Abstract
Objectives
The purpose of this study was to carry out systematic review of the literature and meta-analysis to evaluate the diagnostic utility of cerebrospinal fluid (CSF) levels of the 42 amino acid form of amyloid-beta (Aβ1–42) as a biomarker for differentiating Alzheimer’s disease (AD) from non-AD dementia.
Methods
Design. Systematic literature review was used to evaluate the effectiveness of the Aβ for the diagnosis of AD. The Scottish Intercollegiate Guidelines Network (SIGN) tool was used to evaluate independently the quality of the studies.
Data sources. The literature review covered from January 1, 2004, to October 22, 2013, and searched eight domestic databases including Korea Med and international databases including Ovid-MEDLINE, EMBASE, and Cochrane Library.
Data Extraction and Synthesis. Primary criteria for inclusion were valid studies on (i) patients with mild cognitive impairment with confirmed or suspected AD and non-AD dementia, and (ii) assessment of Aβ1–42 levels using appropriate comparative tests.
Results
A total of 17 diagnostic evaluation studies were identified in which levels of CSF Aβ1–42 were assessed. Meta-analysis was performed on 11 robust studies that compared confirmed AD (n = 2211) with healthy individuals (n = 1030), 10 studies that compared AD with non-AD dementias (n = 627), and 5 studies that compared amnestic mild cognitive impairment (n = 1133) with non-amnestic type subjects (n = 1276). Overall, the CSF Aβ1–42 levels were reduced in AD compared to controls or non-AD dementia. The effectiveness of test was evaluated for diagnostic accuracy (pooled sensitivity, 0.80 (95% CI 0.78–0.82); pooled specificity, 0.76 (95% CI 0.74–0.78).
Conclusions
Reduced CSF Aβ1–42 levels are of potential utility in the differential diagnosis of AD versus non-AD dementias and controls. Diagnostic accuracy was high in AD versus healthy controls. However, differential diagnosis for MCI or non-AD might be evaluated by other biomarkers.
Introduction
A substantial proportion of current therapeutic development in AD focuses on therapies targeting the Aβ peptide or Aβ aggregates, the core pathology of AD [1,2]. However, large-scale clinical trials of Aβ removal by immunological or pharmacologic means have yielded no reproducible benefits [2]. There are two routes to resolve this dilemma. First, anti-Aβ therapies (and perhaps anti-tau therapies) might be conducted on minimally affected individuals (secondary prevention in stages 1/2). A second strategy is to develop therapies that are likely to be of benefit in symptomatic patients (i.e., in a preclinical stage 3 or prodromal AD) [2]. Therefore, further development of AD therapeutics will require the establishment of biomarkers that accurately reflect the progression of AD pathology, thereby permitting early diagnosis of AD and facilitating drug trials selectively targeting the early predementia stages of the disease [3].
The sampling of cerebrospinal fluid (CSF) represents the most direct and convenient methods to study the biochemical changes occurring in the central nervous system. Aβ1–42, tau, and phosphorylated forms of tau have emerged as attractive diagnostic and prognostic CSF biomarkers for ongoing AD research [4,5]. Decreased CSF Aβ1–42 has been proposed as an useful diagnostic tool for AD [4]. It has been reported that the mean level of Aβ1–42 in the CSF are reduced to around 50% in subjects with AD relative to age-matched controls against initial prediction [4], and diagnosis of AD has evolved towards separate categories of preclinical and overt dementia based on levels of CSF Aβ1–42 [6]. However, CSF Aβ1–42 levels have been reported to fluctuate over time in a cohort of old and young individuals [7], and no absolute threshold has been identified that would differentiate between mild cognitive impairment and AD in mildly symptomatic individuals [8].
In the present study we aimed to review systematically the reported association between CSF Aβ1–42 and AD with a view to evaluating the clinical usefulness of CSF Aβ1–42 in the differential diagnosis of AD versus non-AD cognitive impairment.
Methods
Systematic literature review was performed according to the reporting guidelines of the Arbitration Act Handbook (Hoggins and Green) as proposed by the Cochrane Union (Cochrane collaboration) and the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) group [9]. In this study all researchers were recommended by the Korean Medical Association: these comprised a specialist of the Korean Ministry of Health and Welfare, two experts in laboratory medicine, two neurologists, and one neurological surgeon. Six meetings of all experts were held (three times in writing, three times in person) to (i) establish selection criteria, (ii) review studies selected for inclusion, (iii) overview data extraction, (iv) refine and validate the conclusions of the study.
1. Systematic literature review
Systematic literature searching was performed in the Ovid-MEDLINE, EMBASE, and Cochrane Library data bases, as well as Korea Med, and was completed on October 22, 2013. Medline searching was conducted to locate all studies published in English and Korean from January 2004 to March 2013 using MeSH terms ‘Alzheimer disease/diagnosis’ [Mesh] AND ‘sensitivity and specificity’ [Mesh] AND (imaging OR biomarkers) and (‘dementia/diagnosis’ [Mesh] AND ‘biological markers/cerebrospinal fluid’ [Mesh]) OR ‘AD/diagnosis’ [Mesh]) AND ‘([beta or amyloid] adj2 42). mp.OR (amyloid adj2 [beta or 42]).mp.)’ in Ovid-EMBASE (S1 Table). All 369 abstracts were reviewed using a combination of the search terms. The Patients—Intervention—Comparators—Outcomes (PICO) and search strategy was drafted. Study groups included patients with suspected mild cognitive impairment and/or AD, and study selection focused on reports that included measurements of Aβ levels. The reference standard was clinical diagnosis with medical results being followed up for more than 1 year. Literature searches using MEDLINE and EMBASE are summarized in S1 Table. One report (Swedish Council on Technology Assessment 2008) was identified by searching the Cochrane Library and other databases for ‘Aβ1–42’.
2. Inclusion and exclusion criteria for selected documents
- Inclusion criteria
- Research on mild cognitive impairment (MCI) or patients with suspected or confirmed AD
- Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV)[12]for MCI and Other dementia
- Studies using Aβ1–42 testing
- Comparative research using appropriate tests
- For predictive accuracy of reporting, studies with more than 1 year follow-up
- Research paper using appropriate inspection techniques (eg, diagnostic tools as ELISA immunoassay, amyloid PET, biopsy or autopsy)
- Research paper since 2004
- Exclusion criteria
- Reports restricted to treatment or preclinical animal studies
- Unpublished studies
- Non-research articles (non-systematic reviews, editorials, letters, comments, opinion pieces, congress or conference material, guidelines, notes, news articles, abstracts)
- Studies published only as abstracts or case reports
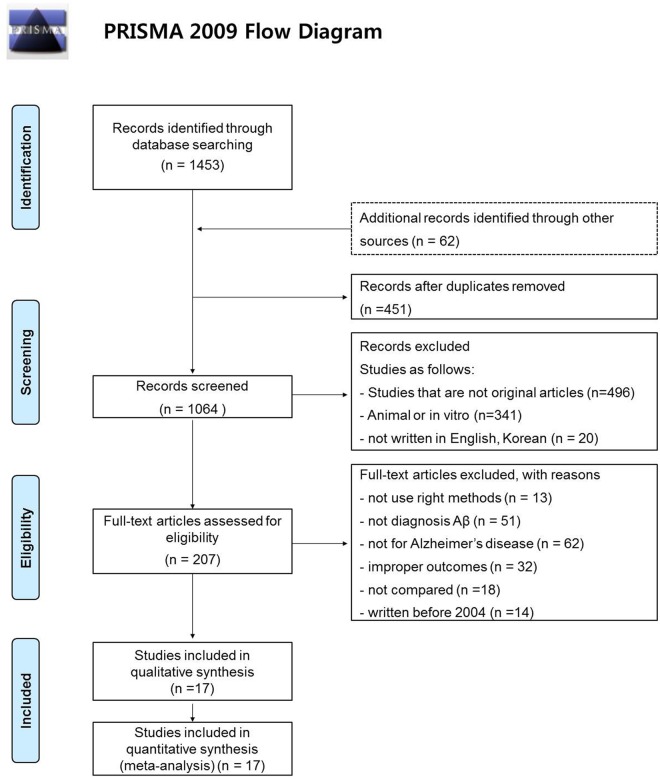
Searching through the literature identified 1515 documents; a further 62 documents were identified using hand searching. Among these, 1097 documents met our exclusion criteria. 451duplicated data from other reports were also excluded. A total of 17studies were included in the final evaluation (Fig. 1).
