Abstract
Objective
To address the focused question, is there an impact of platform switching (PS) on marginal bone level (MBL) changes around endosseous implants compared to implants with platform matching (PM) implant-abutment configurations?
Material and methods
A systematic literature search was conducted using electronic databases PubMed, Web of Science, Journals@Ovid Full Text and Embase, manual search for human randomized clinical trials (RCTs) and prospective clinical controlled cohort studies (PCCS) reporting on MBL changes at implants with PS-, compared with PM-implant-abutment connections, published between 2005 and June 2013.
Results
Twenty-two publications were eligible for the systematic review. The qualitative analysis of 15 RCTs and seven PCCS revealed more studies (13 RCTs and three PCCS) showing a significantly less mean marginal bone loss around implants with PS- compared to PM-implant-abutment connections, indicating a clear tendency favoring the PS technique. A meta-analysis including 13 RCTs revealed a significantly less mean MBL change (0.49 mm [CI95% 0.38; 0.60]) at PS implants, compared with PM implants (1.01 mm [CI95% 0.62; 1.40] (P < 0.0001).
Conclusions
The meta-analysis revealed a significantly less mean MBL change at implants with a PS compared to PM-implant-abutment configuration. Studies included herein showed an unclear as well as high risk of bias mostly, and relatively short follow-up periods. The qualitative analysis revealed a tendency favoring the PS technique to prevent or minimize peri-implant marginal bone loss compared with PM technique. Due to heterogeneity of the included studies, their results require cautious interpretation.
Keywords: meta-analysis, peri-implant marginal bone level, platform switching, systematic review
The radiographically detectable peri-implant bone-level following prosthetic loading is considered one of the relevant success criteria for evaluating dental implant therapy outcomes as well as for proving or excluding peri-implant tissue health (Albrektsson et al. 1986; Laurell & Lundgren 2011; Papaspyridakos et al. 2012). Once accepting a marginal bone loss of up to 1.5 mm during the first year, followed by a bone loss not exceeding 0.2 mm per year (Albrektsson et al. 1986), nowadays marginal bone levels (MBLs) around implants following prosthetic loading are reported to be well preserved, not exceeding 0.5 mm after up to 3 years (Lang & Jepsen 2009) or 5 years (Laurell & Lundgren 2011) of observation. Marginal bone loss may occur around dental implants due to peri-implant infections, but may also occur for reasons other than infections (Albrektsson et al. 2012). However, a limited amount of crestal or marginal bone loss is supposed to be a biologic response to implant placement procedure (Albrektsson et al. 2012).
As introduction of the platform switching concept into construction of implant systems and abutment configurations, their experimental impact on peri-implant bone-level alterations was studied in various finite-element and in vivo studies as well (Becker et al. 2007, 2009; Jung et al. 2008; Cochran et al. 2009; Ferraz et al. 2012), and clinical experiences with this treatment were gained during the last decade (Lazzara & Porter 2006; Canullo & Rasperini 2007). Briefly, platform switching is defined as an “act of changing an implant abutment to one with a smaller diameter, so as to place the implant-abutment interface medial to the edge of the implant platform” (Laney 2007). However, the relatively short follow-up periods of most studies focusing on the effect of platform switching on marginal bone loss compared with platform-matching implant-abutment configurations and different sample sizes led to different conclusions even in systematic reviews, ranging from not revealing any clinical superiority for any particular implant design in maintaining MBLs (Lang & Jepsen 2009) to recognizing the platform-switching technique as appearing useful in limiting bone resorption (Al-Nsour et al. 2012; Annibali et al. 2012). Still, the need for cautious interpretation of the findings gained from systematic reviews due to heterogeneity of existing studies and possible publication bias as well and the need for more long-term, well-conducted, randomized controlled clinical studies to validate the platform switching concept is conceded even within recently published reviews (Atieh et al. 2010; Al-Nsour et al. 2012; Annibali et al. 2012).
Therefore, it seems to be opportune to critically and systematically review the publications of randomized clinical trials (RCTs) and prospective clinical controlled cohort studies (PCCS) regarding the impact of platform switching on MBL changes around endosseous implants compared with platform-matching implant-abutment configurations, to identify the need of and to develop recommendations for future research.
Material and methods
This systematic literature review was conducted considering the preferred reporting items for systematic reviews and meta-analyses (PRISMA) (Moher et al. 2009) (for the PRISMA checklist see Appendix, Table 7). To prepare and structure this systematic review, the focused question was elaborated by use of the PICO format (P: population (patients undergoing implant-prosthetic rehabilitation, which were included into RCTs or prospective controlled clinical studies (PCCS), comparing peri-implant marginal bone loss around endosseous implants with platform switching (PS) or platform-matching (PM) implant-abutment-configurations); I: intervention (use of endosseous dental implants with a PM (the abutment diameter and implant neck diameter were identical) or PS (the abutment diameter was medialized compared with the implant neck diameter) implant-abutment-configuration; C: comparison, and O: outcome (clinical studies comparing treatment outcomes using PM and PS implants with special consideration of radiographically detected peri-implant MBL changes were considered for evaluation).
Focused question
Is there an impact of platform switching implant-abutment-configurations compared with platform-matching implant-abutment-configurations on MBL changes around endosseous implants?
Selection of studies
Publications of RCTs and PCCS reporting comparison of MBL changes at implants with PS- or PM-implant-abutment configurations as primary outcome were selected from electronic databases only, if they met the inclusion criteria.
Inclusion criteria
Publications were included for the systematic review, if published between 2005 up to June 2013 in English or German language and listed in the electronic databases indicated below, or were published in the peer-reviewed German-language Journal of Oral Implantology (Zeitschrift für zahnärztliche Implantologie) or Implantologie (both journals were subjected to manual search), and if results from PCCS or RCTs comparing the radiographically measured mean MBL change of implants and its standard deviation, connected to PM- versus PS-implant-abutment configurations, were reported.
For meta-analysis, RCTs reporting a follow-up period of at least 12 months following implant placement were included only.
Exclusion criteria
Published studies not meeting the inclusion criteria were excluded from this systematic review (i.e., publications in languages others than English or German, case reports, educational statements, expert opinions, narrative reviews on the subject of platform switching, animal studies, in vitro experiments, clinical studies on platform switching without a control group utilizing platform matching implant-abutment configuration). Publications were not included if they did not provide PM- or PS-implant related data concerning MBL changes or marginal bone loss around implants and the comparison of both, or if they did not provide any information concerning the focused question.
Search strategy
A systematic literature search in electronic databases PubMed/Medline, Web of Science, Journals@Ovid Full Text and Embase was conducted, using the following MeSH term and search term combinations, considering the PICO format:
Population/patients/intervention/control
“dental implant-abutment design” [MeSH Terms] OR (“dental” [All Fields] AND “implant-abutment” [All Fields] AND “design” [All Fields]) OR “dental implant-abutment design” [All Fields] OR (“dental” [All Fields] AND “implant” [All Fields] AND “platform” [All Fields] AND “switching” [All Fields])
OR
(“dental implants” [MeSH Terms] OR (“dental” [All Fields] AND “implants” [All Fields]) OR “dental implants” [All Fields] OR (“dental” [All Fields] AND “implant” [All Fields]) OR “dental implant” [All Fields]) AND (platform[All Fields] AND switching[All Fields])
OR
(“dental implants” [MeSH Terms] OR (“dental” [All Fields] AND “implants” [All Fields]) OR “dental implants” [All Fields] OR (“dental” [All Fields] AND “implant” [All Fields]) OR “dental implant” [All Fields]) AND (platform[All Fields] AND switching[All Fields]) AND crestal[All Fields]
Outcome
(“dental implants” [MeSH Terms] OR (“dental” [All Fields] AND “implants” [All Fields]) OR “dental implants” [All Fields] OR (“dental” [All Fields] AND “implant” [All Fields]) OR “dental implant” [All Fields]) AND (crestal[All Fields] AND (“bone and bones” [MeSH Terms] OR (“bone” [All Fields] AND “bones” [All Fields]) OR “bone and bones” [All Fields] OR “bone” [All Fields]) AND level[All Fields])
OR
(“dental implants” [MeSH Terms] OR (“dental” [All Fields] AND “implants” [All Fields]) OR “dental implants” [All Fields] OR (“dental” [All Fields] AND “implant” [All Fields]) OR “dental implant” [All Fields]) AND ((“bone and bones” [MeSH Terms] OR (“bone” [All Fields] AND “bones” [All Fields]) OR “bone and bones” [All Fields] OR “bone” [All Fields]) AND level[All Fields] AND (“Change” [Journal] OR “change” [All Fields]))
OR
(“dental implants” [MeSH Terms] OR (“dental” [All Fields] AND “implants” [All Fields]) OR “dental implants” [All Fields]) AND ((“bone and bones” [MeSH Terms] OR (“bone” [All Fields] AND “bones” [All Fields]) OR “bone and bones” [All Fields] OR “bone” [All Fields]) AND level[All Fields] AND (“Change” [Journal] OR “change” [All Fields]))
A manual search was applied to two German-language peer-reviewed journals additionally, focusing on articles related to platform switching in clinical use.
Moreover, to detect data from unpublished studies, the following electronic registers of clinical trials were searched, using the following MeSH term and search term combinations (“dental implants” [MeSH Terms] AND platform[All Fields] AND switching[All Fields] OR (“dental implants” [MeSH Terms] AND “bone loss” [All Fields] OR “marginal” [All Fields] AND “bone” [All Fields]) AND level[All Fields] AND “change” [All Fields]): http://apps.who.int/trialsearch/; http://www.clinicaltrialsregister.eu/; http://www.clinicaltrials.gov; http://www.centerwatch.com; http://www.controlled-trials.com.
The literature search was conducted to identify PCCS and RCTs in humans. The search protocol regarding inclusion and exclusion criteria was followed by two reviewers (F.P.S. and M.H.), who independently run the search, screened and listed the abstracts of publications to be included. The list was then compared and a κ score was calculated to determine the reviewer′s agreement. A consent final decision regarding the inclusion of articles was reached by discussion of each individual article after full-text analysis.
Quality assessment
A quality assessment of the studies (RCTs) included for the meta-analysis was done following the recommendations for systematic reviews of interventions of the Cochrane collaboration (Higgins & Green 2011), focusing on the following criteria: random sequence generation and allocation concealment (both accounting for selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment. (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), or other possible causes of bias.
Radiographically detected peri-implant MBL change had to be expressed as quantitative data (mean difference between baseline and follow-up examination).
