Abstract
One of the best studied diets for cardiovascular health is the Mediterranean diet. This consists of fish, monounsaturated fats from olive oil, fruits, vegetables, whole grains, legumes/nuts, and moderate alcohol consumption. The Mediterranean diet has been shown to reduce the burden, or even prevent the development, of cardiovascular disease, breast cancer, depression, colorectal cancer, diabetes, obesity, asthma, erectile dysfunction, and cognitive decline. This diet is also known to improve surrogates of cardiovascular disease, such as waist-to-hip ratio, lipids, and markers of inflammation, as well as primary cardiovascular disease outcomes such as death and events in both observational and randomized controlled trial data. These enhancements easily rival those seen with more established tools used to fight cardiovascular disease such as aspirin, beta-blockers, ACE-inhibitors, and exercise. However, it is unclear if the Mediterranean diet offers cardiovascular disease benefit from its individual constituents or in aggregate. Furthermore, the potential benefit of the Mediterranean diet or its components is not yet validated by concrete cardiovascular disease endpoints in randomized trials or observational studies. This review will focus on the effects of the whole and parts of the Mediterranean diet with regard to both population-based as well as experimental data highlighting cardiovascular disease morbidity or mortality and cardiovascular disease surrogates when hard outcomes are not available. Our synthesis will highlight the potential for the Mediterranean diet to act as a key player in cardiovascular disease prevention, and attempt to identify certain aspects of the diet which are particularly beneficial for cardio-protection.
Keywords: Mediterranean Diet, Cardiovascular Disease
Introduction
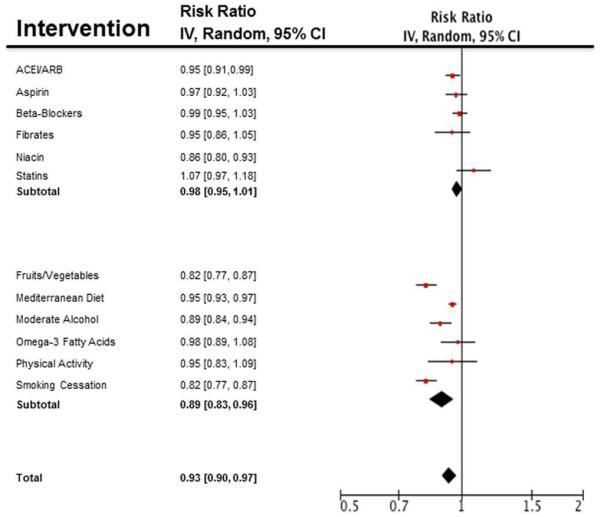
Cardiovascular disease is the leading cause of morbidity and mortality in the world regardless of race, ethnicity, or gender, and costs related to cardiovascular disease in the United States are expected to surpass $300 billion in 2010 (1). Optimistically, simple and cost-effective steps such as a proper diet should be able to alleviate the obesity epidemic and the resultant cardiovascular disease burden as it is estimated that lifestyle choices can account for up to 40% of premature cardiovascular disease deaths (2). The Mediterranean diet – consisting of fish, unsaturated fats, whole grains, fruits and vegetables, nuts and legumes – has consistently been shown to reduce cardiovascular morbidity and mortality as well as surrogate markers in meta-analyses, cohort studies, and randomized control trials (RCTs). These improvements match reductions in cardiovascular disease burden demonstrated by highly proven and advertised interventions, and approach measures such as physical activity and smoking cessation (Figure 1). This historical and narrative review examines current professional society guidelines, RCTs, observational studies, and meta-analyses throughout the literature pertaining to the Mediterranean diet – and the components thereof – dating back to the inception of such a concept with the Seven Countries Study in the 1980s in an effort to critically examine the role of the Mediterranean diet and its components in ameliorating the burden of cardiovascular disease.
Figure 1.
Estimates of risk ratio reduction based on recent meta-analyses of trials examining medication adherence vs. placebo and lifestyle interventions vs. control. Estimates on the effect of niacin were removed as there are no recent meta-analyses which include recent negative data. Relative risks are reported with logarithmic conversions and standard errors plotted on the Forest plot. Estimates of lifestyle modifications such as the Mediterranean diet as a whole (106), fruits and vegetables (59, 61, 62), smoking cessation (103), moderate alcohol (105), omega-3 fatty acids (110), and improved physical activity (102) have substantial benefits for CVD prevention not seen with commonly used standard medical therapies such as statins (100, 101), renin-angiotensin system blockade (104), Fibrates (107), aspirin (108), beta-blockers (109),
The Mediterranean Diet, in toto
The authors of the Seven-Countries Study (3) note that in contrast to the rest of the developed world, the farmers of Crete consumed some of the largest amounts of fat yet had the lowest cardiovascular mortality rate. The diet does not single out specific food items or limit calories, but rather emphasizes an abundance of plant foods, olive oil as the principal source of fat, limited dairy products, consumption of moderate amounts of fish, poultry, and wine, low amounts of red meat, and fresh fruit daily – consistent with current American Heart Association (AHA) and European Society of Cardiology (ESC) recommendations for dietary caloric distribution (4, 5).
Principle in the data favoring the Mediterranean diet is the Lyon Heart Study which showed in an RCT that composite endpoints of cardiovascular disease events and death were reduced for up to four years after an initial event in those randomized to the Mediterannean diet, thus establishing it as a staple in secondary prevention (6). Recently, the PREvencion con DIeta MEDiterannea (PREDIMED) investigators completed an RCT comparing a low fat diet to either the Mediterranean diet supplemented with either olive oil or nuts (7). This trial was, in fact, halted early after a significant reduction in cardiovascular disease events was overwhelmingly evident in the Metiterranean diet arms of the trial, and distinctly marked almost immediately after randomization. This flagship study is one of the largest randomized trials focusing on primary cardiovascular disease prevention, and clearly places the Mediterranean diet at the forefront of preventative cardiovascular medicine. More copious, yet congruent, observational and RCT data exist with one RCT evaluating surrogate markers of cardiovascular disease prevention showing that the Mediterranean diet reduces the risk of repeat cardiovascular events (8). Further RCT evidence supports the use of a Mediterranean diet to reduce genetic predisposition for risk factors, not cardiovascular disease morbidity or mortality and their complications, in a high-risk population (9). This trial (a sub-study of the multicenter PREDIMED study (10, 11)) shows that patients on the Mediterranean diet had fewer monocytes, inflammatory markers, and beneficial modulation of gene expression involved in LDL-oxidation. The Mediterranean diet appears to show beneficial effects regarding the metabolic syndrome (12) and diabetes (11) compared to low-fat diets, especially when enriched with either nuts or olive oil (12).
Observational and ecological studies such as the original Seven-Countries Study have shown positive benefits of the Mediterranean diet in terms of cardio-protection, surrogate markers for cardiovascular disease, as well as overall morbidity and mortality (13, 14). Subsequently, a large meta-analysis of over 50,000 patients showed that the Mediterranean diet significantly reduced the risk of metabolic syndrome and protected against risk factors such as waist circumference, lipids, glucose, and blood pressure (15) in primary prevention (Figure 2). Another meta-analysis of 2650 patients showed that the Mediterranean diet provided a more robust reduction in cardiovascular disease risk factors and inflammatory markers (16).
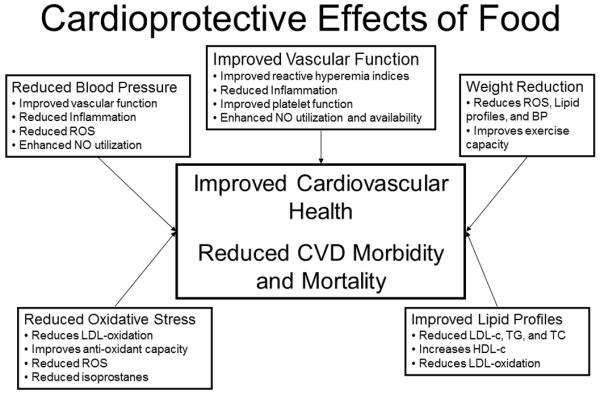
Figure 2.
Collective mechanisms proposed to underlie the protective effect of foods against cardiovascular disease. Clearly, no single ingredient or mechanism can account for all the advantages of certain food groups, and it takes a calorically sensible and balanced variety to derive the greatest benefit for patients.