Fig 1. Literature search algorithm.
Searching through the literature identified 1515 documents; a further 62 documents were identified using hand searching. Of these, 1097 documents met our exclusion criteria. 451documents duplicated data from other reports and were also excluded. A total of 17studieswere included in the final evaluation.
3. Quality of documents
The quality assessment tool selected for literature selection was adopted from the UK Scottish Intercollegiate Guidelines (SIGN) ‘Methodology Checklist’ (2004 March). SIGN is a systematic evaluation tool for the quality of the original literature and divides reports into randomized controlled trials, cohort studies, case—control studies, diagnostic assessments, and economic evaluation studies. Most of the literature on health technology assessment comprises non-randomized clinical trials and observational studies, and selection criteria were adapted accordingly (Table 1). Each stage of categorization was performed independently by two evaluators; their joint recommendations graded reports as summarized in Table 2. The present study excluded ‘The Swedish Council on Technology Assessment in Health Care Study’ in view of limitations as follows: (i) the study did not fulfil PICO standards; (ii) database searching was based on the references of pre-selected literature; (iii) the study included diverse controls ranging from non-AD dementias to other psychiatric or neurological disorders.
Table 1. Levels of Evidence (SIGN 50).
| 1++ | High-quality meta-analyses, systematic reviews of RCTs, or RCTs with a very low risk of bias |
| 1+ | Well-conducted meta-analyses, systematic reviews, or RCTs with a low risk of bias |
| 1- | Meta-analyses, systematic reviews, or RCTs with a high risk of bias |
| 2++ | High-quality systematic reviews of case—control or cohort studies High-quality case—control or cohort studies with a very low risk of confounding or bias and a high probability that the relationship is causal |
| 2+ | Well-conducted case—control or cohort studies with a low risk of confounding or bias and a moderate probability that the relationship is causal |
| 2- | Case—control or cohort studies with a high risk of confounding or bias and a significant risk that the relationship is not causal |
| 3 | Non-analytic studies, e.g., case reports, case series |
| 4 | Expert opinion |
Abbreviation: RCT, randomized controlled trial.
Table 2. Grades of Recommendations (Health Insurance Review Agency 2005)[15].
| A | At least one meta-analysis, systematic review, or RCT rated as 1++, and directly applicable to the target population; or a body of evidence consisting principally of studies rated as 1+, directly applicable to the target population, and demonstrating overall consistency of results |
| B | A body of evidence including studies rated as 2++, directly applicable to the target population, and demonstrating overall consistency of results; or extrapolated evidence from studies rated as 1++ or 1+ |
| C | A body of evidence including studies rated as 2+, directly applicable to the target population and demonstrating overall consistency of results; or extrapolated evidence from studies rated as 2++ |
| D | Evidence level 3 or 4; or extrapolated evidence from studies rated as 2+ |
4. Data Extraction
Because documents put forward for evaluation comprised more than one type of study, data extraction was repeated several times and analyzed by two evaluators. Selection and categorization were performed in consultation with other researchers who advised on problem resolution. The data were then categorized according to type of data, study characteristics, and the reliability of the techniques employed. Final extraction of data from validated primary sources was performed by two evaluators.
5. Statistical Analyses
Funnel plot was used to address publication bias. Sensitivity testing was also conducted to assess the magnitude of publication bias, which was determined using a fail-safe number, defined as the minimum number of patients with non- significant findings that are needed to overturn the conclusion of a meta-analysis [13–15]. Larger fail-safe numbers indicate that the results are less prone to publication bias. For each outcome we tested the heterogeneity of results across the studies using “I2”. If significant heterogeneity was observed (p<.10), a random effects model-which assigns a weight to each study based on individual study variance as well as between study variance- was used to pool the results together. Also Mann-Whitney test was used to compare numerical values of β-amyloid levels between different reports in same disease categories (χ2). Confidence intervals were determined using the means and standard deviations reported in each document. Meta-analysis was performed to assess the overall diagnostic accuracy of the pooled reports based on the random effects model. In addition, the fail-safe Number was calculated manually with EXCEL, suggested by Corwin [16]. SPSS (Statistical Package for the Social Sciences) 21.0 (SPSS/IBM Inc, New York) was used to recalculate the reported the χ2 values. Revman 5.0 Meta DiSc 1.4 version (Hospital Universtario Ramony Cajal, Madrid, Spain) was subsequently used for meta-analysis of the entire dataset.
Results
Following systematic analysis of the literature and retrieval of primary data, meta-analysis was performed on eleven robust studies that compared Aβ1–42 levels in AD (n = 2211) with healthy individuals (n = 1030), 10 studies that compared AD with non-AD dementias (n = 627), and five studies that compared a-MCI (amnestic mild cognitive impairment) (n = 1133) with na-MCI (non-amnestic mild cognitive impairment) subjects (n = 1276). The present evaluation is therefore based on the results of 17 published studies (Fig. 1). The primary documents and the extracted data are listed in Table 3. All selected paper used ELISA Kit of Innotest kind as a test tools, despite not limited to scan tool and the type of the selected documents. Range of test was 125 ~ 2000pg/mL, respectively and threshold was varied from 290 to 679pg/mL according to each document.
