Abstract
Context: Vitamin D inadequacy is a global problem and it is one of the most common endocrine diseases world-wide. In this review article, we covered the important practical clinical issues for screening, prevention and treatment of vitamin D deficiency in adults as well as during pregnancy and lactation.
Keywords: Adults, deficiency, insufficiency, lactation, pregnancy, vitamin D
Introduction
Vitamin D deficiency was first described as an entity in the middle of the 17th century. In AD 1700, Lambert wrote about it[1,2] and in 1885 Pommer stressed on the fact that Vitamin D deficiency should be regarded as a clinical entity of its own.[3]
Vitamin D inadequacy is a health issue of concern especially in India and North China.[4] It used to be almost endemic among Saudis[5] and in other Arab countries or even more culturally conservative groups like orthodox Jewish communities, Amish communities in the US.[6] Several factors, such as lack of exposure to adequate sunlight, insufficient dietary intake and supplementation are associated with the development of deficiencies in vitamin D. Other factors include obesity, age, covering of the skin with clothing, skin pigmentation and use of certain medications and sunscreen chemicals.[7] fortunately, vitamin D supplements can be found in the most drug stores everywhere and they are relatively inexpensive. Even more common is subclinical vitamin D deficiency, which has been documented in several studies conducted in Saudi patients.[8,9] It was shown that low vitamin D levels were more common in women who tended to avoid sunlight and remained entirely covered outdoors due to excessive heat and for socio-cultural reasons. A great proportion of Arabs and Muslim populations wears headgear and Muslim women in particular adhere to a strict dress code; the women always wear clothing that cover most of their bodies. These practices impose an extra burden on the calcium balance of the women, who in addition have disturbances in the calcium balance brought about by multiple parity and prolonged breast feeding. These altogether make vitamin D deficiency a common problem in Saudi Arabia as well all over the Arab and Muslim countries.[10,11]
Vitamin D Metabolism
Vitamin D3 (cholecalciferol) is synthesized non-enzymatically from 7-dehydrocholesterol during exposure of the skin to ultraviolet (UV) rays in sunlight [Figure 1]. Deficiencies in vitamin D can occur when there is an unusual limited exposure to sunlight in addition to lack of vitamin D-rich foods or malabsorption.[12] On the other hand, the conversion of vitamin D into the physiologically active form can be precluded by impaired hydroxylation of the vitamin in the liver.
Figure 1.
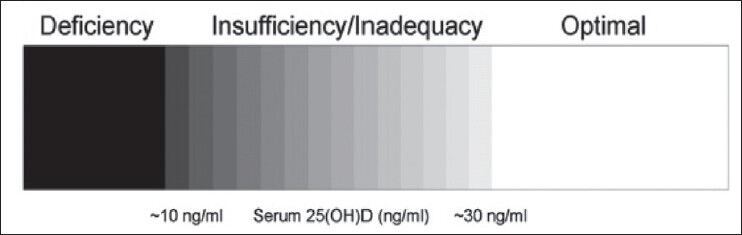
Spectrum of vitamin D status
Vitamin D Deficiency
Vitamin D deficiency can be simply classified as extrinsic or intrinsic. Extrinsic vitamin D deficiency is caused by a combination of decreased endogenous skin synthesis and decreased dietary intake (considered a non-significant factor in the etiology) while intrinsic vitamin D deficiency is caused by a combination of impaired intestinal absorption and increased catabolism, usually triggered by calcium malabsorption.[13] The most common form of nutritional bone disease is nutritional vitamin D deficiency, which is more frequent in parous women. It is characterized by an abnormal mineralization of the newly synthesized organic matrix of bone and it occurs due to inadequate exposure to sunlight in the women whose bone, minerals and vitamin D stores had been depleted.[14]
General Clinical Manifestations
The most common early symptoms of vitamin D deficiency in men and women are lower back pain, bone pain and tenderness, weakness of the muscles, difficulties in moving as well as mounting stairs, inability to stand up without assistance, typical duck-like tottering gait and tetany. It has been shown that secondary hyperparathyroidism and decreased bone mass density can result from insufficient vitamin D. Other conditions such as osteoporosis and increased risk of fragility fractures may occur as a result of inadequate vitamin D levels.[15,16,17]
Impaired mineralization and increased parathyroid hormone (PTH) secretion are known to cause bone changes that are observed radiologically. The presence of Looser's zones, which appear as lucent bands perpendicular to the periosteum, are the most recognized radiographic feature of osteomalacia [Figure 2]. These bands usually develop in the outer border of the scapulae, ribs, pubic rami, femoral neck and to a lesser extent in the metacarpals and shafts of the long bones.[18] Clinically, patients usually complain of local tenderness and pain on movement. Other features that are associated with Looser's zones are symmetrical vertebral biconcavity and evidence of high bone turnover. An unspecific finding is the reduction in bone density. In general, true factures, fractures of the femur and compression fractures of the vertebral column do not occur in patients with vitamin D deficiency unless complicated by conditions like tertiary hyperparathyroidism with osteitis fibrosa.[19]
Figure 2.

