Abstract
Objective
The objective of this study was to test whether subsensory vibratory noise applied to the sole of the foot using a novel piezo-electric vibratory insole, can significantly improve sensation, enhance balance, and reduce gait variability in elderly people. We also aimed to determine the optimal level of vibratory noise, and whether the therapeutic effect would endure and the user’s sensory threshold would remain constant during the course of a day.
Design
A randomized single-blind crossover study of three subsensory noise stimulation levels on 3 separate days.
Setting
Balance and gait laboratory
Participants
12 healthy community-dwelling elderly volunteers aged 65 – 90 years who could feel the maximum insole vibration.
Intervention
A urethane foam insole with the piezo-electric actuators delivering subsensory vibratory noise stimulation to the soles of the feet.
Main Outcome Measures
Balance, gait, and timed up-and-go tests.
Results
The vibratory insoles significantly improved performance on the timed up-and-go test, reduced the area of postural sway, and reduced the temporal variability of walking at both 70% and 85% of the sensory threshold and throughout the course of a day. Vibratory sensation thresholds remained relatively stable within and across study days.
Conclusions
This study provides proof of concept that the application of the principle of stochastic resonance to the foot sole sensory system using a new low voltage piezoelectric technology can improve measures of balance and gait that are associated with falls. Effective vibratory noise amplitudes range from 70% to 85% of the sensory thresholds and can be set once daily.
Keywords: Stochastic Resonance, piezo-electric, mobility, aging, elderly, sensory, vibration, noise, shoe, insole
Introduction
Falls and mobility disorders are common, dangerous, and costly conditions among older people1. Their causes are multifactorial, including impairments in vision, gait, balance, muscle strength and cognition. Loss of peripheral somatosensory function, which is common in aging, diabetes, and other causes of peripheral neuropathy, is also a risk factor for falls2–5. There were no proven methods to improve somatosensory function in humans until recently when the physical principle of stochastic resonance (SR) was applied to the human somatosensory system. The principle asserts that the presence of a particular low level of white noise can be used to enhance the detection of a weak signal6, 7. Although we usually think of noise as something that interferes with the transmission of information, experiments in a variety of biological systems, including ion channels and sensory neurons, have demonstrated that low levels of white noise superimposed on a stimulus can actually improve its detection7. Therefore, we hypothesized that a noise-based device, such as a shoe insole, might be effective in enhancing somatosensory function in the feet and thereby enable those with reduced plantar sole sensation to overcome associated impairments in balance and gait.
We and others have shown that imperceptible (subsensory) vibratory noise applied to the feet can improve balance in healthy young and elderly subjects8 and patients with diabetic neuropathy and stroke9. We have also shown that this approach can significantly reduce stride-, stance- and swing-time variability during walking in elderly people with recurrent falls10. These studies suggested that SR is a potentially viable technology to improve balance and gait if subsensory vibratory noise can be delivered via a shoe insole. However, these early studies used a vibrating tactor that required such a large energy source that it could not be embedded into a shoe. Furthermore, the amplitude of vibratory noise was set 10% below the level that each subject could feel (90% of the sensory detection threshold), which was determined through extensive laboratory testing at the beginning of the experiment. It is not known whether less precise noise levels between 70 and 90% of the sensory threshold would yield similar results, or whether the thresholds change throughout a day and therefore require repeated noise settings at different amplitudes to remain effective during prolonged use.
Following the experiments with these early devices, a new insole stimulation device based on piezo-electric actuators was developed. The actuators were inserted into a typical insole using a standard manufacturing process. These actuators can be driven by a circuit and supplied by a battery, which are both inserted in a small encasing and attached to the tongue of a shoe. Still, many questions remain before an insole using this technology can be developed for therapeutic use. We asked whether: 1) this device could achieve improvements in mobility, balance and locomotor control as previously observed in elderly subjects; 2) the therapeutic effect would endure during the course of a day; 3) the user’s sensory threshold would remain constant throughout the day, and 4) the stimulation amplitude could still achieve a beneficial effect at other subsensory threshold levels. The current study addresses these important questions.
Methods
Design
We conducted a randomized single-blind crossover study of three subsensory noise stimulation levels on 3 separate days in 12 healthy elderly participants aged 65 – 90 years.
