Abstract
Elderly Americans, especially those with multiple chronic conditions, face difficulties paying for prescriptions, resulting in worse adherence and discontinuation of therapy (“cost-related medication nonadherence” or CRN). We investigated whether the gains in medication affordability attributable to Medicare Part D implementation in January 2006 persisted during the six years that followed. Overall, we found continued incremental improvements in medication affordability in the early years of Part D (2007–2009), which then eroded during more recent years (2009–2011). Among elderly beneficiaries with four or more chronic conditions, we observed an increase in the prevalence of CRN from 14.4% in 2009 to 17.0% in 2011, reversing previous downward trends. Similarly, the prevalence of forgoing basic needs in order to purchase medicines among the sickest elderly decreased from 8.7% in 2007 to 6.8% in 2009, then rose to 10.2% in 2011. Our findings highlight the need for targeted policy efforts to alleviate the persistent burden of drug treatment costs in this vulnerable population.
Introduction
Elderly Americans typically have few financial resources available for prescription drugs.1 High out-of-pocket drug costs are associated with worse adherence and medication discontinuation.2 Such cost-related medication nonadherence (CRN) can lead to adverse health outcomes including worse health status and increased risk of hospitalization.3–5
Adequate adherence to medications is particularly important for seniors with multiple chronic conditions. Effective and efficient care for a growing elderly population with multiple chronic conditions is among the most important challenges the US health care system faces.6 Yet, older individuals with multiple chronic conditions are at especially high risk of CRN due to intensive medication use and high out-of-pocket costs.7
The Medicare Part D drug benefit was implemented in 2006 to increase economic access to medicines by decreasing beneficiaries’ out-of-pocket drug expenditures.8 Early evaluations of Part D indicated modest but significant nationwide reductions in CRN and forgoing basic needs to pay for medicines in 2006,9 which were sustained in 2007.10 Improvements in ability to afford medicines were not consistent across subgroups.9–11 In particular, improvements in CRN among elderly with four or more chronic conditions lagged behind improvements for healthier beneficiaries.9 Nevertheless, Part D resulted in significant increases in prescription drug use and lower out-of-pocket drug costs among almost all subgroups of the Medicare population.12
In 2008, the US entered the worst economic recession since the Great Depression. Between 2007 and 2010, the housing market collapsed, financial markets sank into turmoil, and family incomes, home prices, and investment portfolio values fell;13 wealth for elderly households declined by approximately 20% between 2007 and 2009.14,15 The recession and its aftermath left many elderly Americans facing unprecedented economic uncertainty.16 In addition, over the years following Part D implementation, changes in Part D plan benefits potentially introduced barriers to drug therapy and shifted costs onto patients.17–19
There have been no published reports on the prevalence of CRN among the multimorbid elderly in Medicare since 2008.10,20 In this study, we evaluate recent national trends in CRN and spending less on basic needs to afford medicines among elderly beneficiaries by illness burden, and explore the extent to which improvements in affordable access to medications resulting from Part D persisted during subsequent years.
Methods
Data Source and Sample
We used the Access-to-Care (ATC) files of the Medicare Current Beneficiary Survey (MCBS), the principal national survey for Medicare beneficiaries. Administered by the Centers for Medicare and Medicaid Services (CMS), the MCBS is a longitudinal, nationally representative rotating panel survey of approximately 16,000 disabled and elderly Medicare enrollees, who are representative of 42.5 million beneficiaries nationwide. Respondents provide information on health care utilization, expenditures and sources of payments, health insurance coverage, health status and functioning, and a variety of demographic and behavioral factors.21
The MCBS ATC files used in this study included the annual “always enrolled” beneficiary population, i.e., excluding individuals who newly enrolled in Medicare or died during a given calendar year. ATC data primarily consist of responses to the main fall interview, following a four-year panel survey design. The annual replenishment strategy replaces those who have completed survey participation, died, or been lost to follow-up, ensuring a representative sample in each calendar year. The average response rate across the study years (2006–2011) was 79.7% among first-time respondents and 67.0% among all respondents. We included all community-dwelling elderly respondents (approximately 79% of the total, excluding persons under 65 years and those residing in long-term care facilities) from 2006 through 2011 (n = 70,067 person-years). Accounting for overlapping samples among years, the total number of individual respondents was 31,713.
