Abstract
Background and Aims:
Catheter-associated urinary tract infection (CAUTI) is one of the most common health care acquired infection encountered in clinical practice. The present study was planned to assess the knowledge and attitude of health care providers regarding the indications for catheterization and methods of preventing CAUTI.
Methods:
A prospective questionnaire-based survey was done from March 2011 to August 2011. A structured questionnaire comprising of 41 items related to demographic details of the respondents, their knowledge regarding indications for catheterization and methods of preventing CAUTI was given to 54 doctors and 105 nurses. The response was evaluated for statistical correlation using a computer software.
Results:
The mean years of experience of the respondents in the health care setup was 6.8 years. Only 57% of the respondents could identify all the measures for prevention of CAUTI. The knowledge regarding the indication for catheterization though suboptimal was significantly better amongst the doctors as compared to nurses.
Conclusion:
The knowledge regarding indication and preventive measures was suboptimal in our study group. There is a tremendous scope of improvement in catheterization practices in our hospital and education induced intervention would be the most appropriate effort toward reducing the incidence of CAUTI.
Keywords: Catheter, health care personnel, knowledge, prevention, urinary tract infection
Introduction
The most common hospital-acquired infection is catheter-associated urinary tract infection (CAUTI) accounting for almost 40% of all the nosocomial infections. [1,2] The single most important predisposing factor for CAUTI is the insertion of urinary catheter. [1,2] Urinary (Foley) catheters are used very frequently in hospitalized patients, and almost 25% of them undergo urinary catheterization during their stay in the hospital. [3,4] The frequency of urinary catheterization in Intensive Care Unit (ICU) can range as high as 100%. [5]
Catheter-associated urinary tract infection produces substantial morbidity in hospitalized patients including discomfort, fever, malaise and unnecessary antibiotic use, which may become an important source of antibiotic resistant organisms. Further, the catheterized urinary tract acts as a reservoir for the dissemination of these drug resistant organisms to other patients. [3,6]
There are increased chances of catheter blockage, urinary tract stones and even increased risk of malignancy of the urinary tract following CAUTI. If it gets complicated by bacteremia, it increases the cost of care tremendously besides increasing the mortality in these hospitalized patients. [6,7]
Most doctors and nurses are unfamiliar with the indication of catheterization and further there is no defined management plan to monitor the presence of unnecessary catheter.
The incidence of CAUTI is directly proportional to the number of catheter days. Since the number of catheter days in ICU setting is more, the frequency of CAUTI is expected to be higher. But many studies have shown similar rates of CAUTI in the ICU and non ICU patients. [8,9] This shows that all hospitalized patients including non ICU patients are an important group for surveillance and prevention of CAUTI.
Many studies have shown that single most important modifiable risk factor for decreasing the incidence of CAUTI is reducing unnecessary catheter use. [4,10]
Preventive measures such as catheter reminders for removing the catheter as soon as possible restrict the number of catheter days and thus lead to decreased incidence of CAUTI. [10,11]
Most hospitals do not have strict guidelines for the prevention of CAUTI. Training the health care personnel and introducing the prevention of CAUTI as a high priority in hospitals is strongly associated with decreased incidence of CAUTI. [10,11]
There are limited studies from India, which have assessed the knowledge of health care personnel regarding indication for catheterization and methods to prevent CAUTI. The present study was planned to assess the knowledge of various health care personnel regarding indication for catheterization and measures to prevent CAUTI. The study also assessed the attitude of health care provider (HCP) regarding CAUTI.
Methods
A structured questionnaire consisting of 41 items was developed specially for this study. The questions regarding the indication for catheterization and measures for prevention of CAUTI were taken as per Centers for Disease Control (CDC) guidelines. [2] The content of the questionnaire was given independently to all the authors for assessing the simplicity of questions, clarity of language, accuracy and adequacy of questions for the purpose of the study. The survey covered demographic details of the respondents including age, sex, qualification, designation years of experience in health care setup after obtaining graduation and area of posting. The contents of the questionnaire were designed to assess the knowledge of the health care professionals regarding indication for catheter use (10 questions) and the methods of preventing CAUTI (15 questions) in a catheterized patient. The questionnaire also included 10 questions to assess the attitude of HCP regarding CAUTI.