Subject Recruitment
Subjects were recruited from the community, local senior centers, and independent living housing sites by posting flyers and giving brief presentations about the study. Potential subjects were first screened for eligibility over the phone via a brief questionnaire. Those who passed this initial screen were then evaluated for their ability to sense the vibrations delivered by the insoles. These screening visits took place at the potential subject’s home or in the Clinical Research Laboratory at the Hebrew SeniorLife Institute for Aging Research. Informed consent was obtained prior to vibration screening. The subjects who were able to sense the vibration from the insoles in both feet were enrolled into the study. The 3 subsequent study visits took place at the Clinical Research Laboratory. All study visits were completed within a 14 day period with at least a day off in between. The study was approved by the Hebrew SeniorLife Institutional Review Board.
Inclusion Criteria
To be included in this study, participants needed to be between 65–90 years old, able to feel the maximum insole vibrations, fluent in English, capable of understanding and providing written informed consent, and willing to follow study instructions.
Exclusion Criteria
Potential participants were excluded if they had active ulcers on their feet, Parkinson’s disease or other neurodegenerative conditions, moderate to severe chronic pain in their lower extremities that interfered with standing and walking (e.g. due to arthritis, plantar fasciitis, painful peripheral neuropathy); used any type of lower extremity orthotic, could not walk unsupported around their home, could not stand and balance unsupported for at least one minute, could not feel the insole vibration when the insoles were set to maximum, did not feel comfortable wearing the insoles, used an Investigational New Drug within the past 30 days, were active participants in another clinical product performance study within the past 30 days, or had any condition that would make study participation inappropriate in the judgment of the Investigators.
Randomization
Participants were randomized by a computerized algorithm to 3 different vibratory noise levels for the 3 days of testing. These levels were 0%, 70%, and 85% of the baseline sensory threshold measured during the first session of each day. The stimulation level remained constant for each day of testing.
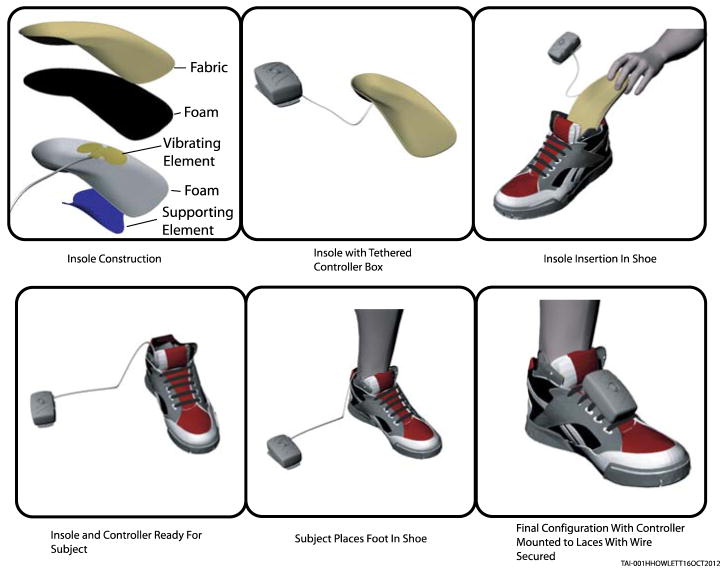
Vibratory Insole Description
The insole, its control box, and placement in a shoe are shown in Figure 1. Two piezo-electric actuators, 2.5 cm diameter each, were placed 2 cm apart in the medial arch region of each three quarters length insole to deliver the vibratory stimulation. The insole was made from urethane foam and double insulated to avoid contact with the piezoelectric actuators delivering the stimulation. Electrical circuit components for setting the threshold values were attached to the insole via a single cable. The battery lasts approximately 8 hours on a full charge, sufficient for the 6-hour duration of each study visit.
Figure 1.
An insole and control box, and Insole Insertion in Shoe
When worn for the study, the insoles were inserted into the subject’s footwear and the control box was secured to the shoelaces or top of the shoe. Research staff ensured the participant was comfortable before beginning any study procedures. Each control box has an indicator light to show that the insole is turned on, adequately charged, and working correctly. There were no instances of a malfunction or discomfort to the participant. The same pair of shoes and insoles was used for each test day for each subject. Each pair of insoles was used in only one subject and they were cleaned with antiseptic spray for each day of testing.