Outcome Measures
Since 2004, the MCBS fall interview has included a set of questions on the affordability of medications which were developed in collaboration with CMS, tested for reliability,22 and used in several studies by the research team.7,9–11,22,23 The main outcomes for this study were cost-related medication nonadherence (hereafter referred to as CRN) and spending less on other basic needs to afford medicines (forgoing basic needs).22,24,25 We used our validated binary composite measure of CRN if a respondent answered yes/ever during the current year to any of the following questions: “did not fill a prescription because of cost?”; “skipped doses to make the medicine last longer?”; “taken smaller doses of a medicine to make the medicine last longer?”; “delayed filling prescription because of cost?”; or, “any medicines prescribed for you that you did not get?” in combination with “reason you did not obtain the medicine was you thought it would cost too much”. We also examined a separate binary measure of having spent less money on food, heat, or other basic needs in order to have money for medicine.7,9–11
Statistical Analysis
We estimated the rates and 95% confidence intervals (CIs) of demographic and health characteristics of respondents. Covariates included previously validated predictors of CRN:7,26 age and sex, in addition to self-reported income, race, health status,27 and presence of specific diseases or conditions. Morbidities included cardiac disease, hypertension, diabetes, cancer, stroke, arthritis, dementia, psychiatric disorder (including depression), neurological disorder (excluding stroke), and pulmonary illness (including asthma and chronic obstructive pulmonary disease). We then calculated the unadjusted annual prevalence of CRN and spending less on basic needs with 95% CIs for all study years (2006–2011), as well as for 2004 and 2005 to illustrate pre-Part D levels. All survey analyses were weighted to represent the national population of community-dwelling elderly Medicare beneficiaries, using the annual cross-sectional survey weights provided in the MCBS.28
To model changes in CRN and spending less on basic needs in the years since Part D implementation, we used logistic regression models. Dividing the study years into two periods, our models compared the odds of CRN and spending less on basic needs between pairs of years (2009 vs. 2007, and 2011 vs. 2009), as well as the entire period (2011 vs. 2007). The year 2007 was the first for which the Part D benefit was fully implemented; 2009 was the first year following the financial market collapse in September 2008, which triggered public awareness of the economic crisis and steep declines in multiple indicators, including the unemployment rate, family income and wealth, and housing prices.29–31 During our final study period (2009 to 2011), external data suggest that scattered signs of economic recovery did not often translate into improved conditions for the elderly; rather, most indicators such as income and savings showed continued stagnation.16,32–34
As in previous reports,9,10 our models controlled for interview sequence, demographic characteristics (sex, age, income, and race), and health status (number of morbidities and health status). We repeated these analyses separately for eight subgroups based on the number of chronic conditions (0–3 and ≥4), income (<$25 000 and ≥$25 000), and type of prescription drug coverage (Part D low-income subsidy, Medicare Advantage, stand-alone prescription drug plan, and non-Part D).7,26 All analyses were conducted in STATA version 12 (StataCorp LP, College Station, TX). This study was reviewed and approved by the Human Subjects Committee of the Harvard Pilgrim Health Care Institute.
Results
Characteristics of Elderly Medicare Beneficiaries
The demographic and health characteristics of the community-dwelling elderly Medicare beneficiary population were similar across study years (Exhibit 1). The proportion reporting four or more conditions increased from 26.7% in 2007 to 27.6% in 2011. During the same period, the proportion enrolled in Medicare Part D increased, particularly for Medicare Advantage plans (17.7% to 21.4%), while non-Part D drug coverage plans became less common.
Exhibit 1.
Characteristics of community-dwelling elderly Medicare beneficiaries in 2007, 2009, and 2011.
| % | |||
|---|---|---|---|
| Characteristics | 2007 (n = 12,190) |
2009 (n = 11,393) |
2011 (n = 11,600) |
| Female sex | 56.4 | 56.1 | 56.3 |
| Age groups | |||
| 65–74 | 50.8 | 52.2 | 53.0 |
| 75–84 | 36.5 | 34.3 | 33.3 |
| ≥85 | 12.7 | 13.5 | 13.6 |
| Income, <$25,000a | 49.6 | 46.1 | 43.8 |
| Black race | 7.7 | 7.9 | 8.0 |
| Number of morbidities | |||
| 0–3 | 73.3 | 73.3 | 72.4 |
| ≥4 | 26.7 | 26.7 | 27.6 |
| Self-reported health status | |||
| Excellent, very good, or good | 78.7 | 81.0 | 80.7 |
| Fair or poor | 21.3 | 19.0 | 19.3 |
| Prescription drug coverageb | |||
| Part D: Low-Income Subsidy | 13.9 | 13.2 | 14.0 |
| Part D: Medicare advantage plan | 17.7 | 20.3 | 21.4 |
| Part D: Stand-alone drug plan | 23.3 | 23.4 | 24.4 |
| Non-Part D coverage | 42.2 | 39.8 | 36.9 |
| None | 2.9 | 3.3 | 3.3 |
Source: Authors’ analysis.
Notes:
MCBS variable, not adjusted for inflation.
Estimated using a combination of self-reported and CMS administrative data, available in the MCBS ATC. Presented hierarchically, such that beneficiaries with a mix of coverage types are counted in the category appearing first. “Non-Part D coverage” includes employer-sponsored drug coverage for current or retired workers, Tricare for veterans, self-purchased plans, and other public and private coverage sources; non-Part D sources above may not all qualify as “creditable”. (Reference: Centers for Medicare and Medicaid Services (CMS). What is creditable coverage? 2006; http://www.cms.gov/Medicare/Prescription-Drug-Coverage/CreditableCoverage/Downloads/whatiscreditablecoverage.pdf. Accessed March 13, 2013.)