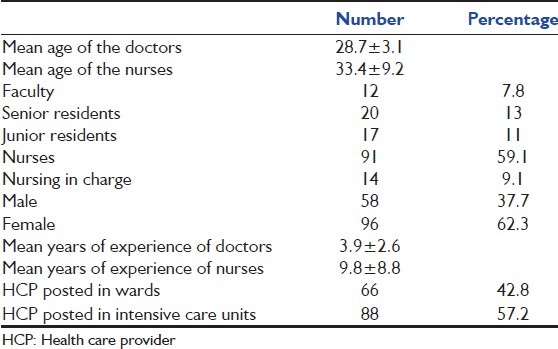
Knowledge regarding indication for catheter insertion was assessed by asking the respondents to grade their answers on a 4 point scale (4: Almost always indicated, 3: Sometimes indicated, 2: Rarely indicated, 1: Never indicated) they were given 10 situations in which they had to grade their answers [Table 1].
Table 1.
Demographic details of the study group (n=154; 49: Doctors; 105: Nurses)
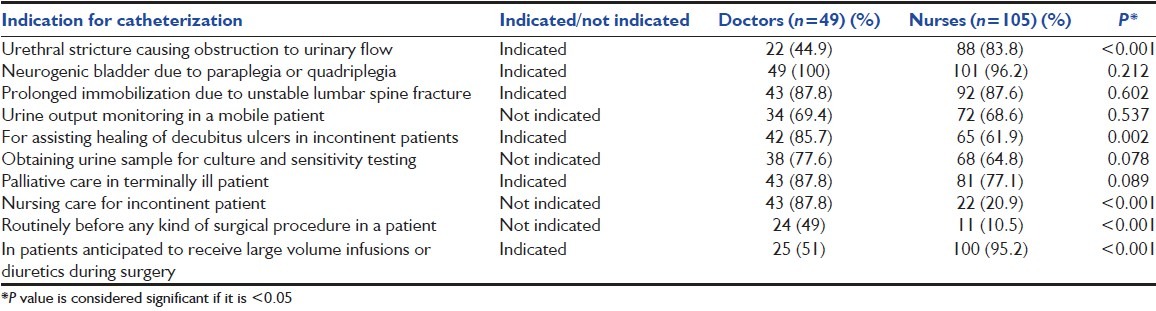
Knowledge regarding the methods to prevent CAUTI included 15 methods [Table 2]. The respondents had to grade their answers on a 4 point scale (4: Large effect, 3: Moderate effect, 2: Some Effect, 1: No effect). The answers for both the indication and prevention of CAUTI were compared with the CDC guidelines. [2] For evaluating the indication for catheterization, the scaled responses were transformed into dichotomous variables. The response almost, always and sometimes indicated, was taken as appropriate for the indication and the response of rarely and not indicated was taken as appropriate for nonindication. For evaluating the preventive measures, the scaled responses were again transformed into dichotomous variables. The response of large effect and moderate effect were taken as effective, and that of some effect or no effect were taken as noneffective.
Table 2.
Frequency of respondents having identified the indications correctly
There were 10 questions to assess the attitude and the answers had to be given as whether they agree or disagree with the statements. This was not compared with any reference, and the format of the questionnaire was designed to be used for this study.
Statistical analysis
The data were compiled and analyzed using SPSS for windows version 12.0. Various statistical test used were simple frequency table, Chi-square test, Fischer's exact t-test for significance and univariate analysis for testing the correlation.
Results
In the present study, 154 health care personnel (doctors = 49 and nurses = 105) out of the 180 participants completed a questionnaire and were included in the study. The response rate in the present study was thus 85.5%. The mean age of the study group was 31.9 years (range: 23–59) and the mean years of experience was 7.94 years (range: 1–36). The demographic details of the study group are described in Table 1.
Though doctors had significantly higher knowledge as compared to nurses regarding various indications for catheterization, more than half of the doctors could not identify important indications such as urethral stricture or in patients receiving large volume infusions during surgery [Table 2]. More than one-third of the respondents identified urine output monitoring in a mobile patient or even obtaining a urine sample for culture sensitivity as a valid indication for catheterization [Table 2].