Study Procedures
Participants were asked to bring their own sneakers and walking shoes to the first study visit and the shoe and insoles that fit most comfortably were used for all studies. All study participants were provided with normal thickness socks to wear at all study visits to ensure a consistent sock thickness across all participants and all visits.
Determining Thresholds
The investigators determined each participant’s vibratory noise perception threshold at the start of each study visit with a computer tablet and custom software that interfaced with the insoles. Each foot was tested separately with the subject standing on a template that was used to assure they were in the same position for each day of testing. The amplitude of vibratory noise was automatically ramped up or down until the participant stated that they could, or could no longer, feel the stimulation. This was done in multiple stages, gradually narrowing the boundary of sensation until a reproducible threshold was determined. Once the threshold values were obtained for each foot, the level of stimulation of each insole was set at 0, 70% or 85% of the threshold value, according to the randomization order. The same thresholds were used throughout a given visit day, but threshold values were reassessed at mid-session and at the conclusion of the study visit to compare with the daily baseline value.
Outcome Measures
Balance was assessed using a Kistler Type 9286B force plate (Kistler, Amherst, NY). Participants were asked to stand on a template on the force plate for a total of eight 1-minute trials, four with eyes open looking at a target “X” on the wall, and four with eyes closed. Trial order was randomized.
Gait was assessed with a 16-foot long pressure sensitive GaitRite mat and data analysis software (CIR Systems, Havertown, PA). Participants were asked to walk across the mat ten times at his/her normal preferred walking speed.
A Timed Up and Go Test (TUG)11 was performed by asking the participants to sit comfortably in a chair and timing, with a stopwatch, how long it took them to stand up and walk three meters, turn around, walk back, and sit down again. Participants were asked to perform five TUG trials at each testing session. In a healthy population of 265 older adults aged 76.4 ± 4.3 years, TUG times were normally distributed and averaged 9.5 ± 1.7 seconds12. They have high inter-rater reliability with an interclass correlation coefficient (ICC) of 0.9813. TUG scores are also related to falls12, 13, with both a sensitivity and specificity of 87%.
The balance, gait, and TUG testing procedures were conducted 3 times during each study visit. A rest period of one hour occurred between each testing session. A health history questionnaire was completed and height and weight were measured for each participant during the first rest period of visit 1.
Data Analysis
We examined the effect of each vibratory noise level on balance, gait, and timed up and go (TUG) tasks, controlling for their within-visit test session, using repeated measures linear mixed effects regression models (SAS, PROC MIXED) and Tukey’s post-hoc tests. We also assessed whether there was attenuation of the response over the course of a day by comparing the results of 3 within-day tests sessions, using similar models. Finally, we plotted the sensory thresholds for each test session and each test day and used similar models to assess whether there were any significant threshold changes over time. All models were adjusted for age. A p-value < 0.05 was considered statistically significant.
Balance Data Reduction
The key outcome measures of the balance tasks were derived from the center of pressure (COP) motion using MatLab (Mathworks, Natick, MA). Balance measures were calculated at each testing session for eyes open and eyes closed trials separately as an average of the four trials. The average of 3 or more trials has been shown to provide acceptable reliability of COP velocity and distance measures with ICCs of 0.70 or greater14. Sway speed was calculated by summing the distances between consecutive COP points and dividing by the total trial time of 60 seconds. Sway area was calculated as the area of the ellipse that encloses approximately 95% of the points on the COP sway path. The values for healthy elderly adults were previously reported to be 191 ± 125 mm2 for eyes open and 207 ± 152 mm2 for eyes closed15. Average sway in the mediolateral (ML) and anteroposterior (AP) directions were also calculated from zero-meaned data by averaging the absolute distance of excursion away from the origin in the x and y directions, respectively.