Unadjusted Changes in Medication Affordability
An estimated 14.9% of elderly beneficiaries experienced CRN in 2005, and 11.3% in 2007 after the full implementation of Medicare Part D (Supplementary Appendix Exhibit 1). Following a downward trend until 2009, when 10.2% of beneficiaries had CRN, the estimated prevalence of CRN subsequently increased to 10.8% in 2011. Similarly, the percentage of beneficiaries forgoing other needs to pay for medicines declined after Part D (8.8% in 2005 to 5.6% in 2007), reaching 4.0% in 2009. In 2011, 5.3% of elderly beneficiaries cut back on basic needs to afford medications.
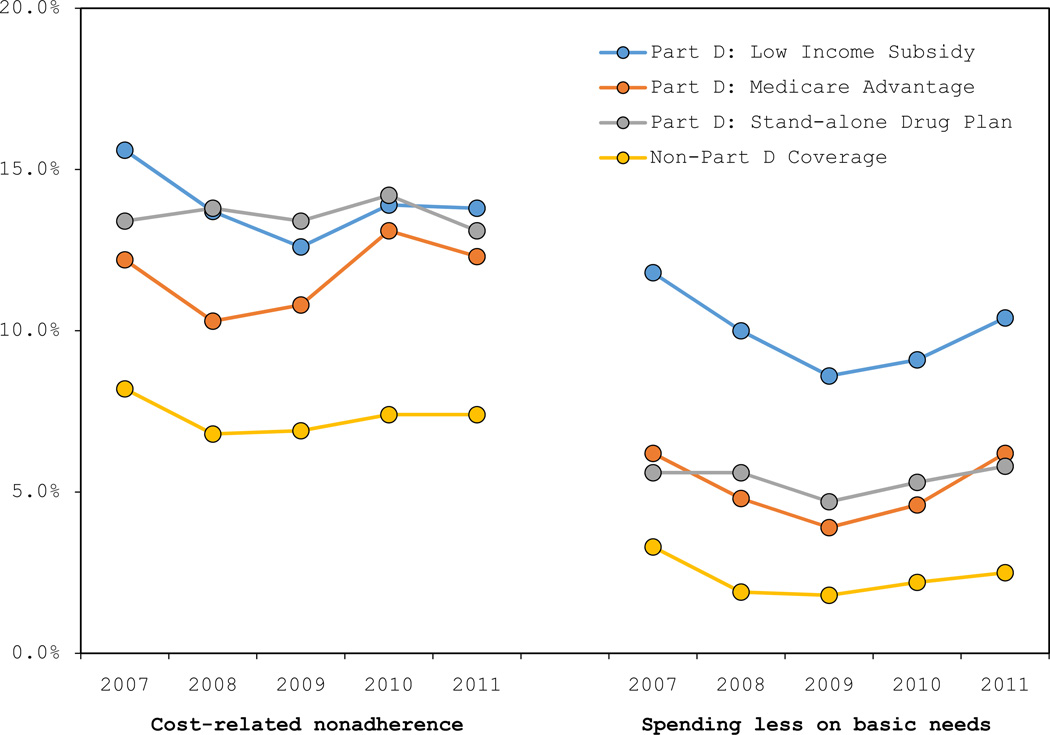
Between 2007 and 2011, elderly beneficiaries with non-Part D prescription drug coverage had consistently lower rates of CRN and spending less on basic needs than those participating in Medicare Part D (Exhibit 2). The risk of foregoing basic needs to afford medications among beneficiaries receiving the low-income subsidy was higher than that among other coverage groups. We observed similar increases in both measures across all major prescription drug coverage categories between 2009 and 2011.
Exhibit 2.
Prevalence of CRN and spending less on basic needs among the overall population of community-dwelling elderly Medicare beneficiaries by prescription drug coverage type (2007–2011).a, b.
Source: Authors’analysis.
Notes:
a Non-Part D coverage includes employer-sponsored coverage for current or retired workers as well as Tricare for veterans, self-purchased plans, and other public and private coverage.
b Prevalence of affordability problems among those with no prescription drug coverage (<4% of elderly) is not included due to sparse data.