In fact, the Mediterranean diet is comparable to other interventions such as aspirin, statins, physical activity, and even antihypertensives such as ace-inhibitors or beta-blockers in terms of reducing the risk of cardiovascular disease morbidity, mortality, and events (Figure 1). These estimates, of course, are rough due to the vast heterogeneity of in the types and varieties of studies and their sizes, subjects, styles, and primary/secondary end points. Consequently, the data regarding the Mediterranean diet for cardiovascular disease morbidity and mortality reduction is robust, and recently cemented by a primary prevention RCT showing overwhelming benefit.
The remainder of this review will examine the foods which comprise the Mediterranean diet in an effort to review the observational versus RCT data of the individual components of the diet which may offer insights into which foods within the diet might offer a reduction in cardiovascular disease morbidity and mortality.
Omega-3 Polyunsaturated Fats, Such as Fish
The marine omega-3 fatty acids are polyunsaturated fatty acids and widely studied in the Mediterranean diet. Per recommendations made by the AHA/ACC, fish should be consumed twice per week in cases of known cardiovascular disease (17). European guidelines endorse the isocaloric consumption of fish for primary and secondary cardiovascular disease and possibly dysrhythmia protection (18).
A multitude of meta-analyses have shown a potential cardiovascular disease morbidity and mortality benefit for mainly secondary prevention with increased fish intake (19-28). A systematic review of RCTs has shown that marine omega-3 portend a benefit for cardiovascular disease risk reduction (29) (RR=0.57), and have been confirmed by numerous RCTs with the principal sources for these data are the Diet and reinfarction trial (DART), Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI)-Prevention, and Japan EPA Lipid Intervention Study JELIS studies (30-33). Recent meta-analyses of observational studies support the intake of higher amounts of fish (40-60 grams/day or 1-2 times/week) in high-risk populations (27, 34, 35). Though less convincing, primary prevention data is favorable so long as patients carefully balance fish intake to 2-3 times/week to minimize the risk of mercury toxicity. A primary drawback in these larger meta-analyses is heterogeneity in fish intake versus fish oil supplementation in the comparisons. Certainly RCTs examining fish oil supplementation in patients already on maximal medical therepy have shown a reduced effect on cardiovascular disease outcomes (33). The well-controlled confounders in fish oil supplementation RCTs may be a source of discrepancies between these studies and larger, positive observational trials.
One of the largest cohort trials examining fish intake and cardiovascular disease, the Physician’s Health Study published in 1995, utilized prospective cohort data to argue against an association between fish consumption and cardiovascular disease benefit (36). These data were then confirmed that same year by a larger cohort of health professionals that showed no association between increased fish consumption (from 1-2 to 5-6 servings/week) and reduced cardiovascular disease mortality (37). As these are observational studies, selection bias and recall bias must be taken into consideration when evaluating these data in relation to the entire body of work as meta-analyses of prior observational data supports the cardiovascular benefits of fish in moderate to high-risk cardiovascular disease patients.
Mechanisms underlying the beneficial effects of fish on cardiovascular disease include improved lipid profiles (38) and reduced blood pressure (39, 40), presumably through reduced inflammation, oxidation, and coagulation (41, 42) (Figure 2). Thus, diets with moderate fish intake seem to confer cardiovascular disease benefits – independent of their presence within the Mediterranean diet – and should comprise a key culinary component for patients seeking a heart-healthy diet either independently or in conjunction with the remainder of the Mediterranean diet.
Unsaturated Fats, Such as Olive Oil
One of the most prominent aspects of the Mediterranean diet is the high concentration of unsaturated fats in its sources of fiber and protein, coupled with a paucity of saturated fats (43, 44). Both the AHA/ACC and ESC guidelines strongly endorse substituting mono- and polyunsaturated fats in place of saturated and trans-fatty acids for both primary and secondary prevention (5, 18, 45).
Research on the impact of olive oil consumption for cardiovascular disease prevention has expanded over the last decades. Hard cardiovascular disease endpoints, however, are currently lacking from the data in the form of RCTs. Instead, interest lies mainly in the mechanisms behind the minor polar compounds with potent antioxidant properties, including simple and complex phenols, which are present in appreciable amounts in extra virgin olive oils. The cardio-protective effects of olive oil are now thought to be attributed to the presence of its phenolic compounds obtained from the water-soluble fraction and include mostly the low-molecular weight molecule hydroxytyrosol and also oleuropein which are both potent antioxidants, free radical scavengers and enzyme modulators (46). Two randomized, blinded crossover trials have assessed the antioxidant effect of dietary supplementation of extra virgin olive oil in humans: EUROLIVE (47) and the Virgin Olive Oil Study (VOLOS) (48). The Italian VOLOS trial (48) studied the inflammatory protective potential of olive oil in 22 mildly dyslipidemic patients. After a seven week treatment period, levels of thromboxane B2 (an index of maximal platelet activation) and total antioxidant capacity of plasma were both reduced with administration of olive oil without change in overall serum lipid profiles. In the The Effect of Olive Oil on Oxidative Damage in European Populations (EUROLIVE) study (47), a randomized, crossover controlled trial performed at six research centers across five European studies, patients received olive oil with low, medium or high phenolic content for three weeks with intervening two week washout periods. There was a linear decrease in markers of oxidative stress with increasing phenolic content by 1.21 to 3.21U/L. A recent randomized crossover trial in a small group of healthy patients demonstrated that not only does the Mediterranean Diet (rich with olive oil) improve endothelial function and reduce systemic inflammation, but it also improves endothelial progenitor cell numbers which the authors report as a marker of increased endothelial repair (49). Ex-vivo observations in healthy volunteers showed that, in contrast to butter- and walnut-rich meals, consumption of an olive oil-rich meal does not induce the postprandial activation of NF-kB pathway in monocytes (50), thus suggesting an anti-inflammatory effect. Recent data from our lab indicates a beneficial effect of olive oil supplementation on endothelial function in low-moderate risk patients (51).
Early meta-analyses primarily evaluating the effects of fatty acids on surrogate markers for cardiovascular disease such as cholesterol indicated that monounsaturated fatty acid intake increased lipid levels, including HDL (52). Scant evidence establishes the effect of monounsaturated fats alone on cardiovascular disease mortality, yet a large meta-analysis suggests an inverse correlation between blood pressure and monounsaturated fats intake (53). Finally, there is RCT data (7) that the Mediterranean diet supplemented with olive oil proffers cardiovascular disease surrogate and morbidity benefit, respectively. However, teasing apart olive oil as being of primary benefit in these trials is difficult to do as nut supplementation showed similar results in primary outcomes.
Fruits and Vegetables
Nearly every diet – including the Mediterranean – aimed at improving cardiovascular health encourages daily intake of multiple servings of both fruits and vegetables. In fact, the ESC strongly endorses the dietary use of fruits and vegetables to reduce cardiovascular disease risk (18), and the AHA has twice re-affirmed a similar stance (5, 45). Additionally, the AHA has strongly recommended the intake of a variety of phytochemicals, of which fruits and vegetables have large quantities, for the prevention of cardiovascular disease (54). These recommendations are based upon a broad base of observational studies, and subsequent meta-analyses, with sparing support from RCT data, pointing to potential benefits of increased fruit and vegetable intake.
Copious observational data shows a reduction in cardiovascular disease surrogates by individuals who report increased consumption of fruits and vegetables. A 2003 study showed a 3.0 mmHg drop in systolic blood pressure among women who consumed a higher amount of fruits, vegetables, or vitamin C with no difference in men (55). A 2004 cross-sectional analysis of a prospective cohort study (the SUN study) showed that fruit and vegetable consumption is inversely associated with blood pressure in a Mediterranean population with a high vegetable-fat intake (56). Increased fruit and vegetable intake has also been linked with a lower body mass index in another cross-sectional study (57). Finally, the prospective Chicago Western Electric Study showed a slight benefit on blood pressure compared to intake of red meat over a seven year period of time (58). This body of work demonstrates that increased red meat consumption produced a net blood pressure elevation in middle-aged men compared to an increased fruit and vegetable intake.