Gait Data
Gait variables were automatically calculated by the GaitRite software and confirmed using an analysis program in MatLab. Gait speed was calculated by dividing distance walked by time. Stride time was calculated separately for the right and left foot as the time between consecutive footfalls. Step width was calculated as the horizontal distance between the midpoint of each consecutive footfall. Double support time was calculated as the time within each stride that both feet were simultaneously in contact with the ground. Means and coefficients of variation (CV) were calculated using footfall data from all ten passes on the mat. CVs were calculated as the standard deviation divided by the mean multiplied by 100. Gait measures assessed 2 or more times with a similar gait mat in the Cardiovascular Health Study population (Mean age 79.4 ± 4.1 years), showed excellent test-retest reliability for gait speed (ICC=0.98) and fair to good reliabilities for gait variability measures (ICCs= 0.40–0.63)16.
TUG Analysis
The key outcome measure of the TUG task was the total time in seconds taken to complete each trial. The average of the five TUG trials at each testing session was used for analysis.
Results
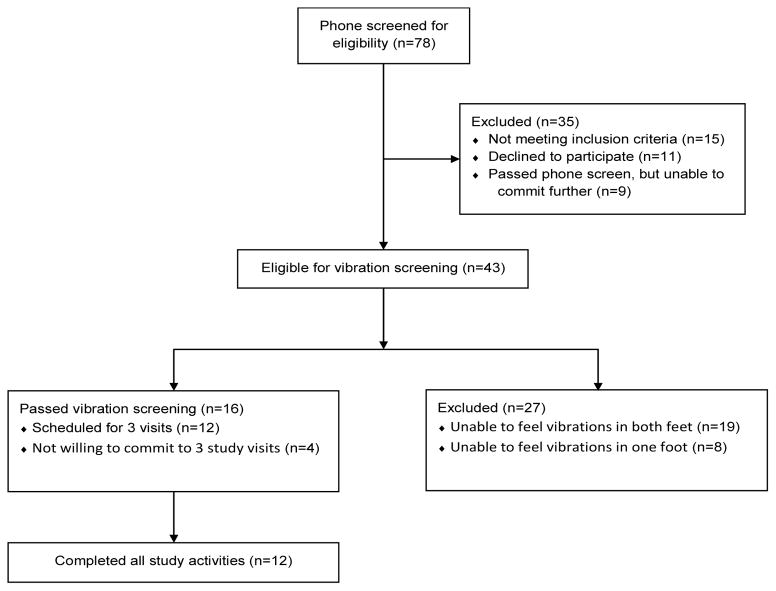
Recruitment
The process of recruitment is illustrated in Figure 2. Among 78 potential subjects who were screened over the phone for eligibility, 43 met our entry criteria and were willing to have a research assistant determine their ability to feel the vibrations delivered by the insoles. Of these, 27 were unable to sense the vibrations in one or both feet and were excluded from the study. Among the remaining 16, only 12 were willing to commit to three study visits. Table 1 shows the characteristics of these 12 individuals and the 27 who were unable to feel the vibrations at their highest amplitude. The 12 enrolled participants were younger and predominantly female compared to the 27 others.
Figure 2.
Study recruitment process.
Table 1.
Characteristics of eligible subjects who completed the study and those who were excluded because they could not perceive the maximal insole vibration.
| Characteristic | Completed Subjects (n=12) | Failed Vibration Screening (n=27) |
|---|---|---|
| Age (years), mean ± SD | 73.8 ± 8.1 | 79.3 ± 7.8 |
| 65–69, n (%) | 5 (41.7) | 4 (14.8) |
| 70–74, n (%) | 1 (8.3) | 5 (18.5) |
| 75–79, n (%) | 2 (16.7) | 1 (3.7) |
| 80–84, n (%) | 3 (25.0) | 9 (33.3) |
| 85–90, n (%) | 1 (8.3) | 8 (29.6) |
| Gender | ||
| Male, n (%) | 1 (8.3) | 8 (29.6) |
| Female, n (%) | 11 (91.7) | 19 (70.4) |
| Race | ||
| African-American, n (%) | 3 (25) | Not available |
| White, n (%) | 9 (75) | Not available |
| Height (cm), mean ± SD | 158.1 ± 10.3 | Not available |
| Weight (lb), mean ± SD | 147.5 ± 29.6 | Not available |
| BMI, mean ± SD | 26.7 ± 4.5 | Not available |
| Education, number (%) with > high school | 9 (75) | Not available |
Effect of Vibratory Noise on Balance, Mobility and Locomotor Control
Table 2 shows the effect of vibratory noise on selected balance measures. Most of these measures improved with noise at both 70% and 85% of the sensory threshold. The average elliptical area of postural sway with eyes open and closed was reduced significantly by the vibratory noise, as was average mediolateral sway with eyes open and closed. The response was similar for both noise amplitudes, except for the area of the ellipse with eyes closed, which did not differ from sham stimulation at the 85% noise level.
