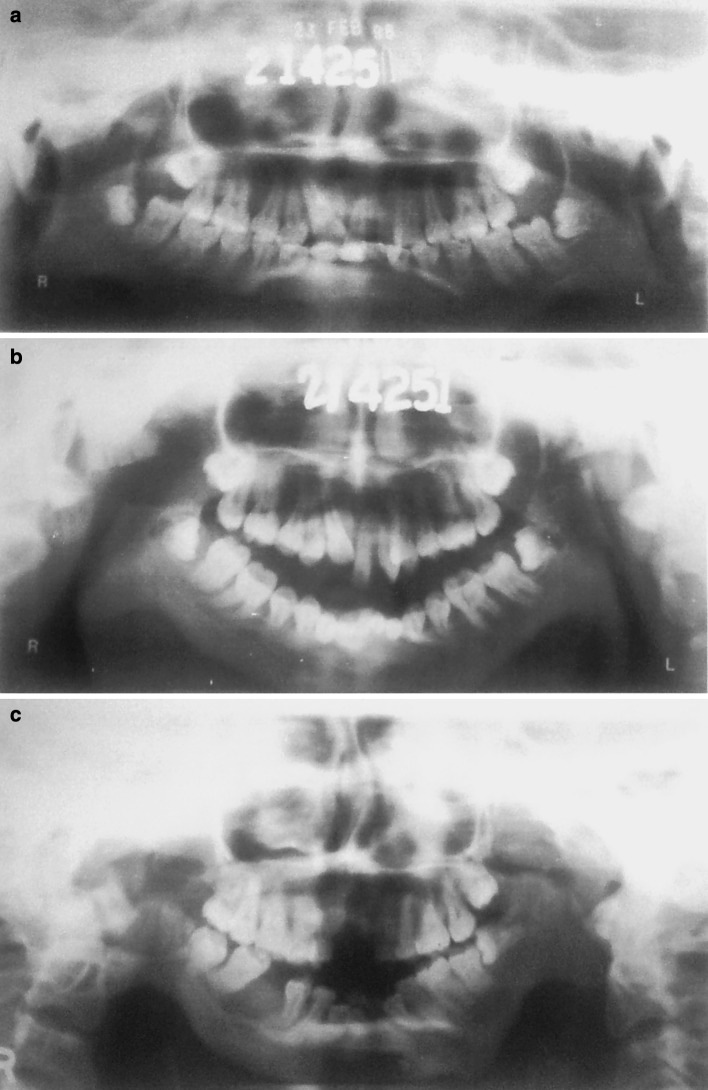
Fig. 3.
a Pre operative OPG. b Immediate post op low ramus osteotomy. c 6 years post op OPG
Immediate mouth opening was evaluated and recorded postoperatively. The minimum recorded value was 2 cm whereas the maximum was 6.4 cm leading the to mean mouth opening of 2.9 cm. Mouth opening recorded in the delayed post op follow ups were recorded as a minimum of 2.5 cm and a maximum of 5 cm.
Most commonly encountered postoperative complications were perforation of auditory canal noted in 4 cases. Middle ear infection (pus discharge) and traction of temporal branch of facial nerve were observed in 1 patient each. Recurrence of ankylosis were recorded in 16 cases.
Results
The average age of patient when he/she reported to the clinic was between 16 and 17 years whereas the historical data collected from the patient revealed that probably the mean age at which condition occurred was between 4 and 7 years of age. Hence in most of the patients who presented themselves to the clinic, the condition was well established. In case of patients of younger age group, the inquiries were made with guardians.
According to our study through the review of 28 patients who came for delayed follow up on request, in 64 % cases etiology was trauma which included simple fall on the chin region (42 %) and forceps delivery (22 %) and 21 % was childhood middle ear infection and rest were cases where history was not very clear but the condition had resulted in early childhood.
Otitis media was a causative factor in 21 % of the patients especially in childhood. This could be because in this study 57 % of the cases were of unilateral ankylosis and 42 % of the cases were of bilateral ankylosis. Both right and left side were equally affected in unilateral cases. Those patients who had unilateral ankylosis since early childhood and presented with mandibular asymmetry, the appearance is usually that of flatness and elongation of unaffected side. The midpoint of the chin and mandibular midline were deviated to ankylosed side.
The techniques used in this study were gap arthroplasty, interpositional arthroplasty and low ramus osteotomy with varying degrees of success (Chart 3). In this study we have seen that gap arthroplasty and interpositional arthroplasty both have given us equally good results in presence of patient compliance with postoperative physiotherapy.