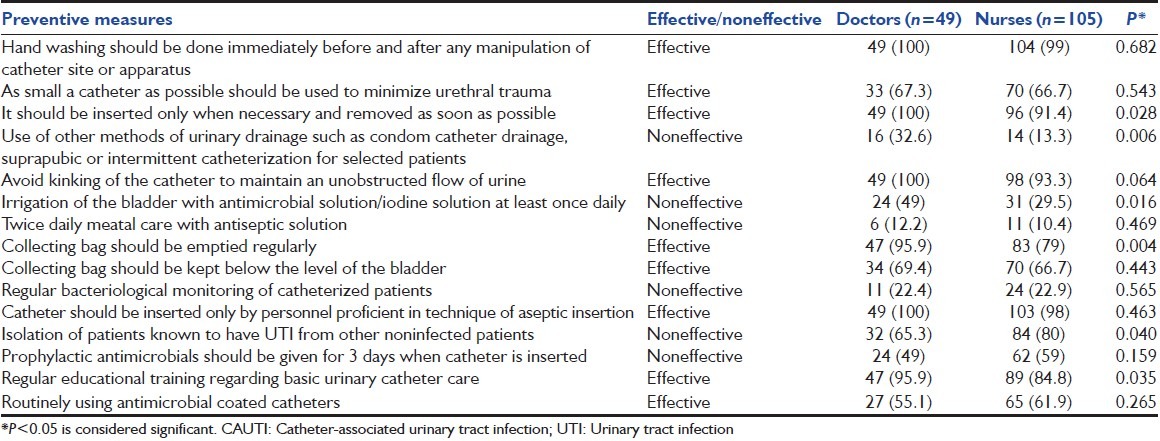
Knowledge regarding various preventive measures was suboptimal in the study group. Most respondents could not correctly identify noneffective measures such as bladder irrigation or twice daily meatal care. In general, the HCP could not differentiate the effective measures from noneffective ones [Table 3].
Table 3.
Number of doctors and nurses correctly identifying methods to prevent CAUTI
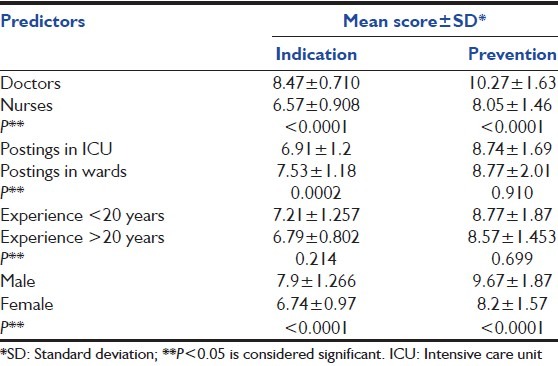
Doctors had significantly better knowledge than nurses regarding the indications of catheterization and preventive measures for CAUTI [Table 4]. HCP posted in high-risk areas such as ICUs had significantly better knowledge than the HCP posted in wards regarding various indications, but there was no difference in their awareness in respect to preventive measures [Table 4]. Experience had no effect on the knowledge regarding indication for catheterization and preventive measures.
Table 4.
Univariate predictors of indications of catheterization
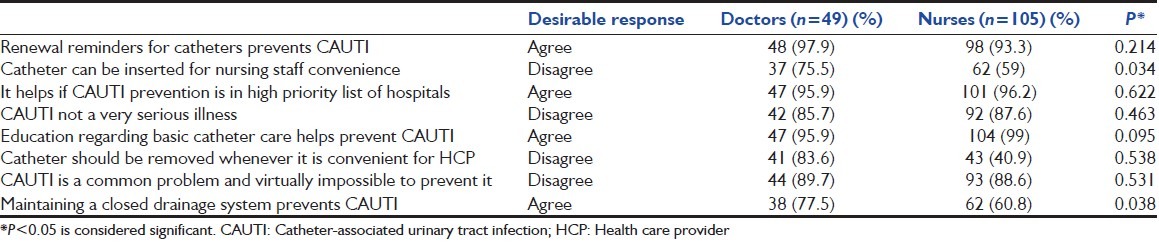
Most of the HCP felt that including prevention of CAUTI as a high priority in the hospitals and use of renewal reminders would definitely help in preventing CAUTI. More than 90% of the HCP also felt that education regarding basic catheter care would also help prevent CAUTI [Table 5]. Almost 40% of the nurses and 25% of the doctors felt that catheters could be inserted even for nursing convenience. Nearly, 10% of the respondents showed hopelessness regarding prevention of CAUTI [Table 5].
Table 5.
Attitudes of doctors and nurses regarding urinary cauterization practices
Discussion
Urinary catheters once inserted in the hospitalized patients tend to remain in place even after the indication for its use ends. [12] This leads to CAUTI being one of the most common health care associated infection. [1,2] The most important preventive measure for decreasing the incidence of CAUTI is limiting catheter use. [13] This is possible only if the HCP has adequate knowledge regarding the appropriate indications for inserting urinary catheters. We assessed the knowledge of doctors and nurses regarding indication for catheterization to help manage the problem of inappropriate catheterization and CAUTI.