Table 3. Selected Documents Reporting CSF Aβ1–42 Measurements in AD and MCI.
| First author | Publication year | Patients | Aβ1–42 | N | Age | MMSE | Cutting point | TP | FP | FN | TN | Level of evidence | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | |||||||||||||
| Vos [34] | 2013 | a-MCI | 550 | 267 | 399 | 70.7±7.8 | 26.5±2.5 | 500 | - | - | - | - | 2++ | |
| na-MCI | 624 | 283 | 226 | 70.7±7.6 | 27.5±2.1 | - | - | - | - | |||||
| Dumurgier [35] | 2013 | AD | 426.8 | 119.5 | 515 | 71.5±9.5 | 18.8±6.2 | Reference | 2++ | |||||
| Other | 605.9 | 260.6 | 365 | 66.7±11.4 | 21.6±0.0 | 515 | 99 (52.1) | 19 (10.0) | 37 (19.5) | 35 (18.4) | Paris | |||
| 368 | 207 (49.3) | 38 (9.0) | 85 (20.2) | 90 (21.5) | Lilly | |||||||||
| 582 | 115 (33.8) | 68 (20.0) | 42 (12.4) | 115 (33.8) | Mong | |||||||||
| Park [36] | 2013 | AD | 194 | 88.7 | 17 | 59.0±8.0 | 15.0±7.0 | 290 | Reference | 2++ | ||||
| Other | 184.5 | 121 | 9 | 70.0±9.0 | 18.0±8.0 | - | - | - | - | |||||
| Control | 383.5 | 101.8 | 12 | 63.0±9.0 | 28.0±1.0 | 15 (51.7) | 2 (6.9) | 2 (6.9) | 10 (34.5) | |||||
| Reijn [37] | 2007 | AD | 401 | 74 | 69 | 69.0±0.0 | 20.5±0.0 | 67 | Reference | 2++ | ||||
| Other | 570 | 238.5 | 26 | 69.5±0.0 | 21.5±0.0 | 60 (63.2) | 10 (10.5) | 9 (9.5) | 16 (16.8) | |||||
| Control | 810 | 170 | 55 | 59.0±0.0 | - | 59 (47.6) | 9 (7.3) | 10 (8.1) | 46 (37.0) | |||||
| Lewczuk [38] | 2004 | AD | 370.5 | 75.5 | 22 | 68.0±0.0 | 14.0±0.0 | 550 | Reference | 2++ | ||||
| Other | 650 | 357.5 | 11 | 75.0±0.0 | 22.0±0.0 | 19 (57.6) | 2 (6.1) | 3 (11.0) | 9 (25.3) | |||||
| Control | 865 | 256 | 35 | 61.0±0.0 | - | 22 (38.6) | 6 (10.5) | 0 (0) | 29 (50.9) | |||||
| Schoonenboom [39] | 2004 | AD | 307 | 200.5 | 47 | 59.0±0.0 | 20.0±0.0 | 413 | Reference | 2++ | ||||
| Other | 603 | 413.5 | 28 | 60.0±0.0 | 25.0±0.0 | 40 (53.3) | 7 (9.3) | 7 (9.3) | 21 (28.1) | |||||
| Control | 604 | 443.5 | 21 | 62.0±0.0 | 29.0±0.0 | 40 (58.8) | 1 (1.5) | 7 (10.3) | 20 (29.4) | |||||
| Le Bastard [40] | 2013 | AD | 355 | 353 | 51 | 75.0±13.0 | 11.0±7.0 | 539 | Reference | 2+ | ||||
| Other | 610 | 406 | 95 | 72.0±10.0 | 10.0±9.0 | 43 (29.5) | 26 (17.8) | 8 (5.5) | 69 (47.2) | |||||
| Control | 699 | 417 | 95 | 47.0±17.0 | - | 48 (32.8) | 11 (7.5) | 3 (2.1) | 84 (57.6) | |||||
| Buchhave [41] | 2009 | AD | 296 | 211.5 | 529 | 74.0±7.2 | 20.4±5.6 | - | - | - | - | - | 2+ | |
| Control | 651 | 168 | 34 | 72.0±8.3 | 28.7±1.2 | - | - | - | - | |||||
| Mattsson [42] | 2009 | AD | 370 | 211.5 | 529 | 71.0±0.0 | 22.0±0.0 | 482 | Reference | 2+ | ||||
| a-MCI | 356 | 163.1 | 271 | 72.0±0.0 | 27.0±0.0 | 223 (29.8) | 134 (17.9) | 47 (6.3) | 345 (46.0) | |||||
| na-MCI | 579 | 216.5 | 479 | 68.0±0.0 | 27.0±0.0 | - | - | - | - | |||||
| Control | 675 | 285.8 | 304 | 67.0±0.0 | 29.0±0.0 | - | - | - | - | |||||
| Smach [43] | 2009 | AD | 400 | 370 | 73 | 73.0±0.0 | 14.0±0.0 | 505 | Reference | 2+ | ||||
| Other | 680 | 315 | 35 | 69.0±0.0 | 18.0±0.0 | 60 (55.5) | 10 (93) | 13 (12.0) | 25 (23.2) | |||||
| Control | 1020 | 230 | 38 | 72.0±0.0 | 28.0±0.0 | 60 (54.1) | 3 (2.7) | 13 (11.7) | 35 (31.5) | |||||
| Herukka [44] | 2008 | a-MCI | 392 | 154 | 13 | - | - | 450 | Reference | 2+ | ||||
| na-MCI | 670 | 249 | 8 | - | - | 6 (28.6) | 2 (9.5) | 2 (9.5) | 11 (52.4) | |||||
| Kapaki [45] | 2007 | AD | 422 | 149 | 67 | 66.0±10.0 | 18.0±0.0 | 61 | Reference | 2+ | ||||
| Other | 400 | 219 | 18 | 69.0±14.0 | 21.0±0.0 | 61 (71.8) | 10 (11.8) | 6 (0.7) | 8 (15.7) | |||||
| Control | 721 | 228 | 72 | 64.0±11.0 | 29.0±0.0 | 48 (35.3) | 8 (5.9) | 19 (13.7) | 61 (45.1) | |||||
| Kapaki [46] | 2005 | AD | 387 | 77 | 33 | 63.0±11.0 | 23.0±0.0 | 562 | Reference | 2+ | ||||
| Other | 800 | 174 | 20 | 60.0±12.0 | 25.0±0.0 | 28 (52.8) | 4 (7.5) | 5 (9.4) | 16 (30.3) | |||||
| Control | 736 | 157 | 50 | 62.0±12.0 | 29.0±0.0 | 23 (27.7) | 6 (7.2) | 10 (12.0) | 44 (53.0) | |||||
| Stefani [47] | 2005 | AD | 396 | 397.5 | 66 | 72.2±8.1 | 18.2±1.7 | 493 | Reference | 2+ | ||||
| Other | 787 | 434 | 20 | 73.6±6.8 | 20.1±2.0 | 58 (67.4) | 8 (9.3) | 8 (9.3) | 12 (14.0) | |||||
| Hampel [48] | 2005 | a-MCI | 678 | 304 | 52 | 72.8±5.3 | 22.4±5.7 | 679 | Reference | 2+ | ||||
| AD | 545 | 230 | 93 | 72.5±8.3 | 28.9±1.0 | 24 (46.2) | 10 (19.2) | 5 (9.6) | 13 (25.0) | |||||
| Control | 962 | 182 | 10 | 67.7±7.7 | 29.5±0.5 | - | - | - | - | |||||
| Perneczky [49] | 2011 | a-MCI | 622.95 | 275.61 | 21 | 67.9±8.8 | 27.7±0.0 | - | Reference | 2– | ||||
| na-MCI | 789.91 | 38.12 | 35 | 61.9±7.7 | 27.5±0.0 | 17 (30.4) | 7 (12.5) | 4 (7.1) | 28 (50.0) | |||||
| Lewczuk [50] | 2007 | a-MCI | 172.6 | 53.5 | 106 | 67.7±8.2 | - | - | Reference | 2– | ||||
| na-MCI | 228 | 37.35 | 49 | 59.7±8.5 | - | 63 (40.6) | 18 (11.6) | 43 (27.7) | 31 (20.1) | |||||
Abbreviations: a-MCI, amnestic mild cognitive impairment; na-MCI, non-amnestic mild cognitive impairment; AD, Alzheimer’s disease; non-AD, non-AD dementia; N, sample size; TP, True Positive; FP, False Positive; FN, False Negative; TN, True Negative.