(a and b) Images of Looser zones
Definition of vitamin D deficiency and vitamin D insufficiency
In practice, severe vitamin D deficiency is defined as serum 25-hydroxyvitamin D (25(OH)D) concentrations <10 ng/mL and may sustain impaired bone mineralization (rickets/osteomalacia), while those with a value less than approximately 30 ng/mL are identified as insufficient[20] and may sustain long-term adverse health consequences. The minimum optimum level of vitamin D is in general 30-32 ng/mL.[21]
Indications for vitamin D testing
In the clinical setting, it is necessary to measure serum 25(OH)D levels in particular groups of patients to confirm the diagnosis of vitamin D deficiency. It seems reasonable to measure 25(OH)D in those identified as being at high risk of vitamin D deficiency and those for whom a prompt musculoskeletal features such as bone pain, decreased serum calcium or phosphorus levels and high serum alkaline phosphatase or PTH. In elderly patients and in those with osteoporosis or those who have an increased risk of falls or fractures, it may also be beneficial to measure 25(OH)D levels.[22] Groups with increased risk of vitamin D deficiency such as patients with malabsorption (e.g., celiac disease, radiation enteritis, bariatric surgery and so forth), individuals with liver disease and those requiring medications known to alter vitamin D status, for example, certain anticonvulsants. Given the relationship of low vitamin D status with cancer, it also seems rational to measure 25(OH)D in those with malignancy.[23] Nevertheless, one could argue that testing for vitamin D insufficiency may be pointless in persons who are at risk of developing deficiencies if they are receiving adequate doses of vitamin D supplements. At present, there is no evidence that it is beneficial to screen asymptomatic individuals for 25(OH)D deficiency.
Prevention of vitamin D deficiency
Box 1 shows a summary of the recommendations for the prevention and management of vitamin D deficiency. The prescription of vitamin D supplements is estimated to prevent deficiencies in about 98% of the general population. It has been shown that serum 25(OH)D levels in elderly patients increase after supplementation with vitamin D and sunlight exposure or exposure to virtual sunlight rays.[24] According to the Institute of Medicine, the recommended dosage of vitamin D in the United States and Canada is 200 IU/day for all children and adults less than 51-year-old, 400 IU/day for people 51-70 years old and 600 IU/day for individuals above the age of 70 years.[25] The United States Food and Drug Administration recommends a daily dose of 400 IU (10 μg/day) of vitamin D3 irrespective of the age because some authors suggested that doses of up to 1000 IU/day of vitamin D3 and intake of 400 IU/day may represent the least amounts required in the prevention of vitamin D deficiency. This is especially true in children and adults who are not exposed to sunlight like is the case during winter.[26]
Treatment of severe vitamin D deficiency
Severe vitamin D deficiency is far less common than inadequacy. However, it does occur, especially in elderly people who are housebound. Several treatment plans have been proposed, but so far the most efficient method for treating vitamin D deficiency is an oral dose of 50,000 IU/week of vitamin D2 or ergocalciferol for 8 weeks, then checking the concentrations of 25(OH)D after 3 months. In some cases, the prescription of another dose of 50,000 IU of vitamin D2 once weekly for 8 weeks may be necessary to increase the serum 25(OH)D concentrations to the desired range of greater than 30-50 ng/mL (75-125 nmol/L).[27]