Overall the knowledge of doctors was significantly better than nurses in identifying the indications for catheterization (P < 0.05). Since in our facility doctors decide on the catheterization protocol, they would be more aware regarding the indications. Educating nurses regarding indications for catheterization will help prevent CAUTI as they could remind the doctors on removing catheters as soon as the indication for catheterization ends. This finding is consistent with other observers in that nurse's daily determination for the need of catheter in a patient helps reduce the incidence of CAUTI. [10,13,14]
Failure to identify the appropriate indications for catheterization would lead to unnecessary catheter use. Almost 79% of the nurses and 12% of the doctors justified the use of catheters for nursing care of incontinent patients. Almost one-third of the respondents justified the use of catheters for routinely obtaining urine samples for culture and sensitivity testing and for urine output monitoring even in mobile patients. This lack of knowledge regarding various indications itself points toward increased catheter usage. It would be worthwhile educating both doctors and nurses regarding the various indications for catheterization as this can keep a check on unnecessary catheter use. [13,14]
Knowledge regarding various preventive measures was also suboptimal in the study group. The health care personnel could not identify the preventive measures, which are less effective or noneffective. Being over cautious is better than being ignorant but this lack of knowledge regarding preventive measures may lead to wastage of time on unimportant issues at the cost of truly effective measures. A complete knowledge regarding all effective preventive measures would help them prioritize the care of the urinary catheters.
Almost 77% (119/154) of the HCP felt that regular bacteriological monitoring is effective for prevention of CAUTI. This causes increased costs of treatment for the patients in addition to increasing sample load in the laboratories. Almost 45% (68/154) of the HCP felt that prophylactic antimicrobials for 3 days can prevent CAUTI.
This is ineffective besides exposing the patients to unnecessary antibiotics and selecting out on antibiotic resistant organisms. In spite of the fact that nurses are involved with routine catheter care in our setup, more than one-third of the nurses did not know that the urinary collection bag should be below the level of the bladder and it should be emptied regularly to allow unobstructed urine flow. These seemingly simple measures can have a major effect in the prevention of CAUTI. [2,10,11,12]
Almost 25% (38/154) of the HCP felt that isolation of the patient helps in preventing CAUTI. If they follow this practice, it will lead to emotional, social stress in the patients. Thus, appropriate knowledge regarding all preventive measure would save on cost and time and would help in more efficient patient care. The knowledge regarding the correct preventive measures can be imparted through educational training and reinforcement thereafter.
In our study, females were more aware regarding the indications and preventive measures. This could also be because in our setup maximum number of nurses are females. We also observed that experience had no effect on awareness levels, and knowledge in one domain did not affect the awareness levels in another domain. The findings are similar to those of other studies. [14,15] The study again reiterates the finding that educating the HCP regarding indications and preventive measures will help them do evidence-based practice. [10,14,15]
More than 95% of the HCP felt that hospitals focusing on prevention of CAUTI as a high priority and use of urinary catheter reminders would help in preventing CAUTI.
Despite this, most of the hospitals in India have not implemented any defined strategy for prevention of CAUTI. The finding is in agreement with other observers and even in many developed nations many hospitals do not have any protocol to monitor the number of catheterization and duration of catheterization. [11,16] Less than 10% of the hospitals used renewal reminders. [11,16]
Most of the HCP also felt the need for education regarding basic catheter care for prevention of CAUTI. Thus, despite the need being felt for these measures, the implementation was lacking at various levels including organizational levels.
Almost 10% of the HCP felt that it was virtually impossible to prevent CAUTI. This hopelessness can be improved by educating them and showing them the definite evidences of prevention of CAUTI following appropriate preventive measures.
Multifaceted interventions in the form of routine educational trainings to HCP regarding CAUTI and its prevention, Implementation of catheter reminder system to discontinue unnecessary catheters, changes in the hospital policies would definitely help in reducing unnecessary catheter use, decrease the number of catheter days, and thus reduce the incidence of CAUTI.
Surveillance of the incidence of CAUTI on a regular basis in all the hospitals would be desirable to initiate preventive measures as early as required.
Conclusion
Catheter-associated urinary tract infection is one of the most common health care associated infections. It is largely preventable if indications for catheterization, methods for catheter care and other preventive measures are followed diligently. In the present study, it was seen that though doctors had significantly better awareness than nursing staff regarding reasons for urinary catheter indication and preventive measures, yet it was suboptimal and had a lot of scope of improvement. Further, it was observed that CAUTI was not thought of as a serious problem.