Changes in Medication Affordability by Morbidity Burden
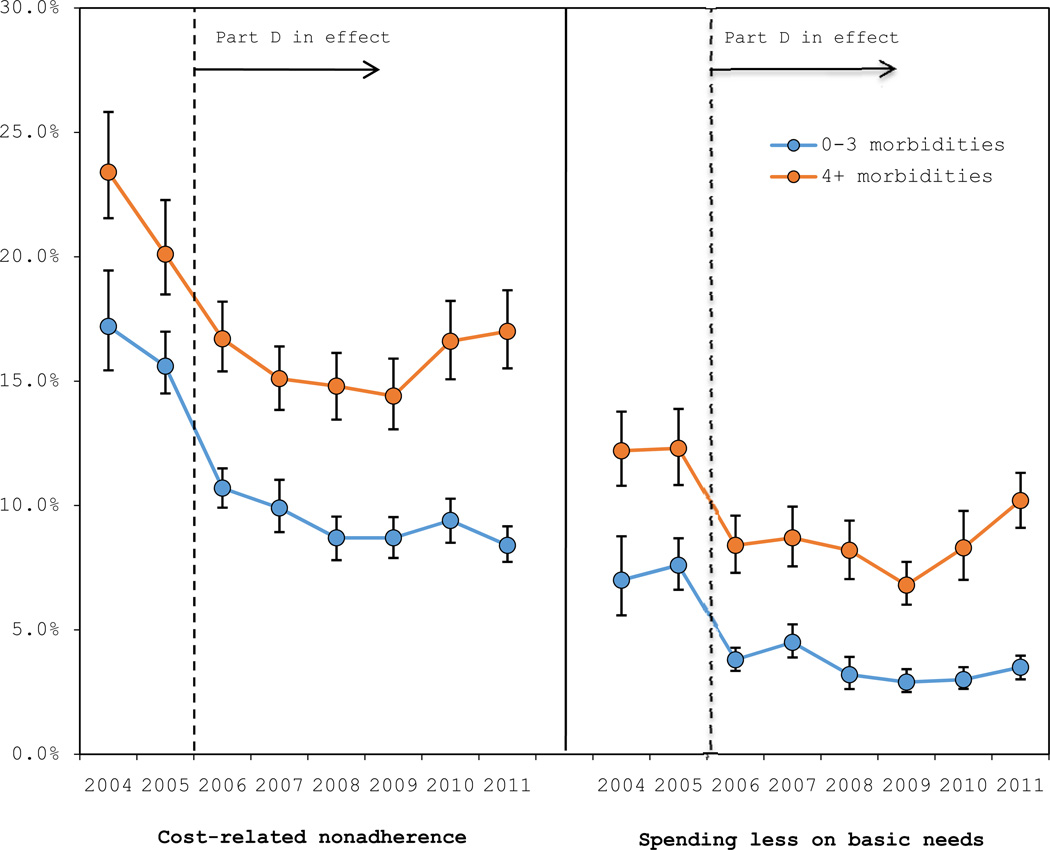
Across all study years, elderly with multiple chronic conditions had more problems affording their medications than other elderly (Exhibit 3). In 2005, prior to Part D, an estimated 20.3% of elderly beneficiaries with four or more chronic conditions experienced CRN. In the early years following the initial Part D impact,9 both measures of economic barriers to paying for medicines continued to decline slightly: the prevalence of CRN decreased from 15.1% in 2007, after Part D, to 14.4% in 2009. However, this trend reversed in subsequent years, rising to 17.0% in 2011. Similarly, the percentage of sicker beneficiaries forgoing other needs to pay for medicines declined after Part D implementation (12.3% in 2005 to 8.7% in 2007). These declines subsequently continued under Part D until the outcome reached its lowest point in 2009 (6.8%). However, by 2011, the prevalence of forgoing basic needs had risen again to 10.2% of sicker beneficiaries.
Exhibit 3.
Prevalence of CRN and spending less on basic needs among community-dwelling elderly Medicare beneficiaries by burden of chronic conditions (2004–2011).a, b, c
Source: Authors’analysis
Notes:
a Estimated with survey weights to represent the national population of community-dwelling elderly Medicare beneficiaries.
b Error bars represent 95% CIs around prevalence rates.
c Corrected CRN measure not available prior to 2006. Due to a survey field error, our composite measure of CRN did not fully capture “not filling a prescription” and omitted “delay filling” in 2004 and 2005. We estimated 2004 and 2005 values in the figure above by applying the relative increase in CRN (corrected measure vs. the underestimate without the newly captured data) observed during 2006–2011.
Among elderly beneficiaries with three or fewer chronic conditions, prevalence of CRN also declined sharply following Medicare Part D implementation (from 15.7% in 2005 to 9.9% in 2007), and continued declining until 2009, leveling off in subsequent years. The prevalence of spending less on basic needs declined from 7.6% in 2005 to 4.5% in 2007 and 2.9% in 2009, rising slightly to 3.5% in 2011.
Adjusted Changes in Medication Affordability
Exhibit 4 shows the changes in CRN and spending less on basic needs over time estimated using multivariate models. The direction of change between 2007 and 2009 for both outcomes was consistently downward for all groups. Then, between 2009 and 2011, the prevalence of affordability problems remained fairly stable among elderly beneficiaries with three or fewer chronic conditions, while the sickest elderly experienced pronounced increases. The odds of CRN among elderly beneficiaries with four or more conditions increased significantly by 20% between 2009 and 2011 (OR: 1.20, 95% CI: 1.03, 1.40) (Supplemental Appendix Exhibit 2). Similarly, we detected a significant increase in the odds of forgoing basic needs in order to purchase medicines between 2009 and 2011 (OR: 1.54, 95% CI: 1.30, 1.82), reversing the previous downward trends (OR 2009 vs. 2007: 0.81, 95% CI: 0.67, 0.99).
Exhibit 4.