Chart 3.
Surgical procedures
We follow a protocol proposed by Kaban [2] in 1990 for management of TMJ ankylosis with little modification. Ankylotic mass is usually resected aggressively via endural approach with extension in temporal region for better access. Ipsilateral coronoidectomy is done when mere excision of the ankylotic mass does not improve the mouth opening. Contralateral coronoidectomy is also done under similar circumstances. Interpositional material of choice in our centre was temporalis fascia and patient was usually started with postoperative mouth opening exercise after 24 h of the surgery. Post operative drains were used whenever haemorrhage was encountered and was left in situ for 24–48 h. Minor complications were encountered post surgically like middle ear infection and perforation of auditory canal. These complications were treated symptomatically by prescribing antibiotic ear drops and ear dressing. In one case traction of the temporal branch of the facial nerve was seen, where patient presented with inability to close the eye, The patient recovered spontaneously after 3–4 months. Our Study confirms the effectiveness of these techniques equally.
Literature Review and Discussion
Our results were consistent with the studies of Topazian [3] and Straith [4] which point towards the time lapse between the age of onset and age of patient reporting to clinic. In the study by Topazian [5] trauma accounts for 75 % of the times as an etiological factor especially childhood trauma in the chin region causing intra-articular fracture of the condyle and haemarthrosis with resultant fibrous or bony ankylosis especially because this injury occurs at early childhood and at the time of injury there may not be much of clinical evidence suggesting trauma to the joints except for pain and hence neglect and ignorance on behalf of parents can lead to progression of the deformation. Beavis (Topazian) [6] has observed that many children between 1 and 10 years of age may be struck on the point of chin with considerable violence and not have ankylosis, whereas there are a few who will. He suggested susceptibility to any other pathologic changes. Straith [4] and Topazian [5] suggest that most of the times congenital ankylosis results from traumatic injuries received at birth and should not be regarded as true congenital abnormality. Otitis media is a common complication of measles or mumps and is caused by secondary infection by haemolytic streptococci or as primary otitis media where the pus in the middle ear burrows forwards and ruptures the glenoid cavity and gets into the joint space leading to suppurative inflammation of the joint. As described in an important study on ankylosis by Topazian [5], infectious diseases such as rheumatoid arthritis, rheumatoid spondylitis, small pox, mumps, thyphoid were listed as less common but possible cause of ankylosis of temporomandibular joint whereas majority of cases were related to trauma and otitis media.
The clinical presentation of the patient depends on duration of condition, age of occurrence, and degree of involvement (severity) and whether unilateral or bilateral. A case of bilateral ankylosis of longstanding duration and age of occurrence in early childhood (before growth) would typically present with “Andy Gump” or Vogelgesicht deformity where the upper anterior teeth are proclined, there is severe mandibular retrognathia and retrogenia and since surrounding tissues continue to grow normally, double chin effect is classically present [7–9]. Additionally one also sees varying degrees of difficulty in speech, mastication and minimal mouth opening, occlusal derangement and poor oral hygiene. All the longstanding cases of ankylosis had a prominent antegonial notches [8, 10, 11].
Salins [12] reported the technique of low ramus osteotomy where he had used temporalis muscle, costocondral graft and masseter as interpositional material. According to our study out of 7 cases treated by procedure of low ramus osteotomy, 6 patients came back with recurrence and for the second surgery either interpositional arthroplasty or gap arthroplasty was used (Fig. 3). There is not much data available in the literature describing the procedure of low ramus osteotomy as well as its success rate. From the historical point of view, it was Esmarch [13] who was credited with the first attempt at surgical correction of ankylosis by removing a full thickness wedge of bone from mandibular ramus below the point of ankylosis and creating a false joint. Risdon [10] in 1934 described a Low Ramus Proceudre. In this procedure ramus is approached by submandibular region and masseter is interposed between the cuts, other than these two instances there is no mention of this procedure in the literature and according to our experience this procedure does not have a good success rate.
There is abundant evidence in the literature which proves the creditability of interpositional arthroplasty and gap arthroplasty. But most of the authors believe that interposition of autograft or alloplastic material definitely reduces the incidence of recurrence, at the same time others feel that creation of sufficient gap between the two surfaces (1.5–2 cm) should be adequate and may not require interpositioning of any material unless there is no bone left out in the medial aspect of the ankylosed joint.