A large 2006 meta-analysis of nearly 200,000 patients showed a 4% relative risk reduction in cardiovascular disease with each serving of vegetables with a 7% relative risk reduction in cardiovascular disease with each daily increase in servings of fruit, although the results were slightly skewed by heterogeneity and publication bias (59). Another large (over 200,000 patients) meta-analysis of observational studies showed a 17% reduction in cardiovascular disease events with three to five servings of fruits and vegetables daily as the primary endpoint (60), data that were reaffirmed two years later (61). Recently, population-based evidence from the Evaluating Pimobendan In Cardiomegaly (EPIC)-Heart study showed, after an eight-year follow up of 313,074 patients without overt atherosclerosis, a 22% lower risk of fatal ischemic heart disease in those consuming eight portions of fruits and vegetables a day as compared to three portions or less (62).
RCT data is not as convincing, and only peripherally addresses the cardiovascular disease benefits of fruits and vegetables by utilizing cardiovascular disease surrogates as endpoints. A 2001 RCT showed that increased fruits and vegetables portended no significant change in lipid or blood pressure profiles, although a strong trend existed for both (63). A subsequent RCT showed a statistically significant effect of fruit and vegetable consumption on both plasma antioxidant concentrations and blood pressure (64).
Interestingly, the potential benefit of fruits and vegetables could lie in reduced total caloric burden, and/or in the numerous micronutrients that they provide. While solid evidence establishes the antioxidant properties of fruit and vegetables (65) and the health benefits of increased flavonol intake (66), alternative mechanisms have been proposed (67) and could include the effects of nitric oxide (NO) species or concomitant weight loss associated with diets high in fruits and vegetables. Although a wide array of RCT, outcomes-based data does not, to our knowledge, exist in the literature, we support the use of fruits and vegetables for cardiovascular disease prevention. However, this may be a case whereupon the synergistic effects of fruits and vegetables along with the remainder of the Mediterranean diet, although not yet tested, provide the most cardiovascular disease benefit.
Whole Grain Foods High in Fiber
Much data suggest a beneficial effect of increased whole grains on cardiovascular disease morbidity and mortality. The AHA guidelines indicate that diets high in fiber, such as whole grains, oats, and barley, reduce cardiovascular disease morbidity and mortality through lipid-lowering, and recommend a total dietary fiber intake of 25-30 g per day from whole foods (68). While the ESC does not have specific guidelines or recommendations regarding the purpose or amount of whole grains consumption, it endorses intake of foods with high in dietary fiber to promote cardiovascular disease health (18).
RCTs show mixed data on surrogate markers of cardiovascular disease such as blood pressure, cholesterol, and markers of inflammation; however, there is no overt information regarding hard cardiovascular disease endpoints. A smaller RCT showed beneficial effects on BMI and waist circumference in the group randomized to hypocaloric whole grains as opposed to hypocaloric refined grains (69). Moreover, the group obtaining all carbohydrates from whole grains for 12 weeks had significant improvements in CRP levels and cholesterol profile. A larger, subsequent, RCT confirmed these results in over 230 participants randomized to three daily servings of refined carbohydrates versus whole grains +/− whole oats, with the latter showing significant improvements in blood pressure and lipid profiles (70). In a recent RCT, over 300 overweight individuals were randomized to control, intermediate whole grain, or high whole grain diets for four months in substitution for their normal carbohydrate intake. No significant differences in cardiovascular disease surrogate markers were observed after four months; although the study might have been under-powered to detect them in such a short period of time, despite a similar design to the positive trials involving whole grains and cardiovascular disease (71).
A single meta-analysis evaluating the merit of whole grains showed a collective benefit in a series of prospective cohort studies, with a 21% reduction in cardiovascular disease events and mortality (72). Larger observational studies have shown a reduction in cardiovascular disease morbidity with increased intake of whole grain sources in the Iowa Women’s Study and the Nurses Health Study (73, 74). Finally, observational data show improved all cause and cardiovascular disease mortality in women with type 2 diabetes who consume whole grains (75).
Mechanisms for the benefit of whole grains on cardiovascular disease are numerous (76), but the whole-body benefits of increased fiber from whole grains appear to be related to reduced inflammation, reactive oxidation, lipid profiles, and blood pressure (77) (Figure 2). Observational studies show that benefits extend to improved glucose metabolism (78, 79), reduction in weight (80), and antioxidant capabilities (81). Alternatively, high-fiber whole grain diets could inhibit absorption of fats, simple carbohydrates, or toxins. Nevertheless, the benefit of increased fiber intake has been confirmed by large cohort studies and meta-analyses, yet the recommendation promoting whole grains has no RCT data regarding a reduction in cardiovascular disease morbidity or mortality behind it. As such, increased whole grain intake should still be pursued for cardiovascular disease prevention, however its isolation from the remainder of the Mediterranean diet might not maximize its true cardio-protective potential.
Nuts and Legumes
Predominantly, the data regarding the beneficial effect of moderate nut consumption is positive, yet similar convincing evidence cannot support the same for legumes. Few meta-analyses or RCTs describe the cardiovascular disease morbidity and mortality impact of nuts, but most early observational data point to a reduction in cardiovascular disease risk with isocaloric nut consumption as a major source of fat (82). One recent analysis predicted that nut consumption could offer a 0.67 preventative risk reduction on heart disease (29). One early evaluation of observational studies showed that replacing walnuts, peanuts, almonds, or other nuts for a serving of carbohydrates or saturated fats reduced blood lipids as well as the risk for cardiovascular disease by 30% and 45%, respectively (82, 83).
Furthermore, a recent 2009 meta-analysis showed a significant reduction in LDL cholesterol, inflammatory and oxidants mediators with increased walnut consumption (84), but no evidence established meaningful reductions in other risk factors or cardiovascular disease mortality. Interestingly, a more recent meta-analysis pointed out benefits of nuts (85) on weight loss. One of the largest studies published in 2006, a meta-analysis of four observational studies (Adventist Health Study, Iowa Women’s Health Study, Nurses’ Health Study, and the Physician’s Health Study), showed an inverse relationship between nut consumption and cardiovascular disease (primary endpoint), with a nearly 40% decrease in the incidence of primary cardiovascular disease with consumption of at least four nut servings per week and up to 10% reduction with a single serving per week (86).
RCT data, again, is less convincing, likely secondary to underpowered studies and large variety of nuts that could be studied. However, recent RCT data, mentioned early in the review offers evidence that the Mediterranean diet supplemented with nuts offers primary cardiovascular disease prevention benefits (7). Again, these benefits were seen in conjunction with the remainder of the Mediterranean diet, so ascribing the benefit solely to nuts would be an overstatement of the data. Numerous cohort studies and quite a few smaller RCTs have shown a benefit in terms of lipid profiles, reducing ROS, improving vascular function, reducing blood pressure, and improving cardiovascular morbidity and mortality. Furthermore, such convincing evidence regarding increased nut consumption on cardiovascular disease prevention would likely lend it to being a food which can be consumed in isolation, without the added benefit offered by the Mediterranean diet although when added to the Mediterranean diet can offer greater cardiovascular disease benefit (12).
Conversely, the data regarding other legumes is not as positive. Legumes are typically considered the seeds of plants that contain roots, which utilize nitrogen-fixing bacteria on their roots, comprised of a wide variety of sources and types difficult to carefully study. These seeds are considered low-glycemic and a useful dietary source of protein and fiber. Initial observational studies showed legume and soy intake to be beneficial toward preventing cardiovascular disease (87) as NHANES data showed an 11% reduction in cardiovascular disease in women who consumed legumes four or more times weekly over those who consumed legumes one, or fewer, times weekly. Similar observational data has been reported out of Japan (88) and China (89).
RCT data rarely addresses hard cardiovascular disease endpoints, and the grouped data only shows marginal benefits with regard to lipid levels, blood pressure, or endothelial function. Small RCTs in low-moderate risk patients show little (90) to no change in lipid levels (91, 92). Yet one meta-analysis shows a 5% reduction in LDL levels in patients who were randomized to high legume intake (93), however this reduction was not noted to have an effect on hard cardiovascular disease endpoints. RCTs have shown a benefit on blood pressure in patients with moderate hypertension (94). And a recent RCT shows no benefit of soy on NO bioavailability or BP in moderately hypertensive, post-menopausal women (95), consistent with prior meta-analyses mentioned above (93).