Changes in CRN (A) and spending less on basic needs (B) among overall and sub-groups of community-dwelling Medicare beneficiaries (See Supplemental Appendix Exhibit 1 for details).
| (A) Cost-related medication nonadherence | ||||
|---|---|---|---|---|
| Adjusted OR a | ||||
| Period 1 | Period 2 |
Overall Period |
||
| Group | No. b | 2009 vs. 2007 | 2011 vs. 2009 | 2011 vs. 2007 |
| Elderly | 69,697 | 0.90 | 1.05 | 0.95 |
| No. of morbidities | ||||
| 0–3 | 49,650 | 0.86 | 0.97 | 0.83* |
| ≥4 | 20,047 | 0.98 | 1.20* | 1.18* |
| Income, US$ | ||||
| <25,000 | 34,776 | 0.94 | 0.99 | 0.94 |
| ≥25,000 | 34,889 | 0.84 | 1.12 | 0.95 |
| (B) Spending less on basic needs | ||||
| Elderly | 69,656 | 0.71** | 1.34** | 0.96 |
| No. of morbidities | ||||
| 0–3 | 49,629 | 0.65** | 1.18 | 0.77* |
| ≥4 | 20,027 | 0.81* | 1.54** | 1.25* |
| Income, US$ | ||||
| <25,000 | 34,748 | 0.78** | 1.25* | 0.98 |
| ≥25,000 | 34,876 | 0.57** | 1.60** | 0.90 |
Source: Authors’ analysis.
Notes:
Adjusted for younger age, female sex, non-white race, income <$25,000, poor health, survey participation, and having 4 or more morbidities.
Numbers of person-years in subgroups do not necessarily add up to overall number of observations. Numbers vary with response rates and availability of data on subgroups.
P<0.05
P<0.001
In subgroup analyses by major prescription drug coverage categories, there was a significant increase in the odds of spending less on basic needs among elderly beneficiaries in Medicare Advantage prescription drug plans (OR 2011 vs. 2009: 1.62, 95% CI: 1.23, 2.12), and those with non-Part D coverage (OR 2011 vs. 2009: 1.42, 95% CI: 1.09, 1.85). We did not observe any other significant changes in either measure in these subgroup analyses (Exhibit 4; Supplemental Appendix Exhibit 3).
An examination of the full 6-year period of observation confirms that early gains were reversed among the sickest beneficiaries. Elderly beneficiaries with four or more chronic conditions had significantly worse outcomes in 2011 compared to 2007 (CRN OR: 1.18, 95% CI: 1.02, 1.36; forgoing basic needs OR: 1.25, 95% CI: 1.04, 1.51). We also observed that the prevalence of foregoing basic needs to afford medications among the sickest elderly in 2011 was no longer significantly better than the level reported in 2005, prior to Part D implementation (OR 2011 vs. 2005: 0.86, 95% CI: 0.72, 1.04). By contrast, there was no reversal among the healthier group. Those with fewer conditions had significantly better outcomes in 2011 as compared to 2007, though their improvements appeared to occur mainly between 2007 and 2009.
Discussion
In this study, we investigated recent national trends in CRN and forgoing other basic needs to pay for medicines among elderly Medicare beneficiaries. Strikingly, we found that financial barriers to prescription drug therapy represent a continuing problem for the sickest Medicare beneficiaries, who are at higher risk of CRN due to illness burden, intense medication needs, and high out-of-pocket costs.7 For the first time since 2004, when affordability indicators were added to a nationally representative survey of elderly Medicare beneficiaries, a trajectory of improvements in both CRN and forgoing basic needs reversed course around 2009: drug affordability deteriorated significantly in subsequent years among the sickest elderly. In 2011, elderly individuals with four or more chronic conditions were worse off in terms of both outcomes than they had been in 2007. In fact, the risk of foregoing basic needs among this key group in 2011 was not significantly better than it had been prior to Part D, suggesting that both the original Part D impact and interim improvements may have been eliminated.
Several factors likely reversed the early gains in medication affordability following Part D implementation, and disproportionately affected the sickest elderly. The severe economic downturn in the US shrank incomes, asset values, and wealth for all age groups including the elderly. Elders also had high rates of mortgage delinquency, which has been associated with CRN.35 It is very likely that new economic strains affected the ability of elderly beneficiaries with multiple chronic conditions to afford their medications. During the same period, the zero cost-of-living adjustment (COLA) in social security may have also affected medication affordability.36
In addition, there is evidence of reduced drug coverage generosity in recent years.18,19 Over our observation period, Part D plans increased premiums and more have begun to charge deductibles. Plans have also generally increased patient copayments within formulary tiers, and more frequently applied restrictions such as prior authorization requirements.17,19,37 While these benefit changes may have been designed to steer patients toward less expensive medications, they may also have had the effect of introducing barriers to drug therapy and shifting the overall drug cost burden toward patients, particularly those with multiple chronic conditions.