Table 2.
The effect of vibratory stimulation level on balance when standing with eyes open and eyes closed
| Outcome Variable | Mean for Each Stimulation Level (95% CI Lower, CI Upper) | P value* | ||
|---|---|---|---|---|
| 0% | 70% | 85% | ||
| Sway speed, EO (mm/s) | 12.31 (10.45, 14.17) | 12.00 (10.14,13.85) | 12.11 (10.25, 13.97) | 0.49 |
| Sway speed, EC (mm/s) | 19.62 (14.60, 24.65) | 18.75 (13.73, 3.77) | 19.47 (14.45, 24.50) | 0.14 |
| Area ellipse, EO (mm2) | 190.8 (150.8, 230.9)a | 156.2 (116.2, 6.3)b | 159.9 (119.8, 99.9)b | <0.01 |
| Area ellipse, EC (mm2) | 248.6 (196.7, 300.6)a | 217.8 (165.9, 269.8)b | 235.0 (183.0, 286.9)ab | 0.02 |
| ML average sway, EO (mm) | 2.63 (2.26, 2.99)a | 2.29 (1.92, 2.66)b | 2.37 (2.01, 2.74)b | 0.01 |
| ML average sway, EC (mm) | 2.83 (2.37, 3.29)a | 2.70 (2.12, 3.04)b | 2.58 (2.24, 3.16)b | 0.04 |
| AP average sway, EO mm) | 3.90 (3.44, 4.36) | 3.76 (3.29, 4.22) | 3.63 (3.17, 4.10) | 0.11 |
| AP average sway, EC (mm) | 4.76 (4.15, 5.37) | 4.58 (3.97, 5.19) | 4.79 (4.18, 5.40) | 0.27 |
Abbreviations: EO = Eyes Open; EC = Eyes Closed; ML = Mediolateral; AP = Anteroposterior.
Superscripts represent homogeneous groups within each row and are derived from Tukey’s post hoc testing for models with a significant main effect of stimulation level. Means with different superscript are significantly different from each other.
P values reflect the effect of stimulation level on each dependent variable. No significant interactions between stimulation level and test session were observed.
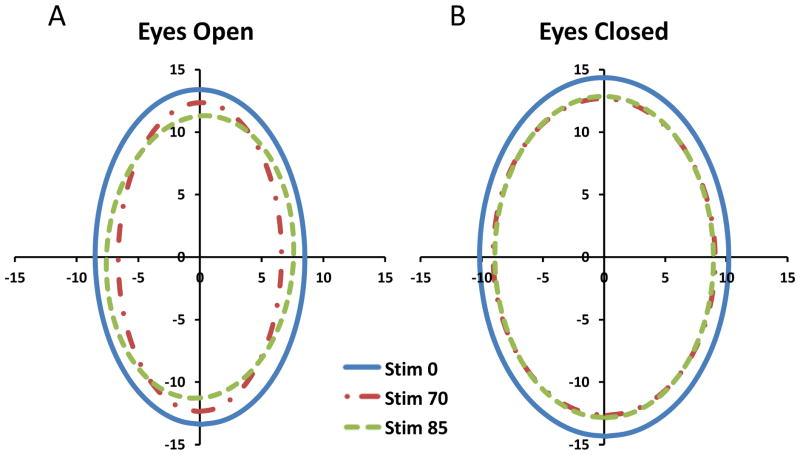
Figure 3 shows the average area of the ellipse for a representative subject with eyes open and closed during testing at the 3 vibration levels. One can see that the ellipse encircling 95% of the center of pressure excursions during both 70% and 85% noise amplitudes is smaller than when no vibration was delivered by the insoles. There were no statistically significant effects of vibration on the magnitude of anteroposterior sway or sway speed.