After correcting the deficiency in patients who are susceptible to developing vitamin D deficiency, physicians should prescribe cholecalciferol (vitamin D3), which is longer half-life, greater activity, at a dose of 50,000 IU every 2 weeks in order to maintain them in a vitamin D–sufficient state. Alternatively, an intake of vitamin D3 at a dose of 1000 IU should be maintained.[28,29] Cutaneous exposure to sunlight or artificial UV-B radiation is also beneficial, particularly if the patient is susceptible to developing a deficiency in vitamin D. Exposure of the arms and legs to direct sunlight for a maximum of 5-10 min between 10 AM and 3 PM during spring, summer and autumn will prevent vitamin D inadequacy.[30] There are no reports of vitamin D toxicity due to long-term exposure to sunlight; this has only resulted from dietary intake when the doses of vitamin D were greater than 10,000 IU/day. No cases of toxicity have also been observed when vitamin D was administered at doses of 4000 IU/day for 3 months and 50,000 IU/week for 2 months.[31,32]
Vitamin D recommendations for pregnant and lactating women
Vitamin D dosing recommendations for pregnant women should be aimed at preventing problems in neonates and infants and a vitamin dose sufficient for the mother during pregnancy should be such that the cord blood 25(OH)D level is normal at birth. Pregnant women should be encouraged to take 4,000 IU/day 2 and lactating women at least 4,000 IU/day. These doses are necessary to raise maternal milk vitamin D levels in the adequate range so that the infant is ingesting at least 400 IU/L breast milk.[33,34]
The alternative give the lactating woman enough vitamin D so that the total circulating 25(OH)D level is no less than 80 nmol/L or 32 ng/mL and to give her breastfeeding infant the time-honored 400 IU vitamin D/day. With the latter scenario, the normal vitamin D status would be attained in both mother and infant. The shortcoming is that both mother and baby would need to be supplemented.[35]
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Ribemont-Dessaignes A, Lepage G. Paris: 1894. Precis d’obstétrique; p. 931. [Google Scholar]
- 2.Snapper I. New York: 1943. Medical Clinics on Bone Diseases. [Google Scholar]
- 3.Pommer G. Leipzig: 1885. Untersuchungen uber Osteomalacie und Rachitis. [Google Scholar]
- 4.Teotia M, Teotia SP. Highlights of vitamin D deficiency osteomalacia (India) In: Teotia SP, Teotia M, editors. Nutritional and Metabolic Bone and Stone Disease: Asian Perspective. 1st ed. New Delhi: CBS Publishers; 2007. pp. 234–53. [Google Scholar]
- 5.Sedrani SH. Low 25-hydroxyvitamin D and normal serum calcium concentrations in Saudi Arabia: Riyadh region. Ann Nutr Metab. 1984;28:181–5. doi: 10.1159/000176801. [DOI] [PubMed] [Google Scholar]
- 6.Zadshir A, Tareen N, Pan D, Norris K, Martins D. The prevalence of hypovitaminosis D among US adults: Data from the NHANES III. Ethn Dis. 2005;15:S5–97. 101. [PubMed] [Google Scholar]
- 7.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 8.Sedrani SH, Elidrissy AW, El Arabi KM. Sunlight and vitamin D status in normal Saudi subjects. Am J Clin Nutr. 1983;38:129–32. doi: 10.1093/ajcn/38.1.129. [DOI] [PubMed] [Google Scholar]
- 9.Al Faraj S, Al Mutairi K. Vitamin D deficiency and chronic low back pain in Saudi Arabia. Spine (Phila Pa 1976) 2003;28:177–9. doi: 10.1097/00007632-200301150-00015. [DOI] [PubMed] [Google Scholar]
- 10.Al-Jurayyan NA, El-Desouki ME, Al-Herbish AS, Al-Mazyad AS, Al-Qhtani MM. Nutritional rickets and osteomalacia in school children and adolescents. Saudi Med J. 2002;23:182–5. [PubMed] [Google Scholar]
- 11.Dawodu A, Kochiyil J, Altaye N. Pilot study of sunlight exposure and vitamin D status in Arab women of childbearing age. East Mediterr Health J. 2011;17:570–4. [PubMed] [Google Scholar]
- 12.Webb AR, Kline L, Holick MF. Influence of season and latitude on the cutaneous synthesis of vitamin D3: Exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. J Clin Endocrinol Metab. 1988;67:373–8. doi: 10.1210/jcem-67-2-373. [DOI] [PubMed] [Google Scholar]
- 13.Hollis BW. Circulating 25-hydroxyvitamin D levels indicative of vitamin D sufficiency: Implications for establishing a new effective dietary intake recommendation for vitamin D. J Nutr. 2005;135:317–22. doi: 10.1093/jn/135.2.317. [DOI] [PubMed] [Google Scholar]
- 14.Heaney RP, Davies KM, Chen TC, Holick MF, Barger-Lux MJ. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr. 2003;77:204–10. doi: 10.1093/ajcn/77.1.204. [DOI] [PubMed] [Google Scholar]
- 15.Rosen CJ. Clinical practice. Vitamin D insufficiency. N Engl J Med. 2011;364:248–54. doi: 10.1056/NEJMcp1009570. [DOI] [PubMed] [Google Scholar]