We investigated whether the recent worsening trends in medication affordability could be attributed to changes in beneficiaries’ type of prescription drug coverage, and found that there were generally similar increases across all major coverage sources. It is therefore unlikely that Part D plan changes alone were responsible for rising problems of access to medications. Indeed, published reports documented similar reductions in generosity more generally in US health insurance, which potentially compounded the effect of the economic downturn.38,39 Such changes across the healthcare system could explain why elderly Americans are reporting persistent affordability problems while news reports simultaneously exclaim that “[total US] spending on prescription drugs fell for the first time on record”.40
The Affordable Care Act (ACA) is set to broaden access to public and private health insurance and improve Medicare Part D coverage. Specifically, by 2020, CMS will gradually phase out the Medicare Part D coverage gap (or “doughnut hole”) in which beneficiaries who have reached a defined total drug spending threshold must then pay 100% out of pocket until they reach a “catastrophic” level. The ACA has provided financial relief to elderly beneficiaries in the coverage gap by persuading pharmaceutical companies to offer a 50% discount on branded drugs starting in 2011, and by gradually adding government subsidies to fill the remaining gap for brand and generic drugs.
Given the constant evolution of policies affecting the Medicare population, policymakers and researchers must closely monitor trends in affordability such as those we highlight here, and support more in-depth investigation of the underlying causes. Policymakers should also consider additional strategies to help the sickest beneficiaries, who clearly remain burdened by medication costs. Policy options include increased outreach to and participation in the Part D low-income subsidy for qualified individuals in need.41 Beneficiaries may also need more assistance in selecting a Part D plan that fits their medical and financial circumstances, given reports that they often choose plans that require more out-of-pocket spending than necessary.42 Programs focusing on clinicians and pharmacists can help patients mitigate excessive costs, for example, by substituting lower-cost therapies with comparable benefit-harm profiles.43 Increasing low-income subsidy enrollment and assisting beneficiaries with better choices can potentially improve affordability for Medicare beneficiaries in all current coverage categories.
The findings of this study should be interpreted in light of its limitations. We are able to describe recent reversals in affordability, but the data do not permit us to definitively determine the root causes. For example, data on actual drug utilization and out-of-pocket spending by MCBS respondents are not yet available for the most recent years of observation, and the recession literature does not clearly pinpoint the timing of harms as they affected specific population segments, such as the elderly. In addition, self-reports could be subject to reporting and recall biases. Nevertheless, the affordability measures used in our study have been validated22,24,25 and used extensively in previous studies,7,9–11,23,44 and we expect potential misreporting of CRN behavior to be consistent over time.
Perhaps unsurprisingly, we detected more statistically significant changes in our measure of cutting back on basic needs to afford medications, as compared to the CRN measure. This suggests that the basic needs question may be a more direct measure of patients’ economic hardship and more sensitive to changes in financial circumstances over time. CRN addresses specific clinical behaviors that are subject to influences beyond economic hardship, such as ongoing health system efforts to increase adherence and providers’ ability to adapt regimens to patients’ economic circumstances. In tandem, these measures have demonstrated their sensitivity and utility as a barometer of medication affordability in a stable survey population.
The body of research evaluating the impact of Medicare Part D provided unequivocal evidence of population-level decreases in out-of-pocket costs and increased medication use following its implementation in 2006.12,45 Nevertheless, using data on a nationally representative sample of Medicare beneficiaries, we provide updated evidence that many elderly Americans face persistent, and indeed, worsening, economic barriers to prescription drug therapy. Our finding that the gains in medication affordability among elderly with multiple chronic conditions following Part D were later lost during a period of both economic downturn and benefit changes highlights a pressing need to find new ways to ensure economic access to drug treatment for vulnerable Medicare beneficiaries.
Supplementary Material
Endnotes