Figure 3. Effects of subsensory vibratory stimulation on ellipse area of center of pressure for one subject.
Subsensory vibratory stimulation reduced the magnitude of postural sway. (A) For subject with eyes open, area of ellipses for stimulation levels of 0%, 70%, and 85% were 357 mm2, 257 mm2, and 269 mm2, respectively. (B) For subject with eyes closed, area of ellipses for stimulation levels of 0%, 70%, and 85% were 459 mm2, 362 mm2, and 361 mm2, respectively.
Table 3 shows the results for the TUG test, walking speed, and selected gait variables. The TUG time was significantly reduced by both levels of vibratory noise. Also, the noise stimulation significantly reduced the variance in most gait measures. The coefficients of variation (CV) for stride time, step width, and double support times were significantly reduced by both levels of vibratory noise. However, mean walking speed, step width, and double support time were not changed significantly. There was a small, marginally significant effect on mean stride time in the right and left leg.
Table 3.
The effects of vibratory stimulation level on mobility and locomotor control
| Outcome Variable | Mean for Each Stimulation Level (CI Lower, CI Upper) | P value* | ||
|---|---|---|---|---|
| 0% | 70% | 85% | ||
| TUG (s) | 9.75 (9.01, 10.49)a | 9.44 (8.70, 10.18)b | 9.34 (8.60, 10.08)b | <0.01 |
| Gait variable means | ||||
| Gait speed (cm/s) | 122.9 (114.1, 131.7) | 124.5 (115.7, 133.4) | 124.6 (115.8, 133.5) | 0.29 |
| Stride time, right foot (s) | 1.038 (1.008, 1.067) | 1.026 (0.996, 1.055) | 1.026 (0.997, 1.056) | 0.08 |
| Stride time, left foot (s) | 1.038 (1.009, 1.068)a | 1.025 (0.996, 1.055b | 1.025 (0.996, 1.055)b | 0.04 |
| Step width, mean (cm) | 64.84 (61.51, 68.17) | 65.08 (61.74, 68.41) | 65.19 (61.86, 68.52) | 0.60 |
| Double support (s) | 0.305 (0.277, 0.334) | 0.304 (0.275, 0.333) | 0.306 (0.277, 0.334) | 0.91 |
| Gait variable CV (% of mean) | ||||
| Stride time, right foot | 2.65 (2.43, 2.87)a | 2.31 (2.09, 2.54)b | 2.27 (2.05, 2.49)b | <0.01 |
| Stride time, left foot | 2.83 (2.61, 3.06)a | 2.32 (2.10, 2.55)b | 2.42 (2.20, 2.65)b | <0.01 |
| Step width | 3.83 (3.35, 4.30) | 3.48 (3.01, 3.95) | 3.46 (2.99, 3.93) | 0.12 |
| Double support | 8.36 (7.39, 9.33)a | 6.45 (5.48, 7.42)b | 6.49 (5.52, 7.47)b | <0.01 |
Abbreviations: TUG = Time Up and Go; CV = Coefficients of Variation.
Superscripts represent homogeneous groups within each row and are derived from Tukey’s post hoc testing for models with a significant main effect of stimulation level. Means with different superscript are significantly different from each other.
P values reflect the effect of stimulation level on each dependent variable. No significant interactions between stimulation level and test session were observed.
Stability of Sensory Thresholds
Figure 4 displays the threshold values for each participant’s right and left foot at each visit and test session. Overall, there were no significant differences in thresholds across test sessions within a test day, and only a marginally significant difference between test days for the left foot (P=0.05).
Figure 4.
Threshold values for each subject across each visit and testing session. Left and right feet are plotted separately.
Effect of Different Vibratory Noise Amplitudes
As shown in Tables 2 and 3 there were no significant differences in the effect of the 70% and 85% vibration levels on the balance, gait, and TUG measures. Furthermore, there were no interactions between vibration level and test session for the TUG or any of the balance or gait variables, indicating that the effects of a given vibration level did not change over the course of the day.