- 16.Holick MF. The vitamin D epidemic and its health consequences. J Nutr. 2005;135:2739S–48S. doi: 10.1093/jn/135.11.2739S. [DOI] [PubMed] [Google Scholar]
- 17.Tangpricha V, Pearce EN, Chen TC, Holick MF. Vitamin D insufficiency among free-living healthy young adults. Am J Med. 2002;112:659–62. doi: 10.1016/s0002-9343(02)01091-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cooper C, Javaid K, Westlake S, Harvey N, Dennison E. Developmental origins of osteoporotic fracture: The role of maternal vitamin D insufficiency. J Nutr. 2005;135:2728S–34. doi: 10.1093/jn/135.11.2728S. [DOI] [PubMed] [Google Scholar]
- 19.Gaugris S, Heaney RP, Boonen S, Kurth H, Bentkover JD, Sen SS. Vitamin D inadequacy among post-menopausal women: A systematic review. QJM. 2005;98:667–76. doi: 10.1093/qjmed/hci096. [DOI] [PubMed] [Google Scholar]
- 20.Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet. 1998;351:805–6. doi: 10.1016/s0140-6736(05)78933-9. [DOI] [PubMed] [Google Scholar]
- 21.Glendenning P, Fraser WD. 25-OH-vitamin D assays. J Clin Endocrinol Metab. 2005;90:3129. doi: 10.1210/jc.2004-2399. [DOI] [PubMed] [Google Scholar]
- 22.Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81:353–73. doi: 10.4065/81.3.353. [DOI] [PubMed] [Google Scholar]
- 23.Anonymous. New York: The Bone and Cancer Foundation; 2008. Vitamin D deficiency: Information for cancer patients. [Google Scholar]
- 24.Feskanich D, Willett WC, Colditz GA. Calcium, vitamin D, milk consumption, and hip fractures: A prospective study among postmenopausal women. Am J Clin Nutr. 2003;77:504–11. doi: 10.1093/ajcn/77.2.504. [DOI] [PubMed] [Google Scholar]
- 25.Grant AM, Avenell A, Campbell MK, McDonald AM, MacLennan GS, McPherson GC, et al. Oral vitamin D3 and calcium for secondary prevention of low-trauma fractures in elderly people (randomised evaluation of calcium or vitamin D, RECORD): A randomised placebo-controlled trial. Lancet. 2005;365:1621–8. doi: 10.1016/S0140-6736(05)63013-9. [DOI] [PubMed] [Google Scholar]
- 26.United States Food and Drug Administration Web site. Reference daily intakes, recommended dietary allowances. [Last Accessed on 2012 Feb 13]. Available from: www.fda.gov/fdac .
- 27.Dawson-Hughes B, Mithal A, Bonjour JP, Boonen S, Burckhardt P, Fuleihan GE, et al. IOF position statement: Vitamin D recommendations for older adults. Osteoporos Int. 2010;21:1151–4. doi: 10.1007/s00198-010-1285-3. [DOI] [PubMed] [Google Scholar]
- 28.Binkley N, Gemar D, Engelke J, Gangnon R, Ramamurthy R, Krueger D, et al. Evaluation of ergocalciferol or cholecalciferol dosing, 1,600 IU daily or 50,000 IU monthly in older adults. J Clin Endocrinol Metab. 2011;96:981–8. doi: 10.1210/jc.2010-0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vieth R, Chan PC, MacFarlane GD. Efficacy and safety of vitamin D3 intake exceeding the lowest observed adverse effect level. Am J Clin Nutr. 2001;73:288–94. doi: 10.1093/ajcn/73.2.288. [DOI] [PubMed] [Google Scholar]
- 30.Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: What clinicians need to know. J Clin Endocrinol Metab. 2011;96:53–8. doi: 10.1210/jc.2010-2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koutkia P, Chen TC, Holick MF. Vitamin D intoxication associated with an over-the-counter supplement. N Engl J Med. 2001;345:66–7. doi: 10.1056/NEJM200107053450115. [DOI] [PubMed] [Google Scholar]
- 32.Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–30. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 33.Kovacs CS. Calcium and bone metabolism in pregnancy and lactation. J Clin Endocrinol Metab. 2001;86:2344–8. doi: 10.1210/jcem.86.6.7575. [DOI] [PubMed] [Google Scholar]
- 34.Kovacs CS. Calcium and bone metabolism during pregnancy and lactation. J Mammary Gland Biol Neoplasia. 2005;10:105–18. doi: 10.1007/s10911-005-5394-0. [DOI] [PubMed] [Google Scholar]
- 35.Wagner CL, Hulsey TC, Fanning D, Ebeling M, Hollis BW. High-dose vitamin D3 supplementation in a cohort of breastfeeding mothers and their infants: A 6-month follow-up pilot study. Breastfeed Med. 2006;1:59–70. doi: 10.1089/bfm.2006.1.59. [DOI] [PubMed] [Google Scholar]