All the health care personnel including the doctors should have regular training regarding prevention of CAUTI, and all efforts should be made by hospital authorities to include prevention of CAUTI in its high priority list. Surveillance of the incidence of CAUTI would also be helpful in recording the improvement observed as a result of these education based and administrative interventions.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Warren JW. Catheter-associated urinary tract infections. Int J Antimicrob Agents. 2001;17:299–303. doi: 10.1016/s0924-8579(00)00359-9. [DOI] [PubMed] [Google Scholar]
- 2.Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:625–63. doi: 10.1086/650482. [DOI] [PubMed] [Google Scholar]
- 3.Warren JW. The catheter and urinary tract infection. Med Clin North Am. 1991;75:481–93. doi: 10.1016/s0025-7125(16)30465-5. [DOI] [PubMed] [Google Scholar]
- 4.Brennan ML, Evans A. Why catheterize.: Audit findings on the use of urinary catheters? Br J Nurs. 2001;10:580–90. doi: 10.12968/bjon.2001.10.9.9389. [DOI] [PubMed] [Google Scholar]
- 5.Datta P, Rani H, Chauhan R, Gombar S, Chander J. Health-care-associated infections: Risk factors and epidemiology from an intensive care unit in Northern India. Indian J Anaesth. 2014;58:30–5. doi: 10.4103/0019-5049.126785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Getliffe K, Newton T. Catheter-associated urinary tract infection in primary and community health care. Age Ageing. 2006;35:477–81. doi: 10.1093/ageing/afl052. [DOI] [PubMed] [Google Scholar]
- 7.Stickler DJ, Zimakoff J. Complications of urinary tract infections associated with devices used for long-term bladder management. J Hosp Infect. 1994;28:177–94. doi: 10.1016/0195-6701(94)90101-5. [DOI] [PubMed] [Google Scholar]
- 8.Lewis SS, Knelson LP, Moehring RW, Chen LF, Sexton DJ, Anderson DJ. Comparison of non-intensive care unit (ICU) versus ICU rates of catheter-associated urinary tract infection in community hospitals. Infect Control Hosp Epidemiol. 2013;34:744–7. doi: 10.1086/671000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weber DJ, Sickbert-Bennett EE, Gould CV, Brown VM, Huslage K, Rutala WA. Incidence of catheter-associated and non-catheter-associated urinary tract infections in a healthcare system. Infect Control Hosp Epidemiol. 2011;32:822–3. doi: 10.1086/661107. [DOI] [PubMed] [Google Scholar]
- 10.Fakih MG, Dueweke C, Meisner S, Berriel-Cass D, Savoy-Moore R, Brach N, et al. Effect of nurse-led multidisciplinary rounds on reducing the unnecessary use of urinary catheterization in hospitalized patients. Infect Control Hosp Epidemiol. 2008;29:815–9. doi: 10.1086/589584. [DOI] [PubMed] [Google Scholar]
- 11.Saint S, Kowalski CP, Kaufman SR, Hofer TP, Kauffman CA, Olmsted RN, et al. Preventing hospital-acquired urinary tract infection in the United States: A national study. Clin Infect Dis. 2008;46:243–50. doi: 10.1086/524662. [DOI] [PubMed] [Google Scholar]
- 12.Apisarnthanarak A, Rutjanawech S, Wichansawakun S, Ratanabunjerdkul H, Patthranitima P, Thongphubeth K, et al. Initial inappropriate urinary catheters use in a tertiary-care center: Incidence, risk factors, and outcomes. Am J Infect Control. 2007;35:594–9. doi: 10.1016/j.ajic.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 13.Elpern EH, Killeen K, Ketchem A, Wiley A, Patel G, Lateef O. Reducing use of indwelling urinary catheters and associated urinary tract infections. Am J Crit Care. 2009;18:535–41. doi: 10.4037/ajcc2009938. [DOI] [PubMed] [Google Scholar]
- 14.Apisarnthanarak A, Thongphubeth K, Sirinvaravong S, Kitkangvan D, Yuekyen C, Warachan B, et al. Effectiveness of multifaceted hospitalwide quality improvement programs featuring an intervention to remove unnecessary urinary catheters at a tertiary care center in Thailand. Infect Control Hosp Epidemiol. 2007;28:791–8. doi: 10.1086/518453. [DOI] [PubMed] [Google Scholar]
- 15.Drekonja DM, Kuskowski MA, Johnson JR. Internet survey of Foley catheter practices and knowledge among Minnesota nurses. Am J Infect Control. 2010;38:31–7. doi: 10.1016/j.ajic.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 16.Saint S, Kowalski CP, Forman J, Damschroder L, Hofer TP, Kaufman SR, et al. A multicenter qualitative study on preventing hospital-acquired urinary tract infection in US hospitals. Infect Control Hosp Epidemiol. 2008;29:333–41. doi: 10.1086/529589. [DOI] [PubMed] [Google Scholar]