However, subsequent meta-analyses have been less convincing regarding cardiovascular disease benefit, particularly with regard to surrogate endpoints. Due to a potential anti-inflammatory and vaso-protective benefit, a multitude of studies has examined the effect of soy on endothelial function. A fairly recent meta-analysis of RCTs shows no benefit of soy on endothelial function (96); however when the age-related results are adjusted for baseline endothelial function, there is a moderate benefit of soy supplementation. A larger sample of RCTs studies showed no benefit from soy supplementation on normotensive patients (97) and an earlier meta-analysis mirrored these findings (98). Thus, despite an abundance of observational data, and recent, well-designed RCTs and subsequent meta-analyses, we find little direct evidence that legume intake, alone, has direct cardiovascular disease benefit. Interestingly, while nutritionally similar and usually grouped together with nuts – which do have a positive cardiovascular disease impact – It could be hypothesized that legume intake must be part of the Mediterranean diet as a whole, and cannot be supplemented in isolation for cardiovascular disease protection.
Conclusions
The Mediterranean Diet is arguably the best-studied and most evidence-based diet to prevent not only CVD but also other chronic diseases, as it has become the standard for healthy eating and a dietary template of particular value. The primary advantage of the Mediterranean diet appears to lie in its synergy among various cardio-protective nutrients and foods (99). Indeed, the diet and, to a lesser degree, its components have been found to reduce cardiovascular disease risk by mechanisms including reduction of surrogates of cardiovascular disease such as blood pressure, lipids, endothelial dysfunction, glucose, BMI, and waist circumference as well as by providing increased NO bioavailability, antioxidant properties, as well as anti-inflammatory effects (Figure 2).
As illustrated in this review, the Mediterranean diet has proven secondary cardiovascular disease prevention benefit and improvements in surrogate markers for cardiovascular disease as evidenced by copious observational, RTC, and even meta-analyses. Certain constituents of the Mediterranean diet, including fish and nuts, have established cardiovascular morbidity/mortality benefits (Table 1), which can possibly be noted in isolation from the remainder of the Mediterranean diet. Both observational and RCT data documented improvement in cardiovascular disease prevention (Table 1) with constituents of the Mediterranean diet which should be consumed in moderation to ensure a balanced diet and avoid caloric excess. Preventive measures depend strongly upon length of time followed—it is a life-long commitment, not something that can be done episodically. Duration may be more important than intensity, especially because high intensities are difficult to sustain. Simply changing one or following a few dietary constituents does not exclude detrimental effects of the rest of the diet or lifestyle. This is, of course, why the dietary pattern is much more important than the effects of individual constituents. In fact, the content of this review reveals that our best culinary interventions may not involve specific foods, but relate to a collection of healthy nutrients comparable to the Mediterranean diet – that is comprised of a group of foods considered beneficial for cardiovascular health.
Table 1.
| Food Group | Population- based Data |
RCT Data |
CVD Effect |
Proposed Mechanisms |
|---|---|---|---|---|
| Mediterranean Diet |
+++ | +++ | +++ | Improved lipids, reduces ROS, endothelial function, platelet function |
| Unsaturated Fats | + | + | + | Improved lipids, reduces ROS, endothelial function, platelet function |
| Fish | +/− | ++ | + | Improves lipid profiles and BP |
| Fruits/Vegetables | ++ | + | + | Improves lipid profiles and BP; reduces ROS |
| Whole Grains | ++ | + | + | Improved glucose metabolism, reduced inflammation, ROS, lipid profiles, and blood pressure |
| Eggs | +/− | +/− | NC | Controversial data without mechanistic evidence |
| Garlic | +/− | +/− | NC | Improves lipid profiles |
| Alcohol | ++ | + | ++ | Improves lipid profiles, BP, (+/−) ROS, and endothelial function |
| Nuts | ++ | ++ | + | +/− ROS and lipid profiles; improves BP and endothelial function |
American Journal of Medicine, Clinical Bullet Points.
The Mediterranean Diet has been proven by randomized controlled trials, observational studies, and meta-analyses to be beneficial for both primary and secondary prevention of cardiovascular disease
No specific component of the Mediterranean diet has been shown to be as beneficial as the whole.
Calorically mindful portions of each individual component should be recommended to patients for cardiovascular prevention, and further study is required to understand the contribution of the constituents of the Mediterranean diet.
Acknowledgments
This work was partly supported by NIH grants #HL92954 and #HL085307. AJF is supported by the Walter and Gertrud Siegenthaler Foundation, the young academics Support Committee of the University of Zurich, and the Swiss foundation for medical-biological scholarships (SSMBS; SNSF No PASMP3_132551).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflicts to disclose, and each author has contributed substantially to the work with access to all materials and data.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R, Sorlie P, Stafford R, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J, American Heart Association Statistics Committee. Stroke Statistics Subcommittee Heart Disease and Stroke Statistics—2010 Update. A Report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2010;121:e1–e170. [Google Scholar]
- 2.Schroeder S. Shattuck Lecture. We can do better--improving the health of the American people. N Engl J Med. 2007;357(12):1221–8. doi: 10.1056/NEJMsa073350. [DOI] [PubMed] [Google Scholar]
- 3.Keys A, Aravanis C. Seven Countries: A Multivariate Analysis of Death and Coronary Heart Disease. Harvard University Press; Cambridge, MA: 1980. [Google Scholar]
- 4.Kris-Etherton P, Innis S. Position of the American Dietetic Association and Dietitians of Canada: dietary fatty acids. J Am Diet Assoc. 2007;107:1599–611. [PubMed] [Google Scholar]
- 5.Lichtenstein A, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, Franklin B, Kris-Etherton P, Harris WS, Howard B, Karanja N, Lefevre M, Rudel L, Sacks F, Van Horn L, Winston M, Wylie-Rosett J, American Heart Association Nutrition Committee Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114(1):82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 6.de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99(6):779–85. doi: 10.1161/01.cir.99.6.779. [DOI] [PubMed] [Google Scholar]
- 7.Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, Lamuela-Raventos R, Serra-Majem L, Pintó X, Basora J, Muñoz MA, Sorlí JV, Martínez JA, Martínez-González MA. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. NEJM. 2013;368(14):1279–90. doi: 10.1056/NEJMc1806491. [DOI] [PubMed] [Google Scholar]