As one study reported on two different PS configurations, which were compared to the same control group (PM), the respective implant cohorts were subdivided into two study groups (Kielbassa et al. 2009 for comparison between PS group [implants with internal hexagon implant-abutment connection] and PM group [implants with an internal tube-in-tube connection]; Kielbassa et al. 2009; a for comparison between PS group [implants with external hexagon implant-abutment connection] and PM group [implants with an internal tube-in-tube connection]) and included into the meta-analysis as such. In one study, the allocation of at least one of each implant type with medialised (PS) or conventional (PM) abutments to 10 patients and a total number of 25 implants were reported (Trammell et al. 2009). Therefore, a total number of 12 implants within the PS group and PM group as well was assumed.
Data extraction and statistical analysis
The κ score was calculated to determine the reviewer′s agreement for inclusion or exclusion of publications and for the quality assessment of RCTs included, using the SPSS 19.0 statistical software package (SPSS Inc., Chicago, IL, USA).
Data reporting mean values of radiographically detected MBL changes and their standard deviations of each study were extracted independently by two reviewers (F.P.S. and M.H.) and compared thereafter.
The statistical heterogeneity among the RCTs selected for meta-analysis was assessed utilizing the DerSimonian–Laird estimate τ2 for inter study variance. The meta-analysis was performed using a random effects model to investigate on a possible difference between the mean bone loss in the groups of PS- compared with PM-implant-abutment configurations on an implant-based analysis. Forest and funnel plots were generated to show means and standard deviations of all studies considered and to detect possible bias in the selection of studies, respectively. Further a test for funnel-plot asymmetry was carried out based on linear regression. The meta-analysis was carried out using R 3.0 and the R package meta 2.4 (http://www.r-project.org/). The level of significance was α = 0.05.
Results
The initial search yielded 924 publications found in PubMed/Medline, 547 in Web of Science, 192 publications in Journals@Ovid Full text, and 34 publications in Embase. Three more German language publications were identified by manual search. After removing duplicate studies, an entire yield of 807 publications were screened considering the formal inclusion and exclusion criteria. Following the evaluation concerning the inclusion criteria, 93 abstracts were considered for further investigation, of which 23 publications were considered for full-text analysis. Following a discussion after full-text analysis, 22 studies were included for further investigation, finally seven PCCS and 15 RCTs met the inclusion criteria for systematic review and qualitative synthesis. Of the 15 RCTs, 13 were eligible for inclusion into a meta-analysis. A κ–score of 0.90 indicates a high reviewers’ agreement regarding the included publications. The process of identification of the included studies from the initial yield is described in Fig. 1. The numbers of patients, gender distribution, and implant data are listed in Table 1 and Figs 2–4, respectively.
Fig 1.
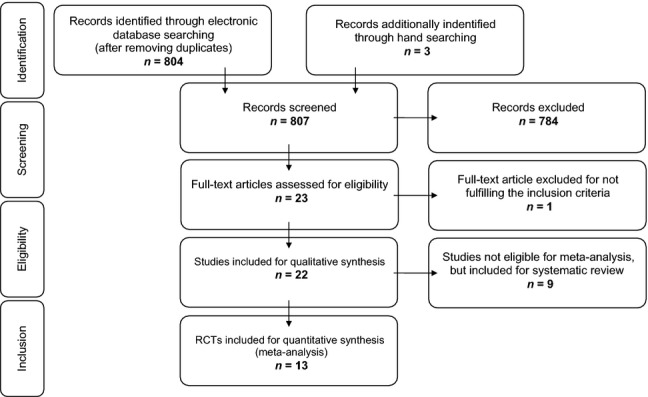
Search strategy and results of identification, screening for eligibility and inclusion of publications considered for systematic review and meta-analysis.
Table 1.
Overview on study type, demographic data, implant data of studies included for the systematic review
| Study type | n Patients | % Male patients | % Female patients | Mean age (years) and range | n Implants | Implant placement mode | Healing period | |
|---|---|---|---|---|---|---|---|---|
| de Almeida et al. (2011) | PCCS | 26 | n. a. | n. a. | 41 (25–70) | 42 | Late | 30–180 days |
| Canullo et al. (2012) | RCT | 40 | 60 | 40 | 58.2 | 80 | Late | 2–3 months |
| Canullo et al. (2010) | RCT | 31 | 54.8 | 45.2 | 52.1 (36–78) | 69 | Late | 3 months |
| Canullo et al. (2009) | RCT | 22 | 59.1 | 40.9 | 50 (32–76) | 22 | imm. | imm. restor. |
| Cappiello et al. (2008) | PCCS | 45 | n. a. | n. a. | n. a. | 131 | Late flapless | 8 weeks |
| Crespi et al. (2009) | RCT | 45 | 40 | 60 | 48.7 (25–67) | 64 | imm. flapless | imm. restor., imm. loading |
| Dursun et al. (2012) | PCCS | 19 | 47.4 | 52.6 | 42.9 (25–57) | 32 | Late | 3 months |
| Enkling et al. (2011) | RCT | 25 | 60 | 40 | 51 (SD 10.5) | 50 | late | 3 months |
| Fernández-Formoso et al. (2012) | RCT | 51 | 35.3 | 64.7 | 43 (26–69) | 114 | Late | 3 months |
| Fickl et al. (2010) | PCCS | 36 | 50 | 50 | 55.3 (17–69) | 89 | Late | 3 months |
| Gultekin et al. (2013) | RCT | 25 | 20 | 80 | 41.3 (19–59) | 93 | Late | 3 months |
| Hürzeler et al. (2007) | RCT | 15 | 46.7 | 53.3 | 55.3 (17–69) | 22 | n. a. | n. a. |
| Kielbassa et al. (2009) | RCT | 169 | 48.0 | 52 | 48.7 (17–79) | 241 | Late | imm. restor. |
| Linkevicius et al. (2010) | PCCS | 4 | 25 | 75 | 43 (37–56) | 12 | n. a. | 2 months |
| Peñarrocha-Diago et al. (2012) | RCT | 15 | 26.7 | 73.3 | 56.9 (44–77) | 120 | Late | 3 months |
| Pieri et al. (2011) | RCT | 37 | 36.8 | 63.2 | 46 (26–67) | 37 | imm. | imm. restor. |
| Prosper et al. (2009) | RCT | 60 | 53.3 | 46.7 | 53.9 (SD 6.8) | 360 | Late | mandib.: 3 months; maxilla 6 months |
| Telleman et al. (2012a) | RCT | 17 | 0 | 100 | 53.7 (21–67) | 62 | Late | 3 months |
| Telleman et al. (2012b) | RCT | 78 | n. a.* | n. a.* | PS group 51.6 (27–67) PM-group 48.0 (18–70) | 106 | Late | 4 months |
| Trammell et al. (2009) | RCT | 10 | n. a. | n. a. | n. a. | 25 | n. a. | 2 months |
| Veis et al. (2010) | PCCS | n. a. | n. a. | n. a. | n. a. | 282 | n. a. | mandib.: 3–5 months; maxilla: 5–6 months |
| Vigolo & Givani (2009) | PCCS | 144 | n. a. | n. a. | 37 (25–55) | 182 | n. a. | 4 months |
PCCS prospective clinical controlled study; RCT randomized clinical trial; imm. immediate; imm. restor. immediate restoration.
Female/male ratio given for the entire cohort of study participants, but not for the sample adjusted for dropouts (n. a. = not announced).
Fig 2.
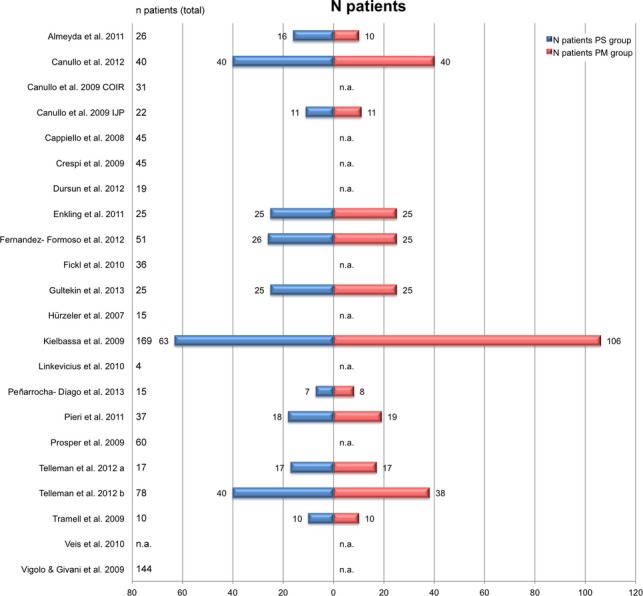
Distribution of patients among the test groups (PS) and control groups (PM). n.a., Not announced; PS, platform switching; PM, platform matching.
Fig 4.
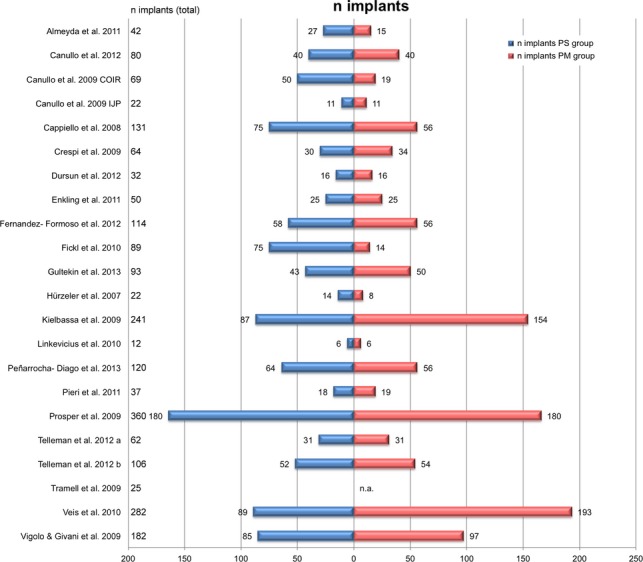
Distribution of implants among the test groups (PS) and control groups (PM). n. a., Not announced; PS, platform switching; PM, platform matching.
Fig 3.
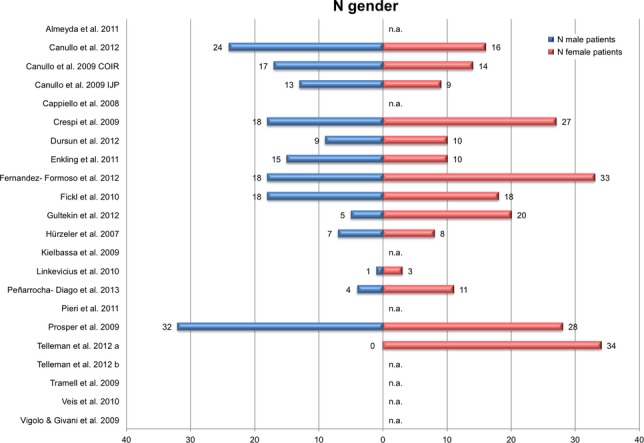
Distribution of male and female patients among the patients included for the studies. n. a., Not announced.
The search for data from unpublished studies in http://www.clinicaltrialsregister.eu/ revealed a yield of 54 registered clinical studies of which – after removing three duplicates and 45 studies not meeting the topic – six focused on the topic of platform switching. Of these, two were announced in status of patient recruitment, one was in status of finished patient recruitment and active yet, one was announced with unknown status and two were completed with results, which were not posted yet (NCT 00728884; NCT 00746187). The search in http://www.controlled-trials.com revealed 15 studies, of which one was duplicate with a study from http://www.clinicaltrialsregister.eu, two were found duplicate within the register, seven studies did not meet the topic of platform switching, three studies were in status of recruiting, one was in status of finished patient recruitment and active yet and one study was completed, but duplicate registered (NCT 00746187) in http://www.controlled-trials.com but not posting results yet. Therefore, data from unpublished studies were not available so far for further analyses, including funnel-plot analysis for possible detection bias.
Quality assessment of the included RCTs
Results of the quality assessment of RCTs are listed in Table 2, following the recommendations by Higgins and Green (2011). The difference of the assessment results was low, resulting in a κ score of 0.923 (disagreement in four of 105 fields) between the reviewers. Consent was reached by discussion.
Table 2.
Risk of bias summary among RCTs (following the recommendations of Higgins & Green 2011)
| Random sequence generation (selection bias) | Allocation concealment (selection bias) | Blinding of participants and personnel (performance bias) | Blinding of outcome assessment (detection bias) | Incomplete outcome data (attrition bias) | Selective reporting (reporting bias) | Other bias | Within-study risk of bias tendency | |
|---|---|---|---|---|---|---|---|---|
| Canullo et al. (2012) | Low | Low | Low | Low | Low | Low | Low | Low risk of bias for all key domains |
| Canullo et al. (2010) | Low | Low | Low | High | High | Low | Low | High risk of bias in two key domains |
| Canullo et al. (2009) | Low | Low | Low | Low | Low | Low | Low | Low risk of bias for all key domains |
| Crespi et al. (2009) | High | High | High | High | Low | Low | Low | High risk of bias in four key domains |
| Enkling et al. (2011) | Low | High | Low | Low | Low | Low | Low | High risk of bias in one key domain |
| Fernández-Formoso et al. (2012) | Low | Low | High | Unclear | Low | Unclear | Unclear | High risk of bias in one key domain and unclear risk of bias in three key domains |
| Gultekin et al. (2013) | Low | Low | Low | High | High | Low | Low | High risk of bias in two key domains |
| Hürzeler et al. (2007) | High | High | Low | High | Low | Low | Unclear | High risk of bias in three key domains and unclear risk of bias in one key domain |
| Kielbassa et al. (2009) | Low | Low | Low | High | High | Low | Unclear | High risk of bias in two key domains and unclear risk of bias in one key domain |
| Peñarrocha-Diago et al. (2012) | Unclear | Unclear | Low | Low | High | Low | Unclear | High risk of bias in one key domain and unclear risk of bias in three key domains |
| Pieri et al. (2011) | Low | Low | Low | High | Low | Low | Low | High risk of bias in one key domain |
| Prosper et al. (2009) | Low | Low | Low | Low | High | High | Unclear | High risk of bias in two key domains and unclear risk of bias in one key domain |
| Telleman et al. (2012a) | Low | Low | Low | Unclear | High | Low | Low | High risk of bias in one key domain and unclear risk of bias in one key domain |
| Telleman et al. (2012b) | Low | Low | Low | Low | High | Low | Low | High risk of bias in one key domain |
| Trammell et al. (2009) | Low | High | Low | High | Low | Low | Unclear | High risk of bias in two key domains and unclear risk of bias in one key domain |
Information indicating a low risk of bias was found in two studies. Three studies revealed a high risk of bias in one key domain only, two more studies revealed a high risk of bias in one key domain and an unclear risk of bias in three key domains, one study revealed a high as well as an unclear risk of bias in one key domain. For two studies a high risk of bias in two key domains, and for three studies, a high risk of bias was found for two key domains as well as one unclear risk of bias in one key domain. One study each revealed a high risk of bias in three key domains with an unclear risk for one key domain, and a high risk of bias for four key domains. Two RCTs excluded from meta-analysis revealed a high risk of bias for two key domains each, and one of these showed an unclear risk of bias for one key domain, additionally.
According to the definitions (Higgins and Green 2011), the overall ranking revealed only two studies with a low risk of bias. All other studies revealed a tendency of a high risk of bias, resulting in an overall unclear and high risk of bias across studies (see Table 8).
Systematic review
The results of RCTs with a follow-up period exceeding 12 months following the beginning of prosthetic loading are listed in Table 3. In all but one study (Crespi et al. 2009), significant differences between the mean marginal bone loss around PM implant and PS implants were found in favor of that at PS implants. The mean patient number was 34.7 (SD 17.7, range 10–60), the mean implant number was 103.3 (SD 127.98, range 22–360). The maximum follow-up period was 25 months following prosthetic loading, the minimum was 18 months following implantation. In three of the studies, a submerged healing mode was followed (Canullo et al. 2012, 2010; Prosper et al. 2009), whereas the implants in the three other studies and in another cohort of the study published by Prosper et al. (2009) healed non-submerged. Moreover, in two studies, immediate restorations were fixed on implants (Canullo et al. 2009; Crespi et al. 2009), of which the implants in the study published by Crespi et al. 2009 were exposed to immediate loading. In all but two (Canullo et al. 2012;: use of external hexagon; Crespi et al. 2009: use of internal conical connection and external hexagon) of these studies, implant-abutment connection configuration was an internal hexagonal connection type.
Table 3.
Comparison of mean bone loss considering RCTs with an observation period exceeding 12 months following prosthetic loading
| Position of implant shoulder; implant-abutment connection | Mean marginal bone loss and standard deviation (SD), PM-group (control) | Mean marginal bone loss and standard deviation (SD), PS group (test) | Level of significance | Remarks | Healing type | Duration of follow-up period | |
|---|---|---|---|---|---|---|---|
| Canullo et al. (2012) | Epicrestal EH/n.a.d. | 1.6 mm (SD 0.3) | 0.5 mm (SD 0.1) | P ≤ 0.05 | Maxillary posterior sites only, SFEA in 29 patients (58 implants) | Submerged | 18 months following prosthetic restoration |
| Canullo et al. (2010) | Epicrestal IH | 1.5 mm | 1.0–0.6 mm | P < 0.005 | SFEA, residual bone height 4 mm | Submerged | 21 months following implantation |
| Canullo et al. (2009) | Epicrestal IH | 1.2 mm (SD 0.38) | 0.3 mm (SD 0.16) | P < 0.005 | Immediate restoration without loading | Non-submerged | 25 (24–27) months following prosthetic loading |
| Crespi et al. (2009) | 1 mm subcrestal IC/EH | 0.78 mm (SD 0.45) | 0.73 mm (SD 0.52) | P > 0.05 | Immediate implants exposed to immediate loading | Non-submerged | 24 months following implantation |
| Prosper et al. (2009) | Submerged healing: epicrestal; IH non-submerged healing: supracrestal IH | 0 mm – 40.0% <0.5 mm – 28.3% <1.0 mm – 25.0% <1.5 mm – 3.3% >1.6 mm – 3.3% of submerged PM-implants 0 mm – 43.3% <0.5 mm – 20.0% <1.0 mm – 18.3% of submerged PM-implants | 0 mm – 93.3% <0.5 mm – 3.3% <1.0 mm – 3.3% of submerged PS implants 0 mm – 91.7% <0.5 mm – 5.5% <1.0 mm – 3.3% of non-submerged PS implants | P < 0.0001 P = 0.0006 | Different healing modes; platform-enlarged (PS mode only) and standard implants (PM and PS mode as well) | Submerged; non-submerged | 24 months following implantation |
| Trammell et al. (2009) | Epicrestal IH | 1.19 mm (SD 0.58) | 0.99 mm (SD 0.53) | P = 0.036 | Non-submerged | 24 months following prosthetic restoration |
PM, Platform matching; PS platform switching; SFEA sinus floor elevation and augmentation; SD standard deviation. Configuration of implant-abutment connection: EH external hexagon; IC internal conical connection; IH internal hexagon; n.a.d. not announced in detail.
Table 4 depicts the results of RCTs with a follow-up period of 12 months following the beginning of prosthetic loading. In all but one study (Kielbassa et al. 2009), significant differences between the mean marginal bone loss around PM implant and PS implant were found, again in favor of PS-implant-abutment configuration. The mean patient number was 52.0 (SD 55.02, range 15–177), the mean implant number was 109.9 (SD 94.13, range 22–325). Three studies reported a submerged healing of the implants (Gultekin et al. 2013; Fernández-Formoso et al. 2012; Peñarrocha-Diago et al. 2012), five publications reported non-submerged healing mode, of which one cohort (Fernández-Formoso et al. 2012) was comprising PM-implants. In one study, the healing mode was not clearly stated (Hürzeler et al. 2007). Two studies reported immediate implant placement into the alveolar socket and subsequent immediate restoration of implants without immediate loading (Kielbassa et al. 2009; Pieri et al. 2011). In four studies, implant-abutment connections via internal hexagon type were used (Kielbassa et al. 2009; Peñarrocha-Diago et al. 2012; Telleman et al. 2012a,b), in three studies, external hexagonal implant-abutment connections were used (Hürzeler et al. 2007; Kielbassa et al. 2009; Peñarrocha-Diago et al. 2012), two studies each reported the use of internal conical- (Fernández-Formoso et al. 2012; Gultekin et al. 2013) or internal tube-in-tube- (Kielbassa et al. 2009; Gultekin et al. 2013), and one study reported the use of internal octagonal (Pieri et al. 2011) implant-abutment connection types.
Table 4.
Comparison of mean bone loss considering RCTs with an observation period of 12 months following prosthetic loading
| Position of implant shoulder; implant-abutment connection | Mean marginal bone loss and standard deviation (SD), PM-group (control) | Mean marginal bone loss and standard deviation (SD), PS group (test) | Level of significance | Remarks | Healing type | |
|---|---|---|---|---|---|---|
| Fernández-Formoso et al. (2012) | Epicrestal IC | 2.23 mm (SD 0.22) | 0.68 mm (SD 0.88) | P < 0.001 | Submerged; non-submerged | |
| Gultekin et al. (2013) | n. a. IC/IT | 0.83 mm (SD 0.16) | 0.35 (SD 0.13) | P < 0.01 | Different implant neck and abutment configurations | Submerged |
| Hürzeler et al. (2007) | Epicrestal EH | 2.02 mm (SD 0.49) | 0.22 mm (SD 0.53) | P < 0.02 | n. a. | |
| Kielbassa et al. (2009) | n. a. IH/EH/IT | 0.63 mm (SD 1.18) | IT 0.95 mm (SD 1.37) EH 0.64 mm (SD 0.94) | P = 0.729 | Immediate placement and immediate restoration without loading | Non-submerged |
| Peñarrocha-Diago et al. (2012) | Epicrestal EH/IH | 0.38 mm (SD 0.51) | 0.12 mm (SD 0.17) | P = 0.047 | Different implant neck and abutment configurations | Submerged |
| Pieri et al. (2011) | Supracrestal IO | 0.51 mm (SD 0.24) | 0.2 mm (SD 0.17) | P = 0.0004 | Immediate placement and immediate restoration without loading | Non-submerged |
| Telleman et al. (2012a) | Epicrestal IH | 0.85 mm (SD 0.65) | 0.53 mm (SD 0.54) | P = 0.003 | Non-submerged | |
| Telleman et al. (2012b) | Epicrestal IH | 0.73 mm (SD 0.48) | 0.51 mm (SD 0.51) | P = 0.01 | Non-submerged |
Configuration of implant-abutment connection: EH external hexagon; IC internal conical connection; IH internal hexagon; IO internal octagon; IT internal tube-in-tube.
In Table 5, one study (Enkling et al. 2011) is listed, reporting no significant difference between the mean marginal bone loss of PM- and PS-implant-abutment connections after a follow-up period of up to 12 months following implantation and submerged healing. The mean marginal bone loss of the PS implants was found slightly less compared with PM implants.
Table 5.
Comparison of mean bone loss considering RCTs with an observation period of <12 months following prosthetic loading
| Position of implant shoulder | Mean marginal bone loss and standard deviation (SD), PM-group (control) | Mean marginal bone loss and standard deviation (SD), PS group (test) | Level of significance | Healing type | Duration of follow-up period | |
|---|---|---|---|---|---|---|
| Enkling et al. (2011) | Epicrestal IH | 0.58 mm (SD 0.55) | 0.53 mm (SD 0.35) | P = 0.4 | Submerged | 12 months following implantation |
Configuration of implant-abutment connection: IH internal hexagon.
Additionally, seven PCCS comprising a test group (PS-implant-abutment connection) and a control group (PM-implant-abutment connection) as well were identified by literature search within the databases, meeting the inclusion criteria. Since lacking random allocation to one of the intervention groups (PM or PS), these studies were evaluated separately (Table 6). Three studies revealed a significant difference between the marginal bone loss in PM and PS groups in favor of PS technique (Cappiello et al. 2008; Vigolo & Givani 2009; Fickl et al. 2010), one more study showed a remarkable mean marginal bone loss in the PM group compared to the PS group without statistical investigation of a significance between both groups, however (de Almeida et al. 2011). Three studies revealed no significant differences between the PM and the PS groups regarding mean marginal bone loss after up to 24 months follow-up (Linkevicius et al. 2010; Veis et al. 2010; Dursun et al. 2012), of which one study reported a sample size of four patients receiving twelve implants (Linkevicius et al. 2010). In the study published by Veis et al. 2010, only the PS subgroup of subcrestally installed implants revealed a significantly lower mean marginal bone loss, compared to the PM subgroup. This difference was not consistent for the subgroups of supracrestally or epicrestally installed implants. The mean patient number was 45.7 for these PCCS (SD 50.2, range 4–144), the mean implant number was 110 (SD 96.6, range 12–282). Four studies reported submerged healing of the implants, three groups reported non-submerged healing (Cappiello et al. 2008; Linkevicius et al. 2010; Dursun et al. 2012). In all excepting two studies (Veis et al. 2010; Vigolo & Givani 2009: use of external hexagonal implant-abutment connection), an internal hexagonal implant-abutment connection was used.
Table 6.
Comparison of bone loss considering PCCS
| Position of implant shoulder | Mean marginal bone loss PM group (control) | Mean marginal bone loss PS group (test) | Difference | Remarks | Healing type | Follow-up period | |
|---|---|---|---|---|---|---|---|
| de Almeida et al. (2011) | Subcrestal 0.7 mm (PM-group); 1.8 mm PS group) IH | 2.3 mm | 0.3 mm | n. a. | Submerged | Mean 33.4 (6–60) months following implantation | |
| Cappiello et al. (2008) | Subcrestal IH | 1.67 mm (SD 0.37) | 0.95 mm (SD 0.32) | P < 0.001 | Provisional prosthesis delivered 8 weeks following implantation in average | Non-submerged | 12 months following prosthetic loading |
| Dursun et al. (2012) | Epicrestal IH | 0.56 mm (SD 0.35) | 0.72 mm (SD 0.53) | P = 0.48 | Non-submerged | Max. 6 months following implantation | |
| Fickl et al. (2010) | Subcrestal (PS); epicrestal (PM) IH | 1.00 mm (SD 0.22) | 0.39 mm (SD 0.07) | P < 0.01 | Submerged | 12 months following prosthetic loading | |
| Linkevicius et al. (2010) | Epicrestal IH | Mesial 1.81 mm (SD 0.39) distal 1.70 mm (SD 0.25) | Mesial 1.60 mm (SD 0.46) distal 1.76 mm (SD 0.45) | P > 0.408 | Sample size: 4 patients; 12 implants | Non-submerged | 12 months following prosthetic loading |
| Veis et al. (2010) | Supracrestal | 0.60 mm (SD 0.67) | 0.69 mm (SD 0.47) | P = 0.127 | Submerged | 24 months following prosthetic restoration | |
| Epicrestal | 1.23 mm (SD 0.96) | 1.13 mm (SD 0.42) | P = 0.649 | ||||
| Subcrestal | 0.81 mm (SD 0.79) | 0.39 mm (SD 0.52) | P = 0.046 | ||||
| Total EH | 0.88 mm (SD 0.85) | 0.75 mm (SD 0.55) | P = 0.661 | ||||
| Vigolo & Givani (2009) | Epicrestal after 1 year | 0.9 mm (SD 0.3) | 0.6 mm (SD 0.2) | P < 0.05 | Submerged | 5 years following prosthetic restoration | |
| After 5 years EH | 1.1 mm (SD 0.3) | 0.6 mm (SD 0.2) |
Configuration of implant-abutment connection: EH external hexagon; IH internal hexagon; n.a., not announced.
The implants were mainly located in the posterior regions of the mandible (Trammell et al. 2009; Enkling et al. 2011; Dursun et al. 2012) or maxilla (Canullo et al. 2010, 2012), or in posterior regions of the mandible and maxilla as well (Fernández-Formoso et al. 2012; Hürzeler et al. 2007; Prosper et al. 2009; Telleman et al. 2012a,b; Vigolo & Givani 2009). Two studies reported results obtained from implant sites located in the anterior and premolar regions of the maxilla (Canullo et al. 2009), and maxilla and mandible as well (Crespi et al. 2009), one study reported results obtained from implants inserted into edentulous maxillae and mandibles (Peñarrocha-Diago et al. 2012; locations not further specified), and in various locations of the maxilla and mandible (Kielbassa et al. 2009; locations specified in detail). Implant sites were not further specified in the remaining publications (Cappiello et al. 2008; Fickl et al. 2010; Linkevicius et al. 2010; Veis et al. 2010; de Almeida et al. 2011; Pieri et al. 2011; Gultekin et al. 2013).
In four studies, information regarding the general medical health status was not reported (Hürzeler et al. 2007; Cappiello et al. 2008; Fickl et al. 2010; Veis et al. 2010), five studies stated “good health” to characterize the general health status of the included patients (Canullo et al. 2009, 2010; Crespi et al. 2009; de Almeida et al. 2011; Enkling et al. 2011). The general health status of study participants was defined by exclusion criteria in the thirteen remaining publications.
An investigation regarding the effect of tobacco smoking on MBL changes considering the PM and PS groups as well was generally not performed in the included studies. Five studies reported the exclusion of patients smoking more than 10 cigarettes per day (Canullo et al. 2009, 2010, 2012; Crespi et al. 2009; Trammell et al. 2009), in one study patients smoking more than 20 cigarettes per day were excluded from participation in the study (Pieri et al. 2011), six more studies reported exclusion of smokers generally (Prosper et al. 2009; Dursun et al. 2012; Fernández-Formoso et al. 2012; Telleman et al. 2012a,b; Gultekin et al. 2013). Peñarrocha-Diago et al. (2012) included smokers and reported three patients smoking up to ten cigarettes per day. The remaining nine studies did not provide information regarding the frequency of smokers among the included patients.
Eight of the included studies (Hürzeler et al. 2007; Crespi et al. 2009; Kielbassa et al. 2009; Vigolo & Givani 2009; Fickl et al. 2010; Veis et al. 2010; de Almeida et al. 2011; Pieri et al. 2011) did not report on the periodontal health status of the patients included into the study.
However, inclusion of periodontally compromised patients can be supposed by the fact, that patients requiring tooth removal due to periodontitis were included in two of these studies (Crespi et al. 2009; Pieri et al. 2011). Characterization of the periodontal health status of the included patients in the remaining studies was expressed by excluding patients revealing a full mouth plaque score and a full mouth bleeding score of more than 25% (Canullo et al. 2009, 2010), or by exclusion of patients suffering from untreated or active periodontitis. In the study published by Peñarrocha–Diago et al. (2012), completely edentulous patients were included only. None of the studies investigated on the impact of PS or PM technique on MBL changes in an analysis stratified for periodontally healthy or periodontally compromised patients.
In 22 included studies, 17 different implant systems were used, of which nine represented internal hexagonal implant-abutment connection configuration (Frialit-2® [Dentsply Implants, Mannheim, Germany], Global® [Sweden and Martina, Padua, Italy], Osseotite® certain [Biomet 3i, Palm Beach Gardens, FL, USA], Osseotite® prevail [Biomet 3i], SIC® Ace [SIC Invent, Basel, Switzerland], Nobel active® [Nobel Biocare, Zurich, Switzerland], Revois® [Curasan, Kleinostheim, Germany], Screw vent® [Zimmer Dental, Carlsbad, CA, USA], Winsix® [Bio SAF IN, Ancona, Italy]), three represented an internal conical connection (Ankylos® [Dentsply Implants, Mannheim, Germany], Straumann® Bone level [Straumann, Basel, Switzerland], Straumann® Tissue level [Straumann]), two represented an external hexagonal implant-abutment connection (Seven® [Sweden and Martina, Padua, Italy], Biomet 3i® [Biomet 3i, Palm Beach Gardens, FL, USA]), one represented an internal octagonal connection (Samo® [Samo Biomedica, Granarolo dell'Emilia/ Bologna, Italy]) and one was characterized as internal tube-in-tube-connection (Nobel replace® [Nobel Biocare, Zurich, Switzerland]). In one study (Canullo et al. 2012) the implant system was described briefly, but not named.
In most of the studies, periapical radiographs with standardized projections and/or paralleling technique were used and digitally measured. Enkling et al. (2011), Kielbassa et al. (2009) and Veis et al. (2010) used panoramic radiographs also. Gultekin et al. (2013) performed radiographic analyses utilizing a cone beam computed tomography. Apart from studies published by de Almeida et al. (2011), Cappiello et al. (2008), Dursun et al. (2012), Fernández-Formoso et al. (2012), Kielbassa et al. (2009), Pieri et al. (2011), Trammell et al. (2009), Veis et al. (2010), and Vigolo & Givani (2009), digital radiographs were used exclusively.
Meta-analysis
Meta-analysis was carried out, excluding two RCTs published by Canullo et al. (2010) and Prosper et al. (2009) due to lack of data reporting mean values of MBL changes comparing PS- and PM-implant-abutment configurations and their standard deviations, respectively. For meta-analysis, summary measures of each included study (mean values of MBL changes comparing PS- and PM-implant-abutment configurations) were used only, since individual data were not available and could not be extracted from the studies. Included RCTs comprised a total of 549 patients receiving 1035 implants. Due to the heterogeneous but relatively short follow-up periods (one study each reporting a follow-up of 12 months following implantation, 18 months following prosthetic loading, 25 months following prosthetic loading, two studies reporting a follow-up of 24 months following implantation, and eight studies reporting a follow-up of 12 months following prosthetic loading), a subgroup analysis of these studies concerning different observation periods was not performed.
Funnel-plot calculation showed no asymmetry (P = 0.733), revealing no evidence supporting bias of selected studies (Fig. 5), and therefore, the null-hypothesis assuming no publication bias was not rejected.
Fig 5.
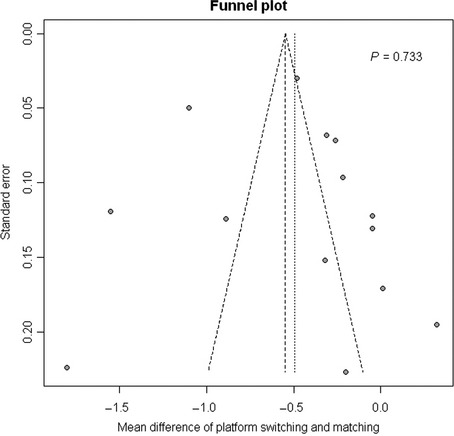
Funnel plot of mean differences of mean marginal bone loss at implants with PS- and PM-implant-abutment configurations. PS, Platform switching; PM, platform matching.
The DerSimonian–Laird estimate for inter study variance τ2 = 0.182 (I2 = 96.2%) was found significantly different from 0 (P < 0.0001), indicating a substantial degree of heterogeneity. Therefore, treatment effects were assumed to be not homogeneous among the studies considered, and a random effects model for combining effects of all studies was applied. Mean difference of marginal bone loss of 0.49 mm (CI95% 0.26; 0.73) between PM implants and PS implants was found significantly different from 0 (P < 0.0001, mixed effects model). Mean bone loss for PS implants was 0.49 mm (CI95% 0.38; 0.60) and 1.01 mm (CI95% 0.62; 1.40) for PM-implants. Fig. 6 depicts the forest plot of mean differences of marginal bone loss between PS and PM implants on an implant-based analysis.
Fig 6.
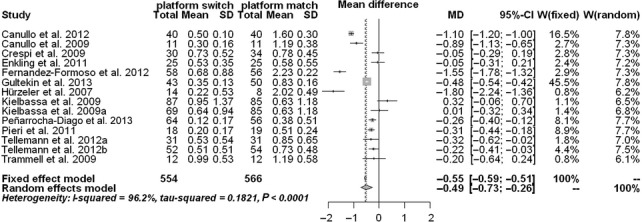
Forest plot of mean differences of effects of PS and PM on marginal bone level changes and two-sided CI95% of all treatment effects. PS, Platform switching; PM, platform matching.
Discussion
The systematic review and meta-analysis were conducted to address the focused question, whether there is an impact of platform switching on MBL changes around endosseous implants. Among other success criteria, the change of the peri-implant bone level is considered an important criterion for the evaluation of implant therapy outcome and an evidence for the presence or absence of peri-implant tissue health (Albrektsson et al. 1986; Laurell & Lundgren 2011; Papaspyridakos et al. 2012). Therefore, efforts were made to preserve the peri-implant MBL stable following and throughout the prosthetic loading phase. PS technique was supposed to be one of the technical-driven factors to achieve marginal or crestal bone stability. Recently, published systematic reviews and meta-analyses supported this assumption by confirming the effectiveness of the PS technique, significantly limiting marginal bone resorption around endosseous dental implants, while the cumulative estimated implant success rate was detected to reveal no statistically significant difference between both intervention groups of PS and PM implants (Atieh et al. 2010; Annibali et al. 2012). However, both groups of authors cautiously summarize their findings, especially emphasizing the bone-preserving effects on large-diameter implants (Annibali et al. 2012) or the extent of the implant-abutment mismatch (Atieh et al. 2010).
Nevertheless, within the limitations of the recently published RCTs included for meta-analysis presented here, the results of former systematic reviews could be confirmed, revealing a significant difference between the mean MBL change at endosseous implants with a PS- compared to a PM-implant-abutment configuration in favor of less bone loss utilizing PS-implant-abutment configurations. These findings were supported by the results of the qualitative analysis of RCTs and PCCS, revealing a tendency in favor of the PS technique.
Although English language articles were included into this systematic review only and a publication bias cannot be excluded for this reason, a cornucopia of articles addressing the technique and effects of PS were found via electronic databases, of which 22 met the inclusion criteria for this systematic review, and 13 were found eligible to be included into meta-analysis, following the PRISMA recommendations (Moher et al. 2009).
Significant differences of peri-implant MBL changes favoring the PS technique were found in five out of six RCTs with a follow-up period exceeding 12 months and in seven of eight RCTs with a 12-month follow-up following prosthetic loading. A single RCT reporting a follow-up of 12 months following implant insertion failed to show a significant impact of the PS technique on peri-implant MBL changes (Enkling et al. 2011). Considering the results of PCCS included into this systematic review, only three studies indicated a peri-implant MBL change significantly less in the PS groups compared to those utilizing PM-implant-abutment connections. In one study, this difference was remarkable in favor of the PS group obviously, but a statistical analysis to calculate the level of significance was not performed (de Almeida et al. 2011). Three of the PCCS revealed no significant differences between both treatment groups. Summarizing the findings of the included publications, especially among the RCTs remarkably more studies indicated results favoring significantly the PS technique to prevent MBL changes, than did the outcomes of PCCS included into this systematic review. Therefore, heterogeneity among the study conditions is supposed to have a crucial influence on study outcomes. Nevertheless, meta-analysis of 13 RCTs revealed a significantly less mean MBL change at PS implants compared with PM implants, thus confirming the supposed bone level stabilizing effect of PS-implant-abutment configurations at least when considering short-term observations. The longest follow-up period within the RCTs was reported up to 27 months (25 months in average) by Canullo et al. (2009), whereas the longest follow-up period within the PCCS was reported 5 years (Vigolo & Givani 2009).
Investigations on methodological quality of the RCTs included revealed that most informations were obtained from studies with an unclear or high risk of bias for one or more key domains. Due to the nature of the studies, a personnel blinding was excluded from assessment of performance bias. As only a few studies reported on radiographic examiners different from surgeons involved in the patients′ treatment, the bias concerning the outcome assessment was rated unclear or high in 10 of 15 RCTs. Drop-outs accounted for attrition bias in seven of 15 RCTs. Due to the risk of bias, the results of the meta-analysis should be interpreted with caution.
Several implant-, clinician-, and patient-related factors may contribute to marginal bone loss, which were found varying among the included studies, or were not addressed while characterizing the included patients.
Significant differences in peri-implant MBL changes considering several implant shape and surface configurations were found within a systematic review (Esposito et al. 2007), but these differences disappeared in the meta-analysis. However, rough implant surfaces were found more susceptible for inflammatory peri-implant tissue destruction compared to titanium implants with turned surfaces (Esposito et al. 2007).
The influence of periodontal disease of the included patients was not addressed in none of the studies. However, periodontally compromised patients may exhibit significantly peri-implant marginal bone loss compared to periodontally healthy subjects (Karoussis et al. 2007; Ong et al. 2008). Especially periodontally compromised smoking patients with treated periodontitis revealed significantly more peri-implant marginal bone loss compared to periodontally healthy smokers (Aglietta et al. 2011), therefore smoking and the history of periodontitis should be considered risk factors for marginal bone loss around endosseous implants. Among patient-related factors, smoking alone has a detrimental effect on early bone tissue response even around moderately roughened oxidized implant surfaces (Shibli et al. 2010) and is considered to be associated with increased peri-implant marginal bone loss (Feloutzis et al. 2003; Peñarrocha et al. 2004; Aalam & Nowzari 2005; Strietzel et al. 2007; Heitz-Mayfield & Huynh-Ba 2009; Aglietta et al. 2011; Albrektsson et al. 2012). None of the studies included into this systematic review, investigated the effects of PS on peri-implant marginal bone loss among smokers compared with non-smokers.
In some of the studies insertion depths differed (de Almeida et al. 2011; Fickl et al. 2010; Prosper et al. 2009; Veis et al. 2010), some others reported results obtained with different implant systems with different diameters and different distances between the abutment diameter and the diameter of the implant neck (Crespi et al. 2009; Kielbassa et al. 2009; Dursun et al. 2012; Fernández-Formoso et al. 2012; Peñarrocha-Diago et al. 2012). Moreover, the studies differed regarding the use of implant-abutment connection type and the surface texture at the implant neck. Therefore, results of the meta-analysis – even when revealing significant differences of mean marginal bone loss favoring the PS technique within limited observation periods – should be interpreted with caution.
Future investigations on the effect of PS should consider a uniform design of RCTs preferably, with comparable conditions regarding the implant and abutment diameter, the implant-abutment connection type, the implant surface at the neck portion and insertion depth as well as longer observation periods of at least 5 years. Patient-related confounding factors for peri-implant marginal bone loss (e.g., medical history, history of periodontitis, smoking) should be considered in evaluating study designs for investigations on PS effects on the peri-implant MBL too.
Summary
The meta-analysis of 13 RCTs revealed a significantly less mean MBL change at implants with a PS-implant-abutment configuration compared with PM-implant-abutment design. These results were obtained from studies with unclear as well as high risk of bias mostly. The mean observation periods were short, ranging between 12 months following implantation up to 25 months following prosthetic loading. However, within the limits of the recently available publications of RCTs and PCCS, the tendency revealing from the studies′ results favors the PS technique to prevent or minimize peri-implant marginal bone loss, compared to implants with PM abutments.
Due to heterogeneity of the 22 included studies, their results must be interpreted cautiously, and the answer to the focused questions whether platform switching has an impact on MBL changes around endosseous implants remains controversial.
Besides longer observation periods, further investigations on the effects of PS should consider a uniform and comparable study design while excluding or exactly documenting possible confounding factors.
Acknowledgments
Dr. Christine Haas from the German Institute for Medical Documentation and Information is gratefully acknowledged for her valuable advice concerning the search of data from clinical trials yet unpublished.
Appendix
Table A1.
PRISMA checklist
| Section/topic | Item no. | Checklist item | Reported on page no. |
|---|---|---|---|
| Title | 1 | Impact of platform switching on marginal peri-implant bone-level changes. A wsystematic review and meta-analysis. | 1 |
| Abstract | |||
| Structured summary | 2 | Objective: To address the focused question: Is there an impact of platform switching (PS) on marginal bone-level changes around endosseous implants compared to implants with platform-matching (PM) implant-abutment configurations? | 2 |
| Material and methods: A systematic literature search was conducted using electronic databases PubMed, Web of Science, Journals@Ovid Full Text and Embase and manual search for human randomized clinical trials (RCTs) and prospective clinical controlled cohort studies (PCCS) reporting on marginal bone level changes at implants platform switching, compared to platform-matching implant-abutment connections, published between 2005 and June 2013, following the recommendations for preferred reporting items for systematic reviews and meta-analyses (PRISMA) | |||
| Results: 22 publications were found eligible for the systematic review. The qualitative analysis of 15 RCTs and 7 PCCS revealed more studies (13 of 15 RCTs and three out of seven PCCS) showing a significantly less mean marginal bone level change around implants with PS implant-abutment connections compared to PM-implant-abutment connections, thus indicating a clear tendency favoring the platform-switching technique. A meta-analysis including 13 RCTs revealed a significantly less mean marginal bone-level change (0.49 mm CI95% [0.38; 0.60]) at PS implants compared to PM implants (1.01 mm [CI95% 0.62; 1.40] (P < 0.0001) on an implant-based analysis | |||
| Conclusions: The Meta-analysis revealed a significantly less mean marginal bone-level change at implants with a PS implant-abutment configuration compared with PM implant-abutment design. These results were from studies with unclear as well as high risk of bias mostly and relatively short follow-up periods. The qualitative analysis of RCTs and PCCS revealed a tendency favoring the PS technique to prevent or minimize peri-implant marginal bone loss, compared to PM technique. Due to heterogeneity of the included studies, their results require cautious interpretation. Besides longer observation periods, further investigations should consider a uniform and comparable study design while excluding or exactly documenting possible confounding factors | |||
| Introduction | |||
| Rationale | 3 | The radiographically detectable peri-implant bone level following prosthetic loading is considered one of the relevant success criteria for evaluating dental implant therapy outcomes. Marginal bone loss may occur around dental implants due to peri-implant infections, but also for other reasons. A limited amount of crestal or marginal bone loss is supposed to be a biologic response to implant placement procedure. Since introduction of the platform-switching concept into construction of implant systems and abutment configurations, their experimental impact on peri-implant bone level alterations was studied in various finite-element, in vivo, and clinical studies as well. Platform switching is considered as the changing of an implant abutment to one with a smaller diameter, so as to place the implant-abutment interface medial to the edge of the implant platform. The relatively short follow-up periods of most studies focusing on the effect of platform switching on marginal bone loss compared to platform matching implant-abutment configurations and different sample sizes led to different conclusions even in systematic reviews, ranging from not revealing any clinical superiority for any particular implant design in maintaining marginal bone levels to recognizing the platform switching technique as appearing useful in limiting bone resorption. Therefore, the rationale for this systematic review and meta-analysis was to systematically review the publications of RCTs and PCCS regarding the impact of platform switching on marginal bone level changes around endosseous implants compared with platform-matching implant-abutment configurations, to identify the need of and to develop recommendations for future research | 3 |
| Objective | 4 | To address the focused question: Is there an impact of platform switching (PS) on marginal bone-level changes around endosseous implants compared to implants with platform-matching (PM) implant-abutment configurations? | 4 |
| Methods | |||
| Protocol | 5 | A systematic literature search in electronic databases was conducted, studies were selected according to predefined inclusion criteria, following a review protocol and a search strategy, described in the Material and methods section | 5, 6 |
| The authors were invited to perform a systematic review on the topic of periimplant marginal bone loss at implants with platform-switching or platform-matching implant-abutment configurations by the Camlog foundation | 2 | ||
| Eligibility criteria | 6 | Randomized controlled trials and prospective clinical controlled studies in humans were selected only, published between 2005 and June 2013 in English or German, following the PICO format. P: population [patients undergoing implant-prosthetic rehabilitation, which were included into randomized controlled clinical trials or prospective controlled clinical studies, comparing peri-implant marginal bone loss around endosseous implants with platform-switching (PS) or platform-matching (PM) implant-abutment-configurations]; I: intervention [use of endosseous dental implants with a PM (the abutment diameter and implant neck diameter were identical) or PS (the abutment diameter was medialized compared to the implant neck diameter) implant-abutment-configuration]; C: comparison, and O: outcome [clinical studies comparing treatment outcomes using PM and PS implants with special consideration of radiographically detected peri-implant marginal bone level changes were considered for evaluation] | 5 |
| Information sources | 7 | Data bases: PubMed/Medline, Web of Science, Journals@Ovid Full Text, Embase. Handsearch: German-language peer-reviewed journals Journal of Oral Implantology (Zeitschrift fuer zahnaerztliche Implantologie) or Implantologie | 6 |
| For detection of unpublished data from clinical studies: http://apps.who.int/trialsearch/; http://www.clinicaltrialsregister.eu/; http://www.clinicaltrials.gov; http://www.centerwatch.com; http://www.controlled-trials.com | 7 | ||
| Search | 8 | For PubMed/Medline, Web of Science, Journals@Ovid Full Text, Embase, the following search strategy was used: Population/Patients/Intervention/Control “dental implant-abutment design”[MeSH Terms] OR (“dental”[All Fields] AND “implant-abutment”[All Fields] AND “design”[All Fields]) OR “dental implant-abutment design”[All Fields] OR (“dental”[All Fields] AND “implant”[All Fields] AND “platform”[All Fields] AND “switching”[All Fields]) OR (“dental implants”[MeSH Terms] OR (“dental”[All Fields] AND “implants”[All Fields]) OR “dental implants”[All Fields] OR (“dental”[All Fields] AND “implant”[All Fields]) OR “dental implant”[All Fields]) AND (platform[All Fields] AND switching[All Fields]) | 6 |
| OR (“dental implants”[MeSH Terms] OR (“dental”[All Fields] AND “implants”[All Fields]) OR “dental implants”[All Fields] OR (“dental”[All Fields] AND “implant”[All Fields]) OR “dental implant”[All Fields]) AND (platform[All Fields] AND switching[All Fields]) AND crestal[All Fields] Outcome (“dental implants”[MeSH Terms] OR (“dental”[All Fields] AND “implants”[All Fields]) OR “dental implants”[All Fields] OR (“dental”[All Fields] AND “implant”[All Fields]) OR “dental implant”[All Fields]) AND (crestal[All Fields] AND (“bone and bones”[MeSH Terms] OR (“bone”[All Fields] AND “bones”[All Fields]) OR “bone and bones”[All Fields] OR “bone”[All Fields]) AND level[All Fields]) OR (“dental implants”[MeSH Terms] OR (“dental”[All Fields] AND “implants”[All Fields]) OR “dental implants”[All Fields] OR (“dental”[All Fields] AND “implant”[All Fields]) OR “dental implant”[All Fields]) AND ((“bone and bones”[MeSH Terms] OR (“bone”[All Fields] AND “bones”[All Fields]) OR “bone and bones”[All Fields] OR “bone”[All Fields]) AND level[All Fields] AND (“Change”[Journal] OR “change”[All Fields])) OR (“dental implants”[MeSH Terms] OR (“dental”[All Fields] AND “implants”[All Fields]) OR “dental implants”[All Fields]) AND ((“bone and bones”[MeSH Terms] OR (“bone”[All Fields] AND “bones”[All Fields]) OR “bone and bones”[All Fields] OR “bone”[All Fields]) AND level[All Fields] AND (“Change”[Journal] OR “change”[All Fields])). Limits: humans; randomized controlled trial; controlled clinical trial; systematic reviews; meta-analysis; abstract available; language: English, German; date of publication January, 2005 up to June, 2013 | |||
| Study selection | 9 | See Fig. 1: Search strategy and results of identification, screening for eligibility and inclusion of publications considered for systematic review and meta-analysis. Disagreement between the reviewers was resolved by consensus | 5 |
| Data collection process | 10 | Data figuring predefined items of each study published were extracted independently by two reviewers (FPS and MH) into tables, compared and confirmed thereafter | 8 |
| Data items | 11 | Data regarding following items were extracted: sample size (numbers of male and female patients, implants), duration of observation period considering implantation date and date of prosthetic loading as well as last follow-up, mean age | 6 |
| Data reporting mean values of radiographically detected marginal bone-level changes and their standard deviations from RCTs were used for meta-analysis only | |||
| Additionally, data reporting mean values of radiographically detected marginal bone level changes from RCTs and PCCS were used for systematic review | |||
| Risk of bias | 12 | A quality assessment of the studies included for the systematic review and for meta-analysis was done following the Cochrane collaboration recommendations for evaluation of RCTs (Higgins & Green 2011), focusing on the following criteria: random sequence generation and allocation concealment (both accounting for selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), or other possible causes of bias | 7 |
| Summary measures | 13 | The primary measure of the effect of PM- compared to PM-implant-abutment configuration was the radiographically detectable mean marginal bone level change and its standard deviation between the baseline and the end of the follow-up period | 8 |
| Planned method of analysis; synthesis of results | 14 | Meta-Analysis: Statistical heterogeneity among the RCTs selected for meta-analysis was planned to be assessed utilizing the DerSimonian-Laird estimate for inter study variance. If heterogeneity of the studies would be detected, a random effects model was planned to be performed for meta-analysis. A forest plot was planned to be calculated to investigate on a possible difference between the mean marginal bone loss in the groups of PS- compared with PM-implant-abutment configurations on an implant-based analysis | 8 |
| Risk of bias across studies | 15 | A funnel plot was planned to be calculated to detect a possible bias in the selection of studies, and a test for funnel-plot asymmetry was carried out based on linear regression. | 8 |
| Additional analysis | 16 | ||
| Results | |||
| Study selection | 17 | Identification of studies within the databases and handsearch as indicated in the text and in item 7: Records identified through electronic database searching (after removing duplicates): 804 Records identified through hand searching: 3 Screening: Records screened 807 Records excluded (not matching the inclusion criteria) 784 Eligibility: Full-text articles assessed for eligibility 23 Full-text articles excluded for not fulfilling the exclusion criteria 1 Inclusion: Studies included for qualitative synthesis 22 Studies not eligible for meta-analysis 9 Studies included for quantitative synthesis 13 See flow diagram Fig. 1 | 8 |
| Study characteristics | 18 | All studies finally selected for meta-analysis were RCTs performed in humans, published in English language. The study samples included comprised 549 patients receiving a total of 1035 implants. The follow-up period ranged between 12 months following implantation up to 25 months following prosthetic loading. See Tables 1 and 5 also | 9 |
| Risk of bias within studies | 19 | See Tables 2 and 8 | |
| Results of individual studies | 20 | See Fig. 6 | |
| Synthesis of results | 21 | The DerSimonian–Laird estimate for inter study variance τ2 = 0.182 was found significantly different from 0 (P < 0.0001). Therefore, treatment effects were assumed to be not homogeneous among the studies considered, and a random effects model for combining effects of all studies was applied | 13 |
| Mean differences of marginal bone loss of 0.49 mm (CI95% 0.38; 0.60) at PS implants and of 1.01 mm (CI95% 0.62; 1.40) at PM implants were found significantly different (P < 0.0001, mixed effects model). | |||
| Risk of bias across studies | 22 | Funnel-plot calculation showed no asymmetry (P = 0.733), revealing no evidence supporting bias of study selection (see Fig. 5). Assessment of methodological quality of the studies revealed an unclear or high risk of bias | 13 9 |
| Additional analysis | 23 | ||
| Discussion Summary of evidence | 24 | Among other success criteria, the change of the peri-implant bone level is considered an important criterion for the evaluation of implant therapy outcome and an evidence for the presence or absence of peri-implant tissue health. PS technique was supposed to be one of the technical-driven factors to achieve marginal or crestal bone stability. Within the limitations of the recently published RCTs included for meta-analysis presented here, revealed a significant difference between the mean marginal bone level change at endosseous implants with a PS- compared to a PM-implant-abutment configuration in favor of less bone loss utilizing PS-implant-abutment configurations (see item No. 21). These findings were supported by the results of the qualitative analysis of RCTs and PCCS, revealing a tendency in favor of the PS technique. Significant differences of peri-implant marginal bone-level changes favoring the platform-switching technique were found in five out of six RCTs with a follow-up period exceeding 12 months and in seven of eight RCTs with a 12-month follow-up following prosthetic loading. A single RCT reporting a follow-up of 12 months following implant insertion failed to show a significant impact of the platform-switching technique on peri-implant marginal bone-level changes (Enkling et al. 2011). Considering the results of PCCS included into this systematic review, three studies indicated a peri-implant marginal bone level change significantly less in the PS groups compared with those utilizing PM-implant-abutment connections. In one study, this difference was remarkable in favor of the platform-switching group obviously, but a statistical analysis to calculate the level of significance was not performed. Three of the PCCS revealed no significant differences between both treatment groups. Summarizing the findings of the included publications, especially among the RCTs remarkably more studies indicated results favoring significantly the platform-switching technique to prevent marginal bone-level changes, than did the outcomes of PCCS included into this systematic review | 13 |
| Limitations | 25 | Heterogenous methodology was found in most of the studies, accounting for an unclear or high risk of bias across the studies. Follow-up periods of RCTs included were short. Potential confounders (medical history, smoking status, periodontal status) known to interfere with the health of peri-implant tissues and marginal bone level as well were not addressed in most of the studies. Among 22 studies, use of 17 different implant systems with different implant neck geometry and configuration as well as surface texture of the implant neck were reported. Among some of the studies, the insertion depth of the implant neck portion differed | 15 |
| Conclusions | 26 | Meta-analysis of 13 RCTs revealed a significantly less mean marginal bone level change at implants with a PS implant-abutment configuration compared to PM-implant-abutment design. These results were from studies with unclear as well as high risk of bias mostly and relatively short follow-up periods, ranging between 12 months following implantation up to 25 months following prosthetic loading Within the limits of available publications of RCTs and PCCS, the qualitative analysis revealed a tendency favoring the PS technique to prevent or minimize peri-implant marginal bone loss, compared to implants with PM abutments Due to heterogeneity of the 22 included studies, and even of those 13 RCTs included for meta-analysis, their results require cautious interpretation. Therefore, the answer to the focused question whether platform switching has an impact on marginal bone level changes around endosseous implants remains controversial. Besides longer observation periods, further investigations should consider a uniform and comparable study design while excluding or exactly documenting possible confounding factors | 16 |
| Funding | 27 | The preparation and presentation of this systematic review was supported by an unrestricted grant provided by the Camlog foundation, Basel, Switzerland | 2 |
Table A2.
Summary of assessment of risk of bias of RCTs (frequency distributions in %)
| Risk of bias | Selection bias | Performance bias | Detection bias | Attrition bias | Reporting bias | Other bias |
|---|---|---|---|---|---|---|
| Low | 73.3 | 86.7 | 33.3 | 53.3 | 86.6 | 60.0 |
| Unclear | 6.7 | 0 | 20.0 | 0 | 6.7 | 40.0 |
| High | 20.0 | 13.3 | 46.6 | 46.7 | 6.7 | 0 |
Conflict of interest
The authors declare no conflict of interest. None of the authors received any benefit of any kind from commercial or official parties related directly or indirectly to the subject matter of this article. Two of the authors (FPS and MH) use – among several other implant systems – Camlog implants in their daily clinical work.
Source of funding
The preparation and presentation of this systematic review was supported by an unrestricted grant provided by the Camlog Foundation, Basel, Switzerland.
References
- Aalam AA, Nowzari H. Clinical evaluation of dental implants with surfaces roughened by anodic oxidation, dual acid-etched implants, and machined implants. The International Journal of Oral and Maxillofacial Implants. 2005;20:793–798. [PubMed] [Google Scholar]
- Aglietta M, Siciliano VI, Rasperini G, Cafiero C, Lang NP, Salvi GE. A 10-year retrospective analysis of marginal bone level changes around implants in periodontally healthy and periodontally compromised tobacco smokers. Clinical Oral Implants Research. 2011;22:47–53. doi: 10.1111/j.1600-0501.2010.01977.x. [DOI] [PubMed] [Google Scholar]
- Albrektsson T, Zarb GA, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. The International Journal of Oral Maxillofacial Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- Albrektsson T, Buser D, Sennerby L. On crestal/marginal bone loss around dental implants. The International Journal of Prosthodontics. 2012;25:320–322. [PubMed] [Google Scholar]
- Al-Nsour MM, Chan H-L, Wang H-L. Effect of platform-switching technique on preservation of peri-implant marginal bone: a systematic review. The International Journal of Oral Maxillofacial Implants. 2012;27:138–145. [PubMed] [Google Scholar]
- Annibali S, Bignozzi I, Cristalli MP, La Monaca G, Polimeni A. Peri-implant marginal bone level: a systematic review and meta-analysis of studies comparing platform switching versus conventionally restored implants. Journal of Clinical Periodontology. 2012;39:1097–1113. doi: 10.1111/j.1600-051X.2012.01930.x. [DOI] [PubMed] [Google Scholar]
- Atieh MA, Ibrahim HM, Atieh AH. Platform switching for marginal bone preservation around dental implants: a systematic review and meta-analysis. Journal of Periodontology. 2010;81:1350–1366. doi: 10.1902/jop.2010.100232. [DOI] [PubMed] [Google Scholar]
- Becker J, Ferrari D, Herten M, Kirsch A, Schaer A, Schwarz F. Influence of platform switching on crestal bone changes at non-submerged titanium implants: a histomorphometrical study in dogs. Journal of Clinical Periodontology. 2007;34:1089–1096. doi: 10.1111/j.1600-051X.2007.01155.x. [DOI] [PubMed] [Google Scholar]
- Becker J, Ferrari D, Mihatovic I, Sahm N, Schaer A, Schwarz F. Stability of crestal bone level at platform-switched non-submerged titanium implants: a histomorphometrical study in dogs. Journal of Clinical Periodontology. 2009;36:532–539. doi: 10.1111/j.1600-051X.2009.01413.x. [DOI] [PubMed] [Google Scholar]
- Canullo L, Rasperini G. Preservation of peri-implant soft and hard tissues using platform switching of implants placed in immediate extraction sockets: a proof-of-concept study with 12- to 36-months follow-up. The International Journal of Oral and Maxillofacial Implants. 2007;22:995–1000. [PubMed] [Google Scholar]
- Cochran DL, Bosshardt DD, Grize L, Higginbottom FL, Jones AA, Jung RE, Wieland M, Dard M. Bone response to loaded implants with non-matching implant-abutment diameters in the canine mandible. Journal of Periodontology. 2009;80:609–617. doi: 10.1902/jop.2009.080323. [DOI] [PubMed] [Google Scholar]
- Esposito M, Murray-Curtis L, Grusovin MG, Coulthard P, Worthington HV. Interventions for replacing missing teeth: different types of dental implants. Cochrane Database of Systematic Reviews. 2007;17:CD003815. doi: 10.1002/14651858.CD003815.pub3. [DOI] [PubMed] [Google Scholar]
- Feloutzis A, Lang NP, Tonetti MS, Burgin W, Brägger U, Buser D, Duff GW, Kornman KS. IL-1 gene polymorphism and smoking as risk factors for peri-implant bone loss in a well-maintained population. Clinical Oral Implants Research. 2003;14:10–17. doi: 10.1034/j.1600-0501.2003.140102.x. [DOI] [PubMed] [Google Scholar]
- Ferraz CC, Anchieta RB, de Almeida EO, Freitas Júnior AC, Ferraz FC, Machado LS, Rocha EP. Influence of microthreads and platform switching on stress distribution in bone using angled abutments. Journal of Prosthodontic Research. 2012;56:256–263. doi: 10.1016/j.jpor.2012.02.002. [DOI] [PubMed] [Google Scholar]
- Heitz-Mayfield LJA, Huynh-Ba G. History of treated periodontitis and smoking as risks for implant therapy. The International Journal of Oral Maxillofacial Implants. 2009;24(Suppl):39–68. [PubMed] [Google Scholar]
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. 2011. Version 5.1.0. http://handbook.cochrane.org/ [Google Scholar]
- Jung RE, Jones AA, Higginbottom FL, Wilson TG, Schoolfield J, Buser D, Hämmerle CH, Cochran DL. The influence of non-matching implant and abutment diameters on radiographic crestal bone levels in dogs. Journal of Periodontology. 2008;79:260–270. doi: 10.1902/jop.2008.070132. [DOI] [PubMed] [Google Scholar]
- Karoussis IK, Kotsovilis S, Fourmousis I. A comprehensive and critical review of the dental implant prognosis in periodontally compromised partially edentulous patients. Clinical Oral Implants Research. 2007;18:669–679. doi: 10.1111/j.1600-0501.2007.01406.x. [DOI] [PubMed] [Google Scholar]
- Laney WR. Glossary of Oral and Maxillofacial Implants. Berlin: Quintessence; 2007. p. 128. [DOI] [PubMed] [Google Scholar]
- Lang NP, Jepsen S. Consensus report. Implant surfaces and design (working group 4) Clinical Oral Implants Research. 2009;20(Suppl 4):228–231. doi: 10.1111/j.1600-0501.2009.01771.x. [DOI] [PubMed] [Google Scholar]
- Laurell L, Lundgren D. Marginal bone level changes at dental implants after 5 years in function: a meta-analysis. Clinical Implant Dentistry and Related Research. 2011;13:19–28. doi: 10.1111/j.1708-8208.2009.00182.x. [DOI] [PubMed] [Google Scholar]
- Lazzara RJ, Porter SS. A new concept in implant dentistry for controlling postrestorative crestal bone levels. The International Journal of Periodontics and Restorative Dentistry. 2006;26:9–17. [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG the Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Journal of Clinical Epidemiology. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Ong CTT, Ivanovski S, Needleman IG, Retzepi M, Moles DR, Tonetti MS, Donos N. Systematic review of implant outcomes in treated periodontitis subjects. Journal of Clinical Periodontology. 2008;35:438–462. doi: 10.1111/j.1600-051X.2008.01207.x. [DOI] [PubMed] [Google Scholar]
- Papaspyridakos P, Chen C-J, Singh M, Weber HP, Gallucci GO. Success criteria in implant dentistry: a systematic review. Journal of Dental Research. 2012;91:242–248. doi: 10.1177/0022034511431252. [DOI] [PubMed] [Google Scholar]
- Peñarrocha M, Palomar M, Sanchis JM, Guarinos J, Balaguer J. Radiologic study of marginal bone loss around dental implants and its relationship to smoking, implant location, and morphology. The International Journal of Oral Maxillofacial Implants. 2004;19:861–867. [PubMed] [Google Scholar]
- Shibli JA, Iezzi G, Cardoso LA, Onuma T, de Carvalho PSP, d′Avila S, Ferrari DS, Mangano C, Zenóbio EG. Effect of smoking on early bone healing around oxidized surfaces: a prospective, controlled study in human jaws. Journal of Periodontology. 2010;81:575–583. doi: 10.1902/jop.2010.090493. [DOI] [PubMed] [Google Scholar]
- Strietzel FP, Reichart PA, Kale A, Kulkarni M, Wegner B, Küchler I. Smoking interferes with the prognosis of dental implant treatment: a systematic review and meta-analysis. Journal of Clinical Periodontology. 2007;34:523–544. doi: 10.1111/j.1600-051X.2007.01083.x. [DOI] [PubMed] [Google Scholar]
References included for systematic review (qualitative analysis)
- de Almeida FD, Carvalho ACP, Fontes M, Pedrosa A, Costa R, Noleto JW, de Almeida Barros Mourao CF. Radiographic evaluation of marginal bone level around internal-hex implants with switched platform: a clinical case report series. The International Journal of Oral Maxillofacial Implants. 2011;26:587–592. [PubMed] [Google Scholar]
- Cappiello M, Luongo R, di Iorio D, Bugea C, Cocchetto R, Celletti R. Evaluation of peri-implant bone loss around platform-switched implants. The International Journal of Periodontics and Restorative Dentistry. 2008;28:347–355. [PubMed] [Google Scholar]
- Dursun E, Tulunoglu I, Canpinar P, Uysal S, Akalin FA, Tözüm TF. Are marginal bone levels and implant stability affected by single-stage platform switched dental implants? A comparative clinical study. Clinical Oral Implants Research. 2012;23:1161–1167. doi: 10.1111/j.1600-0501.2011.02277.x. [DOI] [PubMed] [Google Scholar]
- Fickl S, Zuhr O, Stein JM, Hürzeler MB. Peri-implant bone level around implants with platform-switched abutments. The International Journal of Oral Maxillofacial Implants. 2010;25:577–581. [PubMed] [Google Scholar]
- Linkevicius T, Apse P, Grybauskas S, Puisys A. Influence of thin mucosal tissues on crestal bone stability around implants with platform switching: a 1-year pilot study. Journal of Oral and Maxillofacial Surgery. 2010;68:2272–2277. doi: 10.1016/j.joms.2009.08.018. [DOI] [PubMed] [Google Scholar]
- Veis A, Parissis N, Tsirlis A, Papadeli C, Marinis G, Zogakis A. Evaluation of peri-implant marginal bone loss using modified abutment connections at various crestal level placements. The International Journal of Periodontics and Restorative Dentistry. 2010;30:609–617. [PubMed] [Google Scholar]
- Vigolo P, Givani A. Platform-switched restorations on wide-diameter implants: a 5-year clinical prospective study. The International Journal of Oral Maxillofacial Implants. 2009;24:103–109. [PubMed] [Google Scholar]
References included for meta-analysis
- Canullo L, Fedele GR, Iannello G, Jepsen S. Platform switching and marginal bone level alterations: the results of a randomized-controlled trial. Clinical Oral Implants Research. 2010;21:115–121. doi: 10.1111/j.1600-0501.2009.01867.x. [DOI] [PubMed] [Google Scholar]
- Canullo L, Goglia G, Iurlaro G, Iannello G. Short-term bone level observations associated with platform switching in immediately placed and restored single maxillary implants: a preliminary report. International Journal of Prosthodontics. 2009;22:277–282. [PubMed] [Google Scholar]
- Canullo L, Rosa JC, Pinto VS, Francischone CE, Götz W. Inward-inclined implant platform for the amplified platform-switching concept: 18-month follow-up report of a prospective randomized matched-pair controlled trial. The International Journal of Oral and Maxillofacial Implants. 2012;27:927–934. [PubMed] [Google Scholar]
- Crespi R, Capparè P, Gherlone E. Radiographic evaluation of marginal bone levels around platform-switched and non-platform-switched implants used in an immediate loading protocol. The International Journal of Oral Maxillofacial Implants. 2009;24:920–926. [PubMed] [Google Scholar]
- Enkling N, Jöhren P, Klimberg V, Bayer S, Mericske-Stern R, Jepsen S. Effect of platform switching on peri-implant bone levels: a randomized clinical trial. Clinical Oral Implants Research. 2011;22:1185–1192. doi: 10.1111/j.1600-0501.2010.02090.x. [DOI] [PubMed] [Google Scholar]
- Fernández-Formoso N, Rilo B, Mora MJ, Martínez-Silva I, Díaz-Afonso AM. Radiographic evaluation of marginal bone maintenance around tissue level implant and bone level implant: a randomised controlled trial. A 1-year follow-up. Journal of Oral Rehabilitation. 2012;39:830–837. doi: 10.1111/j.1365-2842.2012.02343.x. [DOI] [PubMed] [Google Scholar]
- Gultekin BA, Gultekin P, Leblebicioglu B, Basegmez C, Yalcin S. Clinical evaluation of marginal bone loss and stability in two types of submerged dental implants. The International Journal of Oral and Maxillofacial Implants. 2013;28:815–823. doi: 10.11607/jomi.3087. [DOI] [PubMed] [Google Scholar]
- Hürzeler MB, Fickl S, Zuhr O, Wachtel HC. Peri-implant bone level around implants with platform-switched abutments: preliminary data from a prospective study. Journal of Oral and Maxillofacial Surgery. 2007;65(Suppl 1):33–39. doi: 10.1016/j.joms.2007.03.024. [DOI] [PubMed] [Google Scholar]
- Kielbassa AM, de Fuentes RM, Goldstein M, Arnhart C, Barlattani A, Jackowski J, Knauf M, Lorenzoni M, Maiorana C, Mericske-Stern R, Rompen E, Sanz M. Randomized controlled trial comparing a variable-thread novel tapered and a standard tapered implant: interim one-year results. The Journal of Prosthetic Dentistry. 2009;101:293–305. doi: 10.1016/S0022-3913(09)60060-3. [DOI] [PubMed] [Google Scholar]
- Peñarrocha-Diago MA, Flichy-Fernández AJ, Alonso-González R, Peñarrocha-Oltra D, Balaguer-Martínez J, Peñarrocha-Diago M. Influence of implant neck design and implant-abutment connection type on peri-implant health. Radiological study. Clinical Oral Implants Research. 2012;24:1192–1200. doi: 10.1111/j.1600-0501.2012.02562.x. [DOI] [PubMed] [Google Scholar]
- Pieri F, Aldini NN, Marchetti C, Corinaldesi G. Influence of implant-abutment interface design on bone and soft tissue levels around immediately placed and restored single-tooth implants: a randomized controlled clinical trial. The International Journal of Oral Maxillofacial Implants. 2011;26:169–178. [PubMed] [Google Scholar]
- Prosper L, Redaelli S, Pasi M, Zarone F, Radaelli G, Gherlone EF. A randomized prospective multicenter trial evaluating the platform-switching technique for the prevention of postoperative crestal bone loss. The International Journal of Oral Maxillofacial Implants. 2009;24:299–308. [PubMed] [Google Scholar]
- Telleman G, Raghoebar GM, Vissink A&, Meijer HJA. Impact of platform switching on peri-implant bone remodelling around short implants in the posterior region, 1-year results from a split-mouth clinical trial. Clinical Implant Dentistry and Related Research. 2012a doi: 10.1111/j.1708-8208.2012.00461.x. doi: 10.1111/j.1708-8208.2012.00461.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Telleman G, Raghoebar GM, Vissink A, Meijer HJA. Impact of platform switching on inter-proximal bone levels around short implants in the posterior region; 1-year results from a randomized clinical trial. Journal of Clinical Periodontology. 2012b;39:688–697. doi: 10.1111/j.1600-051X.2012.01887.x. [DOI] [PubMed] [Google Scholar]
- Trammell K, Geurs NC, O′Neal SJ, Lui P-R, Haigh SJ, McNeal S, Kenealy JN, Reddy MS. A prospective, randomized, controlled comparison of platform-switched and matched-abutment implants in short-span partoial denture situations. The International Journal of Periodontics and Restorative Dentistry. 2009;29:599–605. [PubMed] [Google Scholar]