*All biochemical measurements, pg/ml
1. Results of systematic literature review
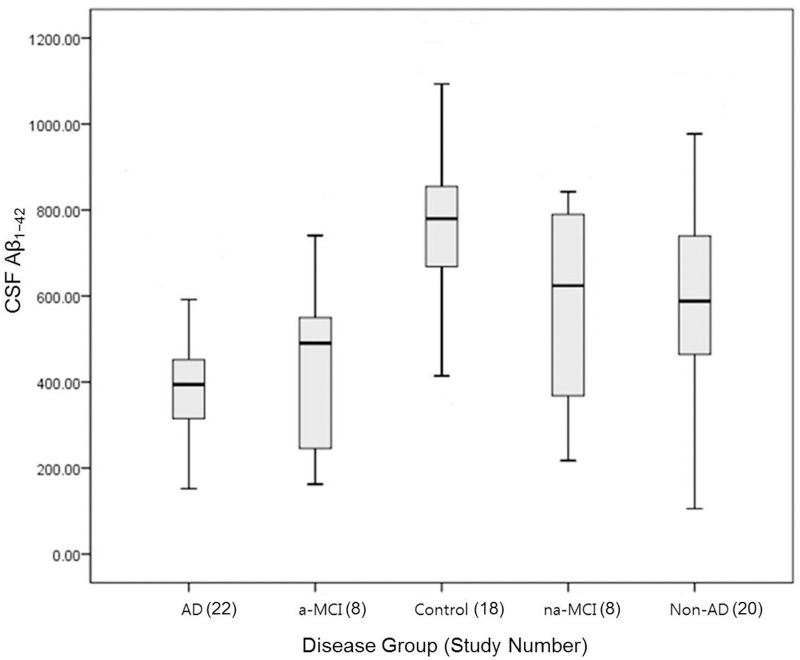
The diagnostic efficacy of CSF Aβ1–42 in AD and healthy controls was reported in eleven documents. CSF Aβ1–42 levels in AD ranged from 194±88.7 to 545±230 pg/ml, whereas levels in the healthy control group ranged from 383.5±101.8 to 1020±230 pg/ml (p <.001) (Figs. 2, 3 and Table 3). Five papers reported diagnostic efficacy of CSF Aβ1–42 for amnestic type MCI (a-MCI) patients and non-amnestic MCI (na-MCI). CSF Aβ1–42 levels ranged from 172.6±53.5 to 622.9±275.6 pg/ml in a-MCI, whereas levels in na-MCI ranged from 228±37.35 to 789.9±38.12 pg/ml (p = .003) (Figs. 2, 3 and Table 3). Diagnostic efficacy of CSF Aβ1–42 in non-AD dementias and AD was reported in 10 studies. CSF Aβ1–42 levels in AD ranged from 194±88.7 to 426.8±119.5pg/ml whereas levels in non-AD dementias ranged from 184.5±121 to 800±174 pg/ml (p <. 0001) (Figs. 2, 3 and Table 3). CSF Aβ1–42 level with 95% confidence intervals in AD was 382.2±102.0 pg/ml (95% CI 336.9–427.4) whereas levels in the healthy control group was 755.6±209.1 pg/ml (95% CI 651.5–859.6). However, CSF Aβ1–42 levels in non-AD (589.0 ± 217.5, 95% CI 105.4–977.2 pg/ml), a-MCI (434.4 ± 200.6, 95% CI 162.4–740.8 pg/ml) and na-MCI (577.9 ± 244.6, 95% CI 217.5–842.5 pg/ml) frequently overlapped (Figs. 2, 3 and Table 3).
Fig 2. CSF Aβ1–42 levels with 95% confidence intervals.
CSF Aβ1–42 levels in AD was 382.2 ± 102.0 pg/ml (95% CI 336.9–427.4) whereas levels in the healthy control group was 755.6 ± 209.1 pg/ml (95% CI 651.5–859.6). However, CSF Aβ1–42 levels in non-AD (589.0 ± 217.5, 95% CI 105.4–977.2 pg/ml), a-MCI (434.4 ± 200.6, 95% CI 162.4–740.8 pg/ml) and na-MCI (577.9 ± 244.6, 95% CI 217.5–842.5 pg/ml) frequently overlapped. Abbreviations: a-MCI, amnestic mild cognitive impairment; na-MCI, non-amnestic mild cognitive impairment; AD, Alzheimer’s disease; non-AD, non-AD dementia.
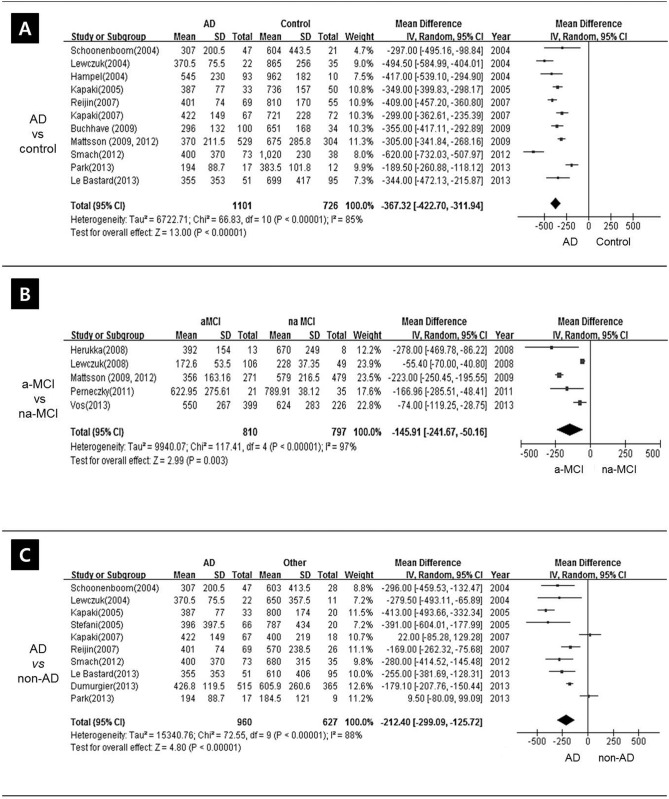
Fig 3. Forest plot of CSF Aβ1–42 levels.
Pooled mean difference (MD) analysis of CSF Aβ1–42 levels revealed that overall levels were significantly lower in AD patients than in healthy controls. However, there was significant heterogeneity and the ranges frequently overlapped. Abbreviations: a-MCI, amnestic mild cognitive impairment; na-MCI, non-amnestic mild cognitive impairment; AD, Alzheimer’s disease; non-AD, non-AD dementia.