- 8.de Lorgeril M, Renaud S, Mamelle N, Salen P, Martin JL, Monjaud I, Guidollet J, Touboul P, Delaye J. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994;343(8911):1454–9. doi: 10.1016/s0140-6736(94)92580-1. [DOI] [PubMed] [Google Scholar]
- 9.Llorente-Cortés V, Estruch R, Mena MP, Ros E, González MA, Fitó M, Lamuela-Raventós RM, Badimon L. Effect of Mediterranean diet on the expression of pro-atherogenic genes in a population at high cardiovascular risk. Atherosclerosis. 2010;208:442–50. doi: 10.1016/j.atherosclerosis.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 10.Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Covas MI, Fiol M, Gómez-Gracia E, López-Sabater MC, Vinyoles E, Arós F, Conde M, Lahoz C, Lapetra J, Sáez G, Ros E, PREDIMED Study Investigators Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med. 2006;145(1):1–11. doi: 10.7326/0003-4819-145-1-200607040-00004. [DOI] [PubMed] [Google Scholar]
- 11.Salas-Salvadó J, Bulló M, Babio N, Martínez-González MÁ, Ibarrola-Jurado N, Basora J, Estruch R, Covas MI, Corella D, Arós F, Ruiz-Gutiérrez V, Ros E, PREDIMED Study Investigators Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care. 2011;34(1):14–9. doi: 10.2337/dc10-1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salas-Salvadó J ea. Effect of a Mediterranean diet supplemented with nuts on metabolic syndrome status: one-year results of the PREDIMED randomized trial. Arch Intern Med. 2008;168(22):2449–58. doi: 10.1001/archinte.168.22.2449. [DOI] [PubMed] [Google Scholar]
- 13.Fung T, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009;119(8):1093–100. doi: 10.1161/CIRCULATIONAHA.108.816736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keys A, Menotti A, Karvonen MJ, Aravanis C, Blackburn H, Buzina R, Djordjevic BS, Dontas AS, Fidanza F, Keys MH. The diet and 15-year death rate in the seven countries study. Am J Epidemiol. 1986;124:903–15. doi: 10.1093/oxfordjournals.aje.a114480. [DOI] [PubMed] [Google Scholar]
- 15.Kastorini C, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB. The effect of Mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534,906 individuals. J Am Coll Cardiol. 2011;57(11):1299–313. doi: 10.1016/j.jacc.2010.09.073. [DOI] [PubMed] [Google Scholar]
- 16.Nordmann A, Suter-Zimmermann K, Bucher HC, Shai I, Tuttle KR, Estruch R, Briel M. Meta-analysis comparing mediterranean to low-fat diets for modification of cardiovascular risk factors. Am J Med. 2011;124(9):841–51. doi: 10.1016/j.amjmed.2011.04.024. [DOI] [PubMed] [Google Scholar]
- 17.Kris-Etherton P, Harris WS, Appel LJ, American Heart Association. Nutrition Committee Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation. 2002;106(21):2747–57. doi: 10.1161/01.cir.0000038493.65177.94. [DOI] [PubMed] [Google Scholar]
- 18.Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, Dallongeville J, De Backer G, Ebrahim S, Gjelsvik B, Herrmann-Lingen C, Hoes A, Humphries S, Knapton M, Perk J, Priori SG, Pyorala K, Reiner Z, Ruilope L, Sans-Menendez S, Scholte op Reimer W, Weissberg P, Wood D, Yarnell J, Zamorano JL, Walma E, Fitzgerald T, Cooney MT, Dudina A, European Society of Cardiology (ESC) Committee for Practice Guidelines (CPG) European guidelines on cardiovascular disease prevention in clinical practice: executive summary: Fourth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by representatives of nine societies and by invited experts) Eur Heart J. 2007;28(19):2375–414. doi: 10.1093/eurheartj/ehm316. [DOI] [PubMed] [Google Scholar]
- 19.Bucher H, Hengstler P, Schindler C, Meier G. N-3 polyunsaturated fatty acids in coronary heart disease: a meta-analysis of randomized controlled trials. Am J Med. 2002;112(4):298–304. doi: 10.1016/s0002-9343(01)01114-7. [DOI] [PubMed] [Google Scholar]
- 20.Carroll D, Roth MT. Evidence for the cardioprotective effects of omega-3 Fatty acids. Ann Pharmacother. 2002;36(12):1950–6. doi: 10.1345/aph.1A314. [DOI] [PubMed] [Google Scholar]
- 21.Chen Q, Cheng LQ, Xiao TH, Zhang YX, Zhu M, Zhang R, Li K, Wang Y, Li Y. Effects of omega-3 fatty acid for sudden cardiac death prevention in patients with cardiovascular disease: a contemporary meta-analysis of randomized, controlled trials. Cardiovasc Drugs Ther. 2011;25(3):259–65. doi: 10.1007/s10557-011-6306-8. [DOI] [PubMed] [Google Scholar]
- 22.Di Minno M, Tremoli E, Tufano A, Russolillo A, Lupoli R, Di Minno G. Exploring newer cardioprotective strategies: ω-3 fatty acids in perspective. Thromb Haemost. 2010;104(4):664–80. doi: 10.1160/TH10-01-0008. [DOI] [PubMed] [Google Scholar]
- 23.Filion K, El Khoury F, Bielinski M, Schiller I, Dendukuri N, Brophy JM. Omega-3 fatty acids in high-risk cardiovascular patients: a meta-analysis of randomized controlled trials. BMC Cardiovasc Disord. 2010;10(24) doi: 10.1186/1471-2261-10-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hooper L, Thompson RL, Harrison RA, Summerbell CD, Ness AR, Moore HJ, Worthington HV, Durrington PN, Higgins JP, Capps NE, Riemersma RA, Ebrahim SB, Davey Smith G. Risks and benefits of omega 3 fats for mortality, cardiovascular disease, and cancer: systematic review. BMJ. 2006;332(7544):752–60. doi: 10.1136/bmj.38755.366331.2F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oomen C, Feskens EJ, Räsänen L, Fidanza F, Nissinen AM, Menotti A, Kok FJ, Kromhout D. Fish consumption and coronary heart disease mortality in Finland, Italy, and The Netherlands. Am J Epidemiol. 2000;151(10):999–1006. doi: 10.1093/oxfordjournals.aje.a010144. [DOI] [PubMed] [Google Scholar]
- 26.von Schacky C, Harris WS. Cardiovascular benefits of omega-3 fatty acids. Cardiovasc Res. 2007;73(2):310–5. doi: 10.1016/j.cardiores.2006.08.019. [DOI] [PubMed] [Google Scholar]
- 27.Whelton S, He J, Whelton PK, Muntner P. Meta-analysis of observational studies on fish intake and coronary heart disease. Am J Cardiol. 2004;93(9):1119–23. doi: 10.1016/j.amjcard.2004.01.038. [DOI] [PubMed] [Google Scholar]
- 28.Yzebe D, Lievre M. Fish oils in the care of coronary heart disease patients: a meta-analysis of randomized controlled trials. Fundam Clin Pharmacol. 2004;18(5):581–92. doi: 10.1111/j.1472-8206.2004.00268.x. [DOI] [PubMed] [Google Scholar]
- 29.Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169(7):659–69. doi: 10.1001/archinternmed.2009.38. [DOI] [PubMed] [Google Scholar]
- 30.Burr M, Ashfield-Watt PA, Dunstan FD, Fehily AM, Breay P, Ashton T, Zotos PC, Haboubi NA, Elwood PC. Lack of benefit of dietary advice to men with angina: Results of a controlled trial. Eur J Clin Nutr. 2003;57:193–200. doi: 10.1038/sj.ejcn.1601539. [DOI] [PubMed] [Google Scholar]
- 31.Miocardico R, Gruppo Italiano per lo Studio della Sopravvivenza Nell’Infarto Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione Trial. Lancet. 1999;354(9177):447–55. [PubMed] [Google Scholar]
- 32.Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, Oikawa S, Sasaki J, Hishida H, Itakura H, Kita T, Kitabatake A, Nakaya N, Sakata T, Shimada K, Shirato K, Japan EPA lipid intervention study (JELIS) Investigators Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (jelis): A randomised open-label, blinded endpoint analysis. Lancet. 2007;369:1090–8. doi: 10.1016/S0140-6736(07)60527-3. [DOI] [PubMed] [Google Scholar]