- 1.Briesacher BA, Ross-Degnan D, Wagner AK, et al. Out-of-pocket burden of health care spending and the adequacy of the Medicare Part D low-income subsidy. Med Care. 2010 Jun;48(6):503–509. doi: 10.1097/MLR.0b013e3181dbd8d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007 Jul 4;298(1):61–69. doi: 10.1001/jama.298.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heisler M, Langa KM, Eby EL, Fendrick AM, Kabeto MU, Piette JD. The health effects of restricting prescription medication use because of cost. Med Care. 2004 Jul;42(7):626–634. doi: 10.1097/01.mlr.0000129352.36733.cc. [DOI] [PubMed] [Google Scholar]
- 4.Soumerai SB, McLaughlin TJ, Ross-Degnan D, Casteris CS, Bollini P. Effects of Limiting Medicaid Drug-Reimbursement Benefits on the Use of Psychotropic Agents and Acute Mental Health Services by Patients with Schizophrenia. N Engl J Med. 1994;331(10):650–655. doi: 10.1056/NEJM199409083311006. [DOI] [PubMed] [Google Scholar]
- 5.Soumerai SB, Ross-Degnan D, Avorn J, McLaughlin T, Choodnovskiy I. Effects of Medicaid drug-payment limits on admission to hospitals and nursing homes. N Engl J Med. 1991 Oct 10;325(15):1072–1077. doi: 10.1056/NEJM199110103251505. [DOI] [PubMed] [Google Scholar]
- 6.Vogeli C, Shields AE, Lee TA, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. 2007 Dec;22(Suppl 3):391–395. doi: 10.1007/s11606-007-0322-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soumerai SB, Pierre-Jacques M, Zhang F, et al. Cost-related medication nonadherence among elderly and disabled medicare beneficiaries: a national survey 1 year before the medicare drug benefit. Arch Intern Med. 2006 Sep 25;166(17):1829–1835. doi: 10.1001/archinte.166.17.1829. [DOI] [PubMed] [Google Scholar]
- 8.Kaiser Family Foundation. The Medicare Prescription Drug Benefit: A Fact Sheet. [Accessed January 7, 2013];2012 http://www.kff.org/medicare/upload/7044-13.pdf. [Google Scholar]
- 9.Madden JM, Graves AJ, Zhang F, et al. Cost-related medication nonadherence and spending on basic needs following implementation of Medicare Part D. JAMA. 2008 Apr 23;299(16):1922–1928. doi: 10.1001/jama.299.16.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Madden JM, Graves AJ, Ross-Degnan D, Briesacher BA, Soumerai SB. Cost-related medication nonadherence after implementation of Medicare Part D, 2006–2007. JAMA. 2009 Oct 28;302(16):1755–1756. doi: 10.1001/jama.2009.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zivin K, Madden JM, Graves AJ, Zhang F, Soumerai SB. Cost-related medication nonadherence among beneficiaries with depression following Medicare Part D. Am J Geriatr Psychiatry. 2009 Dec;17(12):1068–1076. doi: 10.1097/JGP.0b013e3181b972d1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Briesacher BA, Zhao Y, Madden JM, et al. Medicare part D and changes in prescription drug use and cost burden: national estimates for the Medicare population 2000 to 2007. Med Care. 2011 Sep;49(9):834–841. doi: 10.1097/MLR.0b013e3182162afb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jesse Bricker, Arthur Kennickell, Moore Kevin B, Sabelhaus John. Changes in US Family Finances from 2007 to 2010: Evidence from the Survey of Consumer Finances. Federal Reserve Bulletin. 2012;98(2) [Google Scholar]
- 14.Jesse Bricker, Brian Bucks, Arthur Kennickell, Traci Mach, Moore K. Surveying the Aftermath of the Storm: Changes in Family Finances from 2007 to 2009. Washington DC: Divisions of Research and Statistics and Monetary Affairs, Federal Reserve Board; 2011. [Google Scholar]
- 15.Reno Virginia P, Veghte B. Economic Status of the Elderly in the United States. Washington, DC: National Academy of Social Insurance; 2010. [Google Scholar]
- 16.AARP Public Policy Institute. Boomers and the Great Recession: Struggling to Recover. 2012 [Google Scholar]
- 17.Neuman P, Cubanski J. Medicare Part D Update - Lessons Learned and Unfinished Business. N Engl J Med. 2009;361(4):406–414. doi: 10.1056/NEJMhpr0809949. [DOI] [PubMed] [Google Scholar]
- 18.Kaiser Family Foundation. Data Spotlight: Medicare Part D - A First Look at Part D Plan Offerings in 2013. 2013 http://www.kff.org/medicare/upload/8375.pdf. [Google Scholar]
- 19.Kaiser Family Foundation. Medicare Part D Prescription Drug Plans: The marketplace in 2013 and key trends, 2006–2013. [Accessed March 8, 2014];2014 http://kff.org/medicare/issue-brief/medicare-part-d-prescription-drug-plans-the-marketplace-in-2013-and-key-trends-2006-2013/. [Google Scholar]
- 20.Harrold LR, Briesacher BA, Peterson D, et al. Cost-related Medication Nonadherence in Older Patients with Rheumatoid Arthritis. J Rheumatol. 2013 Feb;40(2):137–143. doi: 10.3899/jrheum.120441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Medicare and Medicaid Services (CMS) Technical Documentation for the Medicare Current Beneficiary Study. Baltimore, MD: 2002. [Google Scholar]
- 22.Pierre-Jacques M, Safran DG, Zhang F, et al. Reliability of new measures of cost-related medication nonadherence. Med Care. 2008 Apr;46(4):444–448. doi: 10.1097/MLR.0b013e31815dc59a. [DOI] [PubMed] [Google Scholar]