2. Meta-analysis
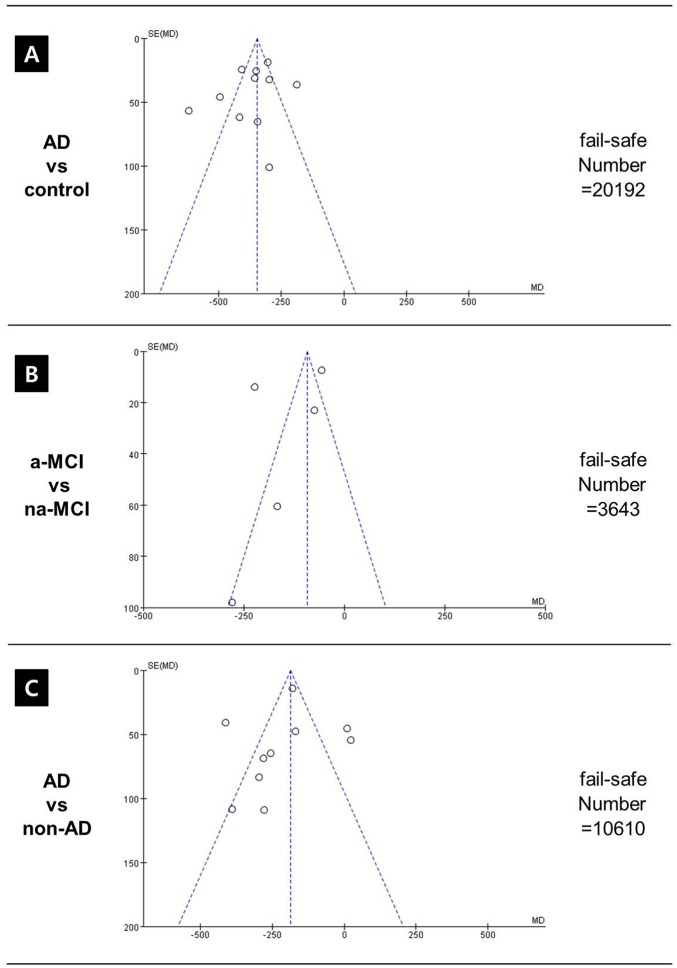
A funnel plot confirming heterogeneity of studies is presented in Fig. 4. Pooled mean difference (MD) analysis of CSF Aβ1–42 levels revealed that overall levels were significantly lower in AD patients than in healthy controls. However, there was significant heterogeneity and the ranges frequently overlapped: pooled MD was -367.32 (95%CI–422.70~–311.94), p < 0.001, I2 = 85%, effect Z = 13.00 (Fig. 3).
Fig 4. A funnel plot confirming heterogeneity of studies.
There was significant heterogeneity between AD and healthy controls. Abbreviations: a-MCI, amnestic mild cognitive impairment; na-MCI, non-amnestic mild cognitive impairment; AD, Alzheimer’s disease; non-AD, non-AD dementia.
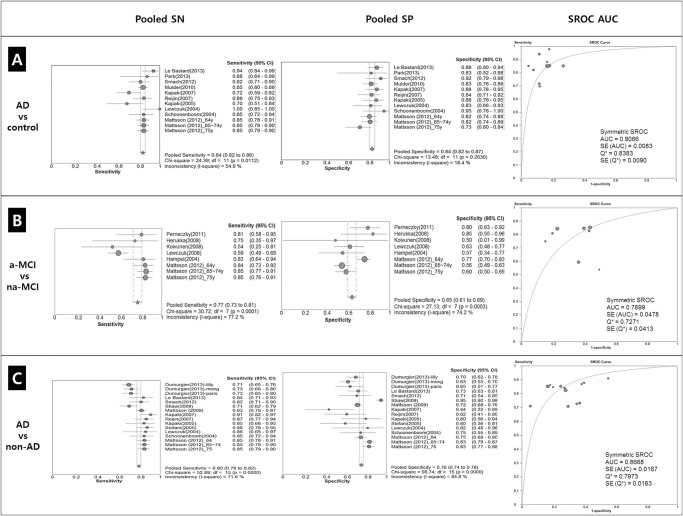
Diagnostic accuracy was evaluated on the basis of ten documents: pooled sensitivity (SN) was 0.84 (95% CI 0.82–0.86), χ2 = 24.39, p = 0.0112, I2 = 54.9%, and pooled specificity (SP) was 0.84 (95% CI 0.82–0.87), χ2 = 13.48, p = 0.2630, I2 = 18.4%. The SROC AUC (Summary Receiver Operating Characteristic Area Under the Curve (SROC AUC) value was 0.9066±0.0083 (Fig. 5).
Fig 5. Forest plot of sensitivities and specificity and Receiver operating characteristics (ROC) curve for AD and control (A).
Diagnostic accuracy was evaluated on the basis of ten documents: pooled sensitivity (SN) was 0.84 (95% CI 0.82–0.86), χ2 = 24.39, p = 0.0112, I2 = 54.9%, and pooled specificity (SP) was 0.84 (95% CI 0.82–0.87), χ2 = 13.48, p = 0.263, I2 = 18.4%. The SROC AUC (Summary Receiver Operating Characteristic Area Under the Curve (SROC AUC) value was 0.9066±0.0083. Forest plot of sensitivities and specificity and Receiver operating characteristics (ROC) curve for a-MCI and na-MCI (B). Diagnostic accuracy was evaluated on the basis of ten documents: pooled sensitivity (SN) was 0.77 (95% CI 0.73–0.81), χ2 = 30.72, p = 0.0001, I2 = 77.2%, and pooled specificity (SP) was 0.65 (95% CI 0.61–0.69), χ2 = 27.13, p = 0.003, I2 = 74.2%. The SROC AUC (Summary Receiver Operating Characteristic Area Under the Curve (SROC AUC) value was 0.7899±0.0478. Forest plot of sensitivities and specificity and Receiver operating characteristics (ROC) curve for AD and non-AD dementia (C). Diagnostic accuracy was evaluated on the basis of ten documents: pooled sensitivity (SN) was 0.80 (95% CI 0.78–0.82), χ2 = 52.88, p = 0.0000, I2 = 71.6%, and pooled specificity (SP) was 0.76 (95% CI 0.74–0.78), χ2 = 98.74, p = 0.0000, I2 = 84.8%. The SROC AUC (Summary Receiver Operating Characteristic Area Under the Curve (SROC AUC) value was 0.8668±0.0167. Abbreviations: AD, Alzheimer’s disease; non-AD, non-AD dementia; df, differences; SROC, Summary Receiver-Operating Characteristic curve; AUC, area under curve; SE, Standard Error; Q*, Heterogeneity statistic.
Pooled MD analysis showed statistically significant higher CSF Aβ1–42 levels in na-MCI compared a-MCI groups, although highly heterogeneity was apparent: pooled MD was -145.91 (95%CI–241.67~–50.16), p = 0.003, I2 = 97%, effect Z = 2.99) (Fig. 3).
The diagnostic accuracy of CSF Aβ1–42 levels was evaluated on the basis of 8published reports. Pooled SN of CSF Aβ1–42 levels was 0.77 (95% CI 0.73–0.81), χ2 = 30.72, p = .0001, I2 = 77.2% and pooled SP was 0.65 (95% CI 0.61–0.69), χ2 = 27.13, p = 0.0003, I2 = 74.2%. The SROC AUC value was 0.7899±0.0478 (Fig. 5)
Pooled MD analysis demonstrated that CSF Aβ1–42 levels were significantly lower in patients with AD versus non-AD dementia, but the results were significantly heterogeneous: the pooled MD was -212.40 (95% CI -299.09~–125.72), p<.00001, I2 = 88%, effect Z = 4.80 (Fig. 3).