- 33.Burr M, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetnam PM, Elwood PC, Deadman NM. Effects of changes in fat, fish and fibre intakes on death and reinfarction: diet and reinfarction trial (DART) Lancet. 1989;2(8666):757–61. doi: 10.1016/s0140-6736(89)90828-3. [DOI] [PubMed] [Google Scholar]
- 34.He K, Song Y, Daviglus ML, Liu K, Van Horn L, Dyer AR, Greenland P. Accumulated evidence on fish consumption and coronary heart disease mortality: A meta-analysis of cohort studies. Circulation. 2004;109:2705–11. doi: 10.1161/01.CIR.0000132503.19410.6B. [DOI] [PubMed] [Google Scholar]
- 35.Marckmann P, Gronbaek M. prospective cohort studies. Fish consumption and coronary heart disease mortality: a systematic review of prospective cohort studies. Eur J Clin Nutr. 1999;53(8):585–90. doi: 10.1038/sj.ejcn.1600832. [DOI] [PubMed] [Google Scholar]
- 36.Morris MC, Manson JE, Rosner B, et al. Fish Consumption and Cardiovascular Disease in the Physicians’ Health Study: A Prospective Study. American Journal of Epidemiology. 1995;142(2):166–75. doi: 10.1093/oxfordjournals.aje.a117615. [DOI] [PubMed] [Google Scholar]
- 37.Ascherio A, Rimm EB, Stampfer MJ, Giovannucci EL, Willett WC. Dietary intake of marine n-3 fatty acids, fish intake, and the risk of coronary disease among men. N Engl J Med. 1995;332(15):977–82. doi: 10.1056/NEJM199504133321501. [DOI] [PubMed] [Google Scholar]
- 38.Balk E, Lichtenstein AH, Chung M, Kupelnick B, Chew P, Lau J. Effects of omega-3 fatty acids on serum markers of cardiovascular disease risk: a systematic review. Atherosclerosis. 2006;189(1):19–30. doi: 10.1016/j.atherosclerosis.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 39.Appel L, Miller ER, 3rd, Seidler AJ, Whelton PK. Does supplementation of diet with ‘fish oil’ reduce blood pressure? A meta-analysis of controlled clinical trials. Arch Intern Med. 1993;153(12):1429–38. [PubMed] [Google Scholar]
- 40.Morris M, Sacks F, Rosner B. Does fish oil lower blood pressure? A meta-analysis of controlled trials. Circulation. 1993;88(2):523–33. doi: 10.1161/01.cir.88.2.523. [DOI] [PubMed] [Google Scholar]
- 41.Calder P. n-3 Fatty acids and cardiovascular disease: evidence explained and mechanisms explored. Clin Sci (Lond) 2004;107(1):1–11. doi: 10.1042/CS20040119. [DOI] [PubMed] [Google Scholar]
- 42.Harris W, Miller M, Tighe AP, Davidson MH, Schaefer EJ. Omega-3 fatty acids and coronary heart disease risk: Clinical and mechanistic perspectives. Atherosclerosis. 2008;197:12–24. doi: 10.1016/j.atherosclerosis.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 43.Howard B, Van Horn L, Hsia J, Manson JE, Stefanick ML, Wassertheil-Smoller S, Kuller LH, LaCroix AZ, Langer RD, Lasser NL, Lewis CE, Limacher MC, Margolis KL, Mysiw WJ, Ockene JK, Parker LM, Perri MG, Phillips L, Prentice RL, Robbins J, Rossouw JE, Sarto GE, Schatz IJ, Snetselaar LG, Stevens VJ, Tinker LF, Trevisan M, Vitolins MZ, Anderson GL, Assaf AR, Bassford T, Beresford SA, Black HR, Brunner RL, Brzyski RG, Caan B, Chlebowski RT, Gass M, Granek I, Greenland P, Hays J, Heber D, Heiss G, Hendrix SL, Hubbell FA, Johnson KC, Kotchen JM. Low-fat dietary pattern and risk of cardiovascular disease: the Women’s Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295(6):655–66. doi: 10.1001/jama.295.6.655. [DOI] [PubMed] [Google Scholar]
- 44.Hu F, Stampfer MJ, Manson JE, Rimm E, Colditz GA, Rosner BA, Hennekens CH, Willett WC. Dietary fat intake and the risk of coronary heart disease in women. N Engl J Med. 1997;337(21):1491–9. doi: 10.1056/NEJM199711203372102. [DOI] [PubMed] [Google Scholar]
- 45.Lichtenstein A, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, Franklin B, Kris-Etherton P, Harris WS, Howard B, Karanja N, Lefevre M, Rudel L, Sacks F, Van Horn L, Winston M, Wylie-Rosett J, American Heart Association Nutrition Committee Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2009;114:82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 46.Fuhrman B, Aviram M. Flavonoids protect LDL from oxidation and attenuate atherosclerosis. Curr Opin Lipidol. 2001;12(1):41–8. doi: 10.1097/00041433-200102000-00008. [DOI] [PubMed] [Google Scholar]
- 47.Covas MI, Nyyssonen K, Poulsen HE, et al. The effect of polyphenols in olive oil on heart disease risk factors: a randomized trial. Ann Intern Med. 2006;145(5):333–41. doi: 10.7326/0003-4819-145-5-200609050-00006. [DOI] [PubMed] [Google Scholar]
- 48.Visioli F, Caruso D, Grande S, et al. Virgin Olive Oil Study (VOLOS): vasoprotective potential of extra virgin olive oil in mildly dyslipidemic patients. Eur J Nutr. 2005;44(2):121–7. doi: 10.1007/s00394-004-0504-0. [DOI] [PubMed] [Google Scholar]
- 49.Marin C, Ramirez R, Delgado-Lista J, Yubero-Serrano EM, Perez-Martinez P, Carracedo J, Garcia-Rios A, Rodriguez F, Gutierrez-Mariscal FM, Gomez P, Perez-Jimenez F, Lopez-Miranda J. Mediterranean diet reduces endothelial damage and improves the regenerative capacity of endothelium. Am J Clin Nutr. 2011;93(2):267–74. doi: 10.3945/ajcn.110.006866. [DOI] [PubMed] [Google Scholar]
- 50.Bellido C, López-Miranda J, Blanco-Colio LM, Pérez-Martínez P, Muriana FJ, Martín-Ventura JL, Marín C, Gómez P, Fuentes F, Egido J, Pérez-Jiménez F. Butter and walnuts, but not olive oil, elicit postprandial activation of nuclear transcription factor kappaB in peripheral blood mononuclear cells from healthy men. Am J Clin Nutr. 2004;80(6):1487–91. doi: 10.1093/ajcn/80.6.1487. [DOI] [PubMed] [Google Scholar]
- 51.Widmer R, Freund MA, Flammer AJ, Sexton J, Lennon R, Romani A, Mulinacci N, Vinceri FF, Lerman LO, Lerman A. Beneficial effects of polyphenol-rich olive oil in patients with early atherosclerosis. Eur J Nutr. 2012 doi: 10.1007/s00394-012-0433-2. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mensink R, Katan MB. Effect of dietary fatty acids on serum lipids and lipoproteins. A meta-analysis of 27 trials. Arterioscler Thromb. 1992;12(8):911–9. doi: 10.1161/01.atv.12.8.911. [DOI] [PubMed] [Google Scholar]
- 53.Shah M, Adams-Huet B, Garg A. Effect of high-carbohydrate or high-cis-monounsaturated fat diets on blood pressure: a meta-analysis of intervention trials. Am J Clin Nutr. 2007;85(5):1251–6. doi: 10.1093/ajcn/85.5.1251. [DOI] [PubMed] [Google Scholar]
- 54.Howard B, Kritchevsky D. Phytochemicals and cardiovascular disease. A statement for healthcare professionals from the American Heart Association. Circulation. 1997;95(11):2591–3. doi: 10.1161/01.cir.95.11.2591. [DOI] [PubMed] [Google Scholar]
- 55.Beitz R, Mensink GBM, Fischer B. Blood pressure and vitamin C and fruit and vegetable intake. Annals of Nutr & Metabolism. 2003;47:214–20. doi: 10.1159/000070488. [DOI] [PubMed] [Google Scholar]
- 56.Alonso A, de la Fuente C, Martín-Arnau AM, de Irala J, Martínez JA, Martínez-González MA. Fruit and vegetable consumption is inversely associated with blood pressure in a Mediterranean population with a high vegetable-fat intake: the Seguimiento Universidad de Navarra (SUN) Study. Brit J Nutr. 2004;92:311–319. doi: 10.1079/BJN20041196. 2004;92:311-9. [DOI] [PubMed] [Google Scholar]
- 57.Lin B, Morrison RM. Higher fruit consumption linked with lower body mass index. Food Review. 2002;25:28–32. [Google Scholar]
- 58.Miura K, Greenland P, Stamler J, Liu K, Daviglus ML, Nakagawa H. Relation of vegetable, fruit, and meat intake to 7-year blood pressure change in middle-aged men: the Chicago Western Electric Study. Am J Epidemiol. 2004;159:572–580. doi: 10.1093/aje/kwh085. 2004;159:572-80. [DOI] [PubMed] [Google Scholar]