The diligence and perseverance of the patients in exercising accounted for retention of good interincisal opening which plays an important role in defining the end treatment outcome. The mouth opening exercise mainly comprised of use of ice cream sticks to improve mouth opening and passive mouth opening with the help of mouth gag and splints [14].
Conclusion
This study was aimed at analyzing the clinical form and function of the post surgical patient reviewing the recent radiographs to analyze the surgical site. The data collected was (1) Age of occurrence and age of reporting with the deformity (2) Etiological history (3) Sex and Side predisposition (4) Procedure used for correction of deformity (5) Recall (follow up) data especially recurrence and physiotherapy.
We arrived at a conclusion that mean age of occurrence of deformity was approximately 4.7 years and age at which patient reported to clinic was 16.2 years. The main etiological factor was trauma (51 %) and ear infection (21 %). 57 % patients presented with unilateral deformity, with both the sides equally effected.
The effectiveness of gap arthroplasty, interpositional arthroplasty and low ramus osteotomy procedures was evaluated. Gap arthroplasty and interpositional arthroplasty were found to be effective procedures.
In the end we conclude that the best done surgical procedure may not prove to be very effective in case patient does not comply with post operative physiotherapy exercise. We still believe that a prospective study for the same would be more definitive and informative.
References
- 1.Sawney CP. Bony ankylosis of the temporomandibular joint: follow up of 70 patients treated with arthroplasty and acrylic spacer interposition. Plastic Reconstr Surg. 1986;77(1):29–38. doi: 10.1097/00006534-198601000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1981;48:1145–1151. doi: 10.1016/0278-2391(90)90529-B. [DOI] [PubMed] [Google Scholar]
- 3.Topazian RG. Comparison of gap and interpositional arthroplasty in the treatment of temporomandibular joint ankylosis. J Oral Surg. 1966;24(5):405. [PubMed] [Google Scholar]
- 4.Straith CL, Lewis JR (1948) Ankylosis of temporomandibular joint. Plast Recostr Surg 3:464–466 [DOI] [PubMed]
- 5.Topazian RJ. Etiology of ankylosis of TMJ: analysis of 44 cases. J Oral Surg Anesth Hosp Dent Serv. 1964;22:227. [PubMed] [Google Scholar]
- 6.Wu XG, Sun KH, Hong M. Chondrocyte clusters in the condylar cartilage of an ankylosed temporomandibular joint. Int J Oral Maxillofacial Surg. 1993;22:336–338. doi: 10.1016/S0901-5027(05)80661-7. [DOI] [PubMed] [Google Scholar]
- 7.Row NL (1982) Ankylosis of temporomandibular joint Part I. J R Coll Surg Edinb 27:67–69 [PubMed]
- 8.Adekeye EO. Ankylosis of the mandible: analysis of 76 cases. J Oral Maxillofac Surg. 1983;41:442–449. doi: 10.1016/0278-2391(83)90129-5. [DOI] [PubMed] [Google Scholar]
- 9.Raveh J, Vullemin T, Ladrach K, Sutter F. Temporomandibular joint ankylosis: surgical treatment and long term result. J Oral Maxillofac Surg. 1989;47:900–906. doi: 10.1016/0278-2391(89)90371-6. [DOI] [PubMed] [Google Scholar]
- 10.Stadnicki G. Congenital double condyle of the mandible causing temporomandibular joint ankylosis: report of case. J Oral Surg. 1971;29:208–211. [PubMed] [Google Scholar]
- 11.Row NL (1982) Ankylosis of temporomandibular joint Part II. JR Coll Surg Edinb 27(3):167–173 [PubMed]
- 12.Salins PC. Soft and hard tissue correction of facial deformity associated with bilateral temporomandibular joint ankylosis. Int J Oral Maxillofac Surg. 1998;27:422–424. doi: 10.1016/S0901-5027(98)80029-5. [DOI] [PubMed] [Google Scholar]
- 13.Silagi JL, El Paso, Jr Schow CE. Temporomandibular joint arthroplasty: review of literature and report of case. J Oral Surg. 1970;28:920–926. [PubMed] [Google Scholar]
- 14.Nwoku LA. Rehabilitating children with temporomandibular joint ankylosis. Int J Oral Surg. 1979;8:271–275. doi: 10.1016/S0300-9785(79)80048-4. [DOI] [PubMed] [Google Scholar]