Diagnostic accuracy was evaluated based on 16 reports. Pooled SN was 0.80 (95% CI 0.78–0.82), χ2 = 52.88 (p = .0000), I2 = 71.6%, and pooled SP was 0.76 (95% CI 0.74–0.78), χ2 = 98.74 (p = .0000), I2 = 84.8%. The SROC AUC value was 0.8668±0.0167 (Fig. 5).
Additionally, a sub-analysis according to age and MMSE was performed to determine the cause of the heterogeneity within the effect size of the difference between AD and non-AD. There were no significant findings (S1 Fig.).
The diagnostic accuracy of CSF Aβ1–42 levels in a-MCI versus AD, and a-MCI versus healthy controls, was only reported in one document and meta-analysis could therefore not be performed.
Discussion
In this study we have evaluated the clinical utility of CSF Aβ1–42 levels in the diagnosis of AD versus healthy controls and non-AD dementias. Data retrieved from systematic literature review did not identify threshold CSF Aβ1–42 levels that can distinguish between healthy controls and subjects with AD because there was highly significant heterogeneity and the ranges frequently overlapped. The fact that there is not a threshold, in other words a cut off, which can distinguish AD from healthy controls, as well from the other categories analyzed should be highlighted and it is a result of the meta-analysis along with those reported. However, this meta-analysis confirms that, overall, CSF Aβ1–42 levels in AD are significantly lower than in healthy controls.
Although meta-analysis was unable to differentiate reliably between a-MCI and healthy controls, several reports have attested to the clinical utility of CSF Aβ1–42 levels in MCI. Maruyama et al. reported that CSF Aβ1–42 levels did not differ significantly between the healthy control group and MCI [17]. Another study showed the values of CSF Aβ1–42 were significantly lower in the progressive MCI group than in the control subjects and the stable MCI group [18]. CSF Aβ1–42 concentration has a high diagnostic accuracy for correct allocation of AD patients in case—control studies and, together with CSF tau levels, can predict incipient AD in patients with MCI [19]. Values of CSF Aβ1–42 differed according to sample state (fresh versus frozen samples), but overall values were lower in AD patients than in MCI patients [20]. However, a threshold value discriminating between a-MCI and healthy controls could not be established. Instead, other studies have employed the ratio of CSF Aβ1–42 to either Aβ1–40, total tau, or phosphorylated tau as a potential measure of the evolution of MCI to AD [19,21–24].
In the present analysis there were significant differences between the a-MCI and na-MCI groups. CSF Aβ1–42 levels were lower in a-MCI (range 172.6±53.5 to 622.9±275.6 pg/ml) than in na-MCI (range 228.0±37.35 to 789.9±38.12pg/ml), and the pooled MD between groups was significant (pooled MD, 59.77 pg/ml). However, there was highly significant heterogeneity (I2 = 66%), and calculated diagnostic accuracy for MCI alone gave SN and SP values, respectively, of 0.52–0.83 and 0.50–0.84.
Significant discriminatory power was also seen in AD versus non-AD dementia. CSF Aβ1–42 levels in AD (range 194.0±88.7 to 545.0±230.0 pg/ml) were significantly below those reported in non-AD dementia (range 184.5±121.0 to 800.0 ± 174.0 pg/ml). The pooled MD value between groups was significantly lower in AD (pooled MD, 187.21 pg/ml). However, there was also significant heterogeneity (I2 = 66%), and the calculated diagnostic accuracy of AD versus non-AD dementia gave SN and SP values, respectively, of 0.71–0.91 and 0.44–0.82.
These findings may be summarized as follows. First, in patients with probable AD, CSF Aβ1–42 levels are of value in differential diagnosis of AD from other dementias and from healthy controls. The mean concentration of Aβ1–42 in the CSF is significantly reduced by around 50%, in subjects with AD relative to age-matched controls [4,25]. There are debates about whether the Aβ1–42 alone is useful or not in differentiating AD from non-AD dementias including frontotemporal dementia, vascular dementia, and dementia with Lewy bodies (DLB). Because concurrent presence of fibrillar Aβ deposits occurs in the majority of patients with DLB, it is possible that the reduced Aβ1–42 levels in the CSF have also been documented in patients with other dementia [4]. However, meta-analytic study indicates that CSF Aβ1–42 can serve as a diagnostic and surrogate biomarker for Aβ deposition in the brain [26]. Second, the ranges of Aβ1–42 levels partially overlap between AD and a-MCI, and it is therefore not possible to establish a cut-off value that discriminates between the two groups. Moreover, it is possible that a-MCI is an extension of AD pathology, and it has been suggested that a-MCI might be redefined to as a-MCI due to AD [6]. There might be the following several reasons; Some outstanding prospective CSF studies in MCI subjects would be particularly useful to add strength to this claim [27,28]. However, we decided to enroll papers published since 2004, because the criteria for MCI were revised to encompass other patterns of cognitive impairment in addition to memory loss [29]. In this paper we analyzed CSF results according to a-MCI and na-MCI. The other is considerable intra- or inter-laboratory variability of CSF analyses, which may influence the diagnostic classification of dementia according to results of CSF [30]. The intra- and inter-laboratory variability in CSF results from differences in pre-analytical and analytical procedures, lot-to-lot variation of analytical kits, freezing conditions and storage time [31–33]. It is necessary for research community to overcome this confusing situation that CSF variability was largest for Aβ1–42.
In summary, this meta-analysis establishes that reduced Aβ1–42 levels are of diagnostic utility in AD, and relatively high CSF levels of Aβ1–42 are indicative of non-AD pathology (e.g., na-MCI, non-AD dementias). However, CSF Aβ1–42 levels alone are insufficient for reliable differential diagnosis of AD. Further research on the use of combinations of biomarkers, for example Aβ1–42 levels in conjunction with other markers (e.g., total Aβ, Aβ1–40, tau, phosphorylated tau), will be necessary in order to develop CSF biochemical measurements permitting reliable diagnosis of AD versus other non-AD cognitive impairments.
Supporting Information
A sub-analysis according to age and MMSE has performed to determine the cause of the heterogeneity within the effect size of the difference between AD and non-AD. There were no significant findings. Abbreviations: AD, Alzheimer’s disease; non-AD, non-AD dementia.
(TIF)
(DOC)
Literature searches using MEDLINE and EMBASE. Abbreviation: PICO, Patients—Intervention—Comparators—Outcomes.
(DOCX)
Data Availability
All sources are from the database of Korean National Evidence-based Healthcare Collaborating Agency (http://www.neca.re.kr/eng/). Specific locations of the data set are listed in Supporting Information.