- 59.Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: a meta-analysis of cohort studies. J Nutr. 2006;136(10):2588–93. doi: 10.1093/jn/136.10.2588. [DOI] [PubMed] [Google Scholar]
- 60.He F, Nowson CA, Lucas M, MacGregor GA. Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: meta-analysis of cohort studies. J Hum Hypertens. 2007;21(9):717–28. doi: 10.1038/sj.jhh.1002212. [DOI] [PubMed] [Google Scholar]
- 61.Dauchet L, Amouyel P, Dallongeville J. Fruits, vegetables and coronary heart disease. Nat Rev Cardiol. 2009;6(9):599–608. doi: 10.1038/nrcardio.2009.131. [DOI] [PubMed] [Google Scholar]
- 62.Crowe F, Roddam AW, Key TJ, Appleby PN, Overvad K, Jakobsen MU, Tjønneland A, Hansen L, Boeing H, Weikert C, Linseisen J, Kaaks R, Trichopoulou A, Misirli G, Lagiou P, Sacerdote C, Pala V, Palli D, Tumino R, Panico S, Bueno-de-Mesquita HB, Boer J, van Gils CH, Beulens JW, Barricarte A, Rodríguez L, Larrañaga N, Sánchez MJ, Tormo MJ, Buckland G, Lund E, Hedblad B, Melander O, Jansson JH, Wennberg P, Wareham NJ, Slimani N, Romieu I, Jenab M, Danesh J, Gallo V, Norat T, Riboli E, European Prospective Investigation into Cancer and Nutrition (EPIC)-Heart Study Collaborators Fruit and vegetable intake and mortality from ischaemic heart disease: results from the European Prospective Investigation into Cancer and Nutrition (EPIC)-Heart study. Eur Heart J. 2011;32(10):1235–43. doi: 10.1093/eurheartj/ehq465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Broekmans W, Klopping-Ketelaars WAA, Kluft C, van den Berg H, Kok FJ, van Poppel G. Fruit and vegetables and cardiovascular risk profile: a diet controlled intervention study. Eur J Clin Nutr. 2001;55(8):636–42. doi: 10.1038/sj.ejcn.1601192. [DOI] [PubMed] [Google Scholar]
- 64.John J, Ziebland S, Yudkin P, Roe LS, Neil HAW, Oxford Fruit and Vegetable Study Group Effects of fruit and vegetable consumption on plasma antioxidant concentrations and blood pressure: a randomized controlled trial. Lancet. 2002;359(9322):1969–74. doi: 10.1016/s0140-6736(02)98858-6. [DOI] [PubMed] [Google Scholar]
- 65.Knekt P, Ritz J, Pereira MA, O’Reilly EJ, Augustsson K, Fraser GE, Goldbourt U, Heitmann BL, Hallmans G, Liu S, Pietinen P, Spiegelman D, Stevens J, Virtamo J, Willett WC, Rimm EB, Ascherio A. Antioxidant vitamins and coronary heart disease risk: a pooled analysis of 9 cohorts. Am J Clin Nutr. 2004;80(6):1508–20. doi: 10.1093/ajcn/80.6.1508. [DOI] [PubMed] [Google Scholar]
- 66.Huxley R, Neil HA. The relation between dietary flavonol intake and coronary heart disease mortality: a meta-analysis of prospective cohort studies. Eur J Clin Nutr. 2003;57(8):904–8. doi: 10.1038/sj.ejcn.1601624. [DOI] [PubMed] [Google Scholar]
- 67.Hollman P, Cassidy A, Comte B, Heinonen M, Richelle M, Richling E, Serafini M, Scalbert A, Sies H, Vidry S. The biological relevance of direct antioxidant effects of polyphenols for cardiovascular health in humans is not established. J Nutr. 2011;141(5):989S–1009S. doi: 10.3945/jn.110.131490. [DOI] [PubMed] [Google Scholar]
- 68.Van Horn L. Fiber, lipids, and coronary heart disease. A statement for healthcare professionals from the Nutrition Committee, American Heart Association. Circulation. 1997;95(12):2701–4. doi: 10.1161/01.cir.95.12.2701. [DOI] [PubMed] [Google Scholar]
- 69.Katcher H, Legro RS, Kunselman AR, Gillies PJ, Demers LM, Bagshaw DM, Kris-Etherton PM. The effects of a whole grain-enriched hypocaloric diet on cardiovascular disease risk factors in men and women with metabolic syndrome. Am J Clin Nutr. 2008;87(1):79–90. doi: 10.1093/ajcn/87.1.79. [DOI] [PubMed] [Google Scholar]
- 70.Tighe P, Duthie G, Vaughan N, Brittenden J, Simpson WG, Duthie S, Mutch W, Wahle K, Horgan G, Thies F. Effect of increased consumption of whole-grain foods on blood pressure and other cardiovascular risk markers in healthy middle-aged persons: a randomized controlled trial. Am J Clin Nutr. 2010;92(4):733–40. doi: 10.3945/ajcn.2010.29417. [DOI] [PubMed] [Google Scholar]
- 71.Brownlee I, Moore C, Chatfield M, Richardson DP, Ashby P, Kuznesof SA, Jebb SA, Seal CJ. Markers of cardiovascular risk are not changed by increased whole-grain intake: the WHOLEheart study, a randomised, controlled dietary intervention. Br J Nutr. 2010;104(1):125–34. doi: 10.1017/S0007114510000644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mellen P, Walsh TF, Herrington DM. Whole grain intake and cardiovascular disease: a meta-analysis. Nutr Metab Cardiovasc Dis. 2008;18(4):283–90. doi: 10.1016/j.numecd.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 73.Liu S, Stampfer MJ, Hu FB, Giovannucci E, Rimm E, Manson JE, Hennekens CH, Willett WC. Whole-grain consumption and risk of coronary heart disease: results from the Nurses’ Health Study. Am J Clin Nutr. 1999;70(3):412–9. doi: 10.1093/ajcn/70.3.412. [DOI] [PubMed] [Google Scholar]
- 74.Jacobs DJ, Meyer KA, Kushi LH, Folsom AR. Whole-grain intake may reduce the risk of ischemic heart disease death in postmenopausal women: the Iowa Women’s Health Study. Am J Clin Nutr. 1998;68(2):248–57. doi: 10.1093/ajcn/68.2.248. [DOI] [PubMed] [Google Scholar]
- 75.He M, van Dam RM, Rimm E, Hu FB, Qi L. Whole-grain, cereal fiber, bran, and germ intake and the risks of all-cause and cardiovascular disease-specific mortality among women with type 2 diabetes mellitus. Circulation. 2010;121(20):2162. doi: 10.1161/CIRCULATIONAHA.109.907360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Anderson J, Baird P, Davis RH, Jr, Ferreri S, Knudtson M, Koraym A, Waters V, Williams CL. Health benefits of dietary fiber. Nutr Rev. 2009;67(4):188–205. doi: 10.1111/j.1753-4887.2009.00189.x. [DOI] [PubMed] [Google Scholar]
- 77.Anderson J, Hanna TJ, Peng X, Kryscio RJ. Whole grain foods and heart disease risk. J Am Coll Nutr. 2000;19(3 Suppl):291S–9S. doi: 10.1080/07315724.2000.10718963. [DOI] [PubMed] [Google Scholar]
- 78.Jenkins D, Wesson V, Wolever TM, Jenkins AL, Kalmusky J, Guidici S, Csima A, Josse RG, Wong GS. Wholemeal versus wholegrain breads: proportion of whole or cracked grain and the glycaemic response. BMJ. 1988;297(6654):958–60. doi: 10.1136/bmj.297.6654.958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tarini J, Wolever TM. The fermentable fibre inulin increases postprandial serum short-chain fatty acids and reduces free-fatty acids and ghrelin in healthy subjects. Appl Physiol Nutr Metab. 2010;35(1):9–16. doi: 10.1139/H09-119. [DOI] [PubMed] [Google Scholar]
- 80.Good C, Holschuh N, Albertson AM, Eldridge AL. Whole grain consumption and body mass index in adult women: an analysis of NHANES 1999-2000 and the USDA pyramid servings database. J Am Coll Nutr. 2008;27(1):80–7. doi: 10.1080/07315724.2008.10719678. [DOI] [PubMed] [Google Scholar]
- 81.Adom K, Liu RH. Antioxidant activity of grains. J Agric Food Chem. 2002;50(21):6182–7. doi: 10.1021/jf0205099. [DOI] [PubMed] [Google Scholar]
- 82.Hu F, Manson JE, Willett WC. Types of dietary fat and risk of coronary heart disease: a critical review. J Am Coll Nutr. 2001;20(1):5–19. doi: 10.1080/07315724.2001.10719008. [DOI] [PubMed] [Google Scholar]
