Abstract
Since 2011 we have taught a public health innovations course at the University of California, Berkeley. Students gain skills in systematic innovation, or human-centered design, while working in small interdisciplinary teams on domestic and global health projects with client organizations.
To support acquisition of meaningful problem-solving skills, we structured the course so that the majority of learning happens in scenarios that do not involve faculty. Taken by students representing 26 graduate programs (as diverse as epidemiology, city planning, and mechanical engineering), it is one of the 10 highest-rated courses offered by the School of Public Health.
We present the blueprints for our course with the hope that other institutions whose students could benefit will borrow from our model.
On a recent April evening in Berkeley, California, 29-year-old Aileen Suzara—her hair wrapped neatly in a multicolored, tartan bandana—stood at the center of the kitchen at La Peña Cultural Center, reviewing final instructions with a team of eight that was responsible for preparing and serving dinner to more than 100 guests. Dozens of customers who had prepaid for an opportunity to sample Chef Suzara’s creations were already waiting on the sidewalk outside La Peña. For this one night, a pop-up restaurant named Sariwa—meaning fresh in Tagalog—would create a space in which these customers could experience farm-fresh, seasonal food influenced by both Filipino and American cuisine and talk about healthy Filipino food.
Such pop-up (temporary) restaurants are not unusual in the San Francisco Bay Area. What was unusual was that this was an integral part of a public health course at the University of California, Berkeley. In addition to being a formally trained chef, Suzara was also a student in the Master of Public Health Nutrition program. The Sariwa pop-up was a prototype—a small-scale experiment—developed not just by Suzara, but by a team of students from the course Eat.Think.Design. They had spent the previous four months exploring the development of a new business venture anchored to the theme of revitalized Filipino cuisine. The core purpose of this venture was to improve population health by shifting the way that Filipino Americans eat and think about food.
We teach the course that acted as the incubator for Sariwa. In describing the development of the course and the students it targets, we hope that our course might serve as a model for other public health institutions interested in the innovation process.
HISTORICAL CONTEXT
The story of Eat.Think.Design. dates to 2010, when we began development of an experimental course at the University of California, Berkeley: Designing Innovative Public Health Solutions.1 The course debuted in spring 2011 and has been taught each of the three subsequent academic years. In 2014, a new thematic focus on food systems necessitated a rebranding to Eat.Think.Design.
A Lancet Commission, convened to discuss the education of health professionals in the 21st century, argued that educational transformation is critical to meet the public health problems we face in this century.2 Specifically, the commission called for a higher level of learning, moving beyond informative learning, which transmits knowledge to create experts, to transformative learning, which transmits leadership attributes to create agents who can successfully implement change. For the decade before we created our course, the School of Public Health worked diligently to create a leadership thread throughout the curriculum and developed linkages across the campus to support this, most notably with the Haas School of Business. During this period, the school experienced a rapid growth in global health content, driven by demand from students and faculty. The school also increased its emphasis on translation of evidence to action, including case studies and team projects.
The next big step in curriculum reform was to address the challenge of implementation—making changes that were sustainable because they made sense, scientifically, economically, and behaviorally. This led us to collaborate to develop a new course that matched an approach (systematic innovation) to a need (sustainable implementation).
The new course focused on systematic approaches to innovation in the context of complex public health issues. It pulled from human-centered design and design thinking, approaches that enable teams to systematically develop novel, effective solutions to complex problems.3 Human-centered design and design thinking have traditionally been applied to consumer challenges, but increasingly they are being used to address societal problems.4 Our course was about developing innovative solutions to existing challenges in public health. To be considered innovative, a solution would have to meet four criteria: (1) it would have to be novel, (2) it would have to be more cost effective than current approaches (not necessarily cheaper), (3) it would have to be implementable, and (4) it would have to have a reasonable likelihood of sustainability. Put more simply, our course would help students develop solutions that stick.