Discussion
In response to our four initial research questions, the results of this study demonstrate that: 1) the vibratory insoles significantly improved performance on the timed up-and-go test, reduced the area of postural sway, and reduced the temporal variability of walking; 2) the therapeutic effect of the insoles persisted throughout the course of a day; 3) vibratory sensation thresholds remained relatively stable within and across study days; and 4) vibratory stimulation at 70% and 85% of the sensory threshold had similar effects on standing balance, mobility, and locomotor control.
The predominant effects of the vibratory noise stimulation on the variability of gait characteristics, rather than temporal or dimensional measures of speed, length, or width, are supported by our previous study that utilized a high-voltage vibratory tactor embedded into a sandal10. These findings are consistent with improvements in sensory feedback to centers in the brain and spinal cord that control the rhythmicity of movement. A previous study of patients with peripheral neuropathy by Wuehr et al17 demonstrated that chronic foot sole sensory impairments are associated with a cautious gait pattern characterized by reduced walking speed, increased gait variability, and prolonged double support time. Manor et al18 further demonstrated that these individuals walk with greater stride time variability across a range of walking speeds, suggesting that such sensory impairments independently disrupt gait rhythmicity. It therefore stands to reason that increased foot sole sensation would improve these functions. Our study demonstrated improvements in gait variability and double support time, but not gait speed – possibly because of our small sample size and limited statistical power. However, the reduction in TUG times suggests that mobility might also be favorably affected. Consistent with our findings, previous work by Dingwell et al19 suggests that sensory feedback may have a greater impact on stride-to-stride gait variability than on mean measures of locomotor performance.
The improvement in mediolateral, rather than anteroposterior sway may be due to larger variance in AP sway and insufficient statistical power to detect a true difference. However, a previous study by Bernard-Demanze et al 20 demonstrated that in older adults with impaired foot sole sensation, a single bout of supra-threshold 5Hz mechanical vibration to the foot soles significantly reduced the magnitude of standing postural sway when the vibration was applied, yet only along the mediolateral axis. The control of mediolateral sway may therefore be particularly sensitive to changes in cutaneous somatosensory function. Since increased sway in the lateral direction has been shown to be associated with falls21, the improvement shown in our study may have particular significance for the prevention of falls.
Study Limitations
There are several limitations to this study. Our sample size was limited by the large proportion of subjects who could not feel the stimulation at its maximal level, making it impossible to determine a sensory threshold and set the vibration below it. Furthermore, a majority of our subjects were women. We suspect that heavier male subjects might have clamped the piezo-electric vibrators, reducing the amplitude of vibration. Unfortunately, our study may not be generalizable to more frail elderly subjects who could benefit therapeutically from this device. Current work is being devoted to increasing the amplitude of vibration in the insole, in order to permit broader clinical application to patients with sensory impairment.
Conclusions
The results of this study provide proof of concept that the application of the principle of stochastic resonance to the foot sole sensory system using a new low voltage piezoelectric technology can improve various measures of balance and gait that are associated with falls. Furthermore, there appears to be a wider range of effective vibratory noise amplitudes than previously thought, ranging from 70% to 90% of the sensory thresholds. This greatly simplifies setting the therapeutic stimulation level of the insole device. The relative stability of sensory thresholds within and between days also implies that the stimulation range can be set at infrequent intervals, rather than hourly or daily.
Acknowledgments
Supported by a grant from MSD, Memphis, TN, and grant AG025037 from the National Institute on Aging, Bethesda, MD. Dr. Lipsitz holds the Irving and Edyth S. Usen and Family Chair in Geriatric Medicine at HSL.