- 83.Hu F, Stampfer MJ. Nut consumption and risk of coronary heart disease: a review of epidemiologic evidence. Curr Atheroscler Rep. 1999;1(3):204–9. doi: 10.1007/s11883-999-0033-7. [DOI] [PubMed] [Google Scholar]
- 84.Banel D, Hu FB. Effects of walnut consumption on blood lipids and other cardiovascular risk factors: a meta-analysis and systematic review. Am J Clin Nutr. 2009;90(1):56–63. doi: 10.3945/ajcn.2009.27457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in Diet and Lifestyle and Long-Term Weight Gain in Women and Men. N Engl J Med. 2011;364:2392–2404. doi: 10.1056/NEJMoa1014296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kelly R. Diet and exercise in the management of hyperlipidemia. Am Fam Physician. 2010;81(9):1097–102. [PubMed] [Google Scholar]
- 87.Bazzano L, He J, Ogden LG, Loria C, Vupputuri S, Myers L, Whelton PK. Legume consumption and risk of coronary heart disease in US men and women: NHANES I Epidemiologic Follow-up Study. Arch Intern Med. 2001;161(21):2573–8. doi: 10.1001/archinte.161.21.2573. [DOI] [PubMed] [Google Scholar]
- 88.Sasazuki SFHSG. Case-control study of nonfatal myocardial infarction in relation to selected foods in Japanese men and women. Jpn Circ J. 2001;65(3):200–6. doi: 10.1253/jcj.65.200. [DOI] [PubMed] [Google Scholar]
- 89.Zhang X, Shu XO, Gao YT, Yang G, Li Q, Li H, Jin F, Zheng W. Soy food consumption is associated with lower risk of coronary heart disease in Chinese women. J Nutr. 2003;133(9):2874–8. doi: 10.1093/jn/133.9.2874. [DOI] [PubMed] [Google Scholar]
- 90.Wangen K, Duncan AM, Xu X, Kurzer MS. Soy isoflavones improve plasma lipids in normocholesterolemic and mildly hypercholesterolemic postmenopausal women. Am J Clin Nutr. 2001;73(2):225–31. doi: 10.1093/ajcn/73.2.225. [DOI] [PubMed] [Google Scholar]
- 91.Sanders T, Dean TS, Grainger D, Miller GJ, Wiseman H. Moderate intakes of intact soy protein rich in isoflavones compared with ethanol-extracted soy protein increase HDL but do not influence transforming growth factor beta(1) concentrations and hemostatic risk factors for coronary heart disease in healthy subjects. Am J Clin Nutr. 2002;76(2):373–7. doi: 10.1093/ajcn/76.2.373. [DOI] [PubMed] [Google Scholar]
- 92.Jenkins D, Kendall CW, Jackson CJ, Connelly PW, Parker T, Faulkner D, Vidgen E, Cunnane SC, Leiter LA, Josse RG. Effects of high- and low-isoflavone soyfoods on blood lipids, oxidized LDL, homocysteine, and blood pressure in hyperlipidemic men and women. Am J Clin Nutr. 2002;76(2):365–72. doi: 10.1093/ajcn/76.2.365. [DOI] [PubMed] [Google Scholar]
- 93.Zhan S, Ho SC. Meta-analysis of the effects of soy protein containing isoflavones on the lipid profile. Am J Clin Nutr. 2005;81(2):397–408. doi: 10.1093/ajcn.81.2.397. [DOI] [PubMed] [Google Scholar]
- 94.He J, Gu D, Wu X, Chen J, Duan X, Chen J, Whelton PK. Effect of soybean protein on blood pressure: a randomized, controlled trial. Ann Intern Med. 2005;143(1):1–9. doi: 10.7326/0003-4819-143-1-200507050-00004. [DOI] [PubMed] [Google Scholar]
- 95.Wong W, Taylor AA, Smith EO, Barnes S, Hachey DL. Effect of soy isoflavone supplementation on nitric oxide metabolism and blood pressure in menopausal women. Am J Clin Nutr. 2012;95(6):1487–94. doi: 10.3945/ajcn.111.032045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Li S, Liu XX, Bai YY, Wang XJ, Sun K, Chen JZ, Hui RT. Effect of oral isoflavone supplementation on vascular endothelial function in postmenopausal women: a meta-analysis of randomized placebo-controlled trials. Am J Clin Nutr. 2010;91(2):480–6. doi: 10.3945/ajcn.2009.28203. [DOI] [PubMed] [Google Scholar]
- 97.Liu X, Li SH, Chen JZ, Sun K, Wang XJ, Wang XG, Hui RT. Effect of soy isoflavones on blood pressure: a meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis. 2012;22(6):463–70. doi: 10.1016/j.numecd.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 98.Taku K, Lin N, Cai D, Hu J, Zhao X, Zhang Y, Wang P, Melby MK, Hooper L, Kurzer MS, Mizuno S, Ishimi Y, Watanabe S. Effects of soy isoflavone extract supplements on blood pressure in adult humans: systematic review and meta-analysis of randomized placebo-controlled trials. J Hypertens. 2010;28(10):1971–82. doi: 10.1097/HJH.0b013e32833c6edb. [DOI] [PubMed] [Google Scholar]
- 99.Jacobs DJ, Gross MD, Tapsell LC. Food synergy: an operational concept for understanding nutrition. Am J Clin Nutr. 2009;89(5):1543S–8S. doi: 10.3945/ajcn.2009.26736B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kostis W, Cheng JQ, Dobrzynski JM, Cabrera J, Kostis JB. Meta-analysis of statin effects in women versus men. J Am Coll Cardiol 2012. 2012;59(6):572–82. doi: 10.1016/j.jacc.2011.09.067. [DOI] [PubMed] [Google Scholar]
- 101.Taylor F, Ward K, Moore HMT, Burke M, Davey Smith George, Casas JP, Ebrahim S. Statins for the primary prevention of cardiovascular disease. Cochrane Heart Group Cochrane Database of Systematic Reviews. 2011 doi: 10.1002/14651858.CD004816.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Naci H, Ioannidis JP. Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. BMJ. 2013;347:f5577. doi: 10.1136/bmj.f5577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Critchley J, Capewell S. Smoking cessation for the secondary prevention of coronary heart disease. Cochrane Database Syst Rev. 2004;1:CD003041. doi: 10.1002/14651858.CD003041.pub2. [DOI] [PubMed] [Google Scholar]
- 104.McAlister F, Marzona I, Dagenais GR, Teo KK, Yusuf S, Jung H, Turnbull F, Neal B, Chalmers J, MacMahon S, Lowering BP, Gerstein H, Marre M, Fox K, Simoons M, Nissen S, Heerspink HL, Brenner B, De Zeeuw D, Pfeffer M, Kober L, Diener HC, Sacco R, Renin Angiotension System Modulator Meta-Analysis Investigators Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers are beneficial in normotensive atherosclerotic patients: a collaborative meta-analysis of randomized trials. Eur Heart J. 2012;33(4):505–14. doi: 10.1093/eurheartj/ehr400. [DOI] [PubMed] [Google Scholar]
- 105.Ronksley P, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671. doi: 10.1136/bmj.d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr. 2010;92(5):1189–96. doi: 10.3945/ajcn.2010.29673. [DOI] [PubMed] [Google Scholar]
- 107.Jun MFC, Lv J, Neal B, Patel A, Nicholls SJ, Grobbee DE, Cass A, Chalmers J, Perkovic V. Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis. Lancet. 2010;375(9729):1875–84. doi: 10.1016/S0140-6736(10)60656-3. [DOI] [PubMed] [Google Scholar]
- 108.Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, Buring J, Hennekens C, Kearney P, Meade T, Patrono C, Roncaglioni MC, Zanchetti A, Antithrombotic Trialists’ (ATT) Collaboration Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009;373(9678):1849–60. doi: 10.1016/S0140-6736(09)60503-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kuyper L, Khan NA. Atenolol vs nonatenolol β-blockers for the treatment of hypertension: a meta-analysis. Can J Cardiol. 2014;30(5 Supple):S47–S53. doi: 10.1016/j.cjca.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 110.Hooper L, Thompson RL, Harrison RA, Summerbell CD, Moore H, Worthington HV, Durrington PN, Ness AR, Capps NE, Davey Smith G, Riemersma RA, Ebrahim SB. Omega 3 fatty acids for prevention and treatment of cardiovascular disease. Cochrane Database Syst Rev. 2004;18(4):CD003177. doi: 10.1002/14651858.CD003177.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]