STUDENTS
We recognized early on that the course would derive much of its value from the students who composed each class. Design thinking requires cross-disciplinary inputs, so we opened recruitment up to all professional schools and disciplines in our Graduate Division. There is growing recognition inside and outside of public health of the value in such cross-disciplinary collaboration.5 It was important to us that cross-disciplinary intersections included disciplines outside of public health, not just its traditional components. We elected to limit enrollment to no more than 25 students to preserve opportunities for experiential learning in the classroom.
We also recognized that today’s students present new opportunities and challenges. Students in the 21st century are digitally competent. Their mastery of parallel processing and their agility with real-time information gathering are formidable. They challenge workplace and educational norms. Their attention span is shorter. Notably, they are more spontaneously collaborative. They eschew reading original research. Rather, they want it filtered. Many are satisfied with superficial understanding. To discover deeper understanding they have to be motivated to delve further, often with games and challenges. Our course has been designed to meet the needs of these students.
TEAM PROJECTS
The key substrate for learning in the class is a semester-long team project. Students work in groups of three on an innovation challenge posed by an organizational client. During the third week of the semester, students pitch projects derived from their own relationships with organizations that do not yet have a tie to the class. Students rank their project preferences and are matched to projects on the basis of a combination of individual preference and team diversity. Only two thirds of projects pitched are actually matched, ensuring that students are invested in their project from an early stage.
To date, the course has supported 31 projects, spanning domestic and global health. Projects have included an entrepreneurship model to provide community access to clean drinking water in Mexico (Fundación Cántaro Azul [Blue Jug Foundation], 2011), a diabetes risk awareness campaign to lead individuals to take preventive action (a health technology startup, 2013), and a strategy for improving the efficiency of mobile produce markets providing free fresh produce to five of the largest food-insecure communities in New York City (City Harvest, 2014).
With support from our course sponsors, we also provide teams access to project funding, for which they must compete. The project funding available to teams has ranged from $4000 to $8250 for a given class (seven to eight projects). Our teams have used this funding to travel to Navajo Nation, Turkey, Uganda, Mexico, Nicaragua, and New York City. Many student teams have worked locally in the San Francisco Bay Area.
The team project is our best opportunity to explore sustainable implementation with students. We emphasize the importance of understanding the perspective of one’s customers to achieve solutions that are likely to stick. For example, one month in advance of Suzara’s pop-up, we encouraged her team to develop and test a rapid prototype of the Sariwa concept, suggesting a half day as an appropriate time frame. The team met on a Saturday morning at the Grand Lake Farmers’ Market in Oakland, California. With no advance planning, and adhering to the half-day limit, team members developed a menu reflecting the Sariwa brand, shopped for ingredients at the farmers’ market, prepared food samples in a kitchen, developed an interview guide, and returned to Grand Lake with food samples to use as the basis for a conversation with two dozen Oakland residents about healthy Filipino food. The pursuit of sustainable implementation often requires approaches such as these, which may differ from the research methods that our students have previously learned.
CURRICULUM
To help students understand different approaches to innovation, we invite six to eight industry guests each year to speak to the class about their experiences with innovation. To ensure that we are always providing a fresh experience for students, we invite an entirely new group of speakers each year. Our speakers have represented media (New York Times, WIRED), funders (Physic Ventures, Robert Wood Johnson Foundation, California HealthCare Foundation), corporations (Intel, Pixar, Toyota do Brasil), design (Point Forward, IDEO.org), government (California Department of Public Health, US Health and Human Services, Memphis City Schools), and social entrepreneurship (Skoll Foundation, World Health Partners, D-Rev).
Our curriculum mimics the innovation process, with a module for each of the stages of the process: understanding, innovating, and prototyping. In addition, we ensure that effective communication skills are adequately addressed throughout the course. Although we have a curriculum plan at the start of each semester, we adapt the curriculum during the semester in response to student and project needs. No two iterations of the course are the same, but the spring 2013 course sequence serves as an example: course introduction, innovation as process, ethnography, interviewing, framing, skill swapping, incentives (behavioral economics), cost benefit, delight (in design), business fundamentals, prototyping and testing, scaling, information design, and storytelling.
DEMAND
One author (R. H.) has introduced many new graduate and undergraduate courses at the School of Public Health over the past three decades, all of them driven by student interest and demand. Our hypothesis is that if courses are developed to meet latent demand among students, word of mouth will accelerate demand for challenging courses, and not just within the school. We have witnessed a steadily increasing demand for the seats in our course. In 2014, more than 60 graduate students applied for the 25 places in the class. In the student selection process, we have to turn away public health students in favor of external entrants to ensure disciplinary diversity. To date, 90 students representing 26 academic programs have taken the course, more than half from programs outside the School of Public Health (Figure 1).
FIGURE 1—
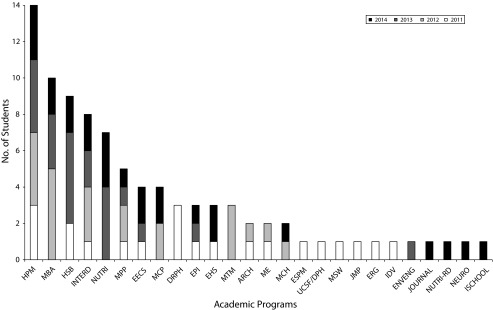
Public health innovations course student enrollment by program: University of California, Berkeley, 2011–2014.
Note. ARCH = Architecture MArch/PhD; DRPH = Doctor of Public Health; EECS = Electrical Engineering and Computer Science MS/PhD; EHS = Environmental Health Sciences MPH/MS/PhD; ENVENG = Environmental Engineering MS/PhD; EPI = Epidemiology MPH/MS/PhD; ERG = Energy and Resources Group MS/PhD; ESPM = Environmental Science, Policy and Management PhD; HPM = Health Policy and Management MPH; HSB = Health and Social Behavior MPH; IDV = Infectious Diseases and Vaccinology MPH; INTERD = Interdisciplinary MPH; ISCHOOL = Master of Information Management and Systems; JMP = Joint Medical Program MS/MD; JOURNAL = Master of Journalism; MBA = Masters of Business Administration; MCH = Maternal and Child Health MPH; MCP = Master of City Planning; ME = Mechanical Engineering MS/PhD; MPH = Masters of Public Health; MPP = Masters of Public Policy; MSW = Master of Social Work; MTM = Master of Translational Medicine; NEURO = Neuroscience MS/PhD; NUTRI = Nutrition MPH; NUTRI-RD = Registered Dietitian; UCSF/DPH = University of California, San Francisco Dental Public Health. A total of 26 graduate programs were represented across four years, more than 50% from outside the School of Public Health. The six programs that contributed the most students were Health Policy and Management MPH (14 students), Haas School of Business MBA (10), Health and Social Behavior MPH (9), Interdisciplinary MPH (8), Nutrition MPH (7), and Goldman School of Public Policy MPP (5).
In 2010, no courses like ours existed at our or any other school of public health. Similar courses existed in schools of business, design, and engineering, but none of them had the focus, explicitly or implicitly, on public health that we sought.1 To meet and even exceed demand, our goal was not to copy exactly from other innovation courses, but rather to create an offering that would be dynamic enough to attract students from other disciplines.
COLLABORATION
In 2013, our course evaluations were the strongest that they had ever been (Table 1); however, we knew that we needed to make a change to stay ahead of the curve and to model what we aimed to teach. In the first three years of the course, students explored such diverse topics as aging, point-of-care HIV diagnostics, and access to health care. We decided to focus on a theme in 2014. After much deliberation, we decided on food as a theme, largely because of campuswide student demand for innovative solutions at the intersection of health and food.
TABLE 1—
Anonymous Student Evaluation Results for the Public Health Innovations Course at University of California, Berkeley: 2011–2014
| Survey Question | 2011 (n = 19), Mean Score | 2012 (n = 18), Mean Score | 2013 (n = 22), Mean Score | 2014 (n = 24), Mean Score |
| Was the aim of this course made clear? | 6.44 | 6.11 | 6.32 | 6.33 |
| How well did the course attain its stated objectives? | 6.22 | 6.22 | 6.50 | 6.00 |
| Was the course as a whole well organized? | 6.17 | 5.67 | 6.18 | 6.08 |
| Were the assignments helpful to your understanding of the course material? | 6.39 | 5.83 | 6.33 | 6.29 |
| Did you have adequate opportunity for personal conference outside of class? | 6.44 | 6.00 | 6.59 | 6.46 |
| Was your performance in this class adequately assessed? | 5.86 | 5.47 | 6.39 | 6.19 |
| Did the content of this course meet your expectations? | 6.11 | 5.94 | 6.59 | 6.42 |
| What is your overall rating of this course? | 6.21 | 6.31 | 6.75 | 6.65 |
Note. This survey is administered for all courses at the School of Public Health. Responses are given on a seven-point scale, with seven the most favorable.
Meeting the demand for a food systems–centered course—a field outside our expertise—required new partnerships and new team members. We assembled a team of former Designing Innovative Public Health Solutions students in the Public Health Nutrition program to assist with curriculum development for the new version of the course. We also added a third faculty member (K. A. M.) to the teaching team, who was willing to lend her extensive experience in nutrition, obesity, and food systems and was interested in the innovation process.
Faculty members are frequently overwhelmed with the teaching–service–research triad, so team teaching often translates to “These are your sessions, these are mine.” However, to motivate students to work collaboratively in interdisciplinary teams, we have to model that behavior in this course. Course development, preparation, teaching, assessment, student communication, and other aspects of administering the course took the three instructors an estimated total of 400 hours for this single three-credit, semester-long course with 25 students in spring 2014. Authentic team teaching is a collaborative, iterative, and time-consuming process.
Replication of a course such as this one requires a move away from traditional models for course development and delivery. A faculty champion must take this on and identify instructional faculty with knowledge of the human-centered design process. The teaching team must commit to engaging students from across disciplines. Support for this resource-intensive model must be negotiated at the outset, so appropriate budget and time allocation can be secured. In light of the relatively higher costs of a course like this, evaluation measures to demonstrate its value for students and faculty must be planned at the outset. Such a replication effort is only warranted if a school sees this—as we did—as aligning with its mission and the evolving needs of its students.
OUTCOMES
The School of Public Health administers a standardized, anonymous evaluation survey at the close of every course. This has been administered all four years that we have taught our innovations course (Table 1). On a seven-point scale for overall course evaluation, the course had a mean of 6.65 in 2013 and 6.75 in 2014, with a median of seven, making it one of the 10 highest-rated courses offered by the School of Public Health.
A schoolwide exit survey conducted in spring 2013 asked graduating students what their most valuable course was. Among hundreds of courses students completed, this course was among the top 10, even though only a small fraction of the students eligible to take the exit survey had the opportunity to take the course. In the exit survey, one student wrote,
Designing Innovative Public Health Solutions . . . promoted real world critical thinking with appropriate application exercises. I am currently employed and use lessons learned from this class every day/week.
We also conduct our own survey to understand how students will use skills from the course in their work moving forward. The following are responses from the spring 2014 cohort to the question, “How will this course influence the way you do your work?”:
Student 1: This class has ensured that I will apply the innovation process to future work problems. Knowing full well how tired the public health model is, this class will continue to encourage me to look outside the familiar public health scope when framing problems.
Student 2: I have already started employing some of the methods in my summer internship. In thinking about strategies to raise awareness on my issue, I've considered framing, passion, behavioral economics, and borrowed innovation. I also recently considered how I can reach out to potential partners to meet at the nexus where our problem set unites and identifying “how we might” work together at those junctions.
Student 3: Ultimately, I want to value creativity. For my entire science career, it's been on the back burner, but I realized it's needed much more than we thought. Secondly, I will wield post-it notes in all my bags. It's so much easier to get ideas that way. I'm excited to stimulate ideas with everybody.