References
- 1.Centers for Disease Control and Prevention NCfIPaC, Division of Unintentional Injury Prevention. Falls Among Older Adults: An Overview. 2008. [Google Scholar]
- 2.Forrest G, Huss S, Patel V, et al. Falls on an inpatient rehabilitation unit: risk assessment and prevention. Rehabil Nurs. 2012;37:56–61. doi: 10.1002/RNJ.00010. [DOI] [PubMed] [Google Scholar]
- 3.Richardson JK, Ashton-Miller JA. Peripheral neuropathy: an often-overlooked cause of falls in the elderly. Postgrad Med. 1996;99:161–72. [PubMed] [Google Scholar]
- 4.Richardson JK, Hurvitz EA. Peripheral neuropathy: a true risk factor for falls. J Gerontol A Biol Sci Med Sci. 1995;50:M211–5. doi: 10.1093/gerona/50a.4.m211. [DOI] [PubMed] [Google Scholar]
- 5.Thurman DJ, Stevens JA, Rao JK. Practice parameter: Assessing patients in a neurology practice for risk of falls (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2008;70:473–9. doi: 10.1212/01.wnl.0000299085.18976.20. [DOI] [PubMed] [Google Scholar]
- 6.Collins JJ, Imhoff TT, Grigg P. Noise-enhanced tactile sensation. Nature. 1996;383:770. doi: 10.1038/383770a0. [DOI] [PubMed] [Google Scholar]
- 7.Sejdic E, Lipsitz LA. Necessity of noise in physiology and medicine. Comput Methods Programs Biomed. 2013;111:459–70. doi: 10.1016/j.cmpb.2013.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Priplata AA, Niemi JB, Harry JD, Lipsitz LA, Collins JJ. Vibrating insoles and balance control in elderly people. Lancet. 2003;362:1123–4. doi: 10.1016/S0140-6736(03)14470-4. [DOI] [PubMed] [Google Scholar]
- 9.Priplata AA, Patritti BL, Niemi JB, et al. Noise-enhanced balance control in patients with diabetes and patients with stroke. Ann Neurol. 2006;59:4–12. doi: 10.1002/ana.20670. [DOI] [PubMed] [Google Scholar]
- 10.Galica AM, Kang HG, Priplata AA, et al. Subsensory vibrations to the feet reduce gait variability in elderly fallers. Gait Posture. 2009;30:383–7. doi: 10.1016/j.gaitpost.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 12.Herman T, Giladi N, Hausdorff JM. Properties of the ‘timed up and go’ test: more than meets the eye. Gerontology. 2011;57:203–10. doi: 10.1159/000314963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80:896–903. [PubMed] [Google Scholar]
- 14.Golriz S, Hebert JJ, Foreman KB, Walker BF. The reliability of a portable clinical force plate used for the assessment of static postural control: repeated measures reliability study. Chiropr Man Therap. 2012;20:14. doi: 10.1186/2045-709X-20-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prieto TE, Myklebust JB, Hoffmann RG, Lovett EG, Myklebust BM. Measures of postural steadiness: differences between healthy young and elderly adults. IEEE Trans Biomed Eng. 1996;43:956–66. doi: 10.1109/10.532130. [DOI] [PubMed] [Google Scholar]
- 16.Brach JS, Perera S, Studenski S, Newman AB. The reliability and validity of measures of gait variability in community-dwelling older adults. Arch Phys Med Rehabil. 2008;89:2293–6. doi: 10.1016/j.apmr.2008.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wuehr M, Schniepp R, Schlick C, et al. Sensory loss and walking speed related factors for gait alterations in patients with peripheral neuropathy. Gait Posture. 2014;39:852–8. doi: 10.1016/j.gaitpost.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 18.Manor B, Wolenski P, Li L. Faster walking speeds increase local instability among people with peripheral neuropathy. J Biomech. 2008;41:2787–92. doi: 10.1016/j.jbiomech.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 19.Dingwell JB, Cusumano JP, Sternad D, Cavanagh PR. Slower speeds in patients with diabetic neuropathy lead to improved local dynamic stability of continuous overground walking. J Biomech. 2000;33:1269–77. doi: 10.1016/s0021-9290(00)00092-0. [DOI] [PubMed] [Google Scholar]
- 20.Bernard-Demanze L, Vuillerme N, Ferry M, Berger L. Can tactile plantar stimulation improve postural control of persons with superficial plantar sensory deficit? Aging Clin Exp Res. 2009;21:62–8. doi: 10.1007/BF03324900. [DOI] [PubMed] [Google Scholar]
- 21.Lord SR, Rogers MW, Howland A, Fitzpatrick R. Lateral stability, sensorimotor function and falls in older people. J Am Geriatr Soc. 1999;47:1077–81. doi: 10.1111/j.1532-5415.1999.tb05230.x. [DOI] [PubMed] [Google Scholar]