Funding Statement
This study was supported by research funds from the Ministry of Health and Welfare. This work was supported by the research fund of Hanyang University (HY-2012). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Aisen PS, Andrieu S, Sampaio C, Carrillo M, Khachaturian ZS, et al. (2011) Report of the task force on designing clinical trials in early (predementia) AD. Neurology 76: 280–286. 10.1212/WNL.0b013e318207b1b9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Golde TE, Schneider LS, Koo EH (2011) Anti-abeta therapeutics in Alzheimer’s disease: the need for a paradigm shift. Neuron 69: 203–213. 10.1016/j.neuron.2011.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cummings JL (2011) Biomarkers in Alzheimer’s disease drug development. Alzheimers Dement 7: e13–44. 10.1016/j.jalz.2010.06.004 [DOI] [PubMed] [Google Scholar]
- 4. Holtzman DM (2011) CSF biomarkers for Alzheimer’s disease: current utility and potential future use. Neurobiol Aging 32 Suppl 1: S4–9. 10.1016/j.neurobiolaging.2011.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Buerger K, Zinkowski R, Teipel SJ, Tapiola T, Arai H, et al. (2002) Differential diagnosis of Alzheimer disease with cerebrospinal fluid levels of tau protein phosphorylated at threonine 231. Arch Neurol 59: 1267–1272. [DOI] [PubMed] [Google Scholar]
- 6. Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, et al. (2011) Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7: 280–292. 10.1016/j.jalz.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bateman RJ, Wen G, Morris JC, Holtzman DM (2007) Fluctuations of CSF amyloid-beta levels: implications for a diagnostic and therapeutic biomarker. Neurology 68: 666–669. [DOI] [PubMed] [Google Scholar]
- 8. Kang JH, Korecka M, Toledo JB, Trojanowski JQ, Shaw LM (2013) Clinical utility and analytical challenges in measurement of cerebrospinal fluid amyloid-beta(1–42) and tau proteins as Alzheimer disease biomarkers. Clin Chem 59: 903–916. 10.1373/clinchem.2013.202937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151: 264–269, w264 [DOI] [PubMed] [Google Scholar]
- 10. McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, et al. (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7: 263–269. 10.1016/j.jalz.2011.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Morris JC, Heyman A, Mohs RC, Hughes JP, van Belle G, et al. (1989) The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology 39: 1159–1165. [DOI] [PubMed] [Google Scholar]
- 12. Cooper JE (1995) On the publication of the Diagnostic and Statistical Manual of Mental Disorders: Fourth Edition (DSM-IV). Br J Psychiatry 166: 4–8. [DOI] [PubMed] [Google Scholar]
- 13. Becher B (2005) Failsafe N or file drawer number In Rothstein H. R., Sutton A. J., & Bornstein M. (Eds.), Publication bias in meta-analysis: Prevention, assessment and adjustment. West Sussez, England: John Wiley & Sons; 14 p. [Google Scholar]
- 14. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR (2010) A basic introduction to fixed-effect and random-effects models for meta-analysis. Research Synthesis Methods 1: 15. [DOI] [PubMed] [Google Scholar]
- 15. Orwin R (1983) A fail-safe N for effect size in meta-analysis. Journal of Educational Statistics 8: 3. [Google Scholar]
- 16. Corwin R (1983) A fail-safe N for effect size in meta-analysis. Journal of Educational Statistics 8: 3. [Google Scholar]
- 17. Maruyama M, Arai H, Sugita M, Tanji H, Higuchi M, et al. (2001) Cerebrospinal fluid amyloid beta(1–42) levels in the mild cognitive impairment stage of Alzheimer’s disease. Exp Neurol 172: 433–436. [DOI] [PubMed] [Google Scholar]
- 18. Herukka SK, Hallikainen M, Soininen H, Pirttila T (2005) CSF Abeta42 and tau or phosphorylated tau and prediction of progressive mild cognitive impairment. Neurology 64: 1294–1297. [DOI] [PubMed] [Google Scholar]
- 19. Hansson O, Zetterberg H, Buchhave P, Londos E, Blennow K, et al. (2006) Association between CSF biomarkers and incipient Alzheimer’s disease in patients with mild cognitive impairment: a follow-up study. Lancet Neurol 5: 228–234. [DOI] [PubMed] [Google Scholar]
- 20. Buerger K, Frisoni G, Uspenskaya O, Ewers M, Zetterberg H, et al. (2009) Validation of Alzheimer’s disease CSF and plasma biological markers: the multicentre reliability study of the pilot European Alzheimer’s Disease Neuroimaging Initiative (E-ADNI). Exp Gerontol 44: 579–585. 10.1016/j.exger.2009.06.003 [DOI] [PubMed] [Google Scholar]
- 21. Hansson O, Zetterberg H, Buchhave P, Andreasson U, Londos E, et al. (2007) Prediction of Alzheimer’s disease using the CSF Abeta42/Abeta40 ratio in patients with mild cognitive impairment. Dement Geriatr Cogn Disord 23: 316–320. [DOI] [PubMed] [Google Scholar]
- 22. Li G, Sokal I, Quinn JF, Leverenz JB, Brodey M, et al. (2007) CSF tau/Abeta42 ratio for increased risk of mild cognitive impairment: a follow-up study. Neurology 69: 631–639. [DOI] [PubMed] [Google Scholar]
- 23. Song MS, Mook-Jung I, Lee HJ, Min JY, Park MH (2007) Serum anti-amyloid-beta antibodies and Alzheimer’s disease in elderly Korean patients. J Int Med Res 35: 301–306. [DOI] [PubMed] [Google Scholar]
- 24. Mitchell AJ (2009) CSF phosphorylated tau in the diagnosis and prognosis of mild cognitive impairment and Alzheimer’s disease: a meta-analysis of 51 studies. J Neurol Neurosurg Psychiatry 80: 966–975. 10.1136/jnnp.2008.167791 [DOI] [PubMed] [Google Scholar]
- 25. Motter R, Vigo-Pelfrey C, Kholodenko D, Barbour R, Johnson-Wood K, et al. (1995) Reduction of beta-amyloid peptide42 in the cerebrospinal fluid of patients with Alzheimer’s disease. Ann Neurol 38: 643–648. [DOI] [PubMed] [Google Scholar]
- 26. Agarwal R, Tripathi CB (2011) Diagnostic Utility of CSF Tau and Abeta(42) in Dementia: A Meta-Analysis. Int J Alzheimers Dis 2011: 503293 10.4061/2011/503293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Andreasen N, Minthon L, Vanmechelen E, Vanderstichele H, Davidsson P, et al. (1999) Cerebrospinal fluid tau and Abeta42 as predictors of development of Alzheimer’s disease in patients with mild cognitive impairment. Neurosci Lett 273: 5–8. [DOI] [PubMed] [Google Scholar]
- 28. Andreasen N, Vanmechelen E, Vanderstichele H, Davidsson P, Blennow K (2003) Cerebrospinal fluid levels of total-tau, phospho-tau and A beta 42 predicts development of Alzheimer’s disease in patients with mild cognitive impairment. Acta Neurol Scand Suppl 179: 47–51. [DOI] [PubMed] [Google Scholar]
- 29. Winblad B, Palmer K, Kivipelto M, Jelic V, Fratiglioni L, et al. (2004) Mild cognitive impairment—beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Intern Med 256: 240–246. [DOI] [PubMed] [Google Scholar]
- 30. Vos SJ, Visser PJ, Verhey F, Aalten P, Knol D, et al. (2014) Variability of CSF Alzheimer’s disease biomarkers: implications for clinical practice. PLoS One 9: e100784 10.1371/journal.pone.0100784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. del Campo M, Mollenhauer B, Bertolotto A, Engelborghs S, Hampel H, et al. (2012) Recommendations to standardize preanalytical confounding factors in Alzheimer’s and Parkinson’s disease cerebrospinal fluid biomarkers: an update. Biomark Med 6: 419–430. 10.2217/bmm.12.46 [DOI] [PubMed] [Google Scholar]
- 32. Schoonenboom NS, Mulder C, Vanderstichele H, Van Elk EJ, Kok A, et al. (2005) Effects of processing and storage conditions on amyloid beta (1–42) and tau concentrations in cerebrospinal fluid: implications for use in clinical practice. Clin Chem 51: 189–195. [DOI] [PubMed] [Google Scholar]
- 33. Vanderstichele H, Bibl M, Engelborghs S, Le Bastard N, Lewczuk P, et al. (2012) Standardization of preanalytical aspects of cerebrospinal fluid biomarker testing for Alzheimer’s disease diagnosis: a consensus paper from the Alzheimer’s Biomarkers Standardization Initiative. Alzheimers Dement 8: 65–73. 10.1016/j.jalz.2011.07.004 [DOI] [PubMed] [Google Scholar]
- 34. Vos SJ, van Rossum IA, Verhey F, Knol DL, Soininen H, et al. (2013) Prediction of Alzheimer disease in subjects with amnestic and nonamnestic MCI. Neurology 80: 1124–1132. 10.1212/WNL.0b013e318288690c [DOI] [PubMed] [Google Scholar]
- 35. Dumurgier J, Gabelle A, Vercruysse O, Bombois S, Laplanche JL, et al. (2013) Exacerbated CSF abnormalities in younger patients with Alzheimer’s disease. Neurobiol Dis 54: 486–491. 10.1016/j.nbd.2013.01.023 [DOI] [PubMed] [Google Scholar]
- 36. Park SA, Kim JH, Kim HJ, Kim TE, Kim YJ, Lee DH, et al. (2013) Preliminary Study for a Multicenter Study of Alzheimer’s Disease Cerebrospinal Fluid Biomarkers Dementia and Neurocognitive Disorders 12: 1–8. [Google Scholar]
- 37. Reijn TS, Rikkert MO, van Geel WJ, de Jong D, Verbeek MM (2007) Diagnostic accuracy of ELISA and xMAP technology for analysis of amyloid beta(42) and tau proteins. Clin Chem 53: 859–865. [DOI] [PubMed] [Google Scholar]
- 38. Lewczuk P, Esselmann H, Otto M, Maler JM, Henkel AW, et al. (2004) Neurochemical diagnosis of Alzheimer’s dementia by CSF Abeta42, Abeta42/Abeta40 ratio and total tau. Neurobiol Aging 25: 273–281. [DOI] [PubMed] [Google Scholar]
- 39. Schoonenboom NS, Pijnenburg YA, Mulder C, Rosso SM, Van Elk EJ, et al. (2004) Amyloid beta(1–42) and phosphorylated tau in CSF as markers for early-onset Alzheimer disease. Neurology 62: 1580–1584. [DOI] [PubMed] [Google Scholar]
- 40. Le Bastard N, Coart E, Vanderstichele H, Vanmechelen E, Martin JJ, et al. (2013) Comparison of two analytical platforms for the clinical qualification of Alzheimer’s disease biomarkers in pathologically-confirmed dementia. J Alzheimers Dis 33: 117–131. 10.3233/JAD-2012-121246 [DOI] [PubMed] [Google Scholar]
- 41. Buchhave P, Blennow K, Zetterberg H, Stomrud E, Londos E, et al. (2009) Longitudinal study of CSF biomarkers in patients with Alzheimer’s disease. PLoS One 4: e6294 10.1371/journal.pone.0006294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mattsson N, Zetterberg H, Hansson O, Andreasen N, Parnetti L, et al. (2009) CSF biomarkers and incipient Alzheimer disease in patients with mild cognitive impairment. JAMA 302: 385–393. 10.1001/jama.2009.1064 [DOI] [PubMed] [Google Scholar]
- 43. Smach MA, Charfeddine B, Ben Othman L, Lammouchi T, Dridi H, et al. (2009) Evaluation of cerebrospinal fluid tau/beta-amyloid(42) ratio as diagnostic markers for Alzheimer disease. Eur Neurol 62: 349–355. 10.1159/000241881 [DOI] [PubMed] [Google Scholar]
- 44. Herukka SK, Pennanen C, Soininen H, Pirttila T (2008) CSF Abeta42, tau and phosphorylated tau correlate with medial temporal lobe atrophy. J Alzheimers Dis 14: 51–57. [DOI] [PubMed] [Google Scholar]
- 45. Kapaki EN, Paraskevas GP, Tzerakis NG, Sfagos C, Seretis A, et al. (2007) Cerebrospinal fluid tau, phospho-tau181 and beta-amyloid1–42 in idiopathic normal pressure hydrocephalus: a discrimination from Alzheimer’s disease. Eur J Neurol 14: 168–173. [DOI] [PubMed] [Google Scholar]
- 46. Kapaki E, Liappas I, Paraskevas GP, Theotoka I, Rabavilas A (2005) The diagnostic value of tau protein, beta-amyloid (1–42) and their ratio for the discrimination of alcohol-related cognitive disorders from Alzheimer’s disease in the early stages. Int J Geriatr Psychiatry 20: 722–729. [DOI] [PubMed] [Google Scholar]
- 47. Stefani A, Bernardini S, Panella M, Pierantozzi M, Nuccetelli M, et al. (2005) AD with subcortical white matter lesions and vascular dementia: CSF markers for differential diagnosis. J Neurol Sci 237: 83–88. [DOI] [PubMed] [Google Scholar]
- 48. Hampel H, Teipel SJ, Fuchsberger T, Andreasen N, Wiltfang J, et al. (2004) Value of CSF beta-amyloid1–42 and tau as predictors of Alzheimer’s disease in patients with mild cognitive impairment. Mol Psychiatry 9: 705–710. [DOI] [PubMed] [Google Scholar]
- 49. Perneczky R, Tsolakidou A, Arnold A, Diehl-Schmid J, Grimmer T, et al. (2011) CSF soluble amyloid precursor proteins in the diagnosis of incipient Alzheimer disease. Neurology 77: 35–38. 10.1212/WNL.0b013e318221ad47 [DOI] [PubMed] [Google Scholar]
- 50. Lewczuk P, Kornhuber J, Vanderstichele H, Vanmechelen E, Esselmann H, et al. (2008) Multiplexed quantification of dementia biomarkers in the CSF of patients with early dementias and MCI: a multicenter study. Neurobiol Aging 29: 812–818. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A sub-analysis according to age and MMSE has performed to determine the cause of the heterogeneity within the effect size of the difference between AD and non-AD. There were no significant findings. Abbreviations: AD, Alzheimer’s disease; non-AD, non-AD dementia.
(TIF)
(DOC)
Literature searches using MEDLINE and EMBASE. Abbreviation: PICO, Patients—Intervention—Comparators—Outcomes.
(DOCX)
Data Availability Statement
All sources are from the database of Korean National Evidence-based Healthcare Collaborating Agency (http://www.neca.re.kr/eng/). Specific locations of the data set are listed in Supporting Information.