Less systematically, we have tracked our course alumni, and the anecdotal evidence suggests that we are having some lasting impact on our students. A Master of Business Administration student (2013) went on to work for the company that was the basis of his team project. A city planning student (2012) instituted an infographic-based report as a standard quarterly reporting procedure globally for his nonprofit food relief organization. A mechanical engineer (2011) became an IDEO.org fellow, and an Energy and Resources Group student from the same cohort became an Ashoka Fellow. An interdisciplinary Master of Public Health student (2011) is working with the Norwegian Directorate of Health to use design to improve geriatric care. Another interdisciplinary Master of Public Health student (2014) has taught the innovation process to public health graduate students.
REFLECTION
In designing interventions to address public health problems, researchers build on evidence-based solutions. However, with many complex and seemingly intractable problems facing us—such as obesity—the existing evidence base doesn’t contain the solutions we need. To find solutions that stick, we have to step outside our comfort zone, just as students are asked to do in our course. We hypothesized that bringing students with different perspectives together; giving them tools to identify human-centered, real-world solutions; and providing space for a creative and iterative process would meet students’ demand for a meaningful innovation design course. The student evaluations and comments suggest that it’s working. Still, we know that we cannot be content with apparent success. We have to be continuously learning.
So, what did we learn from Suzara and her team, after having already taught the course for four years? We recognize that we have not provided adequate opportunities for entrepreneurs. Our focus has been entirely on client organizations. Suzara and her team treated the $650 project funding that they received from the class as seed capital, instead of as a grant. They generated more than $1900 in revenue in a single night, with a net gain of nearly $600. We also learned that our measures of team diversity are too narrow. In many respects, that team was one of our least diverse in four years, comprising three Master of Public Health students, all women. In practice, the team applied diverse professional experiences to the project: environmental advocacy, health care quality improvement, and food catering. What is most exciting to us is that the team, in spite of other work commitments, continues to actively work together on developing the Sariwa concept.
To be credible in teaching innovation, we have to constantly innovate the way that we teach and learn from our students. And we will continue to do that.
Acknowledgments
The course described has been supported by the Blum Center for Developing Economies; the University of California, Berkeley School of Public Health; the Cal Design Lab; the Michigan State University Global Center for Food Systems Innovation, part of US Agency for International Development’s Higher Education Solutions Network; and the University of California, Berkeley Center for Teaching and Learning.
We thank Jamie Creason, Mandy Murphy, Amy Regan, and Erika Tribett for their assistance in developing the curriculum for Eat.Think.Design. We thank Sona Makker, Shannon Hamilton, Victoria Tecca, and Joyce Liu, our course interns, for their contributions to managing and developing the course. We thank Alissa Bernstein for her assistance in developing the article. Finally, we thank all of our course alumni, who have both motivated and shaped the course.
References
- 1. Sandhu J, Hosang N. A TV reporter, an electrical engineer, and an epidemiologist walk into a classroom: designing innovative public health solutions. Paper presented at: Innovations in Public Health Education Symposium, Columbia Mailman School of Public Health; June 3–4, 2013; New York, NY.
- 2.Frenk J, Chen L, Bhutta ZA et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376(9756):1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 3.Beckman SL, Kellogg C, Cahen H. Problem finding, problem solving: teaching MBA students how to think like designers. Innovation (Abingdon) 2010;29(4):37–40. [Google Scholar]
- 4.Sandhu J. Measure early, measure often: rapid, real-time feedback in design for social innovation. PopTech. Made to measure: the new science of impact. 2013. Available at: http://poptech.org/e3_jaspal_sandhu. Accessed on December 8, 2014.
- 5.Van Hartesveldt, Giordan J., editors. Impact of Transformative Interdisciplinary Research and Graduate Education on Academic Institutions. Washington, DC: National Science Foundation; 2008. [Google Scholar]


