Abstract
Background
Consideration of child safeguarding is routine within maternity services but less common in other health services for adults. We audited notifications for child safeguarding from an acute general hospital where the policy includes questioning adults presenting with violence, mental health problems or drug or alcohol misuse to any department within the hospital about children at home and notifying to the local authority children's social care services if there are safeguarding concerns.
Methods
Cross-sectional audit of notifications for child safeguarding, including abuse, neglect or victimization, from all departments in one hospital to the local authority children's social care department during 12 months (2010/11).
Results
Of 681 notifications (57 per month), 40% (270/681) were triggered by parents' presentation to acute hospital services. Of these, 37% (100/270; 12 teenage mothers) presented for maternity care and 60% (162/270; 8 teenage parents) presented to the emergency department (ED). Of the 60% (411/681) of notifications prompted by children presenting for healthcare, most originated from the ED (358/411; 87%): two-thirds of these presented with injury (250/358; 70%).
Conclusion
Given a policy to ask adults about children at home, a substantial proportion of children notified for child safeguarding were recognized through presentations to acute healthcare by their parents. Further research and development of this policy needs to ensure that questioning results in effective interventions for the children and their parents.
Keywords: child maltreatment, child safeguarding, paediatric emergency, social care, victimization
Introduction
Safeguarding and promoting the welfare of children to protect them from maltreatment, prevent impairment, and ensure they grow up with safe and effective care is seen as a core element of healthcare (Marmot 14; Munro 15; Norman et al. 17; Simkiss et al. 25). There is growing recognition that clinicians caring for adults need to consider the effects of physical and mental health problems of parents on the well-being of their children (Brent & Silverstein 2). Recommendations to ‘think family’ in order to recognize and address adversity for children through parental mental health problems, drug or alcohol misuse, violence, or death, has been incorporated into guidance published by professional bodies (Saperia et al. 22; General Medical Council 5; RCGP and NSPCC 20; Royal College of Psychiatrists 21).
Understanding how often presentations to healthcare by parents raise safeguarding concerns about children is important to inform the co-ordination of services, ensure adequate resourcing of safeguarding activity, and provision of training and support for practitioners caring for parents as well as for children. While early recognition of child safeguarding needs is core to maternity services, information on how often child safeguarding concerns arise is lacking for other healthcare services for adults. However, a handful of small studies of children suggest that recognition of safeguarding needs is often triggered by parental problems. A study of Danish general practitioners (GPs) reported that half the cases of child neglect were identified through presentations by parents (Hølge-Hazelton & Tulinius 9). In the UK, a small audit of children admitted to an acute general hospital in 2010 found that 14% (n = 64) of child admissions generated sufficient concern for discussion at a weekly multidisciplinary meeting with social workers and 39% (25/64) were triggered by parental behaviour or concerns about parenting capacity (Kugler et al. 12).
We determined the proportion of notifications from an acute hospital for child safeguarding initiated in response to presentations to hospital by a parent. We measured notifications to children's social care (CSC) from all departments in one inner-city, acute, publicly funded (National Health Service) hospital in London as part of an audit to improve recording of concerns about possible maltreatment as recommended in guidance by the National Institute for Health and Clinical Excellence (NICE) (Saperia et al. 22).
Methods
Safeguarding policy in hospital
We studied notifications for child safeguarding generated by a hospital in central London that includes acute and specialist services for children and adult populations. The hospital admitted over 125 000 patients and saw over 750 000 outpatients (with over 110 000 attendances to the emergency department – ED) in 2011. Hospital attendances for children aged less than 19 years in 2011 comprised 15 801 admissions, 72 341 outpatient visits and 17 019 attendances at the ED.
Since 2003, the hospital has implemented a policy to ask adults presenting with mental health problems, drug or alcohol misuse or violence whether there are children living at home (Rachamim et al. 18). Staff in all departments receive training about child safeguarding. The need for safeguarding can arise if maltreatment is suspected (e.g. physical, emotional or sexual abuse, or neglect by carers), if the child has been exposed to violence among other members of the household or by others, if the child's behaviour places them at risk of harm, or if carers are incapacitated and unable to look after the child. For example, admission of a sick parent to hospital with no one at home to care for his or her child would raise the need for safeguarding as the child's basic physical or psychological needs might not be met, or the child could be at risk of harm. Training includes how to ask adults about children at home and who to contact to discuss concerns. The decision to notify a child to CSC is made only after clinician assessment of the child and their circumstances.
Notification to the CSC department can request a referral for suspected child maltreatment (Saperia et al. 22), a referral for welfare needs (child in need referral), or may be used to share information between the hospital and CSC about a child. Notifications to CSC could be initiated by any hospital department using a two-page form adapted from the Department for Education common assessment framework (eCAF), which was faxed to a single local authority CSC department, regardless of the child's local authority of residence. In the case of presentations by parents, children could be notified to CSC even if they are at home and have not been seen by hospital staff.
We analysed all notifications to the CSC during a 12-month period (6 months in 2010 and the same 6 months in 2011), which were recorded in a database by the nurse responsible for child safeguarding at the hospital (the ‘named nurse’ and one of the co-authors PS) (Department for Education 3). We were unable to determine what action was taken by CSC as this information is not routinely fed back to the hospital. We classified cases according to whether the notification was initiated in response to a presentation by the parent or the child. Teenage mothers (girls <19 years who were mothers or pregnant) were categorized as parents for the purposes of this study. When healthy new-borns had been notified because of concerns about their parents, these were classified as parent presentations. New-borns notified because of complex co-morbidities (e.g. very preterm) and concerns about parents' abilities to cope were classified as child presentations. We present results according to whether the child or parent presented to healthcare. We do not report cell sizes less than five.
Comparison of notifications to CSC with other safeguarding indicators
We determined how notification to CSC compared with other routinely recorded indices relevant to safeguarding in two subgroups: children admitted to hospital in the audit period 2010–11 (excluding new-borns) and children attending the ED for injury in 2011. We could not make comparisons with adult patient groups as concerns about child safeguarding would rarely be coded in adult patients' records.
To analyse child admissions we extracted records for patients aged less than 19 years who had an unplanned admission to hospital for possible maltreatment or violence during the audit period 2010/11 based on a previously reported cluster of diagnostic International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD10) codes recorded in discharge records (Gonzalez-Izquierdo et al. 6). We grouped children according to injury or non-injury and recorded the proportion with safeguarding needs or not based on researcher review (AG-I, AW and RG) of clinical data recorded in electronic patient records and discharge summaries. After clinical record review, we linked all records with ICD10 codes for possible maltreatment or violence to the CSC notification database to determine the proportion with safeguarding needs confirmed by researcher review and the proportion notified to CSC. To compare children with indices of safeguarding needs who attended the ED for injury with those notified to CSC, we searched the electronic ED database for all attendances for codes (CDS version 6 type 010 Accident and emergency) or text strings that reflected assault, maltreatment, violence, self-harm, intentional drug or alcohol intoxication or ingestion or Injury or poisoning of undetermined cause in children <19 years attending during 6 months in 2011 (Fig. 1). Duplicate records and review visits were removed. We linked admission or ED records to CSC notifications using date of attendance, hospital number and date of birth.
Figure 1.
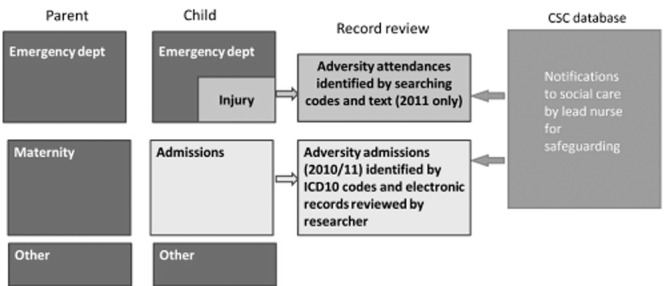
Evaluation of subgroups identified by adversity indicators in electronic records. Notifications to children's social care are made from all boxes shown. CSC, children's social care; ICD10, International Statistical Classification of Diseases and Related Health Problems 10th Revision.
Ethics
Data for all aspects of the study were collected as part of an audit to improve adherence to NICE guidance on recording of child maltreatment in electronic patient records and did not require research ethics approval.
Results
There were 681 notifications to CSC (342 in a 6-month period in 2010 and 339 in the same 6-month period in 2011). On average, there were 57 notifications per month. Table 1 illustrates some of the reasons for notification recorded in the notification database. Further anonymized case summaries are available from the authors.
Table 1.
Reasons for notification to children's social care by age group recorded by child protection nurse
| Infant | Down syndrome has just been confirmed. Lives with mum, dad and young sibling. Mum has depression. Another couple lodging with the family can be abusive and are refusing to leave the home. Police are involved. |
| Baby's mother is depressed and suffering overcrowding in her current home. | |
| Child swallowed a small amount of antiseptic liquid. No concerns about mother but family known for domestic issues. | |
| Children are on child protection register. Seen by GP for fever and cold symptoms but mother unable to give antibiotics. | |
| 1 to <5 years | Patient brought to the ED with a rash and unexplained bruise noted. Mother acting appropriately. Family live in bed and breakfast accommodation because of domestic violence. |
| Child brought with leg pain. X-ray showed spiral fracture, which was unexplained. Ex-partner violent to mother but no recent contact. Mother is pregnant. | |
| Child brought for painful wrist because her aunt hit her. Mother in argument with aunt. | |
| Family currently live on an estate that they do not consider safe. They are intimidated by gangs and cannot let the children play out. Police, health visitor, GP and school are aware. | |
| 10 to 14 years | Lip laceration after an alleged fight with another youth. Concerns over possible bullying. |
| One of group on a scooter involved in an accident. Brought to the ED in police custody. | |
| Patient presented with depression and panic attacks. Very poor living conditions. | |
| Patient had a head injury after falling off a scooter and is on child protection register. | |
| 15 to <18 years | Brought in by ambulance with a head injury and intoxicated. Assaulted a member of staff and was arrested. Mother going to police station. |
| Patient presented with genital problems. Speaks little English, boyfriend is significantly older and there are concerns about her living circumstances. | |
| Father brought child to the ED after 3-day temperature. Numerous previous attendances with unwell child and lack of knowledge about how to manage minor illnesses. | |
| Patient presented to the ED with abdominal pain. No fixed abode and father is in the Middle East and mother was killed. | |
| Parent | Mother and baby live in shared accommodation. They have their own room but share the bathroom and kitchen with seven other people who smoke at home and use illegal substances. Mother does not feel safe there. She locks her room when using the shared facilities. |
| Father brought to the ED after night out with child's mother in which he took cocaine and was involved in a fight. Child was left with grandmother who then came to the ED having left the child with a neighbour. | |
| Child's father came to the ED after assault by perpetrators within the family. Police involved but do not feel the children are at risk. | |
| Child's mother attended the ED with partner and child. She has been acting manically for 6 weeks. She is saying she wants to kill herself and could harm the baby. |
ED, emergency department; GP, general practitioner.
Table 2 shows that 40% of notifications (270/681) were initiated in response to a parent presenting to healthcare. Of these, 37% (100/270) were notified by maternity services. Seven per cent of parents (20/270) were aged less than 19 years old. Most presentations by parents were notified from the ED (162/270; 60%); two-thirds of these were for injury (110/162).
Table 2.
Notifications to children's social services during 12 months (2010/2011)
| Age group (years) |
Percentage of all |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Presentation by: Child/adolescent | <1 | 1–9 | 10–14 | 15–<19 | 19 | Total | CSC‡ notifications | Children or parents | ED |
| Subtotal | 36 | 108 | 77 | 186 | 4 | 411 | 60.4% | 100% | |
| Emergency department (ED) | 27 | 91 | 69 | 167 | 4 | 358 | 52.6% | 87.1% | 68.8% |
| Admission | 9 | 17 | NA | 15 | 0 | 41 | 6.0% | 10.0% | |
| Outpatients | 0 | <5 | <5 | <5 | 0 | 12 | 1.8% | 2.9% | |
| Parent | all <19 | 19+ | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Subtotal | 20 | 250 | 270 | 39.6% | 100% | ||||
| Emergency department | 8 | 154 | 162 | 23.8% | 60.0% | 31.2% | |||
| Maternity† | 12 | 88 | 100 | 14.7% | 37.0% | ||||
| Outpatients/other | 0 | 8 | 8 | 1.2% | 3.0% | ||||
| Total notifications | 681 | 100% |
Includes five babies referred while on postnatal/neonatal wards.
Children's social care services.
For children presenting to healthcare, 87% (358/411) of notifications came from the ED, including four adolescents aged 19 years. Two-thirds of these presentations were for injury (250/358). Boys were notified by the ED nearly as often as girls (46% vs. 54%, 154 and 182; sex unknown in 22 cases).
Table 3 shows the number of children admitted with ICD10 discharge codes reflecting maltreatment or violence (n = 138). We show number of children confirmed to have safeguarding needs based on review of the electronic patient record or CSC notification (n = 93) or notification to CSC (n = 46). The proportions of admissions with confirmed safeguarding needs or notified to CSC were higher among injury than non-injury admissions. Very few notifications (less than five and only among non-injury admissions) to CSC were solely for disability or palliative care without other safeguarding concern.
Table 3.
Child admissions (<19 years) to hospital and proportion notified to children's social care (CSC) or coded for adversity in 12 months (2010/11)
| Admissions with safeguarding indices (% notified to CSC) |
Percentage of admissions |
||||||
|---|---|---|---|---|---|---|---|
| Type of admission | Notified to CSC | Safeguarding needs confirmed by record review | ICD10 codes reflecting safeguarding needs | Total n‡ | Notified to CSC | Safeguarding needs confirmed by record review | ICD10 codes reflecting safeguarding needs |
| Child – total | 46 | 93 (50%) | 138 (33%) | 8829 | 0.5% | 1.1% | 1.6% |
| Injury | 27† | 48 (56%) | 48 (56%) | 830 | 3.3% | 5.8% | 5.8% |
| Non-injury | 19† | 45 (42%) | 90 (21%) | 7999 | 0.2% | 0.6% | 1.1% |
Forty-six child admissions (41 in table 2 and 5 notifications initiated in the emergency department).
From Hospital Episode Statistics for the corresponding 6 months in 2010 and 6 months in 2011.
ICD10, International Statistical Classification of Diseases and Related Health Problems 10th Revision.
To compare safeguarding indices recorded in the ED, we linked 95 of 108 CSC notifications to electronic patient records for injury attendance to the ED. Table 4 shows that 47 attendances with safeguarding indices (relevant codes or text strings in the electronic ED record) were notified (22%; 47/217) as were a similar number (48) without safeguarding indicators. The overall risk of notification was highest for injury attendances at 16–18 years (9%) and lowest for children less than 11 years old (2.6%). The number of notifications in children without safeguarding indicators partly reflects lack of information in the electronic record. Eighty-six per cent (1835/2122) of all children attending the ED for injury were recorded as being registered with a GP but only 69% (305/445) of 16- to 18-year-olds.
Table 4.
Emergency attendances for injury at the emergency department (ED) during 6 months in 2011 and proportion notified to children's social care (CSC)
| Number of ED injury attendances (% notified) |
|||||||
|---|---|---|---|---|---|---|---|
| Safeguarding indices in ED record |
No safeguarding indices in ED record |
Total injury |
|||||
| Child age group | Notified to CSC | Total attending | Notified to CSC | Total attending | Notified to CSC | Total attending | % Injury of all ED attendances‡ |
| 16 to 18 years | 31 | 155 (20%) | 9 | 290 (3.1%) | 40 | 445 (9.0%) | 32% |
| 11 to 15 years | 14 | 14 (35%) | 9 | 411 (2.2%) | 23 | 451 (5.1%) | 37% |
| <11 years | <5 | 22 (10%) | 30 | 1204 (2.5%) | 32 | 1226 (2.6%) | 25% |
| Total | 47 | 217 (22%) | 48 | 1905 (2.5%) | 95† | 2122 (4.5%) | 29% |
95/108 notifications linked.
Estimate based on 2011 provided by hospital.
Discussion
Forty per cent of notifications to CSC from an acute hospital for child safeguarding concerns were initiated in response to presentations to healthcare by parents and the majority of these were from presentations to the ED. In subgroup analyses of children admitted to hospital or attending the ED for injury, notifications to CSC represented a moderate to high thresholds of concern as only one-fifth to one-half of those who had safeguarding indices recorded in their electronic patient record were notified to CSC.
The finding that a large proportion of child safeguarding concerns were triggered by the parents' presentation to hospital is consistent with evidence from two small studies (Hølge-Hazelton & Tulinius 9; Kugler et al. 12), professional guidance (General Medical Council 5; RCGP & NSPCC 20), and anecdotal reports from general practice and child health professionals (Woodman et al. 29,30).
Our findings reflect rates of parent notification that might be achieved given a long-established policy to consider children at risk at home when parents present with behaviour associated with abuse or neglect. Similar policies have been reported in a recent case study of 11 trusts (Lewis 13). Standards for the ED published in 2012 by a consortium of Royal Colleges recommends ‘When treating adults, staff must recognize the potential impact of a parent's or carer's physical and mental health on the well-being of dependents, and take appropriate action’ but falls short of recommending questioning of adults (Intercollegiate Committee for Standards for Children and Young People in Emergency Care Settings 10). However, the high proportion of cases notified to CSC that were identified through presentations to healthcare by parents may not be generalizable to other hospitals where there are lower levels of awareness among clinicians dealing with adults about child safeguarding concerns and no policy of direct questioning. Ease of notification to a single local authority CSC may have also led to high notification rates compared with hospitals where clinicians have to deal with different local authorities, often with different processes and thresholds for action (Lewis 13).
Our study was not able to determine what happened as a consequence of notification to CSC. Lack of systematic feedback from CSC in response to notifications by healthcare professionals is a well-recognized problem with serious potential adverse effects (Lewis 13). Health professionals may wrongly judge that they have taken appropriate action, yet if no action is taken by CSC, the child and in some cases, the parent, may remain at serious risk of harm.
Implications for practice
The children referred to CSC in this study are a mixed population who were considered by healthcare professionals to have safeguarding needs. The risk of subsequent harm for this broad group with safeguarding concerns has not been quantified, but there is robust prognostic evidence of serious adverse outcomes for some subgroups (Hjern et al. 8; Vinnerljung et al. 28; Norman et al. 17). The outlook is similarly bleak for some subgroups of parents of maltreated or otherwise vulnerable children (Franzen & Vinnerljung 4; Kahila et al. 11; Sarkola et al. 23).
What action could be taken in response to safeguarding concerns? Community input may require statutory services such as social services or police but parental healthcare needs, such as mental health problems, which impact on parenting capacity and the child's safety and development, need to be addressed by healthcare (Barlow & Calam 1). General practitioners in the UK have a unique position as providers of primary care to children and their parents, including mental healthcare, particularly for adults (Woodman et al. 29,30). Moreover, evidence is emerging of the effectiveness of family-based interventions for parents and their families, which could be initiated through primary care, to prevent abuse, neglect and violence (Niccols et al. 16; Selph et al. 24; Spoth et al. 27). Evidence for case management interventions implemented by the hospital for children attending the ED is of limited quality and findings are inconsistent (Snider & Lee 26). Development of strategies based in primary care would need to address skill gaps – most researched for GP responses to domestic violence, which show lack of awareness, knowledge and skills to take a history and assess severity of abuse and mental health issues (Ramsay et al. 19; Hegarty et al. 7). However, a first step towards improving ongoing support for children and their parents with safeguarding needs is to ensure registration with a GP.
Our findings suggest that direct questioning of adults presenting to acute hospital services about children at home identifies families where there may be child safeguarding needs, which might not otherwise be detected by healthcare. Whether such identification leads to effective interventions for families requires evaluation on a wider scale across the National Health Services (NHS). Most child healthcare is provided by parents not by child health services. The potential benefits of greater awareness of child safeguarding by adult services for parents are safe and effective care for children.
Key messages
Drug or alcohol misuse, mental illness and violence affecting parents are known to be strong markers of children who may need safeguarding.
Policy encourages clinicians to ‘think family’ with respect to child safeguarding but information is lacking on the proportion of safeguarding notifications prompted by parents' presentations to healthcare.
Forty per cent of safeguarding notifications to children's social care services from an acute London hospital were initiated by parents presenting to hospital: 37% were from maternity-services and 60% from the ED.
One-fifth to one-half of children with safeguarding indicators recorded in their patient records were notified to CSC.
Acknowledgments
We are grateful to Jacqueline Apps, Christina Petropoulos, Anna Turner, Ben Greasley, Angela Huertas-Ceballos, Gemma Birchenough and Jonathan Ricketts for helping to facilitate this audit, and to Annie Herbert for commenting on the report. We would like to thank Terence Stephenson, Catherine Law, Amanda Edwards, Steve Morris, Helen Roberts, Catherine Shaw, Russell Viner and Miranda Wolpert, who are members of the Policy Research Unit for commenting on the report.
Funding
AG-I was supported by funding from the Department of Health Policy Research Programme through funding to the Policy Research Unit in the Health of Children, Young People and Families. This is an independent report commissioned and funded by the Department of Health. The views expressed are not necessarily those of the Department.
Conflict of interests
No competing interests.
References
- Barlow J, Calam R. A public health approach to safeguarding in the 21st century. Child Abuse Review. 2011;20:238–255. [Google Scholar]
- Brent DA, Silverstein M. Shedding light on the long shadow of childhood adversity. JAMA: The Journal of the American Medical Association. 2013;309:1777–1778. doi: 10.1001/jama.2013.4220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department for Education. 2013. Common Assessment Framework (CAF). Department for Education.
- Franzen E, Vinnerljung B. Foster children as young adults: many motherless, fatherless or orphaned: a Swedish national cohort study. Child and Family Social Work. 2006;11:254–263. [Google Scholar]
- General Medical Council. 2011. Protecting children and young people: the responsibilities of all doctors (draft for consultation). General Medical Council, London.
- Gonzalez-Izquierdo A, Woodman J, Copley L, van der Meulen J, Brandon M, Hodes D, Lecky F, Gilbert R. Variation in recording of child maltreatment in administrative records of hospital admissions for injury in England, 1997–2009. Archives of Disease in Childhood. 2010;95:918–925. doi: 10.1136/adc.2009.180216. Available from: PM:20647257. [DOI] [PubMed] [Google Scholar]
- Hegarty KL, O'Doherty LJ, Chondros P, Valpied J, Taft AJ, Astbury J, Brown SJ, Gold L, Taket A, Feder GS, Gunn JM. Effect of type and severity of intimate partner violence on women's health and service use: findings from a primary care trial of women afraid of their partners. Journal of Interpersonal Violence. 2013;28:273–294. doi: 10.1177/0886260512454722. Available from: PM:22929341. [DOI] [PubMed] [Google Scholar]
- Hjern A, Vinnerljung B, Lindblad F. Avoidable mortality among child welfare recipients and intercountry adoptees: a national cohort study. Journal of Epidemiology and Community Health. 2004;58:412–417. doi: 10.1136/jech.2003.014282. Available from: PM:15082742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hølge-Hazelton B, Tulinius C. Beyond the specific child. What is ‘a child's case’ in general practice? British Journal of General Practice. 2010;60:e4–e9. doi: 10.3399/bjgp10X482059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intercollegiate Committee for Standards for Children and Young People in Emergency Care Settings. Standards for Children and Young People in Emergency Care Settings. London, UK: Royal College of Paediatrics and Child Health; 2012. [Google Scholar]
- Kahila H, Gissler M, Sarkola T, Autti-Ramo I, Halmesmaki E. Maternal welfare, morbidity and mortality 6–15 years after a pregnancy complicated by alcohol and substance abuse: a register-based case-control follow-up study of 524 women. Drug and Alcohol Dependence. 2010;111:215–221. doi: 10.1016/j.drugalcdep.2010.04.014. Available from: PM:20627617. [DOI] [PubMed] [Google Scholar]
- Kugler B, Woodman J, Carroll J, Fertleman C, Gilbert R. Child protection guidance needs to address parent behaviour. Child: Care, Health and Development. 2013;39:760–761. doi: 10.1111/cch.12007. Available from: PM:23121306. [DOI] [PubMed] [Google Scholar]
- Lewis J. 2013. Partnership working in child protection: improving liaison between acute paediatric and child protection services. Social Care Institute for Excellence, London (in press)
- Marmot M. 2010. Fair society, healthy lives: strategic review of health inequalities in England post 2010, Marmot Review.
- Munro E. 2011. The Munro review of child protection: final report – a child-centred system, Department for Education, London.
- Niccols A, Milligan K, Sword W, Thabane L, Henderson J, Smith A. Integrated programs for mothers with substance abuse issues: a systematic review of studies reporting on parenting outcomes. Harm Reduction Journal. 2012;9:14. doi: 10.1186/1477-7517-9-14. Available from: PM:22429792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Medicine. 2012;9:e1001349. doi: 10.1371/journal.pmed.1001349. Available from: PM:23209385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachamim E, Hodes D, Gilbert R, Jenkins S. Pattern of hospital referrals of children at risk of maltreatment. Emergency Medicine Journal. 2011;28:952–954. doi: 10.1136/emj.2009.080176. Available from: PM:20972229. [DOI] [PubMed] [Google Scholar]
- Ramsay J, Rutterford C, Gregory A, Dunne D, Eldridge S, Sharp D, Feder G. Domestic violence: knowledge, attitudes, and clinical practice of selected UK primary healthcare clinicians. British Journal of General Practice. 2012;62:e647–e655. doi: 10.3399/bjgp12X654623. Available from: PM:22947586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RCGP & NSPCC. 2011. Safeguarding children and young people in general practice: a toolkit, RCGP and NSPCC, London.
- Royal College of Psychiatrists. 2011. Parents as patients: supporting the needs of patients who are parents and their children.
- Saperia J, Lakhanpaul M, Kemp A, Glaser D. When to suspect child maltreatment: summary of NICE guidance. BMJ (Clinical Research Ed.) 2009;339:b2689-230. doi: 10.1136/bmj.b2689. Available from: PM:19625357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkola T, Gissler M, Kahila H, Autti-Ramo I, Halmesmaki E. Alcohol and substance abuse identified during pregnancy: maternal morbidity, child morbidity and welfare interventions. Acta Paediatrica. 2012;101:784–790. doi: 10.1111/j.1651-2227.2012.02670.x. Available from: PM:22429257. [DOI] [PubMed] [Google Scholar]
- Selph SS, Bougatsos C, Blazina I, Nelson HD. Behavioral interventions and counseling to prevent child abuse and neglect: a systematic review to update the U.S. preventive services task force recommendation. Annals of Internal Medicine. 2013;158:179–190. doi: 10.7326/0003-4819-158-3-201302050-00590. Available from: PM:23338775. [DOI] [PubMed] [Google Scholar]
- Simkiss DE, Spencer NJ, Stallard N, Thorogood M. Health service use in families where children enter public care: a nested case control study using the General Practice Research Database. BMC Health Services Research. 2012;12:65. doi: 10.1186/1472-6963-12-65. Available from: PM:22424404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snider C, Lee J. Youth violence secondary prevention initiatives in emergency departments: a systematic review. CJEM: Canadian Journal of Emergency Medical Care. 2009;11:161–168. doi: 10.1017/s1481803500011131. Available from: PM:19272218. [DOI] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Shin C, Greenberg M, Feinberg M, Schainker L. PROSPER community-university partnership delivery system effects on substance misuse through 6 1/2 years past baseline from a cluster randomized controlled intervention trial. Preventive Medicine. 2013;56:190–196. doi: 10.1016/j.ypmed.2012.12.013. Available from: PM:23276777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinnerljung B, Franzen E, Danielsson M. Teenage parenthood among child welfare clients: a Swedish national cohort study of prevalence and odds. Journal of Adolescence. 2007;30:97–116. doi: 10.1016/j.adolescence.2005.12.002. Available from: PM:16455132. [DOI] [PubMed] [Google Scholar]
- Woodman J, Allister J, Rafi I, de Lusignan S, Belsey J, Petersen I, Gilbert R. A simple approach to improve recording of concerns about child maltreatment in primary care records: developing a quality improvement intervention. The British Journal of General Practice. 2012;62:e478–e486. doi: 10.3399/bjgp12X652346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodman J, Gilbert RE, Allister J, Glaser D, Brandon M. Responses to concerns about child maltreatment: a qualitative study of GPs in England. BMJ Open. 2013;3:e003894. doi: 10.1136/bmjopen-2013-003894. [DOI] [PMC free article] [PubMed] [Google Scholar]