- 23.Nekhlyudov L, Madden J, Graves AJ, Zhang F, Soumerai SB, Ross-Degnan D. Cost-related medication nonadherence and cost-saving strategies used by elderly Medicare cancer survivors. J Cancer Surviv. 2011 Dec;5(4):395–404. doi: 10.1007/s11764-011-0188-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Safran DG, Neuman P, Schoen C, et al. Prescription drug coverage and seniors: findings from a 2003 national survey. Health Aff (Millwood) 2005 Jan-Jun; doi: 10.1377/hlthaff.w5.152. Suppl Web Exclusives:W5-152-W155-166. [DOI] [PubMed] [Google Scholar]
- 25.Safran DG, Neuman P, Schoen C, et al. Prescription drug coverage and seniors: how well are states closing the gap? Health Aff (Millwood) 2002 Jul-Dec; doi: 10.1377/hlthaff.w2.253. Suppl Web Exclusives:W253-268. [DOI] [PubMed] [Google Scholar]
- 26.Briesacher BA, Gurwitz JH, Soumerai SB. Patients at-risk for cost-related medication nonadherence: a review of the literature. J Gen Intern Med. 2007 Jun;22(6):864–871. doi: 10.1007/s11606-007-0180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DeSalvo KB, Fan VS, McDonell MB, Fihn SD. Predicting Mortality and Healthcare Utilization with a Single Question. Health Serv Res. 2005;40(4):1234–1246. doi: 10.1111/j.1475-6773.2005.00404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Briesacher Becky A., Tjia Jennifer, Doubeni Chyke A., CHen Yog, Rao Sowmya R. Methodological Issues in Using Multiple Years of the Medicare Current Beneficiary Survey. Medicare & Medicaid Research Review. 2012;2(1):E1–E20. doi: 10.5600/mmrr.002.01.a04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.United States Senate Permanent Subcommittee on Investigations. Wall Street and the Financial Crisis: Anatomy of a Financial Collapse: Majority and Minority Staff Report. Washington, DC: 2011. [Google Scholar]
- 30.Hall RE. Why Does the Economy Fall to Pieces after a Financial Crisis? The Journal of Economic Perspectives. 2010;24(4):3–20. [Google Scholar]
- 31.Dominguez KME, Shapiro MD. Forecasting the Recovery from the Great Recession: Is This Time Different? National Bureau of Economic Research Working Paper Series. 2013 No. 18751. [Google Scholar]
- 32.Assessing the Impact of Severe Economic Recession on the Elderly: Summary of a Workshop. The National Academies Press; 2011. Malay Majmundar and Steering Committee on the Challenges of Assessing the Impact of Severe Economic Recession on the Elderly. [PubMed] [Google Scholar]
- 33.United States Government Accountability Office. Income Security: Older Adults and the 2007–2009 Recession. Washington, DC: 2011. [Google Scholar]
- 34.AARP Public Policy Institute. [Accessed March 27, 2013];Recovering from the Great Recession: Long Struggle Ahead for Older Americans. 2011 http://assets.aarp.org/rgcenter/ppi/econ-sec/insight50_recovering.pdf. [Google Scholar]
- 35.Alley DE, Lloyd J, Pagán JA, Pollack CE, Shardell M, Cannuscio C. Mortgage Delinquency and Changes in Access to Health Resources and Depressive Symptoms in a Nationally Representative Cohort of Americans Older Than 50 Years. [2011/12/01];American Journal of Public Health. 2011 101(12):2293–2298. doi: 10.2105/AJPH.2011.300245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Penner RG. Medicare Premiums and Social Security's Cost-of-Living Adjustments. 2011 [Google Scholar]
- 37.Hoadley J, Hargrave E, Merrell K. Medicare Part D Formularies, 2006–2011: Update to Chartbook. A study conducted by staff from NORC at the University of Chicago, Georgetown University, and Social & Scientific Systems, Inc., for the Medicare Payment Advisory Commission; 2011. [Google Scholar]
- 38.Roehrig C, Turner A, Hughes-Cromwick P, Miller G. When the Cost Curve Bent — Pre-Recession Moderation in Health Care Spending. N Engl J Med. 2012;367(7):590–593. doi: 10.1056/NEJMp1205958. [DOI] [PubMed] [Google Scholar]
- 39.Truffer CJ, Keehan S, Smith S, et al. Health Spending Projections Through 2019: The Recession's Impact Continues. Health Affairs. 2010 Feb 4; doi: 10.1377/hlthaff.2009.1074. 2010. [DOI] [PubMed] [Google Scholar]
- 40.US Spending on Traditional Prescription Drugs Fell in 2012 for First Time on Record. New York Times. 2013 [Google Scholar]
- 41.Soumerai S. Fix the Medicare Drug Benefit. [Accessed July 1, 2013];Newsweek. 2007 http://www.thedailybeast.com/newsweek/2007/12/01/cures-for-an-ailing-system.html. [Google Scholar]
- 42.Zhou C, Zhang Y. The Vast Majority Of Medicare Part D Beneficiaries Still Don't Choose The Cheapest Plans That Meet Their Medication Needs. Health Affairs. 2012 Oct 1;31(10):2259–2265. doi: 10.1377/hlthaff.2012.0087. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alexander GC, Casalino LP, Meltzer DO. Physician strategies to reduce patients' out-of-pocket prescription costs. Archives of Internal Medicine. 2005;165(6):633–636. doi: 10.1001/archinte.165.6.633. [DOI] [PubMed] [Google Scholar]
- 44.Bambauer KZ, Safran DG, Ross-Degnan D, et al. Depression and cost-related medication nonadherence in Medicare beneficiaries. Arch Gen Psychiatry. 2007 May;64(5):602–608. doi: 10.1001/archpsyc.64.5.602. [DOI] [PubMed] [Google Scholar]
- 45.Polinski JM, Kilabuk E, Schneeweiss S, Brennan T, Shrank WH. Changes in drug use and out-of-pocket costs associated with Medicare Part D implementation: a systematic review. J Am Geriatr Soc. 2010 Sep;58(9):1764–1779. doi: 10.1111/j.1532-5415.2010.03